- 1Department of General Surgery, Endocrinology, Orthopedics and Rehabilitation, Federico II University of Naples, Naples, Italy
- 2Ospedale di Gallarate ASST Valle Olona, Milan, Italy
- 3Department of Medicine and Surgery for Digestive Tract Diseases, Federico II University of Naples, Naples, Italy
Bezoar is a term from Arabic “bāzahr” or ultimately from Middle Persian “p'tzhl” (pādzahr, “bezoar antidote” or less commonaly ægagropile or egagropile (2–4). It was believed to have the power of a universal antidote that works against any poison, and a glass containing a bezoar could neutralize any poison poured into it. In science, it is a mass of hair or undigested vegetable matter found in a human or animal intestines, similar to a hairball. Otherwise, the name could derive from a kind of Turkish goat whose name is just bezoar. Usually, it is found trapped in every part of the gastrointestinal system and must be distinguished by pseudobezoar, which is an nondigestible object voluntarily introduced into the digestive tract. The most common causes are a previous gastric surgery such as a gastric band (for weight loss) or gastric bypass, a reduced stomach acid (hypochlorhydria) or decreased stomach size, and a delayed gastric emptying, typically due to diabetes, autoimmune disorders, or mixed connective tissue disease. Seed bezoars are usually found in the rectum of patients without predisposing factors, causing constipation and pain. Rectal impaction is common after ingestion of seeds, while a true occlusion is rare. Although several cases of phytobezoars composed of various types of seeds are reported in the literature, bezoars of pumpkin seeds have rarely been reported. The authors report a case of fecal impaction by pumpkin seed bezoars with abdominal pain: a difficulty to void with subsequent rectal inflammation and hemorrhoid enlargement was observed. The patient underwent a successful manual disimpaction.
Introduction
In J.K. Rowling's Book of Harry Potter, the apprentice scientist is quizzed on bezoar during the very first Potions Class (1). Bezoar is a term from Arabic “bāzahr” or ultimately from Middle Persian “p'tzhl” (pādzahr, “bezoar antidote”) or less commonly ægagropile or egagropile (2–4). It was believed to have the power of a universal antidote and would work against any poison and that a drinking glass that contained a bezoar could neutralize any poison poured into it. In science, it is a mass of hair or undigested vegetable matter found in a human or animal intestines, similar to a hairball. Otherwise, the name could derive from a kind of Turkish goat whose name is just bezoar.
Usually, it is found trapped in every part of the gastrointestinal system and must be distinguished by pseudobezoar that is an nondigestible object voluntarily introduced into the digestive tract (5, 6).
Bezoars take the name from the core substance so that we can distinguish them: phytobezoars are composed of vegetable fibers and seeds, trichobezoars are formed from hair, lactobezoars are from inspissated milk, and diospyrobezoars are from unripe persimmon fruits (7).
The overall incidence of bezoars is felt to be low and is extremely rare in healthy individuals occurring in far less than 1% of patients in retrospective endoscopic series (7). Kadian et al. (8) reported that they found six cases of gastric bezoars in a 4-year period, during which time 1,400 gastroscopies were done (0.43% of gastroscopies). Ahn et al. (9) reported a similar incidence of 0.43% (14/3,247 esophagogastroduodenoscopy examinations) over a 7-year period. More recently, Mihai et al. (10) noted that there were 49 cases of gastric bezoars over a period of 20 years (0.068% of all endoscopies). Yakan et al. (9) reviewed 432 cases of small bowel obstruction treated within 10 years; of these, 14 (3.2%) cases were caused by phytobezoars. Multiple cases of persimmon phytobezoar (diospyrobezoar) have been reported in regions where the residents frequently consume fresh persimmon fruits and dried persimmons, such as South Korea, Japan, Israel, Spain, Turkey, and the southeastern United States. In a meta-analysis by Ghosheh et al. (11) reviewing 19 reported studies published from 1994 to 2005, laparoscopy was attempted in 1,061 patients presenting with acute small bowel obstruction, and bezoars represented the fifth most common cause, accounting for 0.8% (12).
Certain at-risk groups have been identified and include patients with altered upper GI anatomy after surgery and psychiatric illness or cognitive impairment. The most common causes are a previous gastric surgery such as a gastric band (for weight loss) or gastric bypass, a reduced stomach acid (hypochlorhydria) or decreased stomach size, and a delayed gastric emptying, typically due to diabetes, autoimmune disorders, or mixed connective tissue disease. Other causes are patients who cannot or do not chew their food properly, usually because they have no teeth or poorly fitting dentures and because of an excessive intake of fibers. Edentulous patients with poor mastication of food particles may also be at greater risk for bezoar development, especially if coexisting risk factors, as described above, are also present. In addition, patients with psychiatric illnesses are at an increased risk of bezoar formation due to the possible ingestion of hair and medications (8, 9).
Many cases of bezoars have also been reported in children or adults having psychosocial problems; nevertheless, the condition can occur in normal children with no apparent psychosocial issues (8).
Seed bezoars are usually found in the rectum of patients without predisposing factors, causing constipation and pain. Although the literature has reported several cases of phytobezoars composed of various types of seeds, bezoars formed from pumpkin seeds have rarely been reported (10). The diagnosis may be suggested by the radiologic study and is confirmed by endoscopy. History and digital rectal examination are the mainstays of diagnosis, with manual extraction under local anesthesia being the procedure of choice (13). CT scanning is useful for detecting both gastric and small intestinal bezoars. Phytobezoars are visualized by CT scanning as a round occupational mass in the gastrointestinal tract. Some cases of bezoars can be coincidentally found in asymptomatic patients by esophagogastroduodenoscopy or computed tomography (CT) scanning performed during a health check-up or follow-up of other diseases.
We report a case of a man aged 50 years with a rectal bezoar composed of pumpkin seeds ingested with their shell, necessitating extensive treatment, including manual disimpaction and rectoscopy.
Methodology
The description of the case follows the 2013 CARE Checklist Guidelines (13).
Case Report
Patient Information
A 50-year-old man with no significant medical history was observed in our outpatient room with a 3-day abdominal pain and difficulty passing anything rectally except some sprays of liquid stool. He also complained of hematochezia at defecation. A physical exam revealed a painful tenderness of the abdomen but the presence of normal bowel sounds.
The abdominal wall was mainly painful on the left.
He seemed scared and confused in reporting events and was accompanied by his mother. He reported having spent the Sunday afternoon alone watching TV and eating two bags of pumpkin seeds (about 400 g) with their shell. He was unemployed and showed a depressed attitude. He reported never having had problems of this nature before but having problems of constipation in the last months.
Diagnostic Findings
The plain x-ray of the abdomen showed dilatation of the left and bowel. A proctological inspection revealed a hard bolus in the rectum (Figure 1) with blood loss and a rectoscope examination showed a pumpkin bezoar impacted into the rectum (Figure 2). Starting from the history and results of the proctological inspection, the diagnosis of impaction from seeds was quite clear.
Therapeutic Intervention
Under sedation with propofol, a disimpaction of the bezoar was accomplished with a colon washing. The patient was discharged on the same evening with a prescription of intestinal antibiotics and a large bowel toilet with polyethylene glycol and enemas.
Outcomes
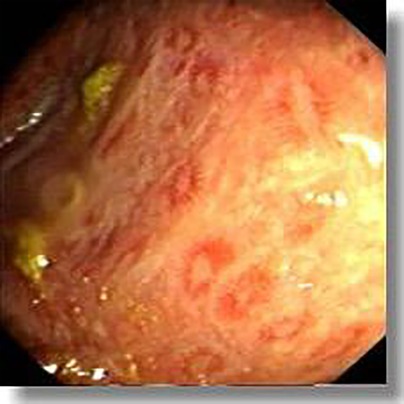
Two days after the first admission, the patient returned to the outpatient department complaining of a persistent difficulty to void with a burning sensation and blood loss. A residual hard bolus, smaller than the first, was detected in the rectum, and another disimpaction under local anesthesia was performed. A proctoscopy showed small diffuse ulcerations of the rectal mucosa and enlargement of hemorrhoids (Figure 3). The colon was empty at the end of the procedure. A daily topical application of sucralfate enemas, stool softeners, and fiber diet was prescribed, and the patient passed normal stools without pain the following day. A suggestion of psychological help was made.
Follow-up
Three weeks after this episode, the rectal mucosa reverted to normal, and the patient declared to move regularly without a burning sensation.
Discussion
Rectal seed bezoar is an uncommon cause of fecal impaction, more frequent in eastern than western countries and particularly in Middle Eastern and South Asian countries where roasted seeds are very popular (14). The composition of a bezoar is essentially mechanical due to its insoluble and indigestible content. The growth is increased by continuous ingestion of the nondegradable content. The most frequent site is the stomach, and rarely can it be observed in the colon and rectum. Clinical symptoms include nausea, vomiting, anorexia, constipation, and obstipation. Rectal ulcerations are not frequent even if the first report of a stercoral ulceration was described by Berry in 1894: an isolated ulcer produced by pressure necrosis of a fecal mass in the rectum (15).
Seed bezoar is a subcategory of phytobezoar caused by the accumulation of indigestible vegetable or fruit seeds in the intestine lumen. They usually pass the stomach and the ileocecal valve and deposit in the colon up to the rectum, where the compound is dehydrated and forms a hard bolus impossible to evacuate (16). Seed bezoars seem to arise mostly in patients without predisposing factors, as a review from the Manatakis report: 12% of cases of previous gastric surgery, neuropsychiatric illness, and endocrinopathies were reported, contrary to fiber bezoar where rates of risk factors exceed 85% (17).
Seed bezoar occurs most frequently in the rectum both in children and adults, and symptoms are mainly constipation followed by abdominal pain and rectal burning. A true intestinal obstruction is rare, and perforation is reported only in one case (18, 19). Fiber bezoar, due to its location in the stomach, causes specific symptoms such as nausea, vomiting, and abdominal bloating. Manual evacuation under general anesthesia for rectal bezoar is the treatment of choice to avoid discomfort to the patients, while surgery is mandatory in the case of intestinal obstruction from small seeds. Manual disimpaction is the most commonly used procedure both in children and adults, while surgery is more frequent in adults than in children (30% vs. 14.5%). Chemical dissolution of the mass works better with fiber bezoars than with seed bezoars; however, Coca Cola Zero is reported to be effective in breaking a phytobezoar into small pieces (20). Finally, endoscopy is ineffective because, in most cases, the endoscope cannot transit beyond the mass (21). In case of true occlusion, surgery is mandatory even if rare
From 1980 to 2018, 52 studies were reported by Manatakis (16) responding to eligibility criteria over a total of 102 papers published. From 2018 to today, another eight papers with a full text available were published. In four out of the eight, bezoar formation was from seeds (granadilla, mango, and sunflowers in two cases), but none of the patients ate pumpkin seeds (22). According to Manatakis, the major complaint was constipation followed by atypical abdominal or rectal pain. One elderly patient was diagnosed with acute abdomen due to rectal perforation, and one intraoperative incident finding was reported.
Preventive therapy to avoid recurrence must be implemented when the bezoar is removed. The patient should be advised to increase the amount of water intake. Dietary habits must be investigated since inadequate chewing, swallowing whole seeds, or eating seeds with their shell may impact as bezoar (11, 23, 24).
Finally, gastric bezoars are common in cystic fibrosis patients after lung transplantation. The etiology is likely multifactorial, related to gastric motility, respiratory secretions, and medications. Of the 215 patients who received lung transplantation, 17 (7.9%) developed gastric bezoars confirmed by upper endoscopy and 94% of patients with bezoars (16 of 17) had cystic fibrosis (P = 0.02), Further investigation is needed to understand the pathogenesis of bezoar formation in this selected population (25).
Conclusion
Seed bezoar is an uncommon cause of fecal impaction, more frequent in eastern than western countries and particularly in Middle Eastern and South Asian countries. Seed bezoar is a subcategory of phytobezoar caused by the accumulation of indigestible vegetable or fruit seeds in the intestinal lumen: it occurs most frequently in the rectum both in children and adults, and symptoms are constipation followed by abdominal pain and rectal burning. Intestinal obstruction is rare, and perforation is reported only in one case. Manual disimpaction is the commonly used procedure both in children and adults, while surgery is more frequent in adults than in children. Preventive therapy to avoid recurrence must be implemented when the bezoar is removed. An increase in the amount of water intake should be advised. Psychiatric support is mandatory in patients with recurrent episodes of seed ingestion.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
Ethical review and approval were not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
MG, general organization, clinical approach, and manuscript. LV, bibliographic research. VS, bibliographic research. GC, review of the manuscript. LS, endoscopic records.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rowling JK. Harry Potter and Philosopher's Stone. (2003), Scholastic Inc. (published first June 26th, 1997).
2. Park S-E, et al. Clinical outcomes associated with treatment nodalities for gastrointestinal bezoars. Gut Liver. (2014) 8(4):400–7. doi: 10.5009/gnl.2014.8.4.400
3. Mao Y, Qiu H, Liu Q, et al. Endoscopic lithotripsy for gastric bezoars by Nd:YAG laser-ignited mini-explosive technique. Lasers Med Sci. (2014) 29:1237–40. doi: 10.1007/s10103-013-1512-1
4. Iwamuro M, et al. Review of the diagnosis and management of gastrointestinal bezoars. World J Gastrointest Endosc. (2015) 7(4):336–45. doi: 10.4253/wjge.v7.i4.336
5. Mazzoleni A. Shellac and lipoid bezoar concretion of the stomach. Gastroenterologia. (1965) 104:316. doi: 10.1159/000202109
6. Vickery RD. Unusual complication of excessive ingestion of vitamin C. Am J Emerg Med. (1995) 13:112–3. 76. doi: 10.1016/0735-6757(95)90277-5
7. Andrus CH, Ponsky JL. Bezoars: classification, pathophysiology, and treatment. Am J Gastroenterol. (1988) 83(5):476–8. PMID: 3284334
8. Kadian RS, Rose JF, Mann NS. Gastric bezoars–spontaneous resolution. Am J Gastroenterol. (1978) 70:79–82. doi: 10.12659/MSM.926539
9. Yakan S, Sirinocak A, Telciler KE, Tekeli MT, Deneçli AG. A rare cause of acute abdomen: small bowel obstruction due to phytobezoar. Ulus Travma Acil Cerrahi Derg. (2010) 16:459–63. PMID: 21038126
10. Mihai C, Mihai B, Drug V, Cijevschi Prelipcean C. Gastric bezoars–diagnostic and therapeutic challenges. J Gastrointestin Liver Dis. (2013) 22:111. PMID: 23539409
11. Ghosheh B, Salameh JR. Laparoscopic approach to acute small bowel obstruction: review of 1061 cases. Surg Endosc. (2007) 21:1945–9. doi: 10.1007/s00464-007-9575-3
12. de Toledo AP, Rodrigues FH, Rodrigues MR, Sato DT, Nonose R, Nascimento EF, et al. Diospyrobezoar as a cause of small bowel obstruction. Case Rep Gastroenterol. (2012) 6:596–603. doi: 10.1159/000343161
13. Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D, et al. The CARE Guidelines: Consensus-based Clinical Case Reporting Guideline Development.
14. Eitan A, Katz IM, Sweed Y, Bickel A. Fecal impaction in children: report of 53 cases of rectal seed bezoars. J Pediatr Surg. (2007) 42(6):1114–7. doi: 10.1016/j.jpedsurg.2007.01.048
15. Eitan A, Bickel A, Katz IM. Fecal impaction in adults: report of 30 cases of seed bezoars in the rectum. Dis Colon Rectum. (2006) 49(11):1768–71. doi: 10.1007/s10350-006-0713-0
16. Mirza MS, Al-Wahibi K, Baloch S, Al-Qadhi H. Rectal bezoars due to pumpkin seeds. Trop Doct. (2009) 39(1):54–5. doi: 10.1258/td.2008.080107
17. Manne JR, Rangu VM, Motapothula UM, Hall MC. A crunching colon: rectal bezoar caused by pumpkin seed consumption. Clin Med Res. (2012) 10(2):75–7. doi: 10.3121/cmr.2011.1016
18. Eng K, Kay M. Gastrointestinal bezoars: history and current treatment paradigms. Gastroenterol Hepatol (N Y). (2012) 8(11):776–8. PMID: 24672418; PMCID: 3966178
19. Espinoza González R. Bezoares gastrointestinales: mitos y realidades [Gastrointestinal bezoars]. Rev Med Chil. (2016) 144(8):1073–7 [Spanish]. doi: 10.4067/S0034-98872016000800016
20. Berry J. Dilatation and rupture og the sigmoid flexure. Br Med J. (1894) 1:301. doi: 10.1136/bmj.1.1741.1050-a
21. Melchreit R, McGowan G, Hyams JS. “Colonic crunch” sign in sunflower-seed bezoar. N Engl J Med. (1984) 310(26):1748–9. doi: 10.1056/nejm198406283102620
22. Manatakis D, Sioula M, Passas I, Zerbinis H, Dervenis C. Rectal seed bezoar due to sunflower seed: a case report and review of the literature. Pan Afr Med J. (2018) 31:157. doi: 10.11604/pamj.2018.31.157.12539
23. Sanders MK. Bezoar: from mystical charms to medical and nutritional management. Pract Gastroenterol. (2004) 28:37–50. Corpus ID: 43195929
24. Steinberg JM, Eitan A. Prickly pear fruit bezoar presenting as rectal perforation in an elderly patient. Int J Colorectal Dis. (2003) 18(4):365–7. doi: 10.1007/s00384-003-0482-3
25. Ertuğrul G, Coşkun M, Sevinç M, Ertuğrul F, Toydemir T. Treatment of gastric phytobezoars with Coca-Cola given via oral route: a case report. Int J Gen Med. (2012) 5:157–61. doi: 10.2147/IJGM.S29453.
26. Ladas SD, Kamberoglou D, Karamanolis G, Vlachogiannakos J, Zouboulis-Vafiadis I. Systematic review: Coca-Cola can effectively dissolve gastric phytobezoars as a first-line treatment. Aliment Pharmacol Ther. (2013) 37(2):169–73. doi: 10.1111/apt.12141
27. Iwamuro M, Yunoki N, Tomoda J, Nakamura K, Okada H, Yamamoto K. Gastric bezoar treatment by endoscopic fragmentation in combination with Pepsi-Cola® administration. Am J Case Rep. (2015) 16:445–8. doi: 10.12659/AJCR.893786
28. Kement M, Ozlem N, Colak E, Kesmer S, Gezen C, Vural S. Synergistic effect of multiple predisposing risk factors on the development of bezoars. World J Gastroenterol. (2012) 18(9):960–4. doi: 10.3748/wjg.v18.i9.960
Keywords: pumpkin seeds, bezoar, occlusion, haematochezia, digital impaction, depression
Citation: Gentile M, Vergara L, Schiavone V, Cestaro G and Sivero L (2022) Harry Potter's Occlusion: Report of a Case of Pumpkin Seed Bezoar Rectal Impact. Front. Surg. 9:902701. doi: 10.3389/fsurg.2022.902701
Received: 23 March 2022; Accepted: 17 June 2022;
Published: 14 July 2022.
Edited by:
Gaetano Gallo, Sapienza University of Rome, ItalyReviewed by:
Dimitrios Balalis, Dimitrios Balalis, GreeceGiovanni Tomasicchio, Università degli Studi di Bari, Italy
Argyrios Ioannidis, Athens Medical Group, Greece
Copyright © 2022 Gentile, Vergara, Schiavone, Cestaro and Sivero. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maurizio Gentile bWFnZW50aWxAdW5pbmEuaXQ=
Specialty section: This article was submitted to Visceral Surgery, a section of the journal Frontiers in Surgery
 Maurizio Gentile
Maurizio Gentile Lorenzo Vergara1
Lorenzo Vergara1 Luigi Sivero
Luigi Sivero