- 1Institute of Hepatopancreatobiliary Surgery, Chongqing General Hospital, Chongqing, China
- 2Department of Ultrasonography, Chongqing General Hospital, Chongqing, China
Hereditary haemorrhagic telangiectasia (HHT) is a rare disease that lacks effective treatment. Here, the authors report the case of a 30-year-old woman presenting with abdominal pain accompanied by severe malnutrition. After a definite diagnosis of HHT involvement in the liver, liver transplantation was the first-choice treatment according to the guidelines of HHT. However, the patient firmly refused liver transplantation. Finally, a new type of surgery, right hemihepatectomy combined with ligation of the common hepatic artery and gastroduodenal artery, was performed based on careful study of the case and with the maximum benefit of the patient in mind. Although the patient developed transient liver dysfunction after surgery, she eventually recovered well and continued to be followed up. As far as we know, this is the first report of this kind of surgery for the treatment of intrahepatic HHT.
Introduction
Hereditary haemorrhagic telangiectasia (HHT) is a rare autosomal dominant disorder characterized by arteriovenous malformations (AVMs) of the internal organs and mucocutaneous telangiectasias (1). The estimated prevalence is 1/5,000–1/8,000 people (2). The liver is the most common visceral organ susceptible to HHT, but such cases are usually asymptomatic. More than half of patients with HHT have hepatic vascular malformations (VMs), but only 8% show symptoms (3). Although asymptomatic liver VMs do not require treatment, symptomatic liver VMs must be treated aggressively since they increase mortality. However, the treatment for liver VMs is limited to anti-angiogenesis, arterial embolization, and ligation and banding of the hepatic artery. Liver transplantation is an effective treatment option, whereas long-term immunosuppressive therapy remains a trade-off of this choice, especially for younger patients. Therefore, more effective treatments for liver VMs should be explored. Here, we report a 30-year-old woman who had HHT with hepatic AVMs and underwent right hemihepatectomy combined with ligation of the common hepatic artery and gastroduodenal artery because of her disease characteristics. Although long-term outcomes require further follow-up, the successful recovery and discharge of the patient demonstrate the feasibility of this procedure for the treatment of partial HHT with hepatic AVMs.
Case description
A 30-year-old woman was admitted to our hospital with abdominal pain and weight loss. The patient had a history of recurrent epistaxis during pregnancy. The patient had no family history of HHT. Physical examination showed tenderness in the upper abdomen. Laboratory results on admission showed moderate anaemia, abnormal liver function and severe malnutrition. Abdominal ultrasonography showed disorder of the intrahepatic duct structure. Magnetic resonance imaging (MRI) showed that intrahepatic bile duct stones were concentrated in the right hemi-liver (Figure 1A). Moreover, hepatic arteriovenous malformations (AVMs) accompanied by bile duct necrosis were identified by computed tomography (CT) (Figure 1B). Finally, three-dimensional reconstruction vividly showed the dilatation of the intrahepatic bile ducts, bile duct calculi, and extensive telangiectasia (Figures 1C, D). Fortunately, cerebral angiography, thoracic and abdominal angiography, gastroscopy, colonoscopy, echocardiography and cardiac biomarker examination showed no obvious abnormalities. According to the Curaçao diagnostic criteria for HHT (4) (Supplementary Table S1), she was diagnosed with HHT with hepatic AVM.
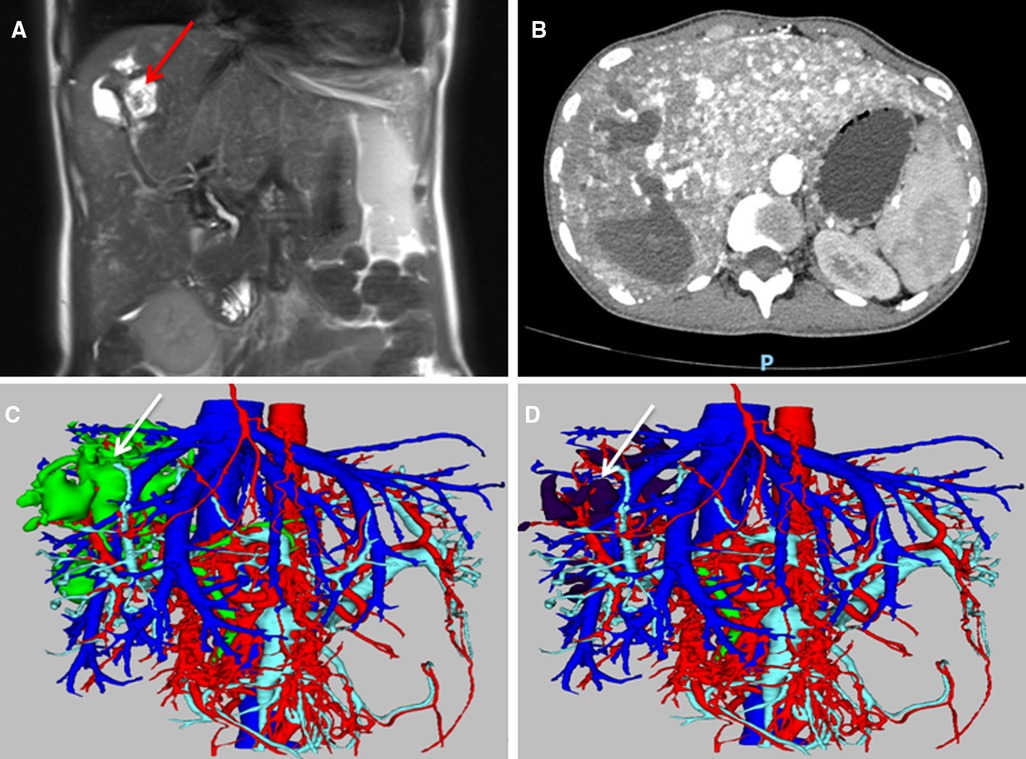
Figure 1. Imaging of HHT involvement in the liver. (A) The MRI results suggested right hepatobiliary dilatation with stone formation (arrow); (B) The arterial phase of CT indicated diffuse telangiectasia and shunting in the liver; (C) Three-dimensional reconstruction showed hepatic telangiectasia and bile duct dilatation (arrow); (D) Three-dimensional reconstruction showed telangiectasia and intrahepatic bile duct stones (arrow).
After diagnosis, the treatment was discussed by a multidisciplinary team, and liver transplantation was deemed one of the best treatment options for this patient according to international guidelines (5). The patient refused liver transplantation, so alternative treatments had to be considered to relieve her abdominal pain symptoms and control her biliary tract infection. Based on the characteristics of the patient, although hepatic AVMs were widespread throughout the liver, the major lesions (bile duct stones and biliary tract infection) were localized to the right hemi-liver. Finally, right hemihepatectomy combined with ligation of the common hepatic artery and gastroduodenal artery was planned. Since ligation of the common hepatic artery and gastroduodenal artery may effectively alleviate the hepatic arteriovenous shunt (6, 7), a right hemihepatectomy was expected to eradicate the bile duct stones and the infected lesion. To achieve optimal treatment outcomes, the patient spent two months on preoperative preparation, which included improving her nutritional status, gaining weight, getting cardiorespiratory exercise, etc.
On intraoperative exploration, the erythema caused by telangiectasia was diffuse throughout the liver, which was consistent with the imaging findings (Figure 2A). Despite careful preoperative preparation, the operation was still very risky. Therefore, several measures were taken to reduce surgical complications:1, portal pressure was monitored to ensure that the portal pressure was reduced while normal perfusion was maintained (Figure 2B); 2, the blood flow velocities of the hepatic artery, portal vein and hepatic vein were monitored by ultrasound to ensure nearly normal blood flow signal after ligation (Figures 2C,D; Supplementary Table S2); and 3, since all indicators met our expectations, right hemihepatectomy was performed as the last step (Figures 2E,F). In the end, the surgery was successful. As expected, even with her extensive preoperative preparation, there was a period of liver insufficiency after surgery (Figure 3). Importantly, the patient recovered thanks to aggressive supportive treatment. The patient has been followed up regularly (every 6 months, including enhanced upper abdominal CT and liver function), and the treatment effect was satisfactory (pain disappeared, liver function returned, weight increased, liver volume was partially compensated for, and hepatic AVMs were relieved) (Figure 4).
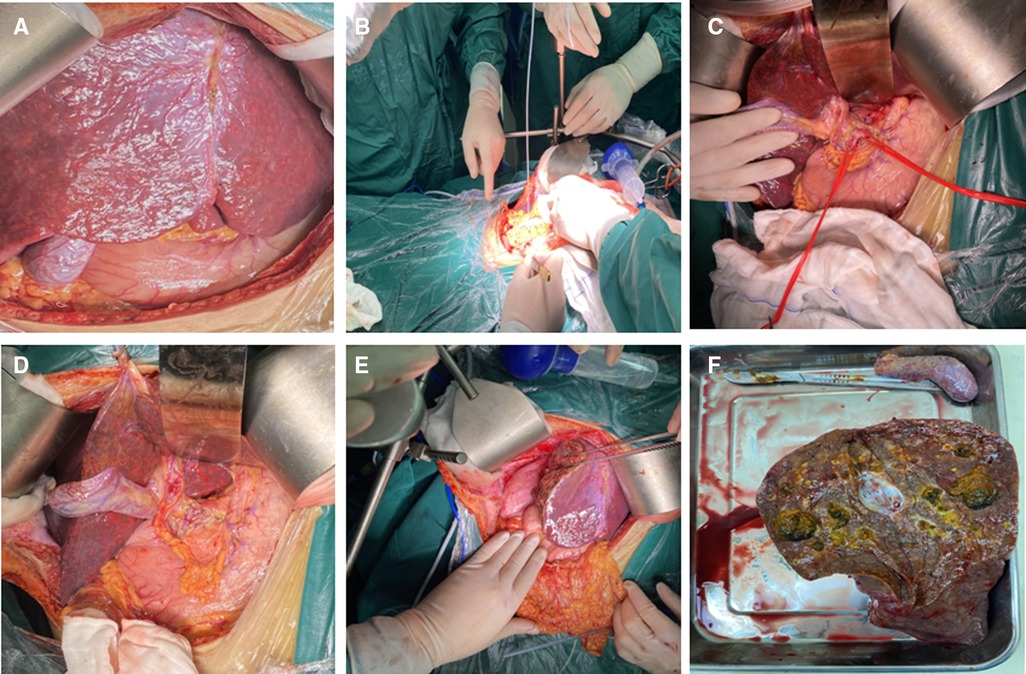
Figure 2. The operative procedure and key intraoperative pictures. (A) Surgical exploration revealed extensive telangiectasia in the liver; (B) Portal venous pressure measurement prior to the surgery; (C) The common hepatic artery and gastroduodenal artery were suspended and pre-occluded; (D), The common hepatic artery and gastroduodenal artery were ligated; (E) Right hemihepatectomy was performed successfully; (F) Right liver specimen and intrahepatic bile duct dilatation with stone formation.
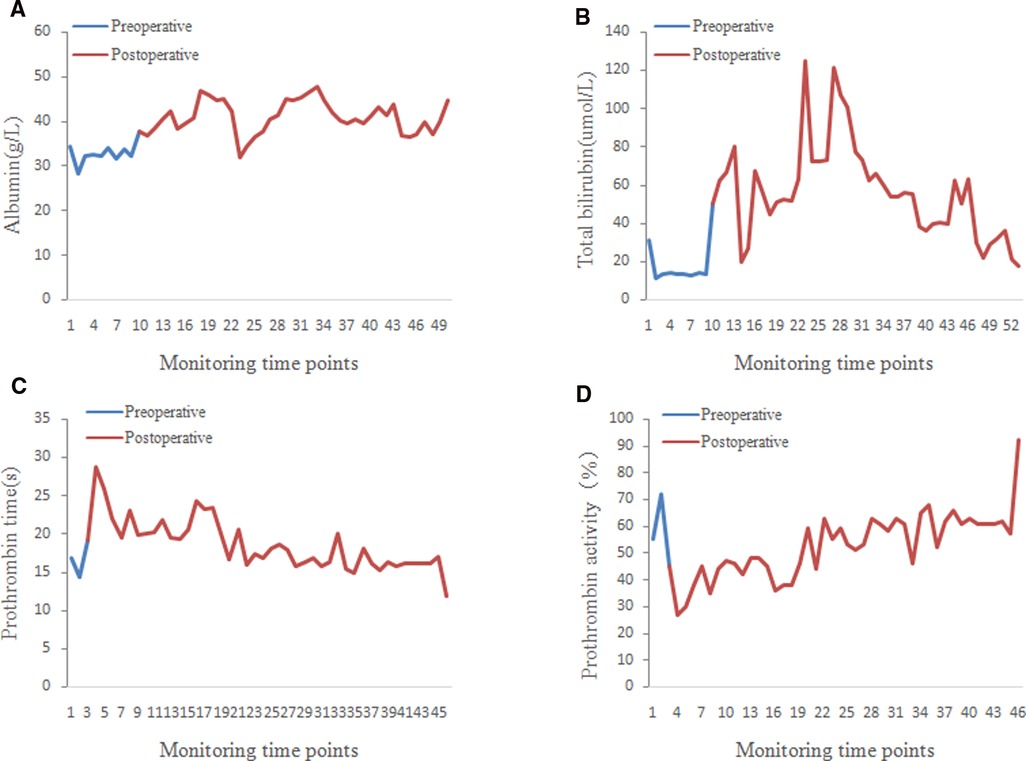
Figure 3. Curve of postoperative liver function-related indexes. Postoperative changes in albumin (A) total bilirubin (B) prothrombin time (C) and prothrombin activity (D).
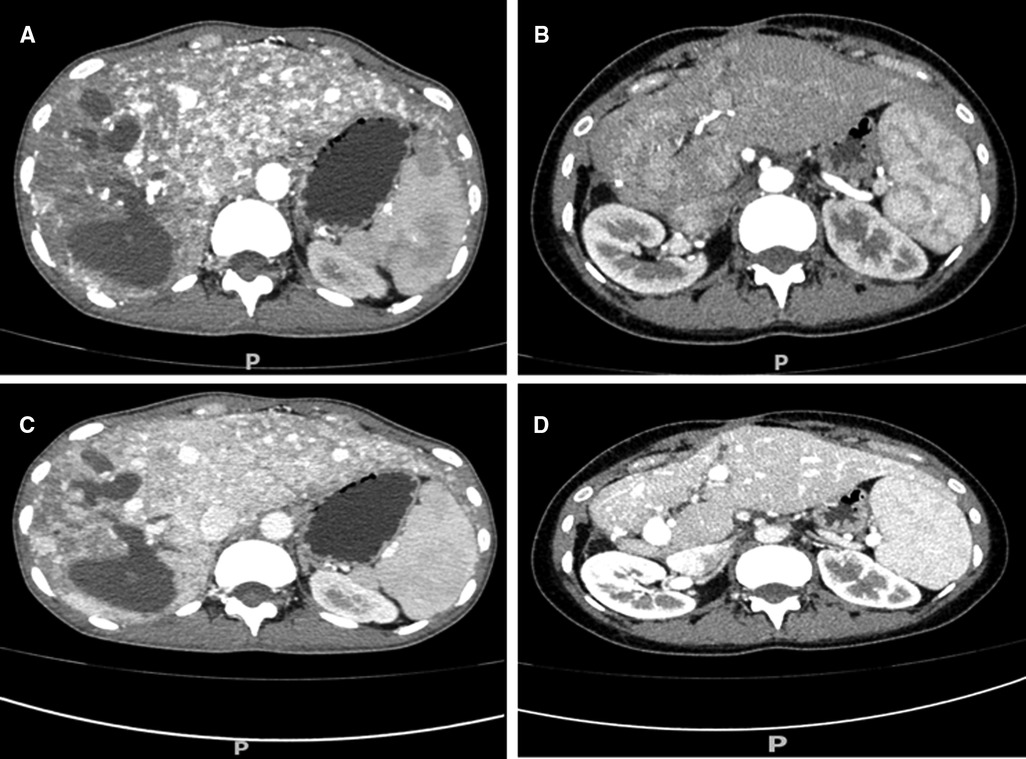
Figure 4. CT image comparison of the hepatic arteriovenous shunt before and after operation. CT arterial phase showed a significant decrease in telangiectasia and the shunt (A, preoperative; B, postoperative). Enhanced CT in the portal phase also showed a significant decrease in the shunt (C, preoperative; D, postoperative).
Discussion
HHT is a rare autosomal dominant disease characterized by organ telangiectasia. The liver is the most commonly affected organ (hepatic AVMs) (8); however, the treatment options are limited and unsatisfactory. Although the vast majority of liver VMs are asymptomatic and do not require treatment, symptomatic liver VMs must be treated aggressively since they increase mortality (9). Intravenous bevacizumab helps relieve symptoms and has been used as a bridge to orthotopic liver transplant (OLT) (10). Given that hepatic artery embolization is associated with mortality, it is only recommended in late-stage high-output cardiac failure (HOCF), only when medical therapies fail, and only when OLT is not an option (5). Moreover, embolization is contraindicated in patients with cholangitis or bile duct necrosis (11). Hepatic artery ligation or banding is considered to be effective in the treatment of HOCF and hepatic arteriovenous shunt in certain patients (6, 7, 12). However, it would not have been enough to cure the disease of this patient, who had bile duct stones and cholangitis in the right hemi-liver. Liver transplantation is considered to be the most effective treatment for hepatic AVMs, but this comes along with life-long immunosuppressive treatment to reduce the risk of organ rejection (13).
This young patient had HHT with liver involvement accompanied by bile duct stones and cholangitis. She refused liver transplantation. Fortunately, in addition to the diffuseness of her hepatic AVMs, her biliary tract lesions were localized to the right hemi-liver. Therefore, we designed right hemihepatectomy combined with ligation of the common hepatic artery and gastroduodenal artery based on the individual characteristics of this patient. Lesion resection for arteriovenous malformations has been previously reported, but right hemihepatectomy combined with artery ligation for the treatment of HHT has not. Georghiou et al. successfully cured pulmonary arteriovenous malformation by lobectomy (14). A recent report suggested that partial liver resection is also an option for large intrahepatic shunts that do not close spontaneously (15). Petrovic et al. reported a successful left lateral bisegmentectomy in a HHT patient with liver abscess (16). These reports provided a rationale for hepatectomy, as long as the patient's residual liver is sufficient. We also performed ligation of the common hepatic artery to alleviate the AVMs, while ligation of the gastroduodenal artery helped to avoid collateral circulation. It is important to emphasize that we deliberately kept the hepatic artery and portal vein pressure slightly higher than normal during the operation to maintain hepatic blood perfusion. As expected, although the patient developed transient liver dysfunction after surgery, she was discharged from the hospital in good health.
In the face of such a rare disease as HHT, available treatment options are limited, and their effect is unsatisfactory. However, for some special cases, we may still be able to design a relatively good individualized treatment other than the traditional treatment and protect the best interests of the patient. The successful treatment of this patient indicates that ligation of the common hepatic artery and gastroduodenal artery combined with hepatectomy is suitable for some HHT patients with localized intrahepatic lesions. This patient's success further broadens the treatment options for HHT.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
Drafting of the manuscript: JX; Perform the operation and patient management: WX; Intraoperative color ultrasound examination: CZ; Surgical design, surgical implementation and overall management: HW. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.900297/full#supplementary-material.
References
1. Elawad O, Albashir AAD, Mirghani Ahmed MM, Elawad A, Mohamed OEE. Hereditary Hemorrhagic Telangiectasia in a Sudanese Patient. Case Rep Med. (2020) 2020:6395629. doi: 10.1155/2020/6395629
2. Grosse SD, Boulet SL, Grant AM, Hulihan MM, Faughnan ME. The use of US health insurance data for surveillance of rare disorders: hereditary hemorrhagic telangiectasia. Genet Med. (2014) 16:33–9. doi: 10.1038/gim.2013.66
3. Siddiki H, Doherty MG, Fletcher JG, Stanson AW, Vrtiska TJ, Hough DM, et al. Abdominal findings in hereditary hemorrhagic telangiectasia: pictorial essay on 2D and 3D findings with isotropic multiphase CT. Radiographics. (2008) 28:171–84. doi: 10.1148/rg.281075037
4. Shovlin CL, Guttmacher AE, Buscarini E, Faughnan ME, Hyland RH, Westermann CJ, et al. Diagnostic criteria for hereditary hemorrhagic telangiectasia (Rendu-Osler-Weber syndrome). Am J Med Genet. (2000) 91:66–67. doi: 10.1002/(SICI)1096-8628(20000306)91:1<66::AID-AJMG12>3.0.CO;2-P
5. Faughnan ME, Mager JJ, Hetts SW, Palda VA, Lang-Robertson K, Buscarini E, et al. Second international guidelines for the diagnosis and management of hereditary hemorrhagic telangiectasia. Ann Intern Med. (2020) 173:989–1001. doi: 10.7326/M20-1443
6. Koscielny A, Willinek WA, Hirner A, Wolff M. Treatment of high output cardiac failure by flow-adapted hepatic artery banding (FHAB) in patients with hereditary hemorrhagic telangiectasia. J Gastrointest Surg. (2008) 12:872–6. doi: 10.1007/s11605-007-0411-9
7. Song X, Chen HQ, Chen YX, Cheng Y, Qu CQ, Liu EY, et al. Individualized management of hepatic diseases in hereditary hemorrhagic telangiectasia. Am Surg. (2011) 77:281–5. doi: 10.1177/000313481107700314
8. Dunphy L, Talwar A, Patel N, Evans A. Hereditary haemorrhagic telangiectasia and pulmonary arteriovenous malformations. BMJ Case Rep. (2021) 14(1):e238385. doi: 10.1136/bcr-2020-238385
9. Thompson KP, Nelson J, Kim H, Pawlikowska L, Marchuk DA, Lawton MT, et al. Predictors of mortality in patients with hereditary hemorrhagic telangiectasia. Orphanet J Rare Dis. (2021) 16:12. doi: 10.1186/s13023-020-01579-2
10. Harwin J, Sugi MD, Hetts SW, Conrad MB, Ohliger MA. The role of liver imaging in hereditary hemorrhagic telangiectasia. J Clin Med. (2020) 9:3750. doi: 10.3390/jcm9113750
11. EASL Clinical Practice Guidelines. Vascular diseases of the liver. J Hepatol. (2016) 64:179–202. doi: 10.1016/j.jhep.2015.07.040
12. Neumann UP, Knoop M, Langrehr JM, Keck H, Bechstein WO, Lobeck H, et al. Effective therapy for hepatic M. Osler with systemic hypercirculation by ligation of the hepatic artery and subsequent liver transplantation. Transpl Int. (1998) 11:323–6. doi: 10.1007/s001470050152
13. Enderby C, Keller CA. An overview of immunosuppression in solid organ transplantation. Am J Manag Care. (2015) 21:s12–23.25734416
14. Georghiou GP, Berman M, Vidne BA, Saute M. Pulmonary arteriovenous malformation treated by lobectomy. Eur J Cardiothorac Surg. (2003) 24:328–30. doi: 10.1016/S1010-7940(03)00249-5
15. Schmalz MJ, Radhakrishnan K. Vascular anomalies associated with hepatic shunting. World J Gastroenterol. (2020) 26:6582–98. doi: 10.3748/wjg.v26.i42.6582
Keywords: hereditary haemorrhagic telangiectasia, right hemihepatectomy, common hepatic artery, gastroduodenal artery, ligation
Citation: Xiang J, Xie W, Zhang C and Wang H (2022) Right hemihepatectomy combined with ligation of the common hepatic artery and gastroduodenal artery for the treatment of intrahepatic HHT: A case report. Front. Surg. 9:900297. doi: 10.3389/fsurg.2022.900297
Received: 20 March 2022; Accepted: 26 July 2022;
Published: 9 August 2022.
Edited by:
Marco Materazzo, Policlinico Tor Vergata, ItalyReviewed by:
Francisco Hernández, University Hospital La Paz, SpainIvan Romic, University Hospital Centre Zagreb, Croatia
© 2022 Xiang, Xie, Zhang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huaizhi Wang d2h1YWl6aGlAZ21haWwuY29t
Specialty Section: This article was submitted to Visceral Surgery, a section of the journal Frontiers in Surgery
 Jifeng Xiang
Jifeng Xiang Wei Xie1
Wei Xie1