- Department of Breast and Thyroid Surgery, Renmin Hospital of Wuhan University, Wuhan, China
Background: Energy-based devices (EBD) have been popularized in thyroidectomy worldwide. Microdissection tungsten needle (MDTN) is characterized by the ultra-sharp tip providing safe and meticulous dissection with effective hemostasis. However, little study has applied MDTN in thyroidectomy.
Methods: This retrospective study compared clinical data of the patients who underwent total thyroidectomy (TT) with central neck dissection (CND) using MDTN, harmonic scalpel (HS), and conventional electrocautery (CE). We assessed outcomes related to surgical efficacy and safety. The injury degree of tissue was assessed by biochemical indicators and early-stage inflammatory factors in the drainage fluid. Histological sections of the thyroid specimens were evaluated to compare levels of thermal damage by the three EBD.
Results: There was a significant decrease in the intraoperative blood loss, operation time and 24-hour drainage volume in the MDTN group compared to the CE group. The total drainage volume, duration of drainage, and average length of stay of the MDTN group were less compared to the CE group though they did not reach statistical significance. No disparity was observed between the MDTN group and HS group in these variables. Total costs were not significantly different among these groups. The incidence of recurrent laryngeal nerve (RLN) injury was the lowest using MDTN compared to the CE (P = 0.034) and HS (not significant). No statistical differences were observed among these groups regarding postoperative wound pain and infection, hypoparathyroidism, and postoperative hemorrhage. Analysis of biochemical indicators showed a lower level of hemoglobin in the MDTN and HS group than the CE group (P = 0.046 and 0.038, respectively) and less triglyceride in the HS group than the MDTN and CE group (P = 0.002 and 0.029, respectively) but no significant difference in cholesterol level in these groups. Early-stage inflammatory factors including TNF-α and IL-6 showed significantly higher concentration in the CE group than the MDTN and HS group. Histological sections of thyroid specimens revealed that MDTN caused the lowest degree of thermal damage followed by HS then CE.
Conclusion: MDTN exhibited comparable surgical efficacy and safety outcomes as HS in thyroidectomy. Therefore, MDTN is a safe and viable alternative for hemostasis in thyroidectomy.
Introduction
Thyroid carcinoma is the most common head and neck tumor with an increasing global incidence in recent years (1), and papillary thyroid carcinoma (PTC) remains the most common histological subtype of the new diagnoses (2). Total thyroidectomy (TT) is the time-tested primary treatment modality of PTC (3).
Thyroidectomy was originated in the 19th century. As the thyroid gland is richly vascularized and adjacent to several important anatomical structures, thyroidectomy was a particularly risky surgery with a complication rate up to 50% and a mortality rate up to 20% in that period (4). It was not until the late 20th century that the surgical complication rate decreased to merely 1% with the popularization of suture and ligation techniques and then the invention of energy-based devices (EBD) for hemostasis. Additionally, with the accumulation of surgical experience, surgeons with high volume can further reduce the complication rate (2, 5–7).
Though the traditional suture and ligation method helps to achieve the purpose of careful hemostasis, it is time-consuming and excessive ligation to the adjacent tissue may cause incidental injury to the nerves and parathyroid glands. Conventional electrocautery (CE) has a relatively large and blunt tip which may increase the operating power output, causing more severe tissue damage and more diffusion of lateral heat (8). Currently, the harmonic scalpel (HS) has been applied for hemostasis and dissection in thyroid surgery as its excellent surgical efficacy has been well-documented (9–16), but it increases the medical costs to a certain extent in our country. The major mechanism of HS is breaking the tertiary structure hydrogen bonds of protein in tissue by emitting mechanical vibration with a frequency of 55.5 kHz (17). Although the majority of researchers have been prone to recommend HS for hemostasis in thyroid surgery, there is no solid evidence to decide which is the best hemostatic modality overall, while certain research aroused concerns about the safety of utilizing HS in thyroid surgery (10, 18, 19). Therefore, more investigation and further development of EBD are still warranted.
Microdissection tungsten needle (MDTN) is a surgical device featured with its ultra-sharp needle using tungsten alloy with a tip radius of curvature less than 10 microns. Based on the mechanism of high-frequency electrocautery, it combines the advantages of scalpel and electrosurgery with lower wattage input and more concentrated thermal delivery to reduce thermal injury compared with CE. It provides meticulous dissection comparable to scalpel while reducing the risk of surgical complication development, contributing to the postoperative recovery of patients. Furthermore, it is more cost-efficient compared to HS, thus it has a wide application prospect in surgery. MDTN has been applied in several fields of surgery with good performance, especially orthopedic and otorhinolaryngologic surgery (20–26). However, little research has been conducted on the application of MDTN in thyroid surgery. This research aimed to compare the surgical efficacy and safety of MDTN with HS and CE for the first time in patients who underwent TT with central neck dissection (CND) for PTC. Additionally, the traumatic degree of soft tissue caused by these devices was investigated. We present the following article in accordance with the STROBE reporting checklist.
Materials and methods
Study design
A retrospective study was conducted on clinical records of patients who were diagnosed with PTC and underwent TT with bilateral CND in our department from March 2018 to June 2019. The exclusion criteria included: (I) patients undergoing unilateral thyroidectomy; (II) patients without bilateral CND operation; (III) history of chronic diseases of vital organs; (IV) history of hematological diseases; (V) patients undergoing lateral neck dissection; (VI) history of preoperative hyperthyroidism; (VII) history of anticoagulant agent use; (VIII) history of thyroid surgery; (IX) patients with follow-up less than 6 months or withdraw. Patients involved were divided into MDTN (BT-500V, BROVET®, China), HS (GEN300, Johnson & Johnson), and CE (SM-ZXDJ-A61, SM company, China) groups according to the use of EBD modality in surgery. The electrosurgical generator of MDTN and CE was Force FX of COVIDEN company and the generator of HS was Ethicon Endo-Surgery from Johnson & Johnson company. MDTN and CE were generally applied by the CUT mode and the output power were 15 and 30 w, respectively. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). All patients signed informed consent. The study protocol was approved by the Ethics Committee of Renmin Hospital of Wuhan University (item ID: ADRY2021-K032).
Surgical procedures
All the patients included in the study underwent TT with bilateral CND under the standard surgical procedure similar to the description by Ramouz et al. (27). CND was performed after TT. During surgery, MDTN, HS, or CE was utilized as the major modality for hemostasis and dissection. Note that if the hemostatic effect was insufficient, ligation and suture were applied. A drainage tube was routinely placed before closure. The dissected specimens of the thyroid were routinely sent for pathological diagnosis after surgery. The H&E staining slices of the thyroid specimens were collected to determine the degree of tissue damage by the three EBD. Analysis of histological changes of the thyroid margin was conducted by a pathologist who was blinded to the EBD usage corresponding to the specimens.
Clinical data
Demographic characteristics including age, sex, BMI (body mass index), history of hypertension, and diabetes mellitus were recorded accordingly. The number of intraoperative dissected lymph nodes and metastatic lymph nodes (histologically confirmed after surgery) was also recorded.
The surgical efficacy indicators included: intraoperative blood loss volume, operation time, 24-hour drainage and total drainage volume, duration of postoperative drainage, average length of hospital stay, and total medical costs. Intraoperative blood loss was defined as the volume of fluid in the negative pressure suction device. The operation time was defined as the time between skin incision and complete closure. The indication of drainage tube removal was 24-hour drainage volume less than 30 ml. Drainage volume was recorded 24 h after surgery and by the time of drainage tube removal.
The safety assessment consisted of two parts: general complications including surgical wound pain and infection, and complications specific to thyroid surgery including recurrent laryngeal nerve (RLN) injury, postoperative hypoparathyroidism, and postoperative hemorrhage. Surgical wound pain level was assessed 24 h after surgery by visual analog scale (VAS) from 0 to 10 (0 for no pain; 1–3 for mild pain; 4–6 for moderate pain; 7–10 for severe pain). For each group, the number of patients reporting moderate or severe pain was documented accordingly. Surgical wound infection was defined as the local symptoms including erythema, swelling, warmth, pain, and purulent secretion in the wound. RLN injury was defined as postoperative hoarseness or vocal cord paralysis revealed by laryngoscopy. Postoperative hypoparathyroidism was defined as either PTH level lower than the normal range (18.5–88 pg/ml in our hospital) or hypocalcemia after surgery along with the symptom of numbness or cramping in hands and feet. Postoperative hemorrhage was defined as surgical wound swelling with symptoms of tracheal compression such as suffocation.
Since March 2019, the drainage fluid of 37 consecutive patients involved (13 from MDTN group, 16 from HS group, 8 from CE group) were collected by the day of drainage tube removal and sent for laboratory examination, including biochemical tests (hemoglobin, cholesterol, and triglyceride) and early-stage inflammatory factors (TNF-α and IL-6).
Statistical analysis
Statistical analysis was performed by SPSS 22.0 software (SPSS Inc., Chicago, IL, USA). Pearson chi-square test or Fisher’s exact test were conducted for categorical variables. Continuous variables were checked for distribution type using histogram and Shapiroe-Wilk test. Continuous variables conformed to the normal distribution were compared by the one-way ANOVA test and expressed as mean ± SD, while those did not conform to the normal distribution were compared by the Kruskal-Wallis ANOVA test and expressed as the median and first-third quartile. The post-hoc pairwise comparison was conducted when the difference was significant. Post-hoc pairwise comparisons were adjusted using a Bonferroni correction. P < 0.05 was considered statistically significant. Note that in this paper, P represented the comparison of the three groups, and P1, P2, P3 respectively represented the results of statistical comparison of MDTN group versus HS group, HS group versus CE group, MDTN group versus CE group.
Results
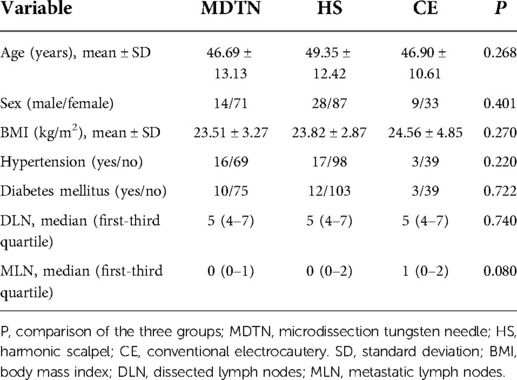
Baseline characteristics
A total of 242 patients were involved in this study, including 85 in the MDTN group, 115 in the HS group, and 42 in the CE group. The baseline characteristics showed no significant differences between the three groups (Table 1). Therefore, the three groups are considered comparable.
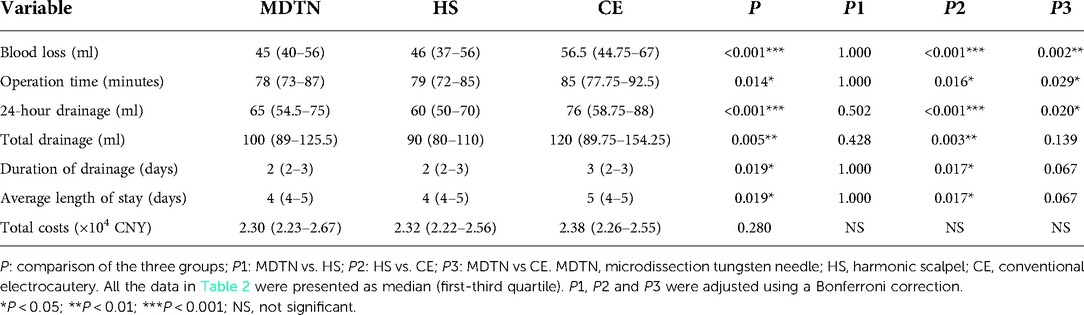
Surgical efficacy assessment
The comparison of surgical effects of the three groups was demonstrated in Table 2. The intraoperative blood loss volume of the MDTN and HS group was significantly less than the CE group (P2 < 0.001, P3 = 0.002). The operation time of the MDTN and HS group was significantly shorter than the CE group (P2 = 0.061, P3 = 0.029). Consistently, compared to the CE group, MDTN and HS group had less 24-hour drainage volume (P2 < 0.001, P3 = 0.020), less total drainage volume (P2 = 0.003, P3 not significant), shorter duration of postoperative drainage (P2 = 0.017, P3 not significant), and shorter average length of hospital stay (P2 = 0.017, P3 not significant). There was no significant difference in the indicators above between the MDTN group and the HS group. The total medical costs of the three groups were not statistically significant (P = 0.280).
Safety assessment
The comparison of safety assessments was demonstrated in Table 3. No case of RLN injury occurred in the MDTN group, which was significantly less than that of the CE group (P3 = 0.034). While the incidences of RLN injury were 0.87% and 7.14% in the HS group and CE group, respectively. No significant difference was shown regarding other complications including surgical wound pain, wound infection, hypoparathyroidism, and postoperative hemorrhage. Both MDTN group and CE group had one case of postoperative hemorrhage, of which the case of MDTN group resulted from an accidental tumble during off-bed activity the day after surgery and was resolved by strengthened local compression, while the case of CE group developed symptoms of airway compression on the day after surgery and underwent an emergency operation for hematoma evacuation. There was no case of lymphatic leakage in all the patients.
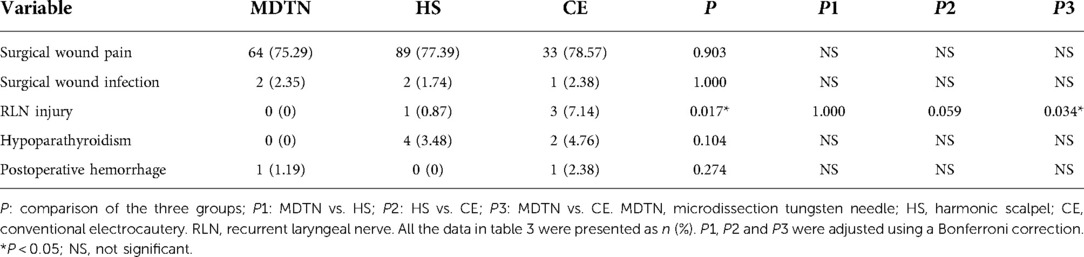
Laboratory examination of drainage fluid
Among all the patients involved, 37 cases (13 from the MDTN group, 16 from the HS group, 8 from the CE group) were analyzed with biochemical tests (Figure 1) and early-stage inflammatory factors (Figure 2) of the drainage fluid. It was indicated that hemoglobin was significantly lower in the MDTN and HS group compared to the CE group (P2 = 0.046, P3 = 0.038), and the content of triglyceride was significantly lower in the HS group compared to the MDTN and CE group (P1 = 0.002, P2 = 0.029). There was no significant difference among the three groups regarding the level of cholesterol. In terms of the early-stage inflammatory factors, levels of TNF-α and IL-6 in the drainage fluid were significantly higher in the CE group compared to the other two groups (P < 0.001).
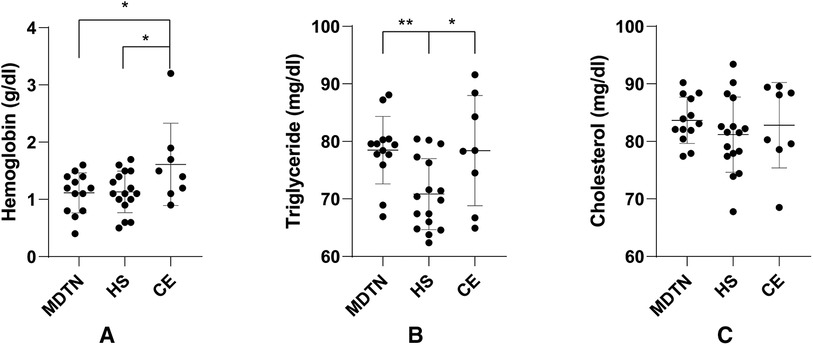
Figure 1. Comparison of biochemical indicators in the drainage fluid from the three groups. (A) Hemoglobin concentrations in the drainage fluid; (B) Triglyceride concentrations in the drainage fluid; (C) Cholesterol concentrations in the drainage fluid. *P < 0.05; **P < 0.01.
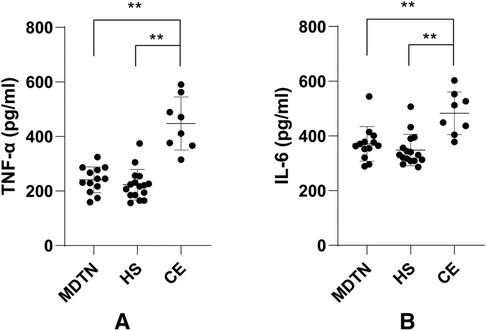
Figure 2. Comparison of early-stage inflammatory factors in the drainage fluid from the three groups. (A) TNF-α levels in the drainage fluid; (B) IL-6 levels in the drainage fluid. **P < 0.01.
Histological section of thyroid specimens
Figure 3 illustrated the H&E staining results of surgical margins of thyroid specimens from the three groups. It was observed that the thyroid margins in MDTN and HS group had a lower degree of thermal damage compared with the CE group. MDTN group (Figures 3A,B) exhibited the least degree of thermal damage because most of the glandular follicles remained structural integrity with continuous follicular epithelium surrounding the colloid, and the width of tissue necrosis was relatively narrower. In the HS group (Figures 3C,D) the follicular structures showed a higher level of damage by coagulative necrosis where more follicles were distorted and the colloid inside showed solid concentration with deeper staining color compared to the MDTN group, but parts of the structure remained relatively complete. In the CE group (Figures 3E,F) thyroid margin was seriously damaged as a wide range of nuclear pyknosis, fragmentation, and karyolysis were observed and tissue carbonization was the severest in all groups, with little intact follicular structure remaining.
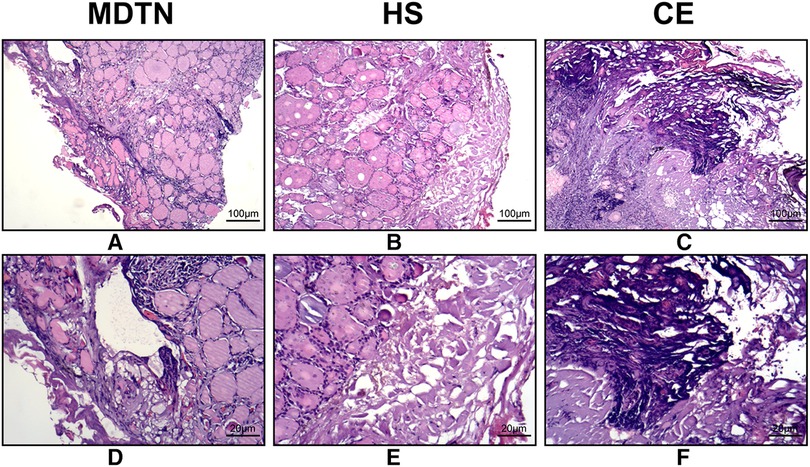
Figure 3. Histological sections (H&E staining) of the surgical margins of thyroid specimens from the three groups. The scale bars were included in the figures. (A,B) MDTN group; (C,D) HS group; (E,F) CE group.
Discussion
In recent decades, a series of EBD have been invented and employed in thyroid surgery to provide a less invasive manner of dissection and hemostasis (17). However, it remains controversial whether EBD performs better than traditional hemostatic methods in all aspects and how to choose among various EBD according to their profiles of efficacy and safety, which prompts the need for continued investigation of EBD.
MDTN is an energy-based device characterized by the ultra-sharp tip that combines the advantages of scalpel and electrocautery while providing effective hemostasis (Figure 4A). However, little research has utilized MDTN in thyroid surgery. Therefore, we conducted this research on the novel application of MDTN in patients who underwent TT with CND with histological diagnosis of PTC (Figure 4B). We assessed comprehensive outcomes including three major contents, which were surgical efficacy, safety outcomes, and trauma degree comparison. Overall, it was discovered that MDTN was comparable to HS, and both devices performed better than CE.
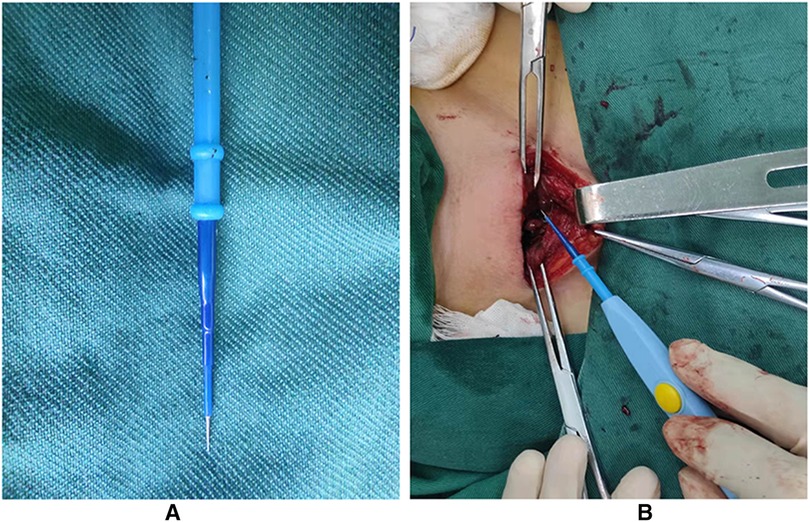
Figure 4. The application of MDTN in thyroidectomy. (A) The sharp tungsten tip of MDTN; (B) The operative view of thyroidectomy utilizing MDTN.
Concerning the surgical efficacy, our study found that MDTN and HS exhibited better profiles in intraoperative blood loss volume, operation time, 24-hour drainage and total drainage volume, days of postoperative drainage, average stay in hospital compared to CE. The analysis of total drainage volume, days of postoperative drainage and average stay in hospital showed that the difference between MDTN group and CE group did not reach statistical significance after adjusting the P value by Bonferroni correction, while the P values were statistically significant before correction. Bonferroni correction is one of the most commonly used methods for multiple hypothesis testing with the major purpose of controlling the probability of type I error. However, many researchers pointed that Bonferroni correction could be relatively conservative and may increase the type II error rate (28). Therefore, it is inappropriate that any scientific inference relies merely on the P value or the statistical significance without consideration of the clinical evidence provided by the data (28). In this case of research, there was an obvious decrease in these surgical variables by using MDTN comparing CE, and the data between HS group and MDTN group were relatively close comparing CE group. Therefore, it is reasonable to conclude that MDTN improved the surgical efficacy to a certain extent compared to CE, but research with larger samples is needed to verify this conclusion. Several prospective research (12–15) and meta-analyses (9, 11) concluded that HS had equally good or superior surgery outcomes compared to other hemostatic techniques and devices. Therefore, HS has been popularized in thyroid surgery worldwide. In this study, we observed a decrease in intraoperative blood loss volume and operation time by utilizing MDTN or HS compared to CE, which proved that MDTN not only achieved better hemostatic effect but can reduce the time for hemostasis and improve the surgical efficiency. In our opinion, it was majorly attributed to the meticulous dissection provided by MDTN when separating the thyroid capsule. Besides, MDTN and HS similarly reduced the volume and duration of postoperative drainage, indicating that MDTN can lessen the damage to soft tissue and lymphatic system in the operation area, thus facilitating the recovery progress and shortening the length of stay of patients. Some research pointed out that the application of EBD increased the costs of treatment (29, 30). Herein we found that there was no significant difference among three groups regarding total in-hospital costs. Further economic efficiency analysis is needed to compare these EBD.
In the safety assessment part, we stated that MDTN did not increase the risk of postoperative complications compared to HS and CE, and even exhibited a better profile in RLN protection. There was no case of RLN injury in the MDTN group while the rates were 0.87% and 7.14% in the HS group and CE group, respectively, but all recovered within three months after surgery. Since EBD can cause injury to RLN due to their thermal effect, numerous researches have been dedicated to exploring the thermophysical properties and safety capability of various EBD to establish standardized guidance for scrupulous and safe utilization of EBD (31). Most of the related studies showed that HS can achieve a good hemostatic effect without increasing the incidence of injury to adjacent nerves (9, 11, 15). One preclinical study stated that HS was safer than CE as it caused less damage to thyroid tissue and RLN in a canine model (8). Our findings showed that MDTN may cause less thermal injury to RLN with no case of RLN paralysis reported. It was probably attributed to the sharp needle tip of MDTN that required less energy and wattage input to accomplish fine dissection, which may reduce lateral thermal energy diffused to RLN and other structures. However, this hypothesis should be testified by a series of preclinical studies and prospective clinical trials.
The main causes of parathyroid gland injury are incidental removal of the gland and damage to the blood supply. In this study, there was no case of postoperative hypoparathyroidism in the MDTN group while four were in the HS group (3.48%) and two were in the CE group (4.76%), of which one patient in the HS group did not recover by six-month follow-up after surgery. The decreased rate of hypoparathyroidism by using MDTN may be attributed to some reasons. First, the sharp and thin tip of MDTN enabled the operator to dissect the thyroid gland while circumventing the parathyroids and their vascular supply. Second, MDTN may reduce lateral thermal damage to the parathyroid gland because the sharp tip of MDTN delivered energy in a more concentrated manner during cauterization. Although these differences failed to attain statistical significance (P1 = 0.138, P3 = 0.108), such disparity may be more obvious with a larger volume of participants. According to the previous research, the rate of postoperative transient hypoparathyroidism was reported about 19%–38% (32). The discrepancy between the results in our study and the previous research could be ascribed to the following clinical factors. First, all the patients who underwent total thyroidectomy in our department are routinely prescribed the oral calcium supplements after surgery, which effectively reduced the incidence of transient postoperative hypocalcemia and the related symptoms. Second, in our department, a series of techniques such as carbon nanoparticle suspension negative imaging (19), indocyanine green (ICG) fluorescence imaging (33), and parathyroid hormone test strip (34) are utilized for the identification and protection of the parathyroid gland. Based on this experience in our department, a decrease in postoperative hypoparathyroidism rate was observed in the patients.
According to previous research, the application of EBD was associated with decreased risk of developing postoperative neck hematoma (35, 36). As we know, neck hematoma is a dangerous but rare surgical complication in thyroid surgery, which is difficult to be evaluated in a small-volume prospective or retrospective study. Herein, only one patient in the CE group developed neck hematoma and received emergency hemostasis, while the patient in the MDTN group who developed postoperative hemorrhage resulted from an accidental tumble and was resolved by local compression. Therefore, the discrepancy in the risk of neck hematoma between the three groups did not reach statistical significance and a larger investigation was still warranted.
The general complications including postoperative pain and wound infection showed no statistical disparity in these groups. Among all the patients included, 75.29% of the MDTN group, 77.39% of the HS group and 78.57% of the CE group reported a moderate or higher level of pain and were prescribed intravenous administration of analgesics. Accordingly, 2.35%, 1.74%, 2.38% of the three groups above had wound infection but all recovered after prescription of antibiotics.
In terms of laboratory examination of 37 samples of drainage fluid, we found that hemoglobin levels in MDTN and HS group significantly decreased compared to CE group, which was in accordance with the result of blood loss volume, indicating that MDTN could achieve comparable hemostatic efficiency as HS to reduce postoperative exudation. It was noticed that triglyceride level was significantly less in the HS group than that in MDTN and CE group. We conjectured that such phenomenon may provide a limited clue that HS performed better regarding lymphoid tissue closure during neck dissection since triglyceride is one of the major components of lymph. However, given the limited volume of our examination, such a hypothesis requires a larger test to elucidate the physiological basis of drainage reduction with HS application.
To further compare the damage degree of tissue caused by these EBD, we tested the drainage fluids of 37 patients for TNF-α and IL-6 levels. It is well-known that TNF-α and IL-6 are classic proinflammatory cytokines functioning in many biological processes such as inflammation, infection, and wound healing (37). Surgical trauma stimulates macrophages and monocytes to activate and secrete TNF-α and IL-6 in the operated tissue, which can induce the cellular production of elastase and matrix metalloproteinase contributing to wound healing. Therefore, we supposed that examination of the drainage fluid from the surgical wound can potentially evaluate the tissue trauma (38). In this study, TNF-α and IL-6 levels were markedly lower in MDTN and HS group than in the CE group, indicating at the cellular level that MDTN and HS reduced the traumatic degree of tissue. However, considering the small number of samples included (37 samples in total), a larger sample size for investigation is warranted to confirm these findings.
Additionally, we performed H&E staining with several specimens of thyroid gland to gain an insight into the thermal damage to soft tissue caused by these EBD at a pathological level. Previous studies suggested that a more severe degree of mechanical and thermal destruction of the tissue would lead to the prevention of an appropriate pathological assessment (39, 40). Some researchers have previously proven MDTN caused very little tissue distortion during fine dissection of skin in a rat model (41). These studies are in accordance with our findings that MDTN reduced tissue necrosis and distortion in thyroid follicular structure, followed by HS with relatively more distorted follicle near the margin, while CE led to extensive carbonization and eschar formation. Thus, it can be concluded that MDTN best preserved the pathological integrity for thyroid cancer diagnosis. However, it should be clarified that only in the cases when the tumor invaded the thyroid capsule that different EBD may affect the diagnosis by pathologist.
Overall, MDTN has overcome the disadvantages of CE and illustrated equally good surgical efficacy and safety outcomes as HS in thyroidectomy. Additionally, MDTN provided a more integrated histological section of thyroid specimens for pathologists. Therefore, MDTN is an advantageous and applicable option for surgeons. However, given the fact that the experience of surgeons is in strong association with surgical outcomes (2), it should be highlighted that surgeons ought to choose appropriate hemostatic modalities according to their experience and awareness of device properties, and flexibly combined them when necessary to achieve optimal outcomes.
There were several limitations in our study. First, since it was a single-center retrospective study, the conclusions were limited in their feasibility compared to randomized controlled trials (RTC). Therefore, we have planned to conduct a prospective study in our center to further investigate the feasibility and safety of the MDTN application. Second, the number of patients enrolled was relatively small, and we will enlarge the scale in the next prospective study. Third, we limited the study object to PTC patients with TT with CND. On one hand, it was beneficial to reduce the influence of surgical methods and pathological types on the results. On the other hand, the application of MDTN in thyroid surgery treating other types of diseases such as benign thyroid goiter still needed investigation.
Conclusion
This is the first clinical study of applying MDTN in thyroidectomy. MDTN can provide meticulous dissection and effective hemostasis while reducing adverse thermal injury to soft tissue. In this study, MDTN exhibited comparable surgical efficacy and safety as HS. Therefore, MDTN is a novel and feasible hemostatic modality for thyroid surgery.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by The Ethics Committee of Renmin Hospital of Wuhan University. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article. The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study protocol was approved by the Ethics Committee of Renmin Hospital of Wuhan University (item ID: ADRY2021-K032) and individual consent for this retrospective analysis was waived.
Author contributions
WZ, SZ, SL, and SS contributed to the study conception and design. ZW and YZ searched prior articles and finished data analysis. WZ and SZ collected the clinical data. WZ and SZ wrote the first draft of the manuscript. SL and SS revised the manuscript. All authors read and approved the final manuscript. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors thank the hospital for providing the data, and all colleagues of the department of Breast and Thyroid Surgery at this institution for their daily clinical and research work.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. (2016):26. doi: 10.1089/thy.2015.0020
2. Wang TS, Sosa JA. Thyroid surgery for differentiated thyroid cancer - recent advances and future directions. Nat Rev Endocrinol. (2018) 14:670–83. doi: 10.1038/s41574-018-0080-7
3. Roman BR, Randolph GW, Kamani D. Conventional thyroidectomy in the treatment of primary thyroid cancer. Endocrinol Metab Clin N Am. (2019) 48:125–41. doi: 10.1016/j.ecl.2018.11.003
4. Or K, Benbassat C, Koren S, Shteinshneider M, Koren R, Cantrell D, et al. Adherence to ATA 2015 guidelines in the management of unifocal non-invasive papillary thyroid cancer: a clinical survey among endocrinologists and surgeons. Eur Arch Otorhinolaryngol. (2018) 275:2851–9. doi: 10.1007/s00405-018-5126-x
5. Ciftci F, Sakalli E, Abdurrahman I, Guler B. Parathyroid function following total thyroidectomy using energy devices. Eur Arch Otorhinolaryngol. (2016) 273:1905–11. doi: 10.1007/s00405-015-3704-8
6. Dionigi G, Chiang FY, Kim HY, Randolph GW, Mangano A, Chang PY, et al. Safety of LigaSure in recurrent laryngeal nerve dissection-porcine model using continuous monitoring. Laryngoscope. (2017) 127:1724–9. doi: 10.1002/lary.26271
7. Mao X-C, Chen C, Wang K-J. Efficacy and safety of LigaSure™ small jaw instrument in thyroidectomy: a 1-year prospective observational study. Eur Arch Otorhinolaryngol. (2018) 275:1257–63. doi: 10.1007/s00405-018-4912-9
8. Yang X, Cao J, Yan Y, Liu F, Li T, Han L, et al. Comparison of the safety of electrotome, Harmonic scalpel, and LigaSure for management of thyroid surgery. Head Neck. (2017) 39:1078–85. doi: 10.1002/hed.24701
9. Cannizzaro MA, Borzì L, Lo Bianco S, Okatyeva V, Cavallaro A, Buffone A. Comparison between Focus Harmonic scalpel and other hemostatic techniques in open thyroidectomy: a systematic review and meta-analysis. Head Neck. (2016) 38:1571–8. doi: 10.1002/hed.24449
10. Garas G, Okabayashi K, Ashrafian H, Shetty K, Palazzo F, Tolley N, et al. Which hemostatic device in thyroid surgery? A network meta-analysis of surgical technologies. Thyroid. (2013) 23:1138–50. doi: 10.1089/thy.2012.0588
11. Revelli L, Damiani G, Bianchi CB, Vanella S, Ricciardi W, Raffaelli M, et al. Complications in thyroid surgery. Harmonic scalpel, harmonic focus versus conventional hemostasis: a meta-analysis. Int J Surg. (2016) 28(Suppl. 1):S22–S32. doi: 10.1016/j.ijsu.2015.12.050
12. Docimo G, Ruggiero R, Gubitosi A, Casalino G, Bosco A, Gili S, et al. Ultrasound scalpel in thyroidectomy. Prospective randomized study. Ann Ital Chir. (2012) 83:491–6. pii: S0003469X1201843X22801381
13. Lee SH, Nguyen TK, Ong WS, Haaland B, Tay GC, Tan NC, et al. Comparing the utility and surgical outcomes of harmonic focus ultrasonic scalpel with ligasure small jaw bipolar device in thyroidectomies: a prospective randomized controlled trial. Ann Surg Oncol. (2019) 26:4414–22. doi: 10.1245/s10434-019-07806-w
14. Rahbari R, Mathur A, Kitano M, Guerrero M, Shen WT, Duh QY, et al. Prospective randomized trial of ligasure versus harmonic hemostasis technique in thyroidectomy. Ann Surg Oncol. (2011) 18:1023–7. doi: 10.1245/s10434-010-1251-5
15. Ruggiero R, Gubitosi A, Conzo G, Gili S, Bosco A, Pirozzi R, et al. Sutureless thyroidectomy. Int J Surg. (2014) 12(Suppl 1):S189–S93. doi: 10.1016/j.ijsu.2014.05.011
16. Canu GL, Medas F, Podda F, Tatti A, Pisano G, Erdas E, et al. Thyroidectomy with energy-based devices: surgical outcomes and complications-comparison between Harmonic Focus, LigaSure Small Jaw and Thunderbeat Open Fine Jaw. Gland Surg. (2020) 9:721–6. doi: 10.21037/gs.2020.03.31
17. Konturek A, Szpyra B, Stopa-Barczyńska M, Barczyński M. Energy-based devices for hemostasis in thyroid surgery. Gland Surg. (2020) 9:S153–S8. doi: 10.21037/gs.2019.10.17
18. Jiang J, Shen M, Lu H. Ultrasonic scalpel with knot tying protects parathyroid function for total thyroidectomy with central neck dissection. Gland Surg. (2020) 9:192–9. doi: 10.21037/gs.2020.01.12
19. Li W, Liu B, Shan C, Liu Z, Wang Q, Rao W, et al. Application of carbon nanoparticles in localization of parathyroid glands during total parathyroidectomy for secondary hyperparathyroidism. Am J Surg. (2020) 220:1586–91. doi: 10.1016/j.amjsurg.2020.04.034
20. Arat YO, Sezenoz AS, Bernardini FP, Alford MA, Tepeoglu M, Allen RC. Comparison of Colorado microdissection needle versus scalpel incision for aesthetic upper and lower eyelid blepharoplasty. Ophthal Plast Reconstr Surg. (2017) 33:430–3. doi: 10.1097/IOP.0000000000000820
21. Carqueville JC, Chesnut C. Histologic comparison of upper blepharoplasty skin excision using scalpel incision versus microdissection electrocautery needle tip versus continuous wave CO2 laser. Dermatol Surg. (2021) 47:1376–8. doi: 10.1097/DSS.0000000000003178
22. González-López JJ, González-García FJ, Sales-Sanz M, Alonso N, Albandea A, Mateos E. Long-term cicatrization analysis in periocular incisions for oculoplastic surgery performed with cold blade and Colorado needle. Ophthal Plast Reconstr Surg. (2014) 30:225–8. doi: 10.1097/IOP.0000000000000054
23. Liang WQ, Qiu YH, Ji CY, Chen YH, Zhang JQ, Yao YY, et al. A comparative study of surgical outcomes using a Colorado microdissection needle versus standard-size needle electrocautery in one-stage hypospadias repair using a transverse preputial island flap. Minerva Pediatr. (2018) 70:27–34. doi: 10.23736/S0026-4946.16.04314-0
24. Perkins J, Dahiya R. Microdissection needle tonsillectomy and postoperative pain: a pilot study. Arch Otolaryngol Head Neck Surg. (2003) 129:1285–8. doi: 10.1001/archotol.129.12.1285
25. Rideout B, Shaw GY. Tonsillectomy using the Colorado microdissection needle: a prospective series and comparative technique review. South Med J. (2004) 97:11–7. doi: 10.1097/01.SMJ.0000084313.89387.1C
26. Sharma R. Safety of Colorado microdissection needle (stryker) for skin opening in craniomaxillofacial surgery. J Maxillofac Oral Surg. (2012) 11:115–8. doi: 10.1007/s12663-011-0179-z
27. Ramouz A, Rasihashemi SZ, Safaeiyan A, Hosseini M. Comparing postoperative complication of LigaSure Small Jaw instrument with clamp and tie method in thyroidectomy patients: a randomized controlled trial [IRCT2014010516077N1]. World J Surg Oncol. (2018) 16:154. doi: 10.1186/s12957-018-1448-9
28. Sedgwick P. Multiple hypothesis testing and Bonferroni's correction. BMJ. (2014) 349:g6284. doi: 10.1136/bmj.g6284
29. Konishi T, Fujiogi M, Niwa T, Morita K, Matsui H, Fushimi K, et al. Comparison of outcomes after differentiated thyroid cancer surgery performed with and without energy devices: a population-based cohort study using a nationwide database in Japan. Int J Surg. (2020) 77:198–204. doi: 10.1016/j.ijsu.2020.03.072
30. Dionigi G, Wu CW, Kim HY, Liu X, Liu R, Randolph GW, et al. Safety of energy based devices for hemostasis in thyroid surgery. Gland Surg. (2016) 5:490–4. doi: 10.21037/gs.2016.09.01
31. Wang JJ, Huang TY, Wu CW, Lin YC, Tseng HY, Liu CH, et al. Improving voice outcomes after thyroid surgery - review of safety parameters for using energy-based devices near the recurrent laryngeal nerve. Front Endocrinol (Lausanne). (2021) 12:793431. doi: 10.3389/fendo.2021.793431
32. Edafe O, Antakia R, Laskar N, Uttley L, Balasubramanian SP. Systematic review and meta-analysis of predictors of post-thyroidectomy hypocalcaemia. Br J Surg. (2014) 101:307–20. doi: 10.1002/bjs.9384
33. Spartalis E, Ntokos G, Georgiou K, Zografos G, Tsourouflis G, Dimitroulis D, et al. Intraoperative indocyanine green (ICG) angiography for the identification of the parathyroid glands: current evidence and future perspectives. In Vivo. (2020) 34:23–32. doi: 10.21873/invivo.11741
34. Xia W, Zhang J, Shen W, Zhu Z, Yang Z, Li X. A rapid intraoperative parathyroid hormone assay based on the immune colloidal gold technique for parathyroid identification in thyroid surgery. Front Endocrinol (Lausanne). (2020) 11:594745. doi: 10.3389/fendo.2020.594745
35. Moran K, Grigorian A, Elfenbein D, Schubl S, Jutric Z, Lekawa M, et al. Energy vessel sealant devices are associated with decreased risk of neck hematoma after thyroid surgery. Updates Surg. (2020) 72:1135–41. doi: 10.1007/s13304-020-00776-9
36. Siu JM, McCarty JC, Gadkaree S, Caterson EJ, Randolph G, Witterick IJ, et al. Association of vessel-sealant devices vs conventional hemostasis with postoperative neck hematoma after thyroid operations. JAMA Surg. (2019) 154:e193146. doi: 10.1001/jamasurg.2019.3146
37. Bennett NT, Schultz GS. Growth factors and wound healing: biochemical properties of growth factors and their receptors. Am J Surg. (1993) 165:728–37. doi: 10.1016/S0002-9610(05)80797-4
38. Henry G, Garner WL. Inflammatory mediators in wound healing. Surg Clin North Am. (2003) 83:483–507. doi: 10.1016/S0039-6109(02)00200-1
39. Cordón C, Fajardo R, Ramírez J, Herrera MF. A randomized, prospective, parallel group study comparing the Harmonic Scalpel to electrocautery in thyroidectomy. Surgery. (2005) 137:337–41. doi: 10.1016/j.surg.2004.09.011
40. Barczyński M, Konturek A, Cichoń S. Minimally invasive video-assisted thyreoidectomy (MIVAT) with and without use of harmonic scalpel–a randomized study. Langenbeck’s Arch Surg. (2008) 393:647–54. doi: 10.1007/s00423-008-0373-8
Keywords: microdissection tungsten needle, harmonic scalpel, energy-based devices, total thyroidectomy, central neck dissection, papillary thyroid carcinoma, hemostasis
Citation: Zheng W, Zhu S, Zhang Y, Wang Z, Liao S and Sun S (2022) Novel application of microdissection tungsten needle in total thyroidectomy with central neck dissection for papillary thyroid carcinoma. Front. Surg. 9:896275. doi: 10.3389/fsurg.2022.896275
Received: 14 March 2022; Accepted: 4 August 2022;
Published: 26 August 2022.
Edited by:
Fabio Medas, University of Cagliari, Italy© 2022 Zheng, Zhu, Zhang, Wang, Liao and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shichong Liao bGlhb3Njd2h1QDE2My5jb20= Shengrong Sun c3VuMTM3QHNpbmEuY29t
†These authors have contributed equally to this work and share first authorship
Specialty Section: This article was submitted to Otorhinolaryngology - Head and Neck Surgery, a section of the journal Frontiers in Surgery
Abbreviations EBD, nergy-based devices; MDTN, microdissection tungsten needle; TT, total thyroidectomy; CND, central neck dissection; HS, harmonic scalpel; CE, conventional electrocautery; RLN, recurrent laryngeal nerve; BMI, body mass index; VAS, visual analog scale; RTC, randomized controlled trial; H&E, hematoxylin and Eeosin staining; TNF-α, tumor Necrosis Factor-alpha; IL-6, interleukin-6; PTH, parathyroid hormone
 Weijie Zheng
Weijie Zheng Shan Zhu†
Shan Zhu† Zhong Wang
Zhong Wang Shengrong Sun
Shengrong Sun