
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg., 20 May 2022
Sec. Reconstructive and Plastic Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.882726
 Jia Wang1*
Jia Wang1* Zhenzhen Zhang2
Zhenzhen Zhang2
Objective: To investigate the effect of gastric negative pressure suction on the incidence of postoperative nausea and vomiting (PONV) in patients undergoing orthognathic surgery.
Methods: A retrospective study of 772 patients who underwent orthognathic surgery from October 2016 to January 2021 was performed, excluding possible confounding factors. The patients were divided into a negative gastric suction group (group 1) and a group without gastric suction (group 2), according to whether gastric suction was used after general anaesthesia. There were 386 patients in each group. The incidence of PONV was compared between the two groups.
Results: The incidence of PONV was 29% in the negative gastric suction group and 58.8% in the non-gastric suction group. The incidence of PONV in the gastric negative pressure suction group was significantly lower than that in the non-gastric negative pressure suction group, and the difference was statistically significant (p < 0.05).
Conclusion: By reducing the risk of perioperative bleeding in orthognathic surgery, gastric negative pressure aspiration can reduce the incidence and operation time of PONV after orthognathic surgery.
Postoperative nausea and vomiting (PONV) have always been a worrying problem after general anaesthesia. The incidence is estimated at 30% in the general surgical population and up to 80% in high-risk cohorts (1). In orthognathic surgery, the proportion is 40% (1–3). Patients undergoing orthognathic surgery were 6.75 times as likely to experience vomiting than those who had other types of surgery (4). PONV can cause bleeding, delayed healing, and wound infection. A painful experience and even accidental inhalation of vomit may endanger the patient’s life.
Gastrointestinal decompression is the use of negative pressure suction, also known as gastric negative pressure suction, which refers to the suction of gastrointestinal contents to reduce internal pressure. A gastrointestinal decompressor or other instrument is used to suck out food, gas, secretions, exudates, etc., from the gastrointestinal tract to relieve the adverse consequences caused by increased internal pressure. It is mostly used for patients before gastrointestinal surgery to facilitate surgery. It is also used for patients after gastrointestinal and abdominal surgery to prevent negatively affecting the results of surgery. In patients with gastrointestinal tumours or other inoperable conditions, the gastrointestinal tract accumulates too much, so the treatment relieves symptoms and pain.
Studies have shown that PONV is associated with many factors, such as anaesthetic drugs, opioids, age, sex, body mass index (BMI), surgical site, and body habits (5). However, there is no mention of whether the gastric negative pressure suction method to reduce intragastric blood stimulation after orthognathic surgery can reduce the incidence of PONV.
Through postoperative observation and communication with patients to reduce the incidence of postoperative PONV, we found that intragastric blood stimulation in patients with orthognathic surgery may also lead to PONV (6, 7), especially within 24 h of the operation. Therefore, this study mainly discusses the relationship between gastric negative pressure suction and the incidence of PONV after orthognathic surgery.
This study followed the Declaration of Helsinki and was approved by the hospital ethics committee. This retrospective study included the clinical data of patients who underwent orthognathic surgery in our hospital from October 2016 to January 2021. Inclusion criteria for this study: (a) patients over 18 years who underwent maxillary or mandibular orthognathic surgery; (b) patients with postoperative PONV (including nausea, vomiting, or retching); and (c) nursing records showing that PONV occurred within 24 h in PACU and ICU. Exclusion criteria: patients with gastrointestinal problems, dizziness, migraine, and pharyngitis were excluded from this study. Finally, 772 patients were selected from 802 patients.
Both groups used intravenous inhalation combined anaesthesia. The anaesthetics used included sevoflurane, oxygen, sufentanil, fentanyl, and propofol. There was no difference in medication between the two groups. The surgical site was divided into three categories: (1) maxillary procedures (maxillary osteotomies); (2) mandibular procedures (mandibular sagittal osteotomies, distraction osteogenesis, genioplasty); and (3) bi-jaw procedures (maxillary and mandibular osteotomies).
On the doctor’s decision, all patients returned to PACU after orthodontic surgery without intermaxillary fixation. No nasogastric tube was used in any patients to reduce the irritation of the stomach tube to the patient’s throat.
Group 1: After the orthognathic surgery, the patients were returned to PACU. Patients under general anaesthesia were not fully awake. Doctors and nurses administered further anaesthesia to facilitate the study. We inserted tubes on one side of the patient’s nasal cavity to attract nasal mucus and blood, then inserted tubes into the stomach to attract the stomach blood, gas, and gastric juices. An anaesthesiologist gave patients anti-nausea drugs (Tropisetron Hydrochloride Injection, 5 mg IV) at the end of the operation and, based on the clinical situation, gave analgesic and sedative drugs. Group 2: gastric negative pressure suction was not used after the operation. The changes in operation time and postoperative PONV incidence were compared between the two groups.
In previous studies, increased BMI, gender differences, maxillary surgery, and prolonged operation time all led to an increase in the incidence of postoperative PONV. The incidence of PONV in women is higher than that in men, and increased blood loss results in increased blood swallowing during maxillary surgery. Therefore, we compared whether there were statistically significant differences between the two groups in terms of gender, operation time, operation methods, BMI, and so on (3, 4, 5, 8). The results showed no statistical difference between the two groups (see Table 1).
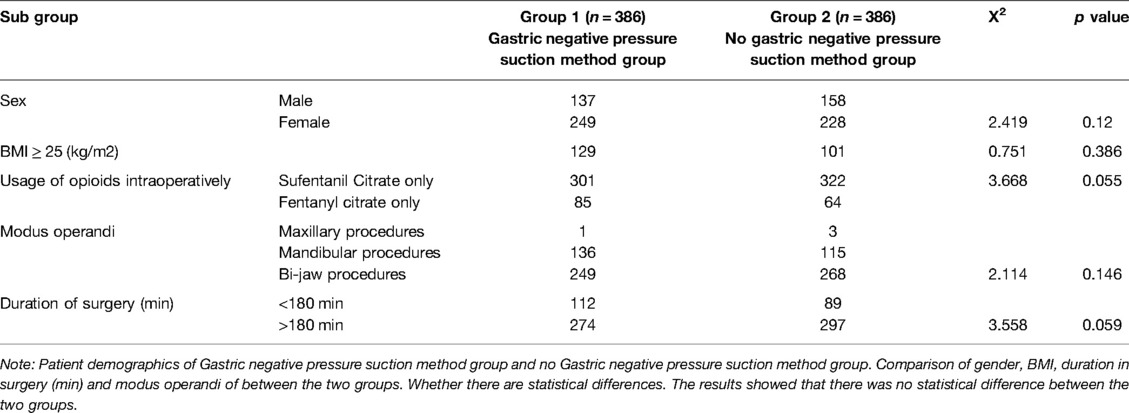
Table 1. Patient demographics of Gastric negative pressure suction method group and no Gastric negative pressure suction method group.
The evaluation standard adopts the PONV evaluation method recommended by the World Health Organization. Grade 0 means that the patient does not have nausea and vomiting. Grade I means that the patient has slight nausea, abdominal discomfort, and no vomiting. Grade II means that the patient has moderate nausea and obvious vomiting. Grade III means that the patient has severe nausea and vomiting with vomiting of gastric contents, and this was difficult to control with drugs. We observed and asked for patients’ subjective symptoms in real-time, recorded the severity of postoperative nausea and vomiting, strictly implemented the evaluation criteria, and took the patient’s feelings when lying still as criteria. We compared the first exhaust time and defecation time after the operation between the two groups. We compared the number of cases requiring the postoperative rescue antiemetic drug metoclopramide injections between the two groups.
SPSS 26.0 statistical software was used to sort and analyse the data, and the results were statistically analysed by Chi-square tests of nonparametric variables. The results were considered significant at the critical level of 5% (p < 0.05).
Patients were divided into a gastric suction group (group 1) and a non-gastric suction group (group 2) according to whether gastric suction was used after general anaesthesia, with 386 patients in each group. Group 1 consisted of 137 males and 249 females. Group 2 consisted of 158 males and 228 females. There were no significant differences between the two groups. The average body fat of group 1 was 129, and that of group 2 was 101. In the first group, the operation time was less than 180 min in 112 cases and more than 180 min in 274 cases. In group 2, the operation time was less than 180 min in 89 cases and more than 180 min in 297 cases. The operation time of the first group was shorter than that of the second group, as shown in Table 1.
The incidence of PONV was 29% in group 1 and 58.8% in group 2. The incidence of PONV in group 1 was significantly lower than in group 2 (p < 0.05), as shown in Table 2 and Figure 1.
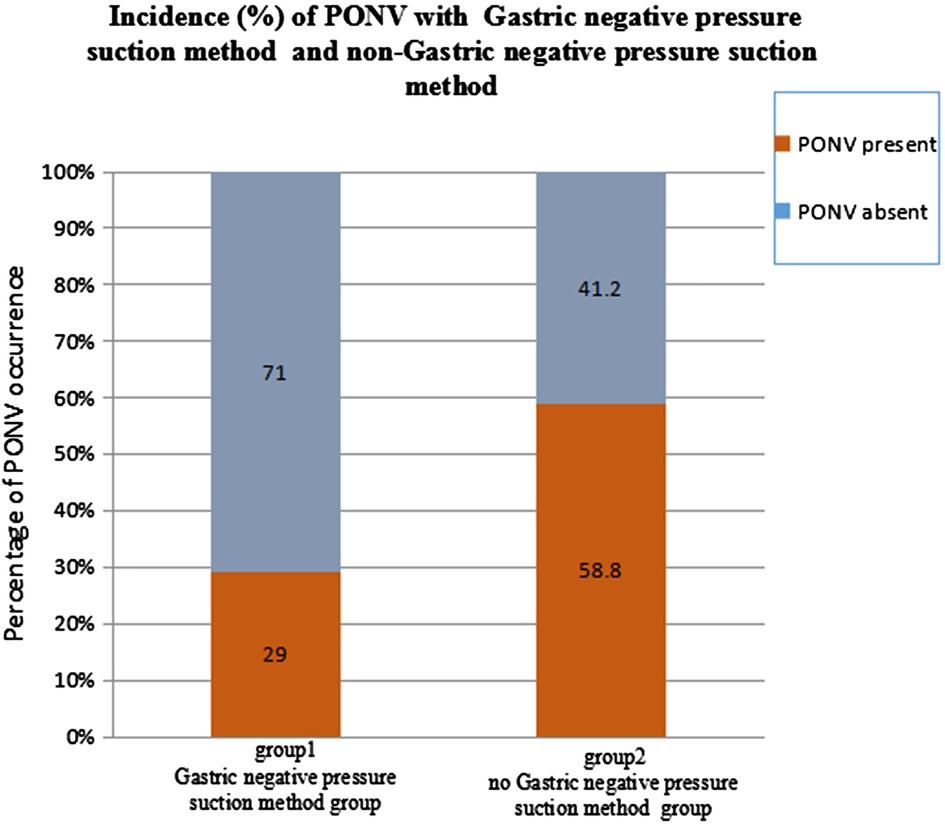
Figure 1. The incidence of PONV in patients undergoing the Gastric negative pressure suction method after orthognathic general anaesthesia was 29.8% lower than that in patients without the Gastric negative pressure suction method.
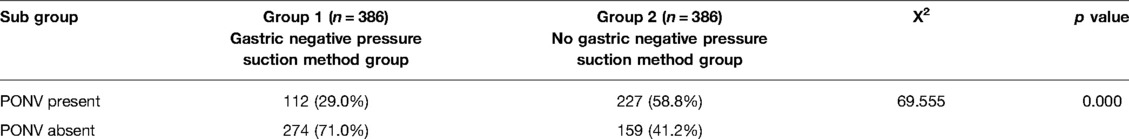
Table 2. PONV results for the Gastric negative pressure suction method and no g Gastric negative pressure suction method.
After oral and maxillofacial surgery, patients are prone to complications such as nausea, vomiting, pain, infection, and scars. The most common postoperative complications are the incidence of nausea and vomiting at about 40%, which seriously affects the prognosis quality of patients and the overall curative effects of surgical treatment (9).
The occurrence of PONV includes the comprehensive results of various factors, including surgical, patient, and anaesthesia factors. Since 2015, we have been making continuous improvements in reducing the incidence of PONV after orthognathic surgery, such as preoperative psychological counselling, shortening the duration of general anaesthesia, applying antiemetic drugs in time after surgery, reducing the application of anaesthetic drugs that can easily cause PONV in patients, and reducing intraoperative bleeding.
In addition, in previous studies, gastric tubes also caused postoperative PONV by stimulating the glossopharyngeal nerve. Indwelling gastric tubes caused chronic stimulation of the pharynx and larynx, and PONV. After orthognathic general anaesthesia, doctors would decide whether to use gastric tubes according to the patient’s condition. However, it was found that patients using gastric tubes after orthognathic surgery had poor tolerance to gastric tube stimulation. This increased the incidence of PONV and delayed postoperative recovery (10, 11). Since 2015, gastric tubes have no longer been used in patients receiving general anaesthesia while undergoing orthognathic surgery in our hospital, but oral care has been increased to reduce the possibility of postoperative PONV and intraoral wound infection.
Previous studies have also proposed whether a pharyngeal pack is performed to absorb blood and irrigation fluids and provide a physical barrier against aspiration of surgical debris into the aerodigestive passages and oesophagus, and reduce the incidence of postoperative PONV, such as the application of pharyngeal packs in nasal surgery and minor oral surgery. However, through analysis and research, it is concluded that a pharyngeal pack has no significant effect on reducing the occurrence of PONV, and some studies suggest that a pharyngeal pack should not be used during surgery. In this study, some patients also received a pharyngeal pack during their operation, but because previous studies showed that a pharyngeal pack had no significance for the incidence of postoperative PONV, these patients were not included in this study (12–15).
In this study, we also excluded patients with the previous PONV, vertigo, migraine, and pharyngitis from this study to reduce confounding factors (1, 5–8). In order to reduce the possibility of perioperative bleeding, patients with hypertension before an operation should take active treatment to control their blood pressure to within the normal range. Controlled hypotension during anaesthesia in Lefort I osteotomy can be regarded as a safe method for reducing intraoperative blood loss and, in turn, improving the surgical field (16).
There are limitations to our study. A team of 11 anaesthesiologists was used, and each anaesthesiologist was responsible for one orthognathic surgery patient. Therefore, there are differences in anaesthesia induction, medication, and medication methods. At the same time, there were three teams that could perform orthognathic surgery, and at least two patients underwent orthognathic surgery every day. The intraoperative and postoperative blood loss of each team was also different. This study is a retrospective study, so there may be bias. It is hoped that a prospective study can be carried out in the future.
In this study, we found intraoperative and postoperative blood swallowing, intraoperative flushing fluid into the stomach, and gastric gas during anaesthesia are risk factors for postoperative PONV. To reduce the risk of bleeding during the perioperative period in patients undergoing orthognathic surgery, the gastric negative pressure suction method after orthognathic surgery can reduce stimulation to the stomach and gastric pressure, thus reducing the incidence of postoperative PONV. During peri-orthognathic surgery, through psychological intervention, comprehensive observation, and timely and accurate records, nurses can take the correct gastric negative pressure suction method. This is of great significance in reducing the incidence of PONV in patients after surgery.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by the ethics committee of the School and Hospital of Stomatology China Medical University. The patients/participants provided their written informed consent to participate in this study.
All authors have been involved in drafting the manuscript and revising it. All authors approve this manuscript and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Apfel CC, Läärä E, Koivuranta M, Greim CA, Roewer N. A simplified risk score for predicting postoperative nausea and vomiting: conclusions from cross-validations between two centers. Anesthesiology. (1999) 91(3):693–700. doi: 10.1097/00000542-199909000-00022
2. Kovac AL. Prevention and treatment of postoperative nausea and vomiting. Drugs. (2000) 59:213–43. doi: 10.2165/00003495-200059020-00005
3. Silva AC, O’Ryan F, Poor DB. Postoperative nausea and vomiting (PONV) after orthognathic surgery: a retrospective study and lit-erature review. J Oral Maxillofac Surg. (2006) 64(9):1385–97. doi: 10.1016/j.joms.2006.05.024
4. Laskin DM, Carrico CK, Wood J. Predicting postoperative nausea and vomiting in patients undergoing oral and maxillofacial surgery. Int J Oral Maxillofac Surg. (2020) 49(1):22–7. doi: 10.1016/j.ijom.2019.06.016
5. Ghosh S, Rai KK, Shivakumar HR, Upasi AP, Naik VG, Bharat A. Incidence and risk factors for postoperative nausea and vomiting in orthognathic surgery: a 10-year retrospective study. J Korean Assoc Oral Maxillofac Surg. (2020) 46(2):116–24. doi: 10.5125/jkaoms.2020.46.2.116
6. Tóth B, Lantos T, Hegyi P, Viola R, Vasas A, Benkő R, et al. Ginger (Zingiber officinale): an alternative for the prevention of postoperative nausea and vomiting. A meta-analysis. Phytomedicine. (2018) 50:8–18. doi: 10.1016/j.phymed.2018.09.007
7. Emami-Sahebi A, Elyasi F, Yazdani-Charati J, Shahhosseini Z. Psychological interventions for nausea and vomiting of pregnancy: a systematic review. Taiwan J Obstet Gynecol. (2018) 57(5):644–9. doi: 10.1016/j.tjog.2018.08.005
8. Pourtaheri N, Peck CJ, Maniskas S, Park KE, Allam O, Chandler L, et al. A comprehensive single-center analysis of postoperative nausea and vomiting following orthognathic surgery. J Craniofac Surg. (2022) 33(2):584–7. doi: 10.1097/SCS.0000000000008052
9. Corcoran TB, Truyens EB, Ng A, Moseley N, Doyle AC, Margetts L. Anti-emetic dexamethasone and postoperative infection risk: a retrospective cohort study. Anaesth Intensive Care. (2010) 38(4):654–60. doi: 10.1177/0310057X1003800406
10. Maza C, López AM, Kulyapina A, Leno B, Tousidonis M, Garcia A, et al. Orthognathic surgery: nasogastric tube responsable of the nausea and vomiting? Int J Oral Maxillofac Surg. (2013) 42(10):1333. doi: 10.1016/j.ijom.2013.07.564
11. Watcha MF, White PF. Postoperative nausea and vomiting. Its etiology, treatment, and prevention. Anesthesiology. (1992) 77(1):162–84. doi: 10.1097/00000542-199207000-00023
12. Koivuranta M, Läärä E, Snåre L, Alahuhta S. A survey of postoperative nausea and vomiting. Anaesthesia. (1997) 52(5):443–9. doi: 10.1111/j.1365-2044.1997.117-az0113.x
13. Al-Lami A, Amonoo-Kuofi K, Kulloo P, Lakhani R, Prakash N, Bhat N. A study evaluating the effects of throat packs during nasal surgery: a randomised controlled trial. Eur Arch Otorhinolaryngol. (2017) 274(8):3109–14. doi: 10.1007/s00405-017-4589-5
14. Al-Jandan BA, Syed FA, Zeidan A, Marei HF, Farooq I. Pharyngeal pack placement in minor oral surgery: a prospective, randomized, controlled study. Ear Nose Throat J. (2018) 97(3):E18–E21. PMID: 29554406
15. Green R, Konuthula N, Sobrero M, Saini A, Parasher A, Pool C. Use of pharyngeal packs in functional endoscopic sinus surgery: a randomized controlled trial. Laryngoscope. (2017) 127(11):2460–65. doi: 10.1002/lary.26651
Keywords: gastric negative pressure suction, orthognathic surgery, PONV, operation time, retrospective study
Citation: Wang J and Zhang Z (2022) Gastric Negative Pressure Suction Method Reduces the Incidence of PONV after Orthognathic Surgery. Front. Surg. 9:882726. doi: 10.3389/fsurg.2022.882726
Received: 24 February 2022; Accepted: 21 April 2022;
Published: 20 May 2022.
Edited by:
Sergio Olate, University of La Frontera, ChileReviewed by:
Essam Ahmed Al-Moraissi, Thamar University, YemenCopyright © 2022 Wang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jia Wang MzY5MzM3NTIxQHFxLmNvbQ==
Speciality section: This article was submitted to Reconstructive and Plastic Surgery, a section of the journal Frontiers in Surgery
Abbreviations: PONV, Postoperative nausea and vomiting; MAP, mean arterial pressure.
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.