- 1Department of Anesthesia, Intensive Care and Emergency, “Città della Salute e della Scienza di Torino” Hospital, Torino, Italy
- 2Department of Cardiovascular and Thoracic Surgery, “Città della Salute e della Scienza di Torino” Hospital, Torino, Italy
- 3Department of Surgical Science, University of Turin, Torino, Italy
- 4Anesthesia and Intensive Care Unit, General and Specialistic Surgical Department, Arcispedale Santa Maria Nuova, Azienda USL – IRCCS di Reggio Emilia, Reggio Emilia, Italy
Non-intubated thoracic surgery (NITS) is a growing practice, alongside minimally invasive thoracic surgery. To date, only a consensus of experts provided opinions on NITS leaving a number of questions unresolved. We then conducted a scoping review to clarify the state of the art regarding NITS. The systematic review of all randomized and non-randomized clinical trials dealing with NITS, based on Pubmed, EMBASE, and Scopus, retrieved 665 articles. After the exclusion of ineligible studies, 53 were assessed examining: study type, Country of origin, surgical procedure, age, body mass index, American Society of Anesthesiologist's physical status, airway management device, conversion to orotracheal intubation and pulmonary complications rates and length of hospital stay. It emerged that NITS is a procedure performed predominantly in Asia, and certain European Countries. In China, NITS is more frequently performed for parenchymal resection surgery, whereas in Europe, it is mainly employed for pleural pathologies. The most commonly used device for airway management is the laryngeal mask. The conversion rate to orotracheal intubation is a~3%. The results of the scoping review seem to suggest that NITS procedures are becoming increasingly popular, but its role needs to be better defined. Further randomized clinical trials are needed to better define the role of the clinical variables possibly impacting on the technique effectiveness.
Systematic Review Registration: https://osf.io/mfvp3/, identifier: 10.17605/OSF.IO/MFVP3.
Introduction
Parallel to the growth of minimally invasive surgical thoracic techniques, non-intubated thoracic surgery (NITS) has been increasingly used (1, 2). NITS procedures appear to avoid either the adverse effects of mechanical ventilation in patients with already impaired pulmonary functional capacity before surgery, and the residual effects of neuromuscular blockers, providing more rapid recovery of respiratory muscle function and less perioperative morbidity (1, 3).
While NITS technique is becoming increasingly popular, there is still no clarity in how it is defined and performed. For example, the procedure is reported in the literature as non-intubated thoracic surgery, but also referred to as tubeless video-assisted thoracoscopic surgery (VATS) or awake thoracic surgery.
Although an expert consensus recently attempted to clarify and establish the critical points of NITS, some perioperative surgical and anesthesiological evaluation variables remained undefined (4).
In order to better clarify the background of NITS, surgical indications, type of patient to be proposed for the procedure, airway management, postoperative complications, and length of stay (LOS) a scoping review based on a systematic literature review was conducted.
Protocol and Registration
The study protocol was developed using the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines (5) revised by the members of the thoracic surgery research team of “Città della Salute e della Scienza” university hospital (Turin – Italy). The final protocol was registered prospectively with the Open Science Framework on 26th September 2021 (https://osf.io/mfvp3/).
Eligibility Criteria
Peer-reviewed articles dealing with NITS with the following characteristics were identified as potentially eligible: (1) randomized controlled trials (RCTs) and non-RCTs (NRCTs); (2) published in English; (3) involving adult participants (>18 years old).
Information Sources and Search Strategy
Potentially relevant studies were searched through September 2021 in Pubmed, EMBASE and Scopus using the search strategies reported in the Supplementary Materials (Supplementary File 1). The results were exported to EndNote V.X9 (Clarivate Analytics, PA, USA), and the duplicates were automatically removed.
Studies Evaluation and Selection of Sources of Evidence
The review process was carried out in two steps consisting of evaluating the titles, abstracts, and then full text of all publications identified by our searches for potentially relevant manuscripts. For both levels, four authors worked in pairs (GLR, EC, EB, and MC) and screened the articles with conflicts resolved by consensus and discussion with other reviewers.
Data Charting Process and Data Items and Synthesis of Results
A planned Excel spreadsheet was developed by reviewers to determine which variables to extract used (study characteristics, patient characteristics, surgical procedures, country, age, number of patients, body mass index (BMI), Forced Expiratory Volume in the 1st second (FEV1), diffusing capacity for carbon monoxide (DLCO), American Society of Anesthesiologists (ASA) physical status classification, intraoperative drugs used, type of anesthesia, type of regional analgesia, bispectral index (BIS) utilization, airway management device, conversion to orotracheal intubation (OTI), conversion to thoracotomy, postoperative pain, postoperative pulmonary complications, and postoperative days of hospitalization). The reviewers independently charted the data in pairs. If not available, any ongoing study was contacted to include unpublished data if applicable. We grouped the studies by the type of study (with or without a comparison group). Where we identified a systematic review, we counted the number of studies included in the review that potentially met our inclusion criteria and noted how many studies had been missed by our search.
Results
Selection of Sources of Evidence PRISMA
We followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines (5). The systematic literature search performed in September 2021 retrieved 665 results. After deduplication, 283 studies were evaluated. Three hundred eighty-two and 234 were, respectively excluded following the first and second evaluation process bringing the number of studies included in the scoping review to 49. To these, four more articles (6–9) previously reported in systematic reviews were added leading the total number of articles included to 53, all published after 2011.
General Characteristics of Included Studies
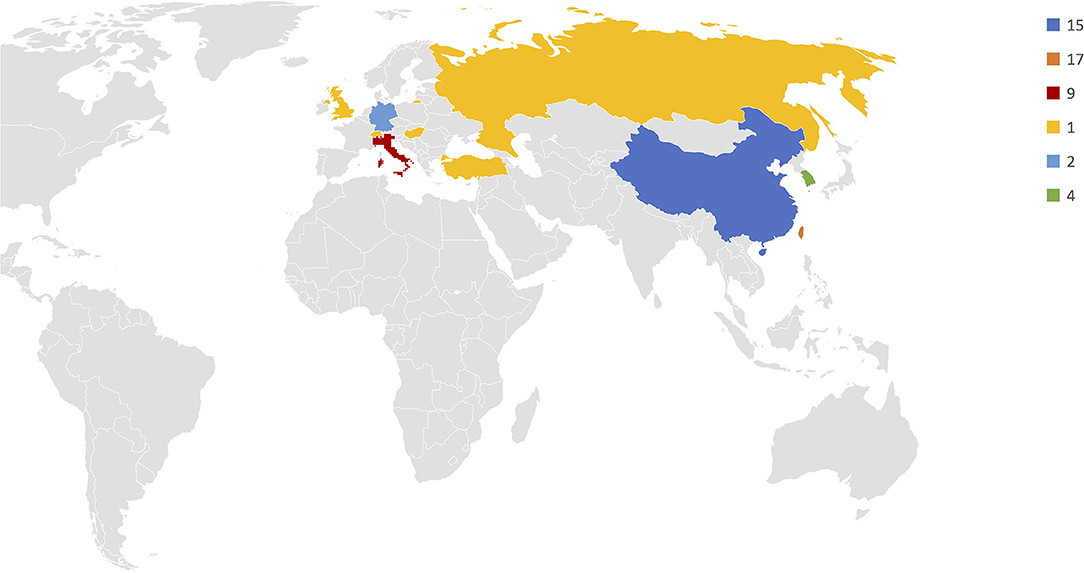
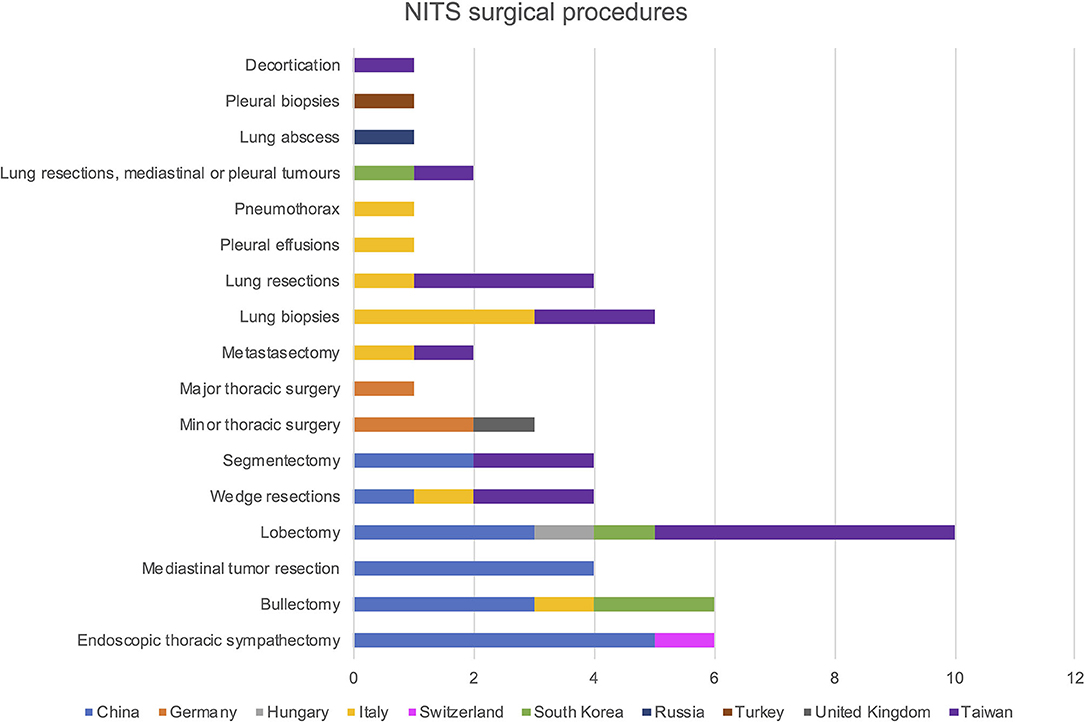
Among the 53 included studies, 30 were cohort studies comparing NITS and intubated-patient thoracic surgery, whereas 22 were single-cohort studies of patients undergoing NITS. Seventeen were conducted in Taiwan, 15 in China, nine in Italy, four in South Korea, two in Germany and one in Turkey, United Kingdom, Russia, Switzerland, and Hungary (Figure 1). Patients' characteristics are summarized in Table 1.
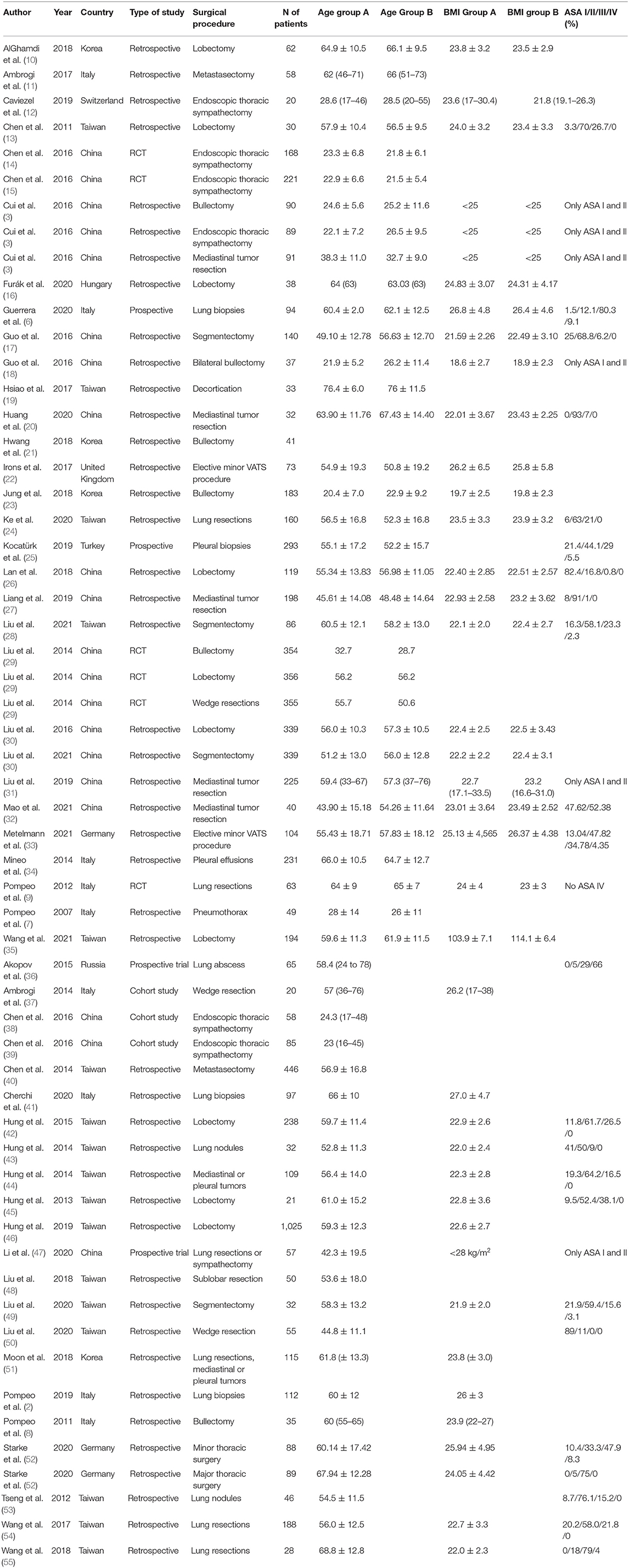
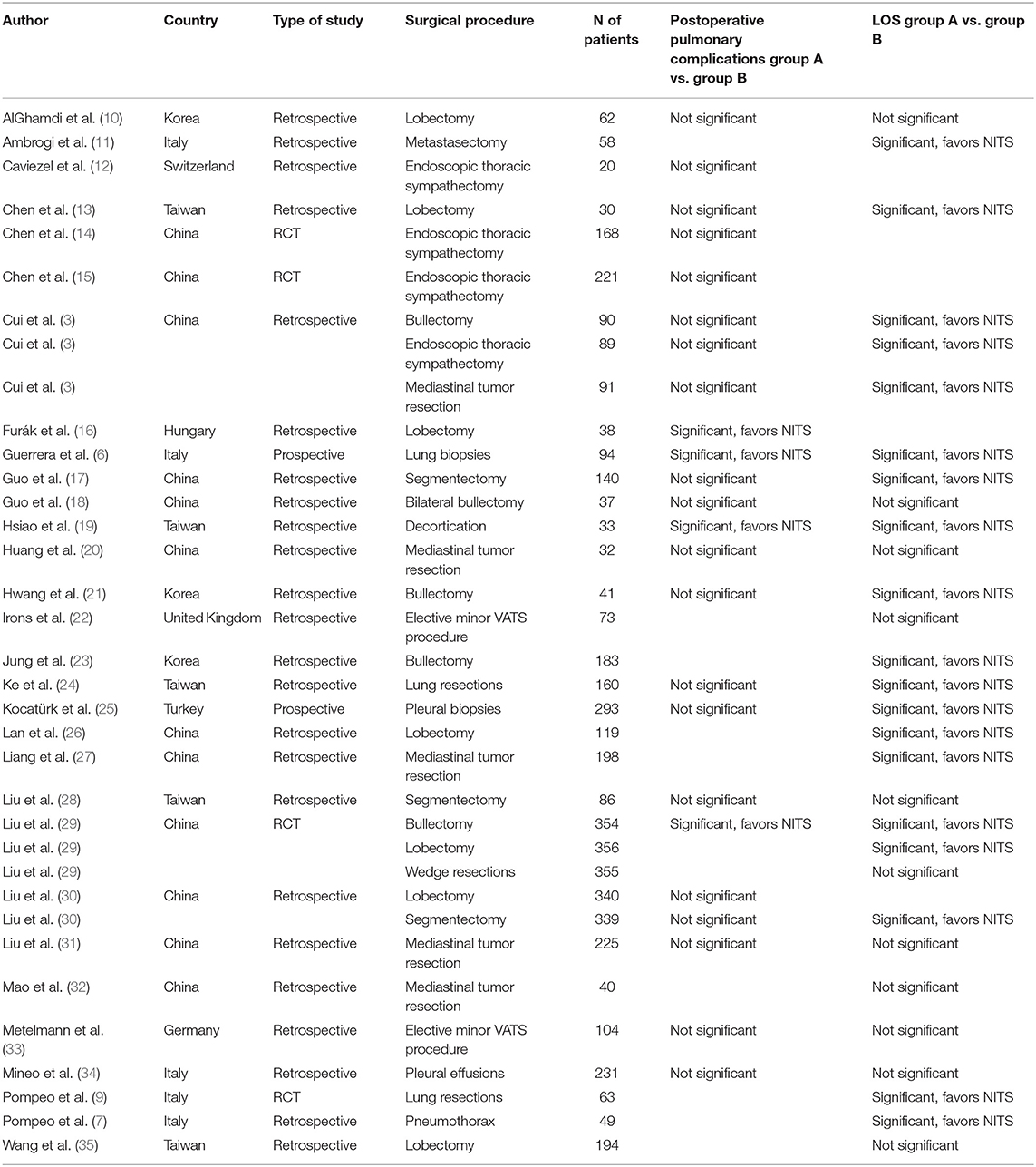
Regarding the described surgical procedures: 17.9% were lobectomies, 10.7% endoscopic thoracic sympathectomies, 10.7% bullectomies, 8.9% lung biopsies, 7.1% mediastinal tumor resections, wedge resections, segmentectomies, and lung resections, respectively. In 5.4% of cases the procedure was classified as minor thoracic surgery, without reporting a precise surgical technique, 3.6% were mastectomy and lung resections, mediastinal or pleural tumors, and major thoracic surgeries. Pleural effusions, pneumothorax, lung abscess, pleural biopsies, and decortications were reported in the 1.8% of cases. Surgical procedures as used in different Country are reported in Figure 2.
Anesthesiological and Intraoperative Management
Not all studies reported information on how the airways were managed. Laryngeal mask (LMA) was used in 37.5% of cases, facemask in 31.3% of cases, Venturi mask in 22.9% of cases, high-flow nasal cannulas (HFNC) in 6.3%, and nasal cannulas in 2.0%. The type of device used in different Countries is reported in Figure 3.
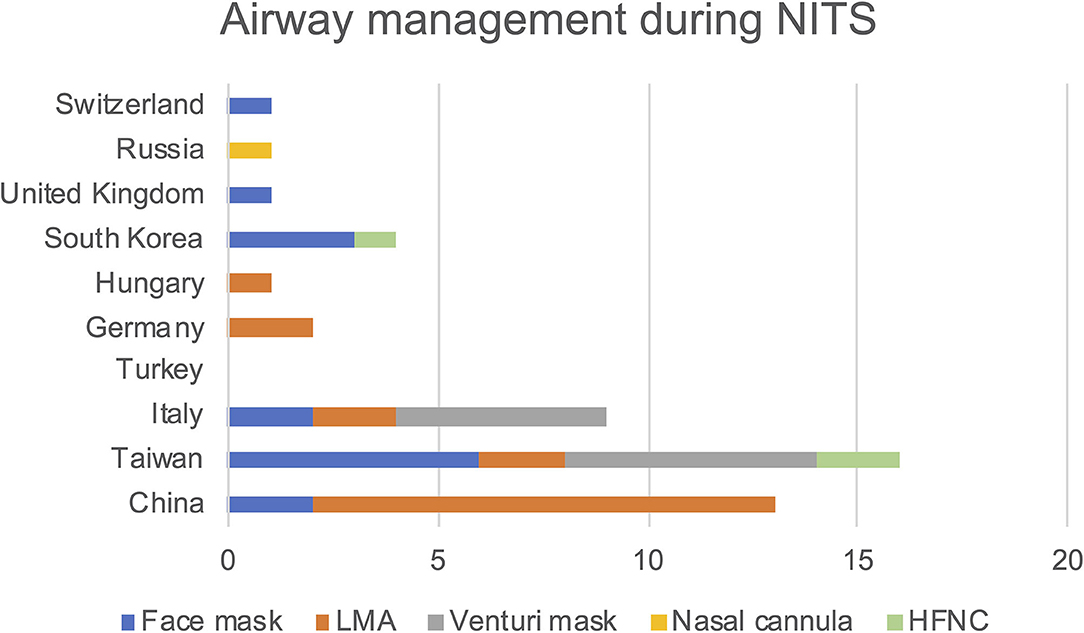
Figure 3. Frequency of airway management devices used within the various clinical trials divided by country of the primary country in which the study was conducted.
Average conversion rate to intubation was 0.9% in China, 3.9% in Taiwan, 2.3% in Italy, 1% in Turkey, 5% in Germany and 3.7% in South Korea. The conversion rate to thoracotomy was estimated to be 0.1% in China, 0.3% in Taiwan, 2.3% in Italy, and 3.5% in South Korea. Not all studies reported these data.
Main Outocomes
Length of hospital stay and postoperative pulmonary complications rate, as collected in studies comparing the cohort of patients treated with NITS and intubated VATS, are shown in Table 2.
Same data as collected from single cohort studies are instead shown in Figure 4. In Figure 4 are also presented the data relating to pulmonary complications by type of procedure as taken from single cohort studies.
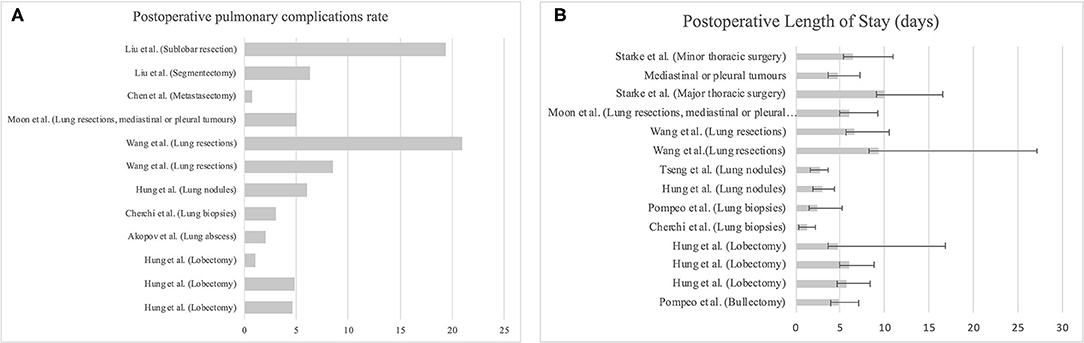
Figure 4. (A) Postoperative pulmonary complications expressed as frequency split by type of surgery. (B). Length of stay, expressed as mean and standard deviation, split by type of surgery.
Perioperative Analgesia
Analgesia performed in the perioperative period was not reported in all studies. Of the studies analyzed, 42.4% used intercostal nerve block, 40.7% thoracic epidural analgesia, 6.8% paravertebral block, 5.1% infiltration with local anesthetic of the wound, 3.4% erector spinae plane block, and 1.6% placed a catheter at the paravertebral site for continuous analgesia. Evaluating NITS vs. non-NITS cohort studies the postoperative pain was significantly lower in the NITS group in five studies (3, 6, 14, 15, 22), whereas the findings were not statistically significant in six studies (19, 21, 25, 28, 31, 32).
Meta-analyzing the available data from observational studies (Figure 5) with a continuous random-effects model showed that the mean postoperative pain rate (VAS) is 1.842 (95% C.I. 1.451–2.233) with a heterogeneity of 96.6%, p < 0.001.
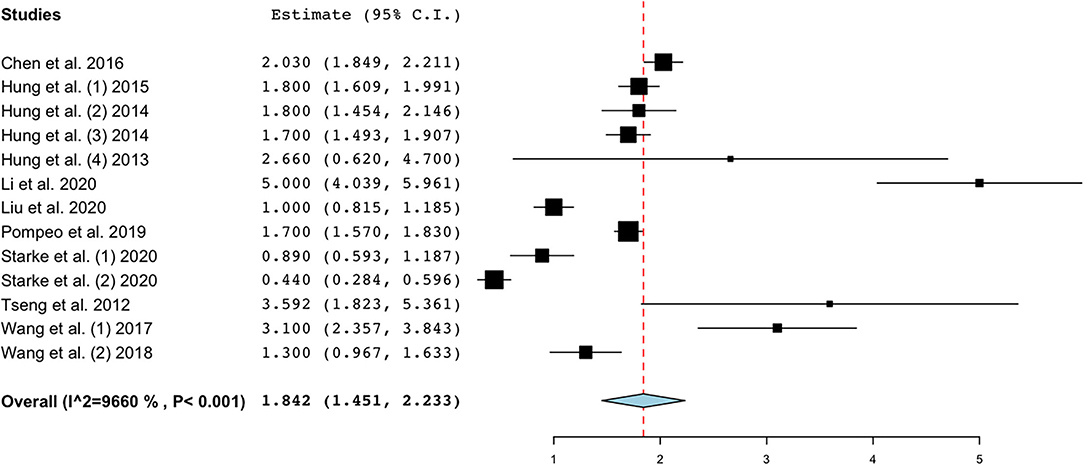
Figure 5. Postoperative pain on day 1 expressed in VAS. Evaluation by all observational studies. Figure created with OpenMetaAnalyst.
Discussion
In this scoping review, we analyzed 53 primary studies regarding NITS published between 2011 and 2021. The studies are all fairly recent confirming that NITS procedures have gained acceptance quite recently.
One of the objectives of this analysis was to evaluate the clinical context in which NITS is performed. Since the consensus of experts we referred to did not investigate this particular aspect in detail (4), we decided to assess whether there is a type of surgical procedure or airway management on which there is consensus among different Countries. What seems to emerge is that NITS is a procedure performed predominantly in Asia, and in some European countries, first Italy. We did not find any studies conducted in the United States. The trials conducted are mostly focused on selected populations, allowing direct comparison between intubated and non-intubated thoracic surgery. The shortage of clinical trials justifies the lack of consensus and guidelines on its management.
We evaluated the type of surgery performed during NITS by Country: while in China it was mainly used in lung parenchymal surgery, and in sympathectomies for hyperhidrosis, in Italy, it was mainly adopted for minor thoracic operations, such as lung biopsies or pleural effusions, confirming what Pompeo et al. reported in their European survey (56). In Taiwan instead, NITS procedures were used in a more heterogeneous manner, including both major parenchymal procedures, such as lobectomies, and minor procedures.
When assessing the anthropometric characteristics of the population, we found that there was a considerable heterogeneity, and this was probably due to a lack of specific guidelines indicating the population in which NITS procedures is most correctly applied. Even considering the NITS expert consensus, we noted that only ASA I and II stage patients, aged between 16 and 60 years, were included. This, in our opinion, hardly represents the average patient who ordinarily undergoes thoracic surgery. Moreover, we believe that such procedures would be rather helpful in frail patients with ASA III and IV status to avoid the stress related to intubation and positive pressure mechanical ventilation in patients with compromised respiratory function (3). There are cases in literature where this technique is used in patients with severe comorbidities, including obesity (57, 58) whereas other groups considered them as contraindications (59).
Regarding airway management, we noted that there was a difference among the Countries considered. The facemask was the most widespread device across the board. In China the LMA was used in most cases, as well as in Germany and in Hungary. This can easily be related to the fact that these Countries mainly performed major thoracic surgery. Although the LMA support during NITS has been described in the literature, it certainly does not allow lighter sedation. To date, there is no recommendation on which device to preferentially use for airway management (60, 61) even if He et al. suggest the use of LMA, nasal cannulas, or face mask as alternatives (4). From our review, the type of device for airway management is highly dependent on the background of the study and the practices of individual centers.
In this regard, a fundamental issue on NITS definition arises, as three studies conducted in China used LMA with extemporaneous curarization, and 22 studies reported during surgery, BIS values below 60, as under general anesthesia. There is still a lack of definition on the depth of sedation in the context of NITS, and this has resulted in the development of other terminologies we refer to, for example, awake thoracic surgery. However, it is confusing and does not allow focusing on the NITS technique in a univocal way: the expert consensus should aim to provide more information on the depth of sedation in NITS contexts.
The rate of conversion to intubation was highly variable from Nation to Nation, as it was the rate of thoracotomy. Considering the percentages reported in these articles, the average conversion rate to orotracheal intubation was about 3%. The lower rate of intubation found in China could be related to its prevalent use of the LMA. It is worth noting the unexpectedly high conversion rate observed in Germany despite the diffuse use of LMA.
Referring to outcome, we found that in 83% of cases there were no significant differences between the two cohorts, whereas in 27% NITS was proven to reduce pulmonary complications. Also, regarding the effectiveness in limiting the LOS, in 63% of cases NITS was considered more effective while 37% found no statistically significant difference between the two groups (Table 2).
When evaluating single cohort studies, pulmonary complications predominantly developed after parenchymal surgery, whereas for the LOS we did not see a clear correlation with the type of surgical procedure (Figure 4). According to Lan et al. (26) patients who underwent NITS had a higher incidence of atelectasis, pleural effusion, or pulmonary exudation in the face of a better LOS and general postoperative comorbidities compared with intubated patients. From the perspective of NITS and pulmonary complications, this issue remains controversial. In four recent meta-analyses, it is confirmed that NITS would appear to reduce the LOS, providing further validation for our analysis (62–65).
From a pain perspective, our findings were inconclusive: there was no evidence to prove the superiority of NITS in terms of postoperative pain over intubated thoracic surgery. About half of the cases had nonsignificant postoperative pain between the two groups; no regional anesthesia was performed but only sedation. Therefore, this fact might have impacted the final result. In contrast, regional anesthesia had been performed in all studies in which there was a statistically significant difference between the two groups. When evaluating postoperative pain among observational studies, although there was high heterogeneity (I2 = 96.6%) a very low score of pain at postoperative day 1 was found (Figure 5). The NITS technique, accompanied by regional anesthesia, might be a good way to reduce postoperative pain in surgery at high risk of developing persistent postoperative pain and prone to high acute postoperative pain (66, 67). Reducing opioid consumption in commonly frail patients, such as those undergoing NITS, could affect postoperative hospitalization and complication outcomes (6).
This study has limitations. The major is that it is based on mostly retrospective studies. Results therefore should always consider the low quality due to bias from retrospective studies.
Conclusion
NITS procedures are becoming increasingly popular, but they need more definition, especially the setting in which they are performed. It would be necessary, for example, to reach an agreement on the patient sedation, and airway management devices to perform NITS techniques in the same way across the countries. The choice of surgical procedure, as well as that of the patient, have not been well-defined in the literature yet. It is our opinion that frail patients have fewer complications during NITS than during intubated thoracic surgery (6). From a postoperative patient management perspective, the impact of NITS techniques on LOS remains unknown as the existing evidence available in the literature is conflicting. A regional anesthesia approach might be recommended in NITS procedures to reduce acute postoperative pain. Future studies should be directed to evaluate the benefits of NITS in patients with impaired lung function or other comorbidities (e.g., obesity, ASA III, ASA IV). Moreover, other randomized controlled trials are needed to establish more robust evidence.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
GR: conceptualization, formal analysis, investigation, methodology, project administration, supervision, validation, visualization, writing—original draft, and writing—review & editing. PL: data curation, software, visualization, writing—original draft, and writing—review & editing. EC: conceptualization, formal analysis, investigation, methodology, project administration, validation, writing—original draft, and writing—review & editing. EB and MC: data curation, formal analysis, investigation, visualization, and writing—original draft. FP: writing—original draft and writing—review & editing. ER: validiation and writing—review & editing. LB: conceptualization and writing—review & editing. FG: conceptualization, project administration, resources, methodology, supervision, validation, writing—original draft, and writing—review & editing. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.868287/full#supplementary-material
References
1. Gonzalez-Rivas D, Bonome C, Fieira E, Aymerich H, Fernandez R, Delgado M, et al. Non-intubated video-assisted thoracoscopic lung resections: the future of thoracic surgery? Eur J Cardiothorac Surg. (2016) 49:721–31. doi: 10.1093/ejcts/ezv136
2. Pompeo E, Rogliani P, Atinkaya C, Guerrera F, Ruffini E, Iñiguez-Garcia MA, et al. Nonintubated surgical biopsy of undetermined interstitial lung disease: a multicentre outcome analysis. Interact Cardiovasc Thorac Surg. (2019) 28:744–50. doi: 10.1093/icvts/ivy320
3. Cui F, Liu J, Li S, Yin W, Xin X, Shao W, et al. Tubeless video-assisted thoracoscopic surgery (VATS) under non-intubated, intravenous anesthesia with spontaneous ventilation and no placement of chest tube postoperatively. J Thorac Dis. (2016) 8:2226–32. doi: 10.21037/jtd.2016.08.02
4. He J, Liu J, Zhu C, Dai T, Cai K, Zhang Z, et al. Expert consensus on tubeless video-assisted thoracoscopic surgery (Guangzhou). J Thorac Dis. (2019) 11:4101–8. doi: 10.21037/jtd.2019.10.04
5. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169:467–73. doi: 10.7326/M18-0850
6. Guerrera F, Costardi L, Rosboch GL, Lyberis P, Ceraolo E, Solidoro P, et al. Awake or intubated surgery in diagnosis of interstitial lung diseases? A prospective study. ERJ Open Res. (2021) 7:00630–2020. doi: 10.1183/23120541.00630-2020
7. Pompeo E, Mineo TC. Awake pulmonary metastasectomy. J Thorac Cardiovasc Surg. (2007) 133:960–6. doi: 10.1016/j.jtcvs.2006.09.078
8. Pompeo E, Tacconi F, Frasca L, Mineo TC. Awake thoracoscopic bullaplasty. Eur J Cardiothorac Surg. (2011) 39:1012–7. doi: 10.1016/j.ejcts.2010.09.029
9. Pompeo E, Rogliani P, Tacconi F, Dauri M, Saltini C, Novelli G, et al. Randomized comparison of awake nonresectional versus nonawake resectional lung volume reduction surgery. J Thorac Cardiovasc Surg. (2012) 143:47–54, 54.e1. doi: 10.1016/j.jtcvs.2011.09.050
10. AlGhamdi ZM, Lynhiavu L, Moon YK, Moon MH, Ahn S, Kim Y, et al. Comparison of non-intubated versus intubated video-assisted thoracoscopic lobectomy for lung cancer. J Thorac Dis. (2018) 10:4236–43. doi: 10.21037/jtd.2018.06.163
11. Ambrogi V, Sellitri F, Perroni G, Schillaci O, Mineo TC. Uniportal video-assisted thoracic surgery colorectal lung metastasectomy in non-intubated anesthesia. J Thorac Dis. (2017) 9:254–61. doi: 10.21037/jtd.2017.02.40
12. Caviezel C, Schuepbach R, Grande B, Opitz I, Zalunardo M, Weder W, et al. Establishing a non-intubated thoracoscopic surgery programme for bilateral uniportal sympathectomy. Swiss Med Wkly. (2019) 149:w20064. doi: 10.4414/smw.2019.20064
13. Chen JS, Cheng YJ, Hung MH, Tseng YD, Chen KC, Lee YC. Nonintubated thoracoscopic lobectomy for lung cancer. Ann Surg. (2011) 254:1038–43. doi: 10.1097/SLA.0b013e31822ed19b
14. Chen J, Du Q, Lin M, Lin J, Li X, Lai F, et al. Transareolar single-port needlescopic thoracic sympathectomy under intravenous anesthesia without intubation: a randomized controlled trial. J Laparoendosc Adv Surg Tech A. (2016) 26:958–64. doi: 10.1089/lap.2015.0470
15. Chen JF, Lin M, Chen P, Quan D, Li X, Lai FC, et al. Nonintubated needlescopic thoracic sympathectomy for primary palmar hyperhidrosis: a randomized controlled trial. Surg Laparosc Endosc Percutan Tech. (2016) 26:328–33. doi: 10.1097/SLE.0000000000000287
16. Furák J, Paróczai D, Burián K, Szabó Z, Zombori T. Oncological advantage of nonintubated thoracic surgery: better compliance of adjuvant treatment after lung lobectomy. Thorac Cancer. (2020) 11:3309–16. doi: 10.1111/1759-7714.13672
17. Guo Z, Yin W, Pan H, Zhang X, Xu X, Shao W, et al. Video-assisted thoracoscopic surgery segmentectomy by non-intubated or intubated anesthesia: a comparative analysis of short-term outcome. J Thorac Dis. (2016) 8:359–68. doi: 10.21037/jtd.2016.02.50
18. Guo Z, Yin W, Zhang X, Xu X, Liu H, Shao W, et al. Primary spontaneous pneumothorax: simultaneous treatment by bilateral non-intubated videothoracoscopy. Interact Cardiovasc Thorac Surg. (2016) 23:196–201. doi: 10.1093/icvts/ivw123
19. Hsiao CH, Chen KC, Chen JS. Modified single-port non-intubated video-assisted thoracoscopic decortication in high-risk parapneumonic empyema patients. Surg Endosc. (2017) 31:1719–27. doi: 10.1007/s00464-016-5164-7
20. Huang W, Deng H, Lan Y, Wang R, Ge F, Huo Z, et al. Spontaneous ventilation video-assisted thoracic surgery for mediastinal tumor resection in patients with pulmonary function deficiency. Ann Transl Med. (2020) 8:1444. doi: 10.21037/atm-20-1652
21. Hwang J, Shin JS, Son JH, Min TJ. Non-intubated thoracoscopic bullectomy under sedation is safe and comfortable in the perioperative period. J Thorac Dis. (2018) 10:1703–10. doi: 10.21037/jtd.2018.02.10
22. Irons JF, Miles LF, Joshi KR, Klein AA, Scarci M, Solli P, et al. Intubated versus nonintubated general anesthesia for video-assisted thoracoscopic surgery-a case-control study. J Cardiothorac Vasc Anesth. (2017) 31:411–7. doi: 10.1053/j.jvca.2016.07.003
23. Jung J, Kim DH, Son J, Lee SK, Son BS. Comparative study between local anesthesia and general anesthesia in the treatment of primary spontaneous pneumothorax. Ann Transl Med. (2019) 7:553. doi: 10.21037/atm.2019.09.89
24. Ke HH, Hsu PK, Tsou MY, Ting CK. Nonintubated video-assisted thoracic surgery with high-flow oxygen therapy shorten hospital stay. J Chin Med Assoc. (2020) 83:943–9. doi: 10.1097/JCMA.0000000000000408
25. Kocatürk C, Kutluk AC, Usluer O, Onat S, Çinar HU, Yanik F, et al. Comparison of awake and intubated video-assisted thoracoscopic surgery in the diagnosis of pleural diseases: a prospective multicenter randomized trial. Turk Gogus Kalp Damar Cerrahisi Derg. (2019) 27:550–6. doi: 10.5606/tgkdc.dergisi.2019.18214
26. Lan L, Cen Y, Zhang C, Qiu Y, Ouyang B. A propensity score-matched analysis for non-intubated thoracic surgery. Med Sci Monit. (2018) 24:8081–7. doi: 10.12659/MSM.910605
27. Liang H, Liu J, Wu S, Zhang Y, Liu H, Yang H, et al. Nonintubated spontaneous ventilation offers better short-term outcome for mediastinal tumor surgery. Ann Thorac Surg. (2019) 108:1045–51. doi: 10.1016/j.athoracsur.2019.04.052
28. Liu HY, Hsu HH, Tsai TM, Chiang XH, Lu TP, Chang CH, et al. Nonintubated versus intubated uniportal thoracoscopic segmentectomy for lung tumors. Ann Thorac Surg. (2021) 111:1182–9. doi: 10.1016/j.athoracsur.2020.06.058
29. Liu J, Cui F, Li S, Chen H, Shao W, Liang L, et al. Nonintubated video-assisted thoracoscopic surgery under epidural anesthesia compared with conventional anesthetic option: a randomized control study. Surg Innov. (2015) 22:123–30. doi: 10.1177/1553350614531662
30. Liu J, Cui F, Pompeo E, Gonzalez-Rivas D, Chen H, Yin W, et al. The impact of non-intubated versus intubated anaesthesia on early outcomes of video-assisted thoracoscopic anatomical resection in non-small-cell lung cancer: a propensity score matching analysis. Eur J Cardiothorac Surg. (2016) 50:920–5. doi: 10.1093/ejcts/ezw160
31. Liu Z, Yang R, Sun Y. Nonintubated uniportal thoracoscopic thymectomy with laryngeal mask. Thorac Cardiovasc Surg. (2020) 68:450–6. doi: 10.1055/s-0039-1696950
32. Mao Y, Liang H, Deng S, Qiu Y, Zhou Y, Chen H, et al. Non-intubated video-assisted thoracic surgery for subxiphoid anterior mediastinal tumor resection. Ann Transl Med. (2021) 9:403. doi: 10.21037/atm-20-6125
33. Metelmann I, Broschewitz J, Pietsch UC, Huschak G, Eichfeld U, Bercker S, et al. Procedural times in early non-intubated VATS program - a propensity score analysis. BMC Anesthesiol. (2021) 21:44. doi: 10.1186/s12871-021-01270-4
34. Mineo TC, Sellitri F, Tacconi F, Ambrogi V. Quality of life and outcomes after nonintubated versus intubated video-thoracoscopic pleurodesis for malignant pleural effusion: comparison by a case-matched study. J Palliat Med. (2014) 17:761–8. doi: 10.1089/jpm.2013.0617
35. Wang ML, How CH, Hung MH, Huang HH, Hsu HH, Cheng YJ, et al. Long-term outcomes after nonintubated versus intubated thoracoscopic lobectomy for clinical stage I non-small cell lung cancer: a propensity-matched analysis. J Formos Med Assoc. (2021) 120:1949–56. doi: 10.1016/j.jfma.2021.04.018
36. Akopov A, Egorov V, Deynega I, Ionov P. Awake video-assisted thoracic surgery in acute infectious pulmonary destruction. Ann Transl Med. (2015) 3:100. doi: 10.3978/j.issn.2305-5839.2015.04.16
37. Ambrogi MC, Fanucchi O, Korasidis S, Davini F, Gemignani R, Guarracino F, et al. Nonintubated thoracoscopic pulmonary nodule resection under spontaneous breathing anesthesia with laryngeal mask. Innovations. (2014) 9:276–80. doi: 10.1097/imi.0000000000000075
38. Chen J, Lin J, Tu Y, Lin M, Li X, Lai F. Nonintubated transareolar endoscopic thoracic sympathectomy with a flexible endoscope: experience of 58 cases. Ann Thorac Cardiovasc Surg. (2016) 22:12–9. doi: 10.5761/atcs.oa.15-00241
39. Chen JF, Lin JB, Tu YR, Lin M, Li X, Lai FC, et al. Nonintubated transareolar single-port thoracic sympathicotomy with a needle scope in a series of 85 male patients. Surg Endosc. (2016) 30:3447–53. doi: 10.1007/s00464-015-4628-5
40. Chen KC, Cheng YJ, Hung MH, Tseng YD, Chen JS. Nonintubated thoracoscopic surgery using regional anesthesia and vagal block and targeted sedation. J Thorac Dis. (2014) 6:31–6. doi: 10.1097/00003643-201406001-00238
41. Cherchi R, Grimaldi G, Pinna-Susnik M, Riva L, Sarais S, Santoru M, et al. Retrospective outcomes analysis of 99 consecutive uniportal awake lung biopsies: a real standard of care? J Thorac Dis. (2020) 12:4717–30. doi: 10.21037/jtd-20-1551
42. Hung MH, Chan KC, Liu YJ, Hsu HH, Chen KC, Cheng YJ, et al. Nonintubated thoracoscopic lobectomy for lung cancer using epidural anesthesia and intercostal blockade: a retrospective cohort study of 238 cases. Medicine. (2015) 94:e727. doi: 10.1097/MD.0000000000000727
43. Hung MH, Cheng YJ, Chan KC, Han SC, Chen KC, Hsu HH, et al. Nonintubated uniportal thoracoscopic surgery for peripheral lung nodules. Ann Thorac Surg. (2014) 98:1998–2003. doi: 10.1016/j.athoracsur.2014.07.036
44. Hung MH, Hsu HH, Chan KC, Chen KC, Yie JC, Cheng YJ, et al. Non-intubated thoracoscopic surgery using internal intercostal nerve block, vagal block and targeted sedation. Eur J Cardiothorac Surg. (2014) 46:620–5. doi: 10.1093/ejcts/ezu054
45. Hung MH, Hsu HH, Chen KC, Chan KC, Cheng YJ, Chen JS. Nonintubated thoracoscopic anatomical segmentectomy for lung tumors. Ann Thorac Surg. (2013) 96:1209–15. doi: 10.1016/j.athoracsur.2013.05.065
46. Hung WT, Hung MH, Wang ML, Cheng YJ, Hsu HH, Chen JS. Nonintubated thoracoscopic surgery for lung tumor: seven years' experience with 1,025 patients. Ann Thorac Surg. (2019) 107:1607–12. doi: 10.1016/j.athoracsur.2019.01.013
47. Li H, Huang D, Qiao K, Wang Z, Xu S. Feasibility of non-intubated anesthesia and regional block for thoracoscopic surgery under spontaneous respiration: a prospective cohort study. Braz J Med Biol Res. (2020) 53:e8645. doi: 10.1590/1414-431x20198645
48. Liu CY, Hsu PK, Chien HC, Hsieh CC, Ting CK, Tsou MY. Tubeless single-port thoracoscopic sublobar resection: indication and safety. J Thorac Dis. (2018) 10:3729–37. doi: 10.21037/jtd.2018.05.119
49. Liu HY, Chiang XH, Hung MH, Wang ML, Lin MW, Cheng YJ, et al. Nonintubated uniportal thoracoscopic segmentectomy for lung cancer. J Formos Med Assoc. (2020) 119:1396–404. doi: 10.1016/j.jfma.2020.03.021
50. Liu Z, Yang R, Sun Y. Tubeless uniportal thoracoscopic wedge resection with modified air leak test and chest tube drainage. BMC Surg. (2020) 20:301. doi: 10.1186/s12893-020-00910-9
51. Moon Y, AlGhamdi ZM, Jeon J, Hwang W, Kim Y, Sung SW. Non-intubated thoracoscopic surgery: initial experience at a single center. J Thorac Dis. (2018) 10:3490–8. doi: 10.21037/jtd.2018.05.147
52. Starke H, Zinne N, Leffler A, Zardo P, Karsten J. Developing a minimally-invasive anaesthesiological approach to non-intubated uniportal video-assisted thoracoscopic surgery in minor and major thoracic surgery. J Thorac Dis. (2020) 12:7202–17. doi: 10.21037/jtd-20-2122
53. Tseng YD, Cheng YJ, Hung MH, Chen KC, Chen JS. Nonintubated needlescopic video-assisted thoracic surgery for management of peripheral lung nodules. Ann Thorac Surg. (2012) 93:1049–54. doi: 10.1016/j.athoracsur.2012.01.062
54. Wang ML, Galvez C, Chen JS, Navarro-Martinez J, Bolufer S, Hung MH, et al. Non-intubated single-incision video-assisted thoracic surgery: a two-center cohort of 188 patients. J Thorac Dis. (2017) 9:2587–98. doi: 10.21037/jtd.2017.08.96
55. Wang ML, Hung MH, Chen JS, Hsu HH, Cheng YJ. Nasal high-flow oxygen therapy improves arterial oxygenation during one-lung ventilation in non-intubated thoracoscopic surgery. Eur J Cardiothorac Surg. (2018) 53:1001–6. doi: 10.1093/ejcts/ezx450
56. Pompeo E, Sorge R, Akopov A, Congregado M, Grodzki T. Non-intubated thoracic surgery-a survey from the European Society of Thoracic Surgeons. Ann Transl Med. (2015) 3:37. doi: 10.3978/j.issn.2305-5839.2015.01.34
57. Al-Shather H, El-Boghdadly K, Pawa A. Awake laparoscopic sleeve gastrectomy under paravertebral and superficial cervical plexus blockade. Anaesthesia. (2015) 70:1210–1. doi: 10.1111/anae.13220
58. Kanawati S, Fawal H, Maaliki H, Naja ZM. Laparoscopic sleeve gastrectomy in five awake obese patients using paravertebral and superficial cervical plexus blockade. Anaesthesia. (2015) 70:993–5. doi: 10.1111/anae.13037
59. Rosboch GL, Ceraolo E, Balzani E, Piccioni F, Brazzi L. The anesthesiologist perspective. Video-Assisted Thoracic Surgery. (2021) 6. doi: 10.21037/vats-21-2
60. Bedetti B, Patrini D, Bertolaccini L, Crisci R, Solli P, Schmidt J, et al. Uniportal non-intubated thoracic surgery. J Vis Surg. (2018) 4:18. doi: 10.21037/jovs.2017.12.09
61. Du X, Mao S, Cui J, Ma J, Zhang G, Zheng Y, et al. Use of laryngeal mask airway for non-endotracheal intubated anesthesia for patients with pectus excavatum undergoing thoracoscopic nuss procedure. J Thorac Dis. (2016) 8:2061–7. doi: 10.21037/jtd.2016.07.52
62. Deng HY, Zhu ZJ, Wang YC, Wang WP, Ni PZ, Chen LQ. Non-intubated video-assisted thoracoscopic surgery under loco-regional anaesthesia for thoracic surgery: a meta-analysis. Interact Cardiovasc Thorac Surg. (2016) 23:31–40. doi: 10.1093/icvts/ivw055
63. Yu MG, Jing R, Mo YJ, Lin F, Du XK, Ge WY, et al. Non-intubated anesthesia in patients undergoing video-assisted thoracoscopic surgery: a systematic review and meta-analysis. PLoS ONE. (2019) 14:e0224737. doi: 10.1371/journal.pone.0224737
64. Xue W, Duan G, Zhang X, Zhang H, Zhao Q, Xin Z, et al. Comparison of non-intubated and intubated video-assisted thoracoscopic surgeries of major pulmonary resections for lung cancer-a meta-analysis. World J Surg Oncol. (2021) 19:87. doi: 10.1186/s12957-021-02181-x
65. Zhang K, Chen H-G, Wu W-B, Li X-J, Wu Y-H, Xu J-N, et al. Non-intubated video-assisted thoracoscopic surgery vs. intubated video-assisted thoracoscopic surgery for thoracic disease: a systematic review and meta-analysis of 1,684 cases. J Thorac Dis. (2019) 11:3556–68. doi: 10.21037/jtd.2019.07.48
66. Gerbershagen HJ, Aduckathil S, van Wijck AJ, Peelen LM, Kalkman CJ, Meissner W. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology. (2013) 118:934–44. doi: 10.1097/ALN.0b013e31828866b3
Keywords: non-intubated thoracic surgery, anesthesia, NITS, VATS, thoracic surgery, regional anesthesia
Citation: Rosboch GL, Lyberis P, Ceraolo E, Balzani E, Cedrone M, Piccioni F, Ruffini E, Brazzi L and Guerrera F (2022) The Anesthesiologist's Perspective Regarding Non-intubated Thoracic Surgery: A Scoping Review. Front. Surg. 9:868287. doi: 10.3389/fsurg.2022.868287
Received: 02 February 2022; Accepted: 24 February 2022;
Published: 04 April 2022.
Edited by:
Davide Tosi, IRCCS Ca' Granda Foundation Maggiore Policlinico Hospital, ItalyReviewed by:
Alberto Sandri, San Luigi Gonzaga Hospital, ItalyPatrick Zardo, Hannover Medical School, Germany
Copyright © 2022 Rosboch, Lyberis, Ceraolo, Balzani, Cedrone, Piccioni, Ruffini, Brazzi and Guerrera. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Giulio Luca Rosboch, Z2l1bGlvcm9zYm9jaEBnbWFpbC5jb20=
 Giulio Luca Rosboch
Giulio Luca Rosboch Paraskevas Lyberis2
Paraskevas Lyberis2 Eleonora Balzani
Eleonora Balzani