- 1Department of Orthopedics, No. 2 Hospital of Baoding, Chengde Medical University, Baoding, China
- 2Department of Bone and Joint, First Affiliated Hospital, Dalian Medical University, Dalian, China
- 3Emergency Center, First Central Hospital of Baoding, Baoding, China
Purpose: We designed a J-shaped external fixator (J-EF) to provide a minimally invasive, one-step surgical method for olecranon fractures. The aim of this study is to retrospectively review the method and the outcomes in 14 patients treated with J-EF fixation.
Methods: Biomechanical comparative study was performed to test the tensile properties of the J-EF using a universal testing machine. Between January 2002 and December 2005, 14 patients (age range: 25–67 years) with Mayo type II olecranon fractures were treated using the external fixation technique. Follow-up was done by standard measures (radiography, range of motion, and complications monitoring) and patient-reported outcomes (Mayo Elbow Performance Score [MEPS] and Disabilities of the Arm, Shoulder, and Hand [DASH] scores) 6 months after surgery. Eight of the patients were reviewed 15 years after the surgery.
Results: Results from biomechanical studies indicate the non-inferiority of J-EF to tension-band wiring (TBW) in tensile properties. At the time of release, the mean elbow flexion arc was 132.5° and the mean forearm rotation arc was 173.6°. The mean DASH score was 14.1 points, and the mean MEPS was 93.9 points. Operative time and intraoperative blood loss were decreased by 41.3% and 64.6%, respectively, in J-EF patients than those in a comparable group treated by TBW. All eight patients are still alive after the surgery and maintaining the original outcome.
Conclusions: External fixation using the J-EF could be considered as an alternative treatment for Mayo type II olecranon fractures as it appears to be a reliable, minimally invasive, and time-saving.
Level of Evidence: Therapeutic Level IV.
Introduction
Olecranon fractures are common injuries, accounting for approximately 20% of fractures of the proximal forearm in adults (1, 2). The mechanism of injury is usually a forceful contraction of the triceps during a fall on the outstretched hand, the humerus acting as a splitting wedge (3, 4). Although some patients can be managed nonoperatively, surgical fixation is usually necessary for displaced fractures (5, 6). Indications for surgical fixation include extensor mechanism weakness, intra-articular displacement, and instability of the humeroulnar joint (7, 8). The most commonly used surgical techniques for the treatment of olecranon fractures are tension-band wiring (TBW) fixation and plate fixation (PF). However, these techniques comes with some complications such as soft tissue injury due to the surgical exposure, postoperative discomfort of elbow due to prominence of metal work and the complications associated with removal of the hardware (9–11). To provide a simple, less invasive treatment option, we designed a J-shaped external fixator (J-EF) to treat Mayo type II olecranon fractures. With patent and license for clinical use, we applied the J-EF to treat 14 patients with Mayo type II olecranon fractures. The aim of this study is to introduce our experience with the use of the J-EF and report the long-term outcomes of patients.
Materials and Methods
Design and Structure of the J-Shaped External Fixator
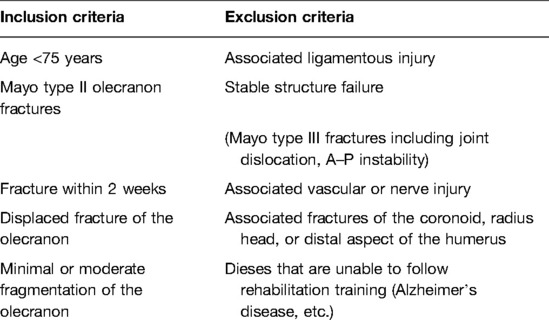
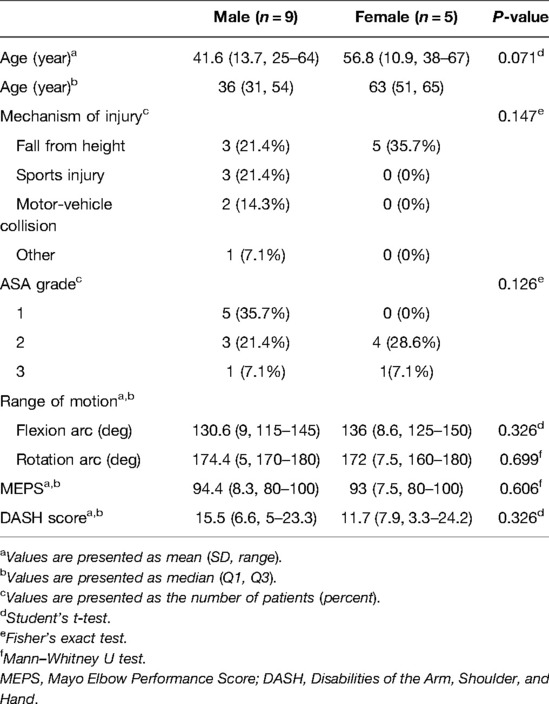
The design of J-EF was based on our previous anatomical study of olecranon from Asian adult cadavers for improved understanding of the anatomical structure of olecranon and for making our design compatible with the anatomical morphology of olecranon. The fixator was 4 × 120 × 14 mm in size, with a groove of 70 × 5 mm in the middle and two semielliptical hooks with 5 mm in between placed at the proximal part of the fixator, and the radian (R) of the hook was 15–20 mm. A longitudinal compression rod was equipped at the distal part of the fixator, which provided a longitudinal compression force and constituted the compression system together with the hooks and cortical screws (Figure 1A–C). The compression system works with the rotation of the pressurized rod in a clockwise manner to drive the fixator downward, therefore producing a compression force on the fracture site from the hooks (Figure 1D).
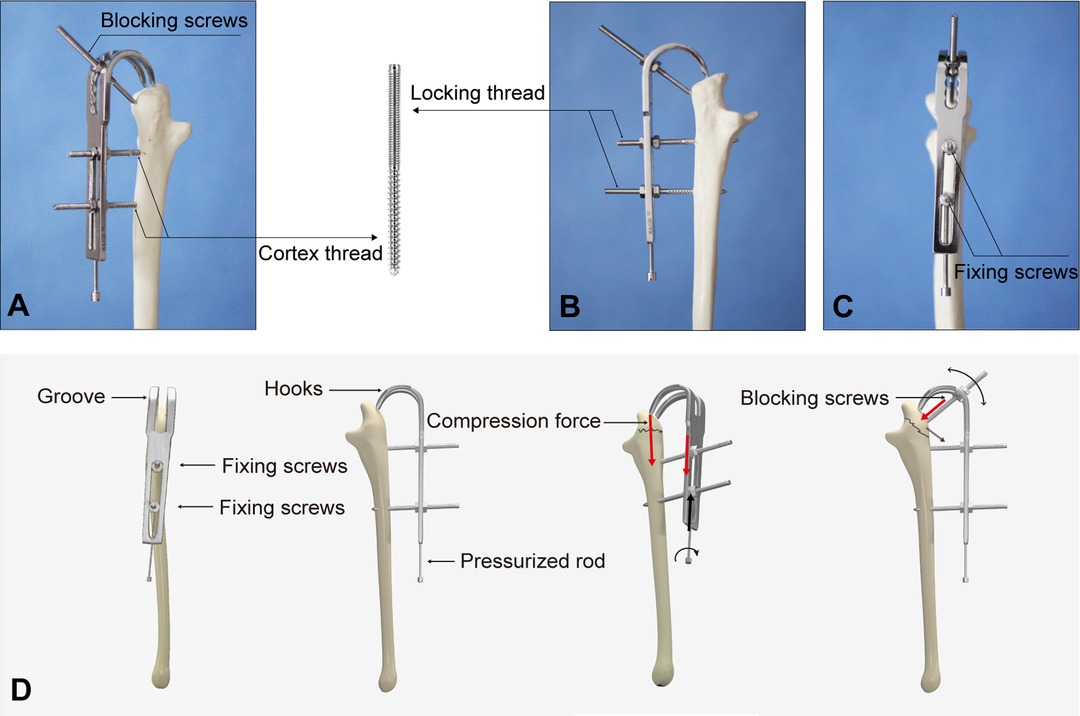
Figure 1. Structure of the J-shaped external fixator (J-EF). General view of the J-EF (A–C). Structure and the compression system of J-EF (D).
We designed the upper part of the fixing screw with the locking screw body, while the lower part with the cortical screw body; so as the screws could be firmly fixed to the body of the fixator through locking threads to achieve a rigid fixation to the proximal ulna from the cortical threads (Figure 1A–C). All the screws were 60 mm in length and 4 mm in diameter. The screws performed two functions in the current study: lower screws served as “fixing screws” to provide firm fixation of the fixator and proximal ulna, and the upper screws around the hook were “blocking screws” to prevent displacement of the fracture fragments (Figure 1D).
Mechanical Performance Evaluation of the J-EF
By taking TBW as a control, biomechanical comparative studies were performed using six pairs of fresh-frozen cadaveric specimens with approval from the ethics committee of Hebei Medical University. The average age of specimens was 42.33 (range: 29–63) years. Fresh cadavers were divided into two groups (n = 6). The models of olecranon fractures were made in each group based on Mayo type II. The fractures were fixed using J-EF in the treatment group and TBW in the control group. The mechanical testing of the tensile strength was performed by a universal testing machine (Institute of Traumatology and Biomechanics, KEYI Med. Ltd., Beijing). The mechanical test was conducted in cyclic loading mode under 50–500 N loading at an amplitude of 225 N and frequency of 1 Hz. The test was run for 500 cycles, and the displacement of the fracture site was recorded by a reluctance transducer at 300 and 500 cycles, respectively. A static tensile strength test was performed with a loading speed of 10 mm/min, and fixation failure was defined as the displacement of the fracture site greater than 2 mm.
Study Population
Between January 2002 and December 2005, we used the J-EF for the treatment of 14 patients with Mayo type II olecranon fracture. Table 1 lists the inclusion and exclusion criteria for the selection of patients. The mean operation time and intraoperative blood loss were compared with those of patients treated with TBW by the same group of doctors. Radiography was performed to assess the process of fracture healing. Improvement in range of motion, complications, and patient-reported outcome (Mayo Elbow Performance Score [MEPS] and Disabilities of the Arm, Shoulder, and Hand [DASH] scores) were recorded 6 months after surgery. Our study was conducted after obtaining the approval from the ethics committee and all patients were provided with informed consent before the surgery.
Surgical Technique
Fixing screws were driven into the ulnar shaft to ensure the stability of the distal part during reduction. Closed reduction was then performed under fluoroscopy, with the assistance of Kirschner wires if needed. The elbow was gradually flexed to 90°, and two 5 mm incisions were made over the dorsal part of the olecranon process for insertion of the hooks of J-EF. The olecranon fixing screws were subsequently assembled with the fixator. Restoration of the articular surface was monitored radiologically as the fracture site was pressurized with the compression system of J-EF. The reduction was considered satisfactory if the step-off or gap of the articular surface was less than 1 mm.
Postoperative Management and Outcome Assessment
Passive and active flexions (up to 90°) were initiated 2 days after the surgery. Unlimited flexion, pronation, and supination were initiated two weeks after surgery. Weight-bearing was not allowed until 2 months after surgery or until the removal of the external fixator. All patients were reviewed every two weeks after surgery. X-rays were obtained 8 weeks and 12 weeks postoperatively to confirm radiological healing. The J-EF was not removed until the fractures shown a gradual loss in fracture line on radiology. Infection, nonunion, deformity healing, postoperative pain, and elbow dysfunction were recorded as the adverse event. Clinical and functional evaluations were performed 6 months after surgery. Joint function was evaluated by the MEPS and DASH scores.
Statistical Analysis
Continuous variables were summarized as means ± standard deviation, and categorical variables were summarized as absolute and relative frequency. Statistical analysis was performed using SPSS 22.0 (IBM Corp., Armonk, NY, USA). P < 0.05 was considered statistically significant.
Results
Structure of the J-Shaped External Fixator
The fixator was 4 × 120 × 14 mm in size, with a groove of 70 × 5 mm in the middle and two semielliptical hooks with 5 mm in between placed at the proximal part of the fixator, and the radian (R) of the hook was 15–20 mm. A longitudinal compression rod was equipped at the distal part of the fixator, which provided a longitudinal compression force and constituted the compression system together with the hooks and cortical screws (Figure 1A–C). The compression system works with the rotation of the pressurized rod in a clockwise manner to drive the fixator downward, therefore producing a compression force on the fracture site from the hooks (Figure 1D).
We designed the upper part of the fixing screw with the locking screw body while the lower part with the cortical screw body; thus, the screws could be firmly fixed to the body of the fixator through locking threads to achieve a rigid fixation to the proximal ulna from the cortical threads (Figure 1A–C). All the screws were 60 mm in length and 4 mm in diameter. The screws performed two functions in the current study: lower screws served as “fixing screws” to provide firm fixation of the fixator and proximal ulna, and the upper screws around the hook were “blocking screws” to prevent displacement of the fracture fragments (Figure 1D).
Biomechanical Properties of J-EF
Shown as the comparative biomechanical data in Figure 2, the tensile strength of the J-EF group with a mean displacement of 1.1 mm (0.15 mm; range: 0.9–1.28 mm) was greater than that of the TBW group with a mean displacement of 1.52 mm (0.16 mm; range: 1.32–1.75 mm) after running 600 cycles (P < 0.05). Similar significant differences (t = −5.666, P = 0) were found in the static tensile loading test between TBW and J-EF, which was 1,113.17 N (83.4 N; range: 997–1,214 N) and 1,369.83 N (73.19 N; range: 1,266–1,484 N), respectively. The difference between the two groups was analyzed by Student’s t-test. The comparative results indicate the noninferiority of J-EF to TBW in biomechanical properties and provide a biomechanical precondition for the clinical application of J-EF.
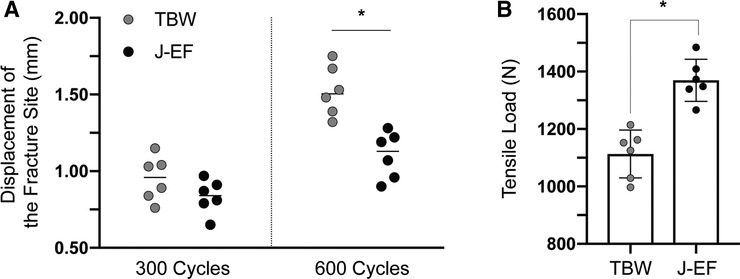
Figure 2. Biomechanical properties of J-EF. Tensile strength of J-EF was tested using tension-band wiring (TBW) as the control. The tensile strength of the J-EF group was greater than that of the TBW group after running 600 cycles (P < 0.05). Similar results were found in the static tensile loading test between TBW and J-EF. The difference between the two groups was analyzed by Student’s t-test.
Patients
The 14 patients (nine males; 64.3%) recruited for our study had a mean age of 47 ± 14.7 (range: 25–67) years. The fracture was on the left side in 11 (78.6%) patients (Table 2). Four (28.6%) patients had Mayo IIB fractures, and ten (71.4%) had Mayo IIA fractures. The most frequent mechanism of injury was falling from height (n = 8, 57.1%), followed by sports injury (n = 3, 21.4%) and traffic accident (n = 2, 14.3%); the remaining patient is a swimmer and injured during training practice. Nine (64.3%) patients had documented comorbidities. The American Society of Anesthesiologists (ASA) grade was not significantly different between male and female patients (P = 0.126).
Operative Time and Intraoperative Blood Loss
For better evaluation of the clinical application of J-EF, we performed statistical analysis on the perioperative clinical data, including operative time and intraoperative blood loss; data were compared with TBW treatment. As shown in Figure 3, the mean operative time was 38 ± 9.6 (range: 23–62) min, which was lower than the mean operative time in a comparable group of patients treated by TBW at our hospital during the same period (64.7 ± 10.4 [range: 48–85] min); the difference was statistically significant (t = 6.79, P < 0.001). Similarly, the mean intraoperative blood loss of the J-EF group was 16.4 ml (range: 5–35 ml; SD: 8.5 ml), which was significantly less (t = 6.01, P < 0.001) than that of the TBW group (mean: 46.4 ml; range: 30–80 ml; SD: 15.9 ml). For accurate measurements, the intraoperative blood loss was calculated according to the suction device; therefore, the true volume of blood loss was less than this amount. According to our experience, intraoperative blood loss using J-EF should be less than 5 ml; therefore, tourniquets are not necessary when using J-EF treatment for most cases. With less blood loss and shorter operation time, J-EF makes the treatment of olecranon fractures more in line with the requirements of ambulatory surgery.
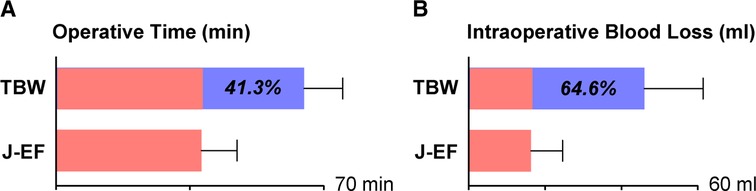
Figure 3. Comparative study of perioperative clinical data between TBW and J-EF treatment. A comparative study of perioperative data including operative time (A) and intraoperative blood loss (B) between J-EF and TBW was performed according to the anesthesia sheets and suction device; the percentage represents the reduction in the J-EF group relative to the TBW group.
Clinical Outcome and Long-Term Review
At 6 months after surgery, the mean elbow flexion arc of patients treated with the J-EF was 132.5° ± 9.2° (range: 115°–150°) and the mean forearm rotation arc was 173.6° ± 6.1° (range: 160°–180°). The mean DASH score was 14.1 ± 7.3 (range: 3.3–24.2) points, and the mean MEPS was 94 ± 8.1 (range: 80–100) points (Table 2). Range of motion and the MEPS and DASH scores were not significantly different between male and female patients (all P > 0.05; Table 2). The mean time to removal of J-EF was 67.1 ± 13.2 (range: 45–97) days. One patient complained of mild intermittent pain in the elbow 2 weeks after surgery, but the pain was relieved after the removal of the fixator with the healing of the fracture. No patient had significant complications including nonunion, malunion, and infection during our 1-year follow-up after surgery. Preoperative and postoperative X-rays of our typical cases are shown in Figure 4.
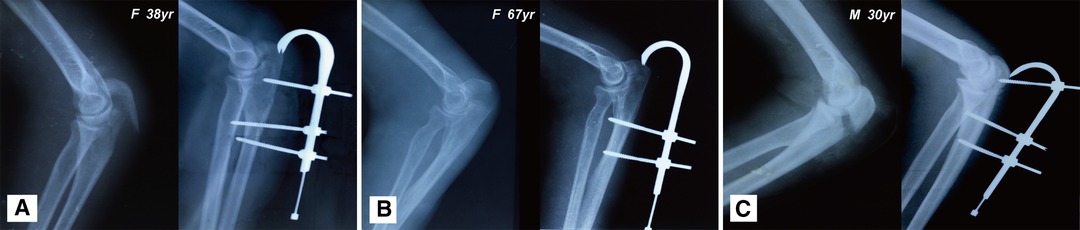
Figure 4. Preoperative and postoperative X-rays of the elbow joint. Typical cases treatment with J-EF in our study. (A) Female patient of 38 years, car accident; (B) female patient of 67 years, fall from height; and (C) male patient of 30 years, sports injury.
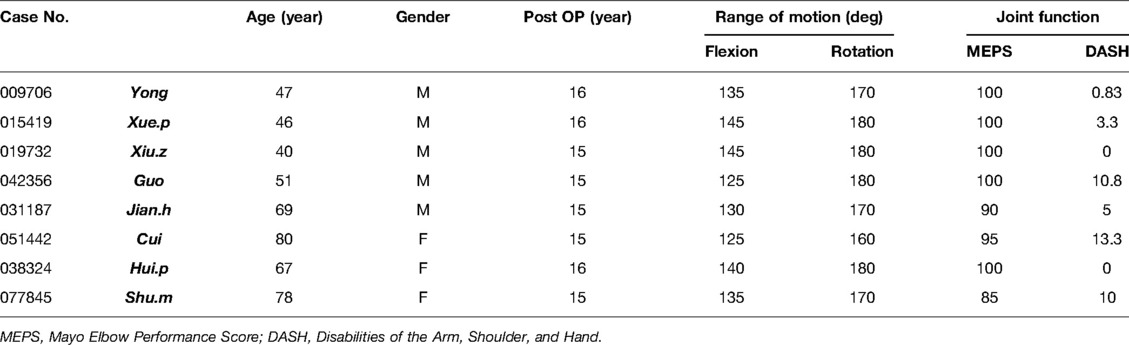
We reviewed and followed up our first group of patients underwent J-EF treatment, who were more than 15 years after surgery, X-rays and the follow-up of typical case was shown in Supplemental Figure 1. Unfortunately, among the first group of 14 patients, we could only be able to follow-up eight patients; the other six patients were lost due to death of natural causes. With a follow-up of the eight patients, all patients achieved a good elbow joint function score, and no complaint of pain or limited range of motion of the elbow was noticed (Table 3).
Discussion
For olecranon fracture, which accounts for approximately 8%–10% of all elbow fractures, the surgical goals are to restore articular integrality, provide stable, reliable fixation and minimize joint stiffness via early mobilization. Typically, most displaced olecranon fractures are managed with open reduction and fixation. TBW is a commonly used surgical fixation technique (12); the prominence of metalwork and soft tissue complications are major concerns and the rates of TBW removal are high (13–16), the external fixator that we used was designed to avoid these problems. The mechanical study has shown that the tensile strength of J-EF is reliable and not inferior to that of TBW. The efficacy of J-EF is attributable to the firm hold of the fracture site achieved via hooks and screws. The fracture is also stabilized by the compression force. Meanwhile, TBW acts like an indirect strapping of the fracture because of the coverage by fascial tissue and the triceps brachii tendon. Due to the elastic mechanical property of TBW, there is a possibility of loosening during postoperative joint activities. Thus, J-EF provides a more reliable fixation for the fracture. Furthermore, we have found that compression adjustment is easily performed through the pressurized rod within 48 h post-surgery if postoperative radiography does not show a satisfactory reduction.
C-arm fluoroscopy was used to ensure anatomical reduction. Rehab activities including gravity-assisted elbow flexion exercises could be initiated within 48 h after surgery because of the absence of plaster immobilization. The time to remove the fixator was 45–97 days. All our cases met the standard of clinical healing with no reports of nonunion, delayed healing, or refracture during the follow-up period. The minimally invasive reduction—with preservation of the periosteum and the subdermal vascular network—can be especially advantageous for professional athletes (12). By way of example, one high-quality athlete in our study, a 13-year-old male diver, underwent J-EF fixation. Elbow function recovered without malunion in 6 months, and no symptoms of traumatic arthritis were found during the long-term follow-up. Besides the case series represented in our study, we also treated a small number of Mayo type IIIa fractures with J-EF fixation and achieved good results. Although open reduction fixation is not the purpose of designing J-EF, minimal incision at the fracture site will be helpful and necessary for the reduction of Mayo type IIIa fractures, according to our experience. However, it must be noted that this technique may not be applicable to highly unstable fractures (for example, Mayo type IIIb); for such patients, we still recommend open reduction and plate fixation (15, 17). Due to limitations on the number of cases, we did not find a significant difference in clinical outcomes of using J-EF between Mayo type IIa and IIb fractures in our present study. Hopefully, we could perform a comparative study on the treatment outcome of J-EF treatment between different types of fractures in our further study. With a relatively small number of included cases, however, this study is limited by the need for sufficient patients to support the feasibility of the study. We are also trying to carry out the dynamic biomechanical study of J-EF after implantation using medical computer technology (18). If possible, we will also use medical imaging and computer technology to conduct a surgical simulation of J-EF treatment for olecranon fractures.
Conclusions
To sum up, being simple to use, less invasive, and providing early rehabilitation, the J-EF may become a reliable treatment option for Mayo type II olecranon fractures.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material; further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committees of Hebei Medical University. Written informed consent to participate in this study was provided by the participant’s legal guardian/next of kin.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
All authors participated in the design of the J-shaped external fixator (J-EF) and postoperative follow-up of patients. YT was the main designer. KT, FS, WZ, and JL improved the design of the J-EF from the anatomical perspective. CtcwC, JZ and CG participated in the writing of the article. All authors contributed to the article and approved the submitted version.
Funding
This work is supported by the National Natural Science Foundation of China (No. 81601901) and the Natural Science Foundation of Liaoning, China (No. 2019-MS-079).
Acknowledgments
The authors thank Mrs. Ruixian Zhang for her years of assistance during our proceeding of study. Although we could not list all the team members as co-authors in the manuscript, we thank our team members Mengqiang Tian, Weidong Yuan, Zongpi Sun, Hongyan Yang, Yongming Yang, Xiaolin Shi, and Fengqin Gou for their valuable contribution and hard work in the past 30 years.
Supplementary Material
The Supplementary Material for this article can be found online at: https://journal.frontiersin.org/article/10.3389/fsurg.2022.855600/full#supplementary-material.
Supplementary Figure 1 | Typical case of Mayo type IIa olecranon fracture treated with J-EF fixation. Male patient, 30 years, traffic accident. Preoperative (A) and postoperative X-rays of the elbow joint were shown in A-D. The elbow joint function 3 months postsurgery (E-G) as well as 16 years follow-up (H-J) of the patient were shown in the supplementary data.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rommens PM, Kuchle R, Schneider RU, Reuter M. Olecranon fractures in adults: factors influencing outcome. Injury. (2004) 35(11):1149–57. doi: 10.1016/j.injury.2003.12.002
2. Duckworth AD, Clement ND, Aitken SA, Court-Brown CM, McQueen MM. The epidemiology of fractures of the proximal ulna. Injury. (2012) 43(3):343–6. doi: 10.1016/j.injury.2011.10.017
3. Furushima K, Itoh Y, Iwabu S, Yamamoto Y, Koga R, Shimizu M. Classification of olecranon stress fractures in baseball players. Am J Sports Med. (2014) 42(6):1343–51. doi: 10.1177/0363546514528099
4. Wiegand L, Bernstein J, Ahn J. Fractures in brief: olecranon fractures. Clin Orthop Relat Res. (2012) 470(12):3637–41. doi: 10.1007/s11999-012-2393-5
5. Bailey CS, MacDermid J, Patterson SD, King GJ. Outcome of plate fixation of olecranon fractures. J Orthop Trauma. (2001) 15(8):542–8. doi: 10.1097/00005131-200111000-00002
6. Cain EL Jr., Dugas JR, Wolf RS, Andrews JR. Elbow injuries in throwing athletes: a current concepts review. Am J Sports Med. (2003) 31(4):621–635. doi: 10.1177/03635465030310042601
7. Rettig AC, Wurth TR, Mieling P. Nonunion of olecranon stress fractures in adolescent baseball pitchers: a case series of 5 athletes. Am J Sports Med. (2006) 34(4):653–6. doi: 10.1177/0363546505281802
8. Stephenson DR, Love S, Garcia GG, Mair SD. Recurrence of an olecranon stress fracture in an elite pitcher after percutaneous internal fixation: a case report. Am J Sports Med. (2012) 40(1):218–21. doi: 10.1177/0363546511422796
9. Brolin TJ, Throckmorton T. Olecranon fractures. Hand Clin. (2015) 31(4):581–90. doi: 10.1016/j.hcl.2015.07.003
10. Buijze G, Kloen P. Clinical evaluation of locking compression plate fixation for comminuted olecranon fractures. J Bone Joint Surg Am. (2009) 91(10):2416–20. doi: 10.2106/JBJS.H.01419
11. Edwards SG, Martin BD, Fu RH, Gill JM, Nezhad MK, Orr JA, et al. Comparison of olecranon plate fixation in osteoporotic bone: do current technologies and designs make a difference? J Orthop Trauma. (2011) 25(5):306–11. doi: 10.1097/BOT.0b013e3181f22465
12. Ren YM, Qiao HY, Wei ZJ, Lin W, Fan BY, Liu J, et al. Efficacy and safety of tension band wiring versus plate fixation in olecranon fractures: a systematic review and meta-analysis. J Orthop Surg Res. (2016) 11(2):137–41. doi: 10.1186/s13018-016-0465-z
13. Duckworth AD, Bugler KE, Clement ND, Court-Brown CM, McQueen MM. Nonoperative management of displaced olecranon fractures in low-demand elderly patients. J Bone Joint Surg Am. (2014) 96(5):67–72. doi: 10.2106/JBJS.L.01137
14. Duckworth AD, Clement ND, White TO, Court-Brown CM, McQueen MM. Plate versus tension-band wire fixation for olecranon fractures: a prospective randomized trial. J Bone Joint Surg Am. (2017) 99(13):1261–73. doi: 10.2106/JBJS.16.00773
15. Flinterman HJ, Doornberg JN, Guitton TG, Ring D, Goslings JC, Kloen P. Long-term outcome of displaced, transverse, noncomminuted olecranon fractures. Clin Orthop Relat Res. (2014) 472:1955–61. doi: 10.1007/s11999-014-3481-5
16. Gruszka D, Arand C, Nowak T, Dietz SO, Wagner D, Rommens P. Olecranon tension plating or olecranon tension band wiring? A comparative biomechanical study. Int Orthop. (2015) 39(3):955–60. doi: 10.1007/s00264-015-2703-0
17. Zelle BA. CORR Insights(R): long-term outcome of displaced, transverse, noncomminuted olecranon fractures. Clin Orthop Relat Res. (2014) 472:1962–3. doi: 10.1007/s11999-014-3553-6
Keywords: external fixation, elbow, olecranon fractures, case series, fracture
Citation: Tian Y, Ge X, Zou J, Song F, Cheong John Chun tien chui wan, Ge C, Zhang W, Li J and Tian K (2022) Case Report: J-Shaped External Fixator for Treatment of Mayo Type II Olecranon Fractures – A Novel Surgical Technique and Report of Clinical Applications. Front. Surg. 9:855600. doi: 10.3389/fsurg.2022.855600
Received: 3 February 2022; Accepted: 20 May 2022;
Published: 15 June 2022.
Edited by:
Aaron Perdue University of Michigan, United StatesReviewed by:
Nabil A. Ebraheim, University of Toledo, United StatesJin Dai, Nanjing Drum Tower Hospital, China
Copyright © 2022 Tian, Ge, Zou, Song, Cheong, Ge, Zhang, Li and Tian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kang Tian ZG11LXRpYW5rYW5nQG91dGxvb2suY29t
†These authors have contributed equally to this work
Specialty section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
Abbreviations: ASA, American Society of Anesthesiologists; DASH, Disabilities of the Arm, Shoulder, and Hand; J-EF, J-shaped external fixator; MEPS, Mayo Elbow Performance Score; MRI, magnetic resonance imaging; PF, plate fixation; TBW, tension-band wiring
 Yue Tian1,2†
Yue Tian1,2† Kang Tian
Kang Tian