- 1Department of Anesthesiology, Hainan Hospital of General Hospital of PLA, Sanya, China
- 2Department of Anesthesiology, Air Force Medical Center, Beijing, China
- 3Department of Anesthesiology, The First Medical Center of General Hospital of PLA, Beijing, China
Background: Erector spinae plane block (ESPB), as a regional anesthesia modality, is gaining interest and has been used in abdominal, thoracic and breast surgeries. The evidence on the efficacy of this block in spinal surgeries is equivocal. Recently published reviews on this issue have concerning limitations in methodology.
Methods: A systematic search was conducted using the PubMed, Scopus, Embase, and Cochrane Central Register of Controlled Trials (CENTRAL). Randomized controlled trials (RCTs) that were done in patients undergoing spinal surgery and had compared outcomes of interest among those that received ESPB and those with no block/placebo were considered for inclusion. Statistical analysis was performed using STATA software. GRADE assessment was done for the quality of pooled evidence.
Results: A total of 13 studies were included. Patients receiving ESPB had significantly reduced total opioid use (Standardized mean difference, SMD −2.76, 95% CI: −3.69, −1.82), need for rescue analgesia (Relative risk, RR 0.38, 95% CI: 0.22, 0.66) and amount of rescue analgesia (SMD −5.08, 95% CI: −7.95, −2.21). Patients receiving ESPB reported comparatively lesser pain score at 1 h (WMD −1.62, 95% CI: −2.55, −0.69), 6 h (WMD −1.10, 95% CI: −1.45, −0.75), 12 h (WMD −0.78, 95% CI: −1.23, −0.32) and 24 h (WMD −0.54, 95% CI: −0.83, −0.25) post-operatively. The risk of postoperative nausea and vomiting (PONV) (RR 0.32, 95% CI: 0.19, 0.54) was lower in those receiving ESPB. There were no differences in the duration of surgery, intra-operative blood loss and length of hospital stay between the two groups. The quality of pooled findings was judged to be low to moderate.
Conclusions: ESPB may be effective in patients with spinal surgery in reducing post-operative pain as well as need for rescue analgesic and total opioid use. In view of the low to moderate quality of evidence, more trials are needed to confirm these findings.
Systematic Review Registration: http://www.crd.york.ac.uk/PROSPERO/, identifier: CRD42021278133.
Introduction
One of the ensuing complications of spinal surgery is the post-operative pain that could range from moderate to severe and could have an impact on timing of mobilization and rehabilitation, length of hospital stay, patient satisfaction and could lead to chronic backpain (1–3). Delayed mobilization could also increase the risk of thrombo-embolic events, delayed wound healing and nosocomial infections (4, 5). The management of post-operative pain in spinal surgeries has been a challenge. The conventional analgesia model is based on use of opioids and therefore, the opioid- related side effects cannot be avoided (6). These side effects include nausea, vomiting, pruritis, urinary retention and dizziness and could be worrisome for the patients (6). One of the techniques to reduce post-operative pain and opioid related side effects is multimodal analgesic (MMA) regimen (7). It involves use of a variety of drugs and delivery mechanisms.
Use of regional anesthesia is an important component of MMA (7, 8). Recently, a novel method for regional anesthesia named erector spinae plane block (ESPB) has received wide attention. Initially the use of ESPB was demonstrated for treating pain associated with shingles (9). It is a paravertebral interfascial block wherein the anesthetic is injected between the transverse process of the vertebrae and erector spinae muscle (10, 11). Upon being injected, the anesthetic diffuses both cranially and caudally and exerts its action on the ventral and dorsal rami of the spinal nerves (9–11). As the local anesthetic is injected in a plane that is farther from the spinal cord, the associated risk of causing trauma to the cord and consequent complication is minimized. Also, the block is relatively easier to perform and is done under the guidance of ultrasonography. Due to all its features, the use of ESPB is common in abdominal such as laparoscopic cholecystectomy, breast and thoracic surgery (12–14). The role of ESPB in spinal surgeries is being explored through recent randomized controlled trials (RCTs); however, the results are conflicting. There have been systematic reviews and meta-analyses published on this issue recently but the methodology in most of these reviews is not adequate.
A systematic review by Jun Ma et al. included 12 studies with 828 patients and documented that ESPB reduced postoperative pain scores and significantly decreased opioid consumption, compared to no block/placebo (15). Further a reduced the incidence of rescue analgesia and postoperative nausea and vomiting (PONV) was noted. A major shortcoming of the review is that the authors majorly included research outputs that were non-peer reviewed (i.e., thesis/dissertation). Another review by Liu et al. found that ESPB significantly reduced postoperative opioid consumption, pain scores within 24 h post-operative period, need for rescue analgesia and risk of PONV (16). However, some studies that were eligible to be included in the review were not included. Further, there have been recent publication of several new studies on this aspect. Taking into account these considerations, there is a need for a comprehensive, methodologically robust systematic review and meta-analysis to assess the efficacy of ESPB, compared to placebo or no block for patients undergoing spinal surgical procedures. The underlying hypothesis for this meta-analysis was that erector spinae block in patients undergoing spinal surgery will lead to better pain control, reduced need for rescue analgesia, reduced need for opioid and lower risk of complications, compared to placebo or no block.
Materials and Methods
Search Strategy
PubMed, Scopus, Embase, and Cochrane Central Register of Controlled Trials (CENTRAL) databases were systematically searched for English language papers published prior to 15th September 2021 using medical subject heading (MeSH) terminology and free text words (Supplementary Table 1). This meta-analysis was conducted in compliance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) guidelines (17) and is registered in the International Prospective Registry of Systematic Reviews (PROSPERO; registration number-CRD42021278133). The literature search aimed at identifying studies that examined the outcomes of interest between patient groups receiving erector spinae plane block (ESPB) and those that received either no block or placebo for spinal surgery. To elaborate further, the population of interest were subjects undergoing spinal surgery, intervention was the use of erector spinae plane block, comparator was the use of placebo or no block and primary outcomes of interest were post-operative patient reported pain scores, total opioid use post-operatively, need for rescue analgesia and risk of complications. Only studies that adopted a randomized controlled design were of interest for the meta-analysis.
Selection Criteria and Methods
After duplicate removal, two subject experts reviewed all studies identified by the search strategy. First, titles and abstracts were examined, followed by subsequent full text review. Any differences of opinion on study inclusion suitability were resolved through discussion. Only those studies were included in the meta-analysis that fulfilled the inclusion criteria. In order to identify additional literature, the reference list of the included studies was also reviewed.
Inclusion Criteria
Randomized controlled trials (RCTs) that were done in patients undergoing spinal surgery and had compared outcomes of interest among those that received ESPB and those with no block/placebo were considered for inclusion.
Exclusion Criteria
Observational studies, case studies, and reviews were excluded. Studies not providing data on the outcomes of interest or not providing comparative findings based on ESPB and placebo/no block were excluded.
Data Extraction and Quality Assessment
Two separate individuals individually extracted relevant data from included studies using a pre-established data extraction sheet. Data extracted included study identifiers (author names, research year), study settings, study design, subject characteristics, procedure performed, anesthetic dosage, sample size, and main findings. Study quality was assessed using the Cochrane risk of bias assessment tool (18).
Statistical Analysis
This meta-analysis was conducted using STATA version 16.0 and reported effect sizes as pooled relative risks (RR), weighted mean differences (WMD), or standardized mean differences (SMD). WMD was reported for continuous outcomes using the same units whereas SMD for continuous outcomes with different units. Continuous data presented in studies as medians with ranges were converted to means with standard deviations according to a method described by Hozo et al. (19). All effect sizes were reported along with 95% confidence intervals (CI). I2 indicated heterogeneity, and when I2 exceeded 40%, a random effects model was used (20). P-values of < 0.05 were considered statistically significant. Egger's test was used to assess publication bias (21). The quality of evidence generated for the outcomes considered was assessed through GRADE criteria using GRADEpro software (22, 23).
Results
Selection of Articles, Study Characteristics, and Study Quality
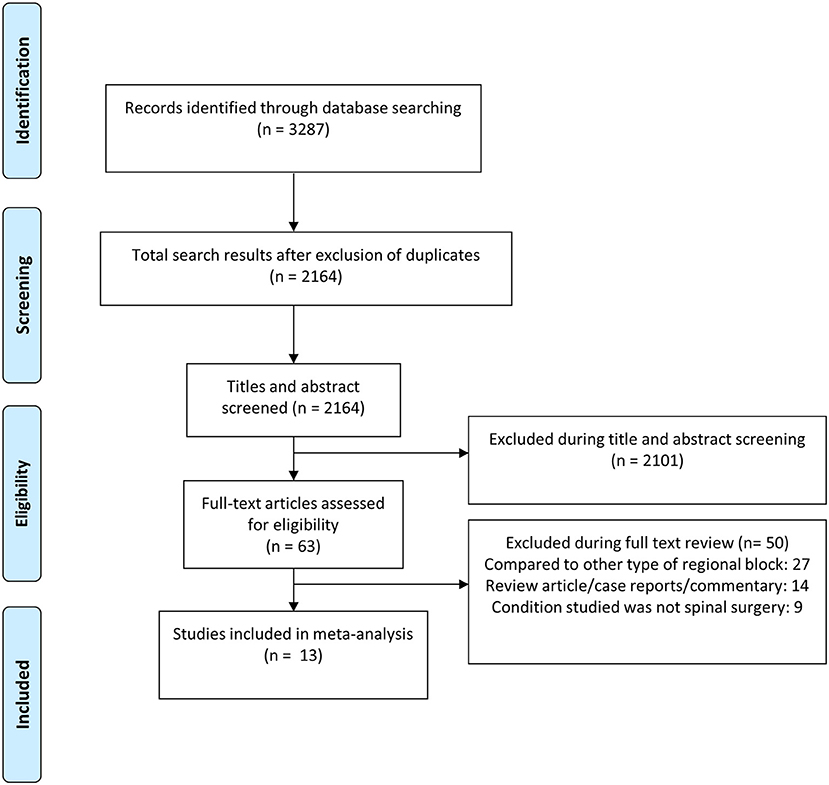
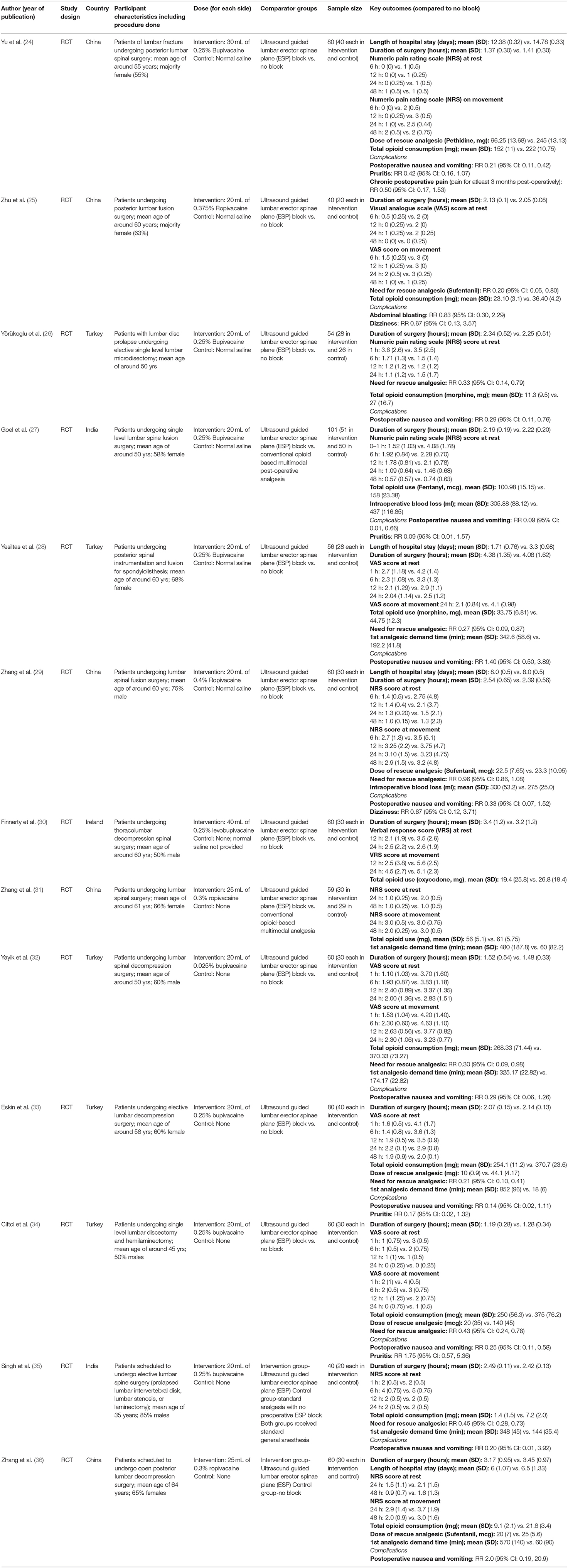
The search strategy yielded 2,164 unique citations (Figure 1). Title and abstract screening eliminated 2,101 citations. Out of the remaining 63 studies, 50 were excluded after full-text review, leaving 13 studies for inclusion (Table 1) (24–36). All the included studies were RCTs. Five studies each were done in China and Turkey. Two studies were done in India and remaining one in Ireland. The included studies were of modest to good quality (Supplementary Table 2). All 13 studies reported random sequence generation. In 10 out of 13 studies, allocation concealment was done and in remaining 3, it is unclear whether it was done. Blinding of participants and personnel was done in 6 studies. In all the studies blinding of outcome assessment was done. GRADE assessment was done for the quality of pooled evidence. The findings of the GRADE assessment are presented as Supplementary Table 3.
Postoperative Opioid Consumption and Need for Rescue Analgesia
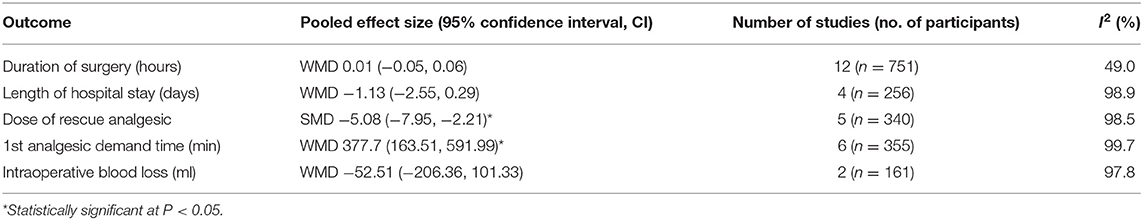
In patients that received erector spinae plane block (ESPB), the total opioid use in the first 48 h post-surgery was significantly lower (SMD −2.76, 95% CI: −3.69, −1.82; N = 12, I2 = 95.7%) than patients with placebo/no block (Figure 2). Egger's test indicated no evidence of publication bias (P = 0.34). Compared to patients with placebo/no block, those with ESPB had significantly reduced need for rescue analgesia (RR 0.38, 95% CI: 0.22, 0.66; N = 8, I2 = 85.1%) (Figure 3). Egger's test indicated no evidence of publication bias (P = 0.18). Also, those receiving ESPB required lower amount of analgesia (SMD −5.08, 95% CI: −7.95, −2.21; N = 5, I2 = 98.5%) and had a higher demand time (in minutes) (WMD 377.7, 95% CI: 163.51, 591.99; N = 6, I2 = 99.7%) (Table 2).
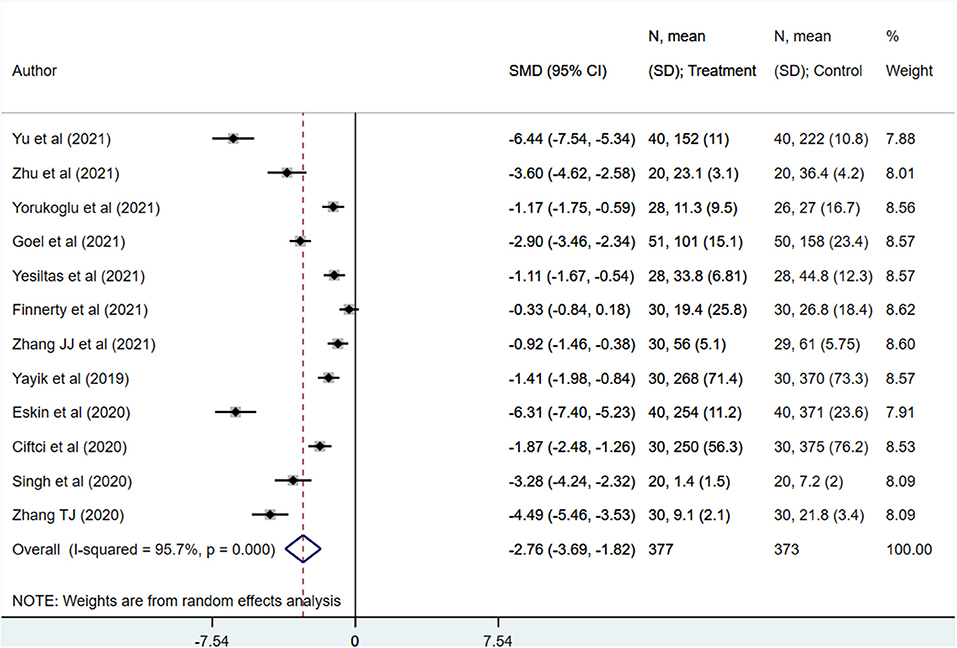
Figure 2. Comparison of postoperative opioid consumption among subjects with erector spinae plane block, compared to placebo or no block.
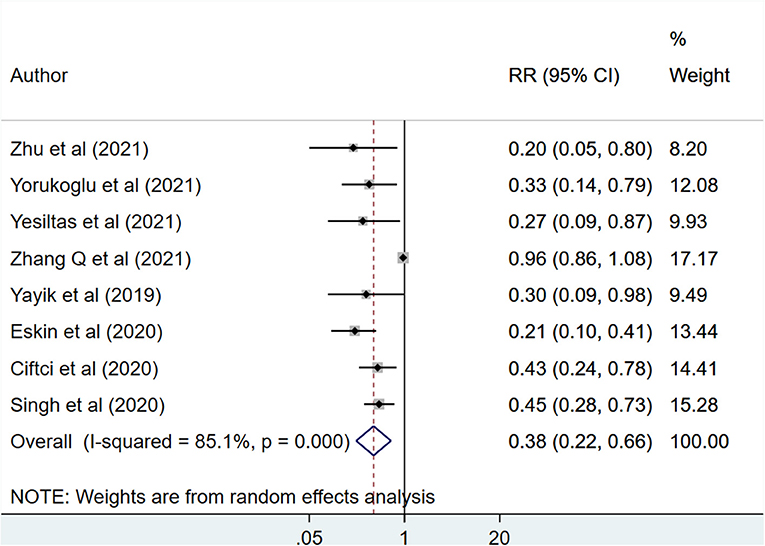
Figure 3. Risk for need of rescue analgesia among subjects with erector spinae plane block, compared to placebo or no block.
Post-operative Pain Scores on Rest and Movement
Patients receiving ESPB reported comparatively lesser pain score at 1 h (WMD −1.62, 95% CI: −2.55, −0.69; N = 7, I2 = 95.7%), 6 h (WMD −1.10, 95% CI: −1.45, −0.75; N = 10, I2 = 91.8%), 12 h (WMD −0.78, 95% CI: −1.23, −0.32; N = 11, I2 = 96.9%) and 24 h (WMD −0.54, 95% CI: −0.83, −0.25; N = 13, I2 = 92.8%) post-operatively compared to those receiving either placebo or no block (Figure 4, Table 3). There was no statistically significant difference in the reported pain scores between patients in both the groups at 48 h post-operatively. Similar findings were noted for pain scores at movement wherein those receiving ESPB reported on comparatively lesser pain score at movement at 1 h (WMD −2.29, 95% CI: −2.94, −1.64; N = 2, I2 = 68.1%), 6 h (WMD −1.63, 95% CI: −2.01, −1.26; N = 5, I2 = 90.1%), 12 h (WMD −1.81, 95% CI: −2.47, −1.15; N = 6, I2 = 96.2%) and 24 h (WMD −0.96, 95% CI: −1.39, −0.53; N = 9, I2 = 91.2%) post-operatively compared to those receiving either placebo or no block (Figure 5, Table 4).
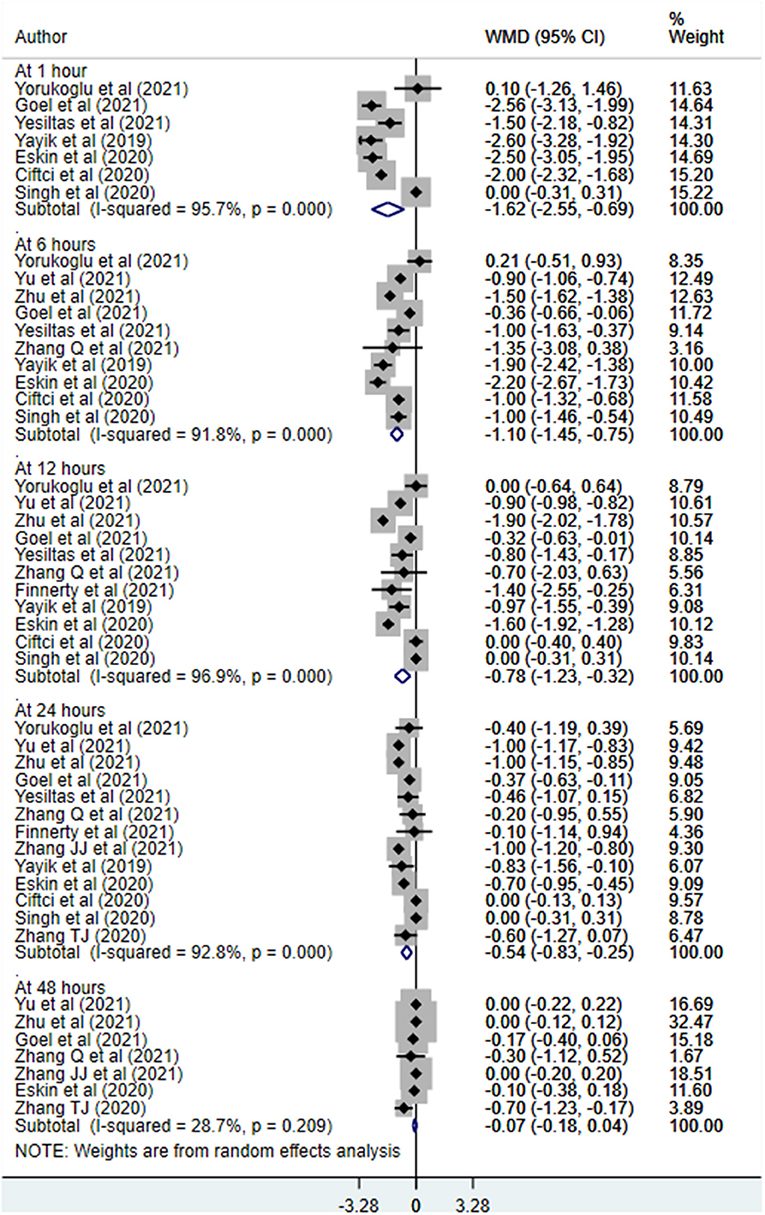
Figure 4. Postoperative pain scores at rest among subjects with erector spinae plane block, compared to placebo or no block.
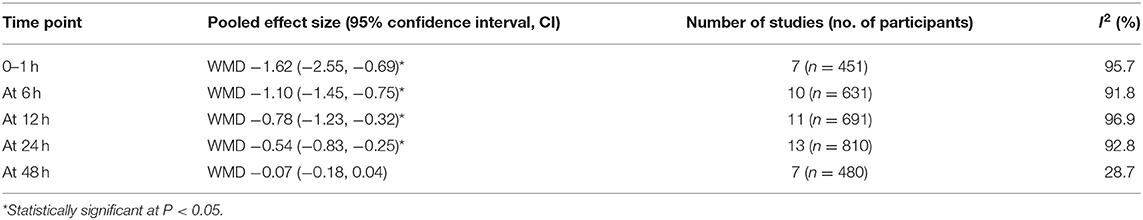
Table 3. Summary result of the postoperative pain scores at rest, comparing subjects with erector spinae plane block to those with placebo or no block.
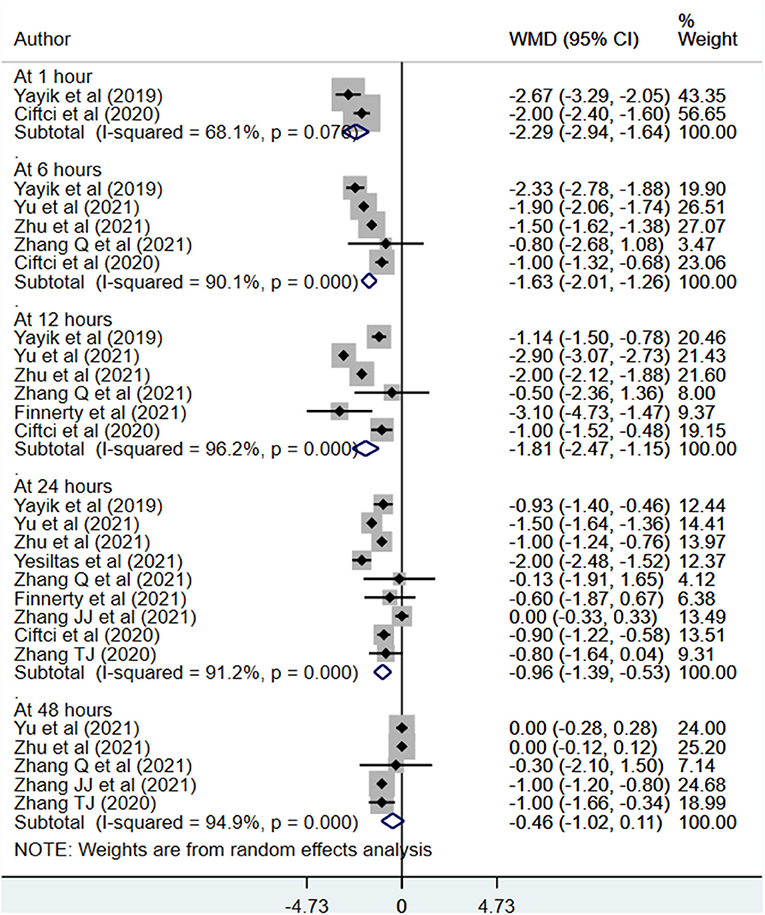
Figure 5. Postoperative pain scores at movement among subjects with erector spinae plane block, compared to placebo or no block.
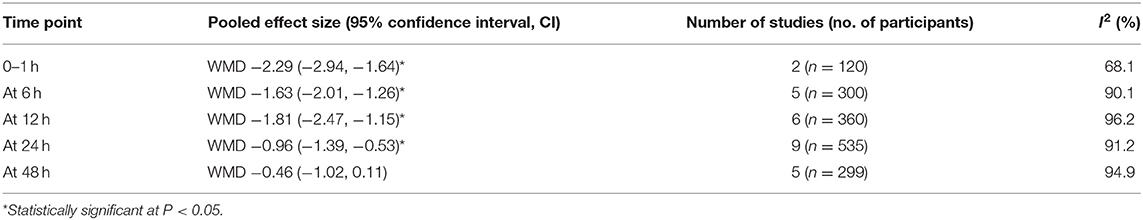
Table 4. Summary result of the postoperative pain scores at movement, comparing subjects with erector spinae plane block to those with placebo or no block.
Complications and Other Outcomes
Postoperative nausea and vomiting (PONV) risk (RR 0.32, 95% CI: 0.19, 0.54; N = 10, I2 = 37.2%) was lower in those receiving ESPB compared to those with placebo/no block (Figure 6). However, pruritis risk (RR 0.45, 95% CI: 0.14, 1.46; N = 4, I2 = 60.4%) and dizziness (RR 0.67, 95% CI: 0.20, 2.21; N = 2, I2 = 0.0%) was similar in both the groups. Egger's test indicated no evidence of publication bias (P = 0.22 for PONV, P = 0.12 for pruritis and P = 0.82 for dizziness). There were no differences in the duration of surgery, intra-operative blood loss, and hospital stay duration between the two groups (Table 2).
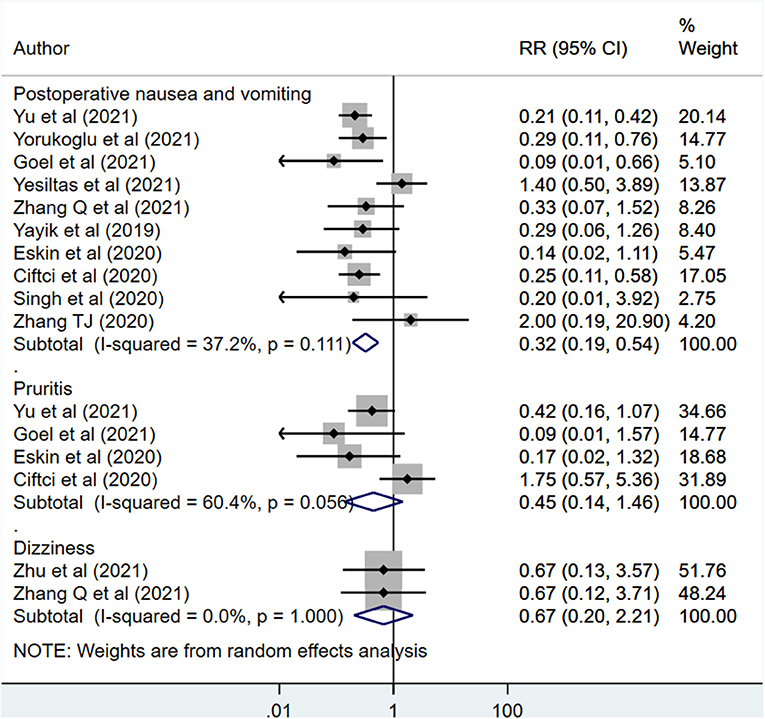
Figure 6. Risk of complications among subjects with erector spinae plane block, compared to placebo or no block.
Discussion
ESPB block is induced through injection of local anesthetic between the erector spinae muscle and the transverse process of the vertebrae (9–11). Upon injection, the anesthetic diffuses both cranially and caudally and acts on the dorsal rami of the spinal nerves. Some studies suggest that ESPB, similar to epidural analgesia, may play a dual role of visceral and somatic analgesia (37, 38). One of the advantages of ESPB is that is ultrasound guided and the plane of delivery of the local anesthetic is away from the spinal cord. This minimizes the risk of spinal injury. Further, the risk of hematoma and pneumothorax is minimal with this technique. All this collectively make ESPB an attraction procedure of choice for post-operative analgesia.
The current meta-analysis was conducted to provide updated evidence on the efficacy of ESPB, compared to placebo or no block for patients undergoing spinal surgical procedures. Through pooling of findings from 13 RCTs, the review noted a substantial reduction in total opioid use post-operatively, reduced need for rescue analgesia, need for lower amount of rescue analgesia and had a higher demand time for analgesia. Patients receiving ESPB reported comparatively lesser pain score at 1 to 24 h post-operatively, both at rest and on movement. At 48 h post-operative period, the pain scores were similar in both the groups. Further, the risk of postoperative nausea and vomiting (PONV) was lower in those receiving ESPB. There were no differences in the duration of surgery, intra-operative blood loss and length of hospital stay between the two groups. On GRADE assessment, the quality of the pooled findings was low to moderate.
The findings are similar to the previous meta-analysis on this issue. Jun Ma et al. in their review of 12 studies (n = 828) documented a significant effect of ESPB on reducing pain scores at rest until 48 h post-operatively but only until 24 h post-operatively on movement (15). There was also a reduced consumption of opioid and a reduced risk of need for rescue analgesia in those that received ESPB. In the ESPB group, there was also a reduced risk of PONV (15). A major limitation of this review is that the authors included non-peer reviewed research findings provided in thesis/dissertation. Further, the review did not provide any evidence on the quality of the pooled findings. Another recent review by Liu et al. documented significantly lower requirement for opioid post-operatively, reduced postoperative pain scores and reduced risk of need for rescue analgesia (16). The risk of postoperative nausea and vomiting was significantly lower in the ESPB group. Kendall et al. in their review included studies among patients undergoing surgical procedures and not necessarily restricted their analyses to only those with spinal surgery (39). They included 13 RCTs with 679 patients and found that ESPB reduced post-operative opioid consumption, as well as post-operative pain at 6 h. This review provided moderate quality evidence in support of ESPB being a useful strategy for alleviation of post-operative pain (39).
Our current review and meta-analysis reaffirm the findings of the previous reviews but does that through better search, identification and inclusion of all relevant publications. The findings of our analysis have important clinical implications as the post-operative pain following spinal surgery affects a substantial proportion of patients (around half) and insufficient pain control may probably delay attainment of early mobilization and rehabilitation. This, further, could lead to sub-optimal well-being of the subjects and could culminate into persistent post-operative pain that may require prolonged use of pain medications. We also did the GRADE assessment of the pooled findings and noted a low to moderate quality for most of the outcomes. Low to moderate quality indicates that further research is required and is likely or very likely to have an important impact on the confidence in the estimate of effect and may change the estimate.
There are some of the limitations of this meta-analysis. In some of the studies, double blinding was not done. Inclusion of such articles may adversely impact the quality of the evidence. The sample sizes considered in the included studies was small. Future studies may be done with larger sample sizes and robust methodology. One of the key limitations is that we were unable to examine the dose response effect of ESPB owing to the lack of substantial variability in the dose of the anesthetic used. For some of the outcomes, there was substantial heterogeneity and therefore, we used the random effects model in such instances. This heterogeneity could be due to the variability in the management protocols and skills of treating surgeon across different institutions where the studies were conducted. There could be other factors leading to heterogeneity such as dosage and nature of anesthetic used, patient characteristics, tools used to assess post-operative pain, difference in the nature of analgesics used for management of post-operative pain. Future studies should be conducted with harmonized guidelines for application of ESPB, protocols for management of post-operative pain and measurement of outcomes.
In conclusion, the current meta-analysis suggests that in patients undergoing spinal surgery, ESPB is efficacious, compared to no block/placebo, in reducing pain both at rest and on movement until 24 h post-operatively, total opioid requirement post-operatively, lowering the risk of need for rescue analgesic and the amount of analgesic required. Further, the block reduces the risk of PONV. Future studies should attempt to understand the dose response effect of ESPB on post-operative analgesia and other outcomes.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Materials, further inquiries can be directed to the corresponding author/s.
Author Contributions
MD and YX designed the project and prepared the manuscript. MD, YX, and QF were involved in data collection and data analysis. QF edited the manuscript. All authors read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.845125/full#supplementary-material
References
1. Gerbershagen HJ, Aduckathil S, van Wijck AJM, Peelen LM, Kalkman CJ, Meissner W. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology. (2013) 118:934–44. doi: 10.1097/ALN.0b013e31828866b3
2. Bajwa SJS, Haldar R. Pain management following spinal surgeries: an appraisal of the available options. J Craniovertebr Junction Spine. (2015) 6:105–10. doi: 10.4103/0974-8237.161589
3. Dunn LK, Durieux ME, Nemergut EC. Non-opioid analgesics: novel approaches to perioperative analgesia for major spine surgery. Best Pract Res Clin Anaesthesiol. (2016) 30:79–89. doi: 10.1016/j.bpa.2015.11.002
4. Efthymiou CA, O'Regan DJ. Postdischarge complications: what exactly happens when the patient goes home? Interact Cardiovasc Thorac Surg. (2011) 12:130–4. doi: 10.1510/icvts.2010.249474
5. Gan TJ. Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res. (2017) 10:2287–98. doi: 10.2147/JPR.S144066
6. Rosenblum A, Marsch LA, Joseph H, Portenoy RK. Opioids and the treatment of chronic pain: controversies, current status, and future directions. Exp Clin Psychopharmacol. (2008) 16:405–16. doi: 10.1037/a0013628
7. Kurd MF, Kreitz T, Schroeder G, Vaccaro AR. The role of multimodal analgesia in spine surgery. J Am Acad Orthop Surg. (2017) 25:260–8. doi: 10.5435/JAAOS-D-16-00049
8. Mergeay M, Verster A, Van Aken D, Vercauteren M. Regional versus general anesthesia for spine surgery. A comprehensive review. Acta Anaesthesiol Belg. (2015) 66:1–9.
9. Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. (2016) 41:621–7. doi: 10.1097/AAP.0000000000000451
10. Urits I, Charipova K, Gress K, Laughlin P, Orhurhu V, Kaye AD, et al. Expanding role of the erector spinae plane block for postoperative and chronic pain management. Curr Pain Headache Rep. (2019) 23:71. doi: 10.1007/s11916-019-0812-y
11. Tulgar S, Aydin ME, Ahiskalioglu A, De Cassai A, Gurkan Y. Anesthetic techniques: focus on lumbar erector spinae plane block. Local Reg Anesth. (2020) 13:121–33. doi: 10.2147/LRA.S233274
12. Leong RW, Tan ESJ, Wong SN, Tan KH, Liu CW. Efficacy of erector spinae plane block for analgesia in breast surgery: a systematic review and meta-analysis. Anaesthesia. (2021) 76:404–13. doi: 10.1111/anae.15164
13. Zhao H, Xin L, Feng Y. The effect of preoperative erector spinae plane vs. paravertebral blocks on patient-controlled oxycodone consumption after video-assisted thoracic surgery: a prospective randomized, blinded, non-inferiority study. J Clin Anesth. (2020) 62:109737. doi: 10.1016/j.jclinane.2020.109737
14. Koo C-H, Hwang J-Y, Shin H-J, Ryu J-H. The effects of erector spinae plane block in terms of postoperative analgesia in patients undergoing laparoscopic cholecystectomy: a meta-analysis of randomized controlled trials. J Clin Med. (2020) 9:E2928. doi: 10.3390/jcm9092928
15. Ma J, Bi Y, Zhang Y, Zhu Y, Wu Y, Ye Y, et al. Erector spinae plane block for postoperative analgesia in spine surgery: a systematic review and meta-analysis. Eur Spine J. (2021) 30:3137–49. doi: 10.1007/s00586-021-06853-w
16. Liu M-J, Zhou X-Y, Yao Y-B, Shen X, Wang R, Shen Q-H. Postoperative analgesic efficacy of erector spinae plane block in patients undergoing lumbar spinal surgery: a systematic review and meta-analysis. Pain Ther. (2021) 10:333–47. doi: 10.1007/s40122-021-00256-x
17. PRISMA. Transparent Reporting of Systematic Reviews and Meta-Analyses. Available online at: http://www.prisma-statement.org/PRISMAStatement/ (accessed September 11, 2021).
18. Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928
19. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. (2005) 5:13. doi: 10.1186/1471-2288-5-13
20. Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions : Cochrane Book Series. London: The Cochrane Collaboration (2008) 674. Available online at: https://onlinelibrary.wiley.com/doi/book/10.1002/9780470712184
21. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–634. doi: 10.1136/bmj.315.7109.629
22. Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. BMJ. (2004) 328:1490. doi: 10.1136/bmj.328.7454.1490
23. Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso-Coello P, Rind D, et al. GRADE guidelines 6. Rating the quality of evidence–imprecision. J Clin Epidemiol. (2011) 64:1283–293. doi: 10.1016/j.jclinepi.2011.01.012
24. Yu Y, Wang M, Ying H, Ding J, Wang H, Wang Y. The analgesic efficacy of erector spinae plane blocks in patients undergoing posterior lumbar spinal surgery for lumbar fracture. World Neurosurg. (2021) 147:e1–7. doi: 10.1016/j.wneu.2020.10.175
25. Zhu L, Wang M, Wang X, Wang Y, Chen L, Li J. Changes of opioid consumption after lumbar fusion using ultrasound-guided lumbar erector spinae plane block: a randomized controlled trial. Pain Phys. (2021) 24:E161–8. doi: 10.36076/ppj.2021.24.E161-E168
26. Yörükoglu HU, Içli D, Aksu C, Cesur S, Kuş A, Gürkan Y. Erector spinae block for postoperative pain management in lumbar disc hernia repair. J Anesth. (2021) 35:420–5. doi: 10.1007/s00540-021-02920-0
27. Goel VK, Chandramohan M, Murugan C, Shetty AP, Subramanian B, Kanna RM, et al. Clinical efficacy of ultrasound guided bilateral erector spinae block for single level lumbar fusion surgery: a prospective, randomized, case-control study. Spine J. (2021) 21:1873–80. doi: 10.1016/j.spinee.2021.06.015
28. Yeşiltaş S, Abdallah A, Uysal Ö, Yilmaz S, Çinar I, Karaaslan K. The efficacy of intraoperative freehand erector spinae plane block in lumbar spondylolisthesis: a randomized controlled study. Spine. (2021) 46:E902–10. doi: 10.1097/BRS.0000000000003966
29. Zhang Q, Wu Y, Ren F, Zhang X, Feng Y. Bilateral ultrasound-guided erector spinae plane block in patients undergoing lumbar spinal fusion: a randomized controlled trial. J Clin Anesth. (2021) 68:110090. doi: 10.1016/j.jclinane.2020.110090
30. Finnerty D, Ní Eochagáin A, Ahmed M, Poynton A, Butler JS, Buggy DJ. A randomised trial of bilateral erector spinae plane block vs. no block for thoracolumbar decompressive spinal surgery. Anaesthesia. (2021) 76:1499–503. doi: 10.1111/anae.15488
31. Zhang J-J, Zhang T-J, Qu Z-Y, Qiu Y, Hua Z. Erector spinae plane block at lower thoracic level for analgesia in lumbar spine surgery: a randomized controlled trial. World J Clin Cases. (2021) 9:5126–34. doi: 10.12998/wjcc.v9.i19.5126
32. Yayik AM, Cesur S, Ozturk F, Ahiskalioglu A, Ay AN, Celik EC, et al. Postoperative analgesic efficacy of the ultrasound-guided erector spinae plane block in patients undergoing lumbar spinal decompression surgery: a randomized controlled study. World Neurosurg. (2019) 126:e779–85. doi: 10.1016/j.wneu.2019.02.149
33. Eskin MB, Ceylan A, Özhan MÖ, Atik B. Ultrasound-guided erector spinae block versus mid-transverse process to pleura block for postoperative analgesia in lumbar spinal surgery. Anaesthesist. (2020) 69:742–50. doi: 10.1007/s00101-020-00848-w
34. Ciftci B, Ekinci M, Celik EC, Yayik AM, Aydin ME, Ahiskalioglu A. Ultrasound-guided erector spinae plane block versus modified-thoracolumbar interfascial plane block for lumbar discectomy surgery: a randomized, controlled study. World Neurosurg. (2020) 144:e849–55. doi: 10.1016/j.wneu.2020.09.077
35. Singh S, Choudhary NK, Lalin D, Verma VK. Bilateral ultrasound-guided erector spinae plane block for postoperative analgesia in lumbar spine surgery: a randomized control trial. J Neurosurg Anesthesiol. (2020) 32:330–4. doi: 10.1097/ANA.0000000000000603
36. Zhang T-J, Zhang J-J, Qu Z-Y, Zhang H-Y, Qiu Y, Hua Z. Bilateral erector spinae plane blocks for open posterior lumbar surgery. JPR. (2020) 13:709–17. doi: 10.2147/JPR.S248171
37. Greenhalgh K, Womack J, Marcangelo S. Injectate spread in erector spinae plane block. Anaesthesia. (2019) 74:126–7. doi: 10.1111/anae.14523
38. Celik M, Tulgar S, Ahiskalioglu A, Alper F. Is high volume lumbar erector spinae plane block an alternative to transforaminal epidural injection? Evaluation with MRI. Reg Anesth Pain Med. (2019). doi: 10.1136/rapm-2019-100514
Keywords: erector spinae plane block, spinal surgery, post-operative analgesia, complications, meta-analysis
Citation: Duan M, Xu Y and Fu Q (2022) Efficacy of Erector Spinae Nerve Block for Pain Control After Spinal Surgeries: An Updated Systematic Review and Meta-Analysis. Front. Surg. 9:845125. doi: 10.3389/fsurg.2022.845125
Received: 29 December 2021; Accepted: 28 January 2022;
Published: 28 February 2022.
Edited by:
Zenon Pogorelić, University Hospital of Split, CroatiaReviewed by:
Sachit Anand, Kokilaben Dhirubhai Ambani Hospital and Medical Research Institute, IndiaAbhijit Nair, Ministry of Health, Oman
Copyright © 2022 Duan, Xu and Fu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qiang Fu, ZHVhbm1kODVAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Mingda Duan1†
Mingda Duan1† Qiang Fu
Qiang Fu