- The First People's Hospital of Yunnan Province Gynecology Department (Affiliated Hospital of Kunming University of Science and Technology), Kunming, China
Background: Robotic-assisted surgery is one of the novel minimally invasive surgical techniques for the treatment of gynecological malignancies. The aim of this systematic review and meta-analysis was to compare the outcomes of robot-assisted vs. conventional laparoscopy for para-aortic lymphadenectomy (PAL) in patients with gynecological malignancies.
Methods: An electronic search in PubMed, Scopus, Cochrane Central Register of Controlled Trials (CENTRAL), and Google Scholar databases was performed for articles, published up to 01st November 2021. Outcomes including operating time (OT), total blood loss (TBL), length of stay (LOS), and complication rate (CR) in robot-assisted vs. conventional laparoscopy were investigated.
Results: A total of nine studies (7 non-RCTs and 2 RCTs) involving 914 participants were included. Of them, 332 patients underwent robotic laparoscopy (robotic group) and 582-conventional laparoscopy (conventional laparoscopy group). A significant decrease in TBL (MD = −149.1; 95% CI: −218.4 to −79.91) [ml] was observed in the robotic group as compared to the conventional laparoscopy group. However, no significant difference was noted for OT, CR, and LOS in the overall findings. Further subgroup analysis showed that the robotic group had a lower OT in mixed histological populations and studies reporting on the extraperitoneal approach. The lower chance of TBL was observed in mixed histological populations and studies involving extraperitoneal approach, Caucasian population, and non-RCTs design.
Conclusions: Robotic laparoscopy has a significant advantage over the conventional laparoscopy approach for PAL in gynecological malignancies. Further prospective observational studies embedded with a large sample size are needed to validate our findings.
Introduction
Para-aortic lymphadenectomy (PAL) is an important step in the surgical staging of a variety of gynecologic malignancies, such as cervical, endometrial, and ovarian cancers (1–3). It may provide significant information on the spread of cancer and the prognosis, and help in developing targeted primary and adjuvant therapy (4). However, complex surgical procedures like PAL might have substantial short- and long-term implications, such as the increased risk of intraperitoneal adhesions and radiation-related complications (1, 2). In 1997, Dargent et al. (5) proposed a method of using laparoscopic surgery for extraperitoneal lymphadenectomy. Laparoscopic extraperitoneal PAL has been proved to be safe and feasible in several trials (6–8) with the limitations of the typical transperitoneal laparoscopic method in terms of operative field exposure (due to obesity and overlaying bowel loops) (6, 7). Working in the retroperitoneal areas, on the other hand, can lead to complications and problems caused by ureteral, vascular, or intestinal disease (9). However, extraperitoneal laparoscopic PAL is still considered a difficult technique that necessitates a steep learning curve and advanced endoscopic abilities (6).
Common staging treatments for endometrial and ovarian malignancies include pelvic and para-aortic lymph node excision, hysterectomy, and bilateral salpingo-oophorectomy (10, 11). As a result, processes become lengthy and demanding. The emergence of robotic-assisted surgery has drastically changed gynecologic surgical practice in recent years (12–15). The use of robotic technology in laparoscopic surgery may overcome technical limitations of conventional laparoscopies, such as limited dexterity, flat two-dimensional vision, and difficulties in hand-eye coordination (16). Minimally invasive surgery for oncologic staging in endometrial and ovarian malignancies also results in a significant reduction in recovery time and length of hospital stay (17, 18). In the past few years, several studies have compared robot-assisted vs. conventional laparoscopy for PAL in patients with gynecological malignancies with limited data (8, 19–27). The main aim of this systematic review and meta-analysis was to compare the outcomes of robot-assisted vs. conventional laparoscopy for PAL in gynecological malignancies.
Materials and Methods
Study Protocol
This meta-analysis was done according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement guidelines and the review protocol was registered on PROSPERO CRD42021281371.
Eligibility Criteria
Inclusion Criteria
(a) Observational or interventional studies comparing the outcomes for patients with gynecological malignancies (endometrial cancer, cervical cancer, Ovarian Cancer) who underwent a para-aortic lymphadenectomy or both pelvic and para-aortic lymphadenectomy, by conventional laparoscopic and robotic approach; (b) Availability of at least one of the following outcome measures (operation time, total blood loss, length of hospital stay, and postoperative complications) in both robotic and conventional laparoscopy groups; (c) patients with gynecological malignancies, aged > 18 years.
Exclusion Criteria
(a) Duplicate studies, case series, case reports, systematic reviews, conference abstracts, preprints, and editorials; (b) Studies that do not describe relevant outcomes; (c) Full texts are unavailable.
Outcome Measures
To assess operating time, total blood loss, length of stay in hospital, and complications rates in robot-assisted vs. conventional laparoscopy for PAL in gynecological cancers.
Search Strategy
The following databases were searched for published articles up to November 1, 2021: PubMed, Scopus, Cochrane Central Register of Controlled Trials (CENTRAL), and Google Scholar. The following search terms were used: “robotics” OR “robot” OR “Conventional” AND “laparoscopy” AND “extraperitoneal” OR “retroperitoneal” AND “gynecological cancers” OR “gynecological malignancy” AND “lymphadenectomy” OR “para-aortic lymphadenectomy”. The titles and abstracts of the publications found in the initial search were examined. Studies were removed if they had no control group or only provided an abstract. Only Randomized Controlled trials (RCTs) and observational studies (prospective/retrospective cohort studies, case-controlled studies) were considered. Relevant studies were then identified and their full texts were independently examined in detail by the two reviewers. All disagreements were resolved in consensus with another reviewer. No language restriction was used during the literature search. References of the included papers were further searched for additional relevant studies.
Data Extraction
A predefined data extraction table was used by two independents researchers to extract relevant information, including first author name, country, ethnicity, year of publication, study design, duration of the study, number of patients, treatment methods, population type, tumor grade, mean age, body mass index (BMI), operating time (OT), total blood loss (TBL), length of stay (LOS), postoperative complication rate (CR), and lymphadenectomy approach (transperitoneal/extraperitoneal). Ethnicity was categorized into Asian and Caucasian populations owing to a difference in the environmental, lifestyle, and cultural traditions in order to compare robotic-assisted vs. conventional laparoscopy for para-aortic lymphadenectomy in gynecological malignancies. Any disagreements were resolved by a discussion with the third researcher.
Quality Assessment
The assessment of the quality of the included studies was conducted by using the Newcastle–Ottawa scale (NOS) (28). This assessment scale uses three broad factors (selection, comparability, and exposure), with the scores ranging from 0 (lowest quality) to 8 (best quality). Two authors independently rated the study's quality. Any disagreement was subsequently resolved by discussion or consultation with a third author.
Publication Bias
A funnel plot analysis was used to assess publication bias (29). Egger's regression test was used to determine the asymmetry of funnel plots (30).
Statistical Analysis
The analysis of continuous outcomes was done using the mean difference (MD) with a 95% CI. Dichotomous outcomes were analyzed using the risk ratios (RR) with 95 % CI. Values reported in median (range) were converted to mean [standard deviation (SD)] using an excel spreadsheet including all formulas that serve as comprehensive guidance for performing meta-analysis as described by Wan et al. (31). Cochran's Q- and I2-tests were used to assess heterogeneity among outcomes of the included studies. When I2 was > 50%, some degree of heterogeneity was assumed, and the random-effects model was employed. In all other cases, the fixed effects model was utilized. Subgroup analysis based on ethnicity, types of study, histological type, and lymphadenectomy approach (transperitoneal/extraperitoneal/both) was done for all the included studies. Selection bias and heterogeneity arising from individual studies were assessed by sensitivity analyses. This involved the sequential deletion of a single study during each turn. A P-value of < 0.05 was considered statistically significant. All statistical analyses were performed using Review Manager version 5.3 software (Nordic Cochrane Center, Copenhagen, Denmark).
Results
Literature Selection
The initial search generated 718 records, of which 415 records remained after duplicates were removed. As summarized in Figure 1, following the exclusion of irrelevant studies and review articles, 25 eligible articles were further evaluated for eligibility. Finally, after evaluating study details, 16 articles were removed due to insufficient data or overlapping data, leaving the current meta-analysis with 09 studies (8, 19–26). PRISMA 2020 checklist has been provided in the Supplementary Table S1.
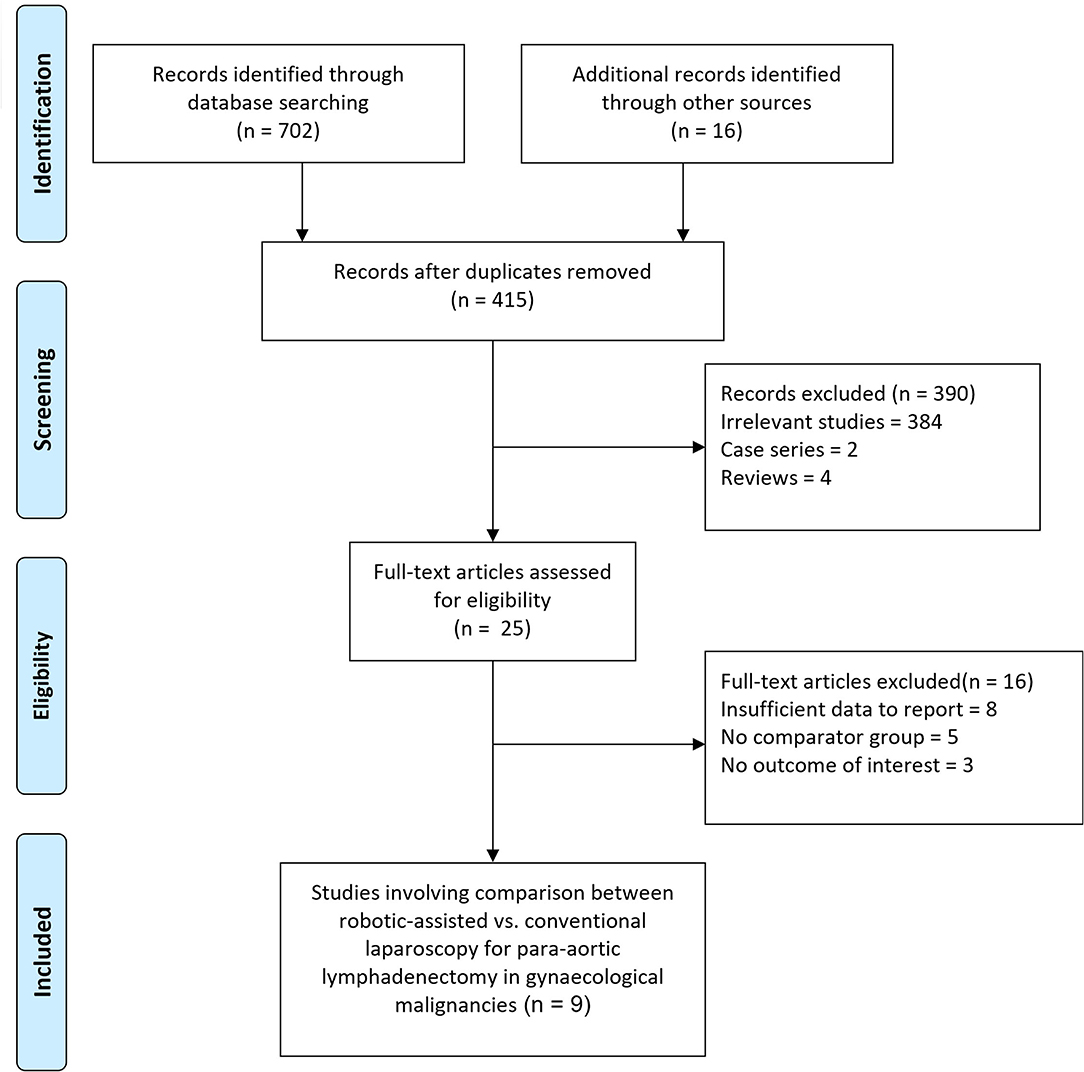
Figure 1. Flow diagram for the selection of studies and specific reasons for exclusion from the present meta-analysis.
Study Characteristics
A total of nine studies [7 non-RCTs (8, 19, 21–25) and 2 RCTs (20, 26)] involving 914 participants (332 patients in the robotic group and 582 in the conventional laparoscopy group) were included in our systematic review and meta-analysis. All included studies were published between 2014 and 2021 and the sample size in the studies ranged from 17 to 162 patients with gynecological malignancies. Of nine studies, six (8, 19, 21–24) were of retrospective cohort and only one study was prospective (25). Six studies were conducted in the Caucasian population (8, 20, 21, 24–26) while three studies were in patients of Asian ethnicity (19, 22, 23). Five studies included patients with endometrial cancer (8, 19, 20, 22, 23), two studies included patients with cervical cancer (21, 24), and two studies included patients with endometrial, ovarian, and cervical cancer (25, 26). The baseline, clinical characteristics, and quality score of the included studies are summarized in Table 1. Most studies were of good quality, with a NOS score of six or higher. PRISMA checklist has been provided in the Supplementary Table S1.
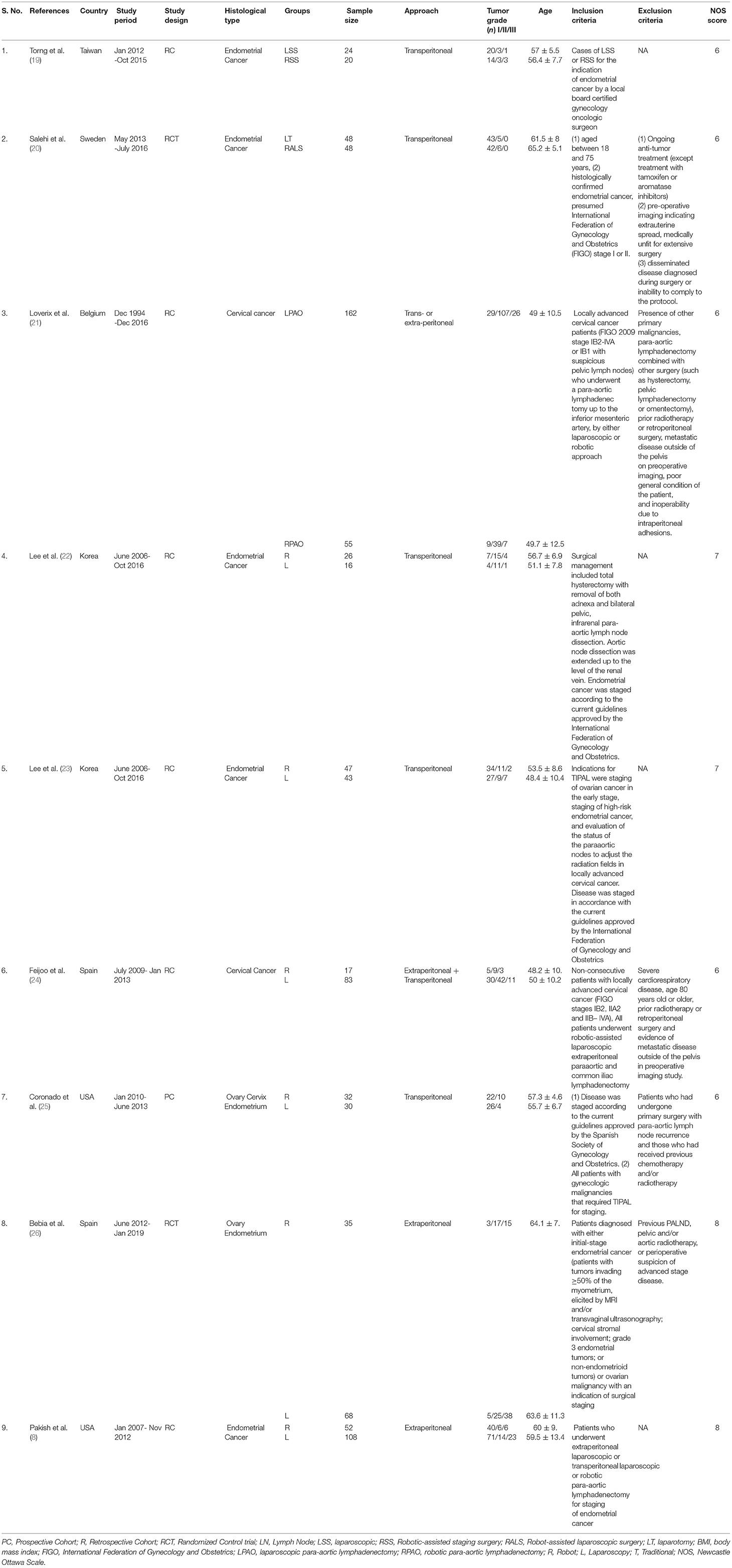
Table 1. Characteristics of included studies for the comparison of robotic-assisted vs. conventional laparoscopy for para-aortic lymphadenectomy in gynecological malignancies.
Operation Time
Eight studies (8, 19–21, 23–26) with a total of 872 patients reported the data for OT (mins) in both robotic and conventional laparoscopy groups. No significant changes were observed in operative time for overall population (MD = −0.67, 95% CI: −17.02 to 15.67) (Figure 2). The random-effect model was applied in the analyses as significant heterogeneity (I2 = 91%, p = <0.0001) was observed. Stratified analysis based on ethnicity, types of study, histological type and lymphadenectomy approach, showed significantly shorter operation time in studies with extraperitoneal approach (MD = −24.4, 95% CI: −44.9 to −3.97, I2 = 92%) (Table 2). However, more operation time was required in the robotic group as compared with the conventional laparoscopy group for studies conducted in the Asian population and with a transperitoneal approach (MD = 58.97, 95% CI: 11.57 to 106.38, I2 = 76%).
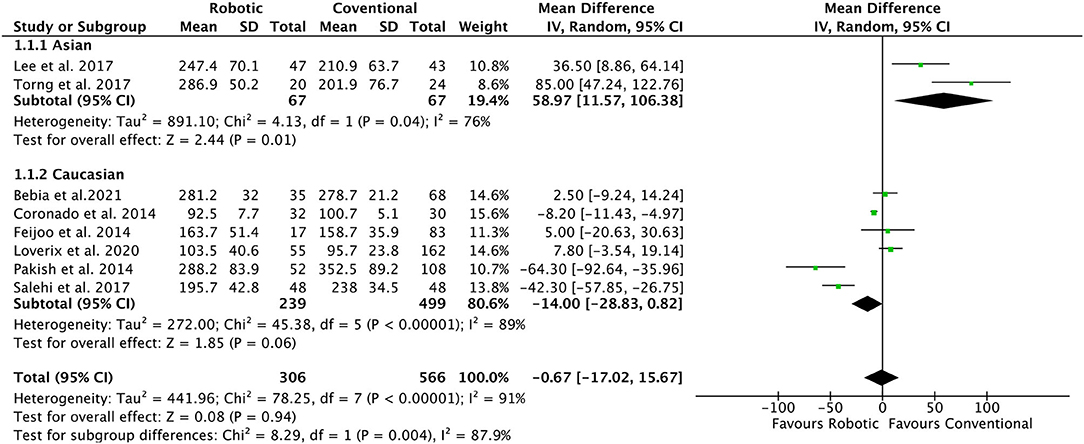
Figure 2. Forest plot of the association of operation time in robotic-assisted vs. conventional laparoscopy for para-aortic lymphadenectomy in gynecological malignancies.
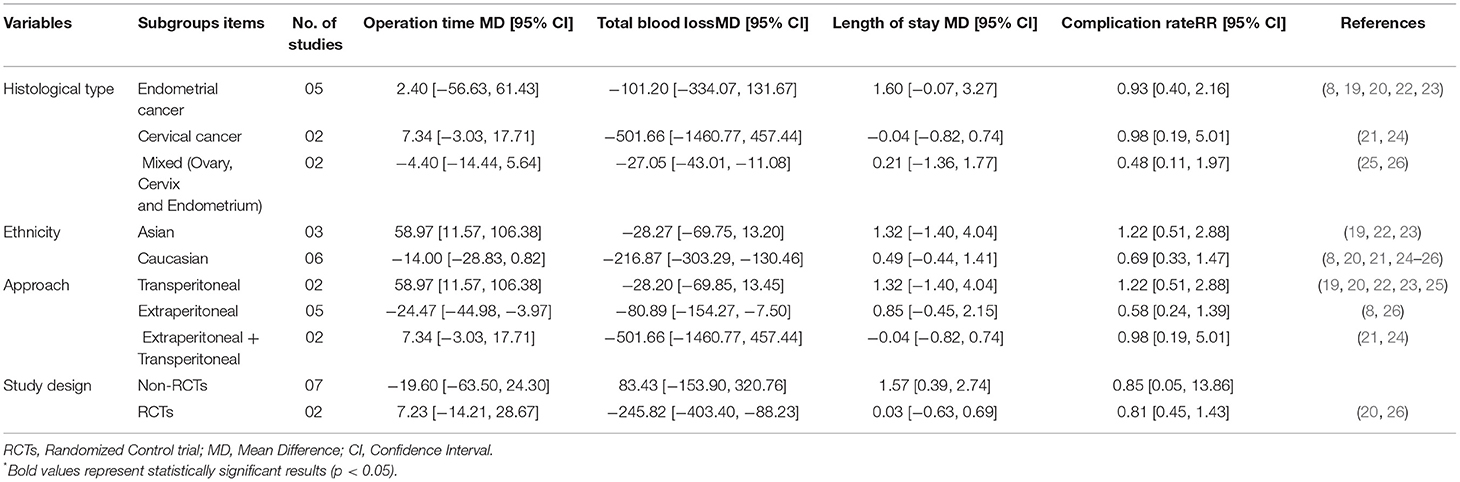
Table 2. Summary of effect size based on subgroup analysis for the comparison of robotic-assisted vs. conventional laparoscopy for para-aortic lymphadenectomy in gynecological malignancies.
Total Blood Loss
All included studies (8, 19–26) reported the data for the perioperative TBL (ml). Data showed an overall lower chance of TBL in robotic as compared to conventional laparoscopy group (MD = −104.2, 95% CI: −218.49 to −79.91; I2 = 98%) (Figure 3). Subgroup analyses suggested a lower chance of TBL in mixed histological population and studies involving extraperitoneal approach (MD = −216.8, 95% CI: −303.3 to −130.4; I2 = 99%), Caucasian population (MD = −80.9, 95% CI: −154.2 to −7.5; I2 = 98%), and non-RCT study design (MD = −245.8, 95% CI: −403.4 to −88.2; I2 = 98%). However, no significant changes in TBL were detected in the robotic group as compared to the conventional laparoscopy group in Asian studies, RCTs studies, transperitoneal approach, and histological types studies (Table 2).
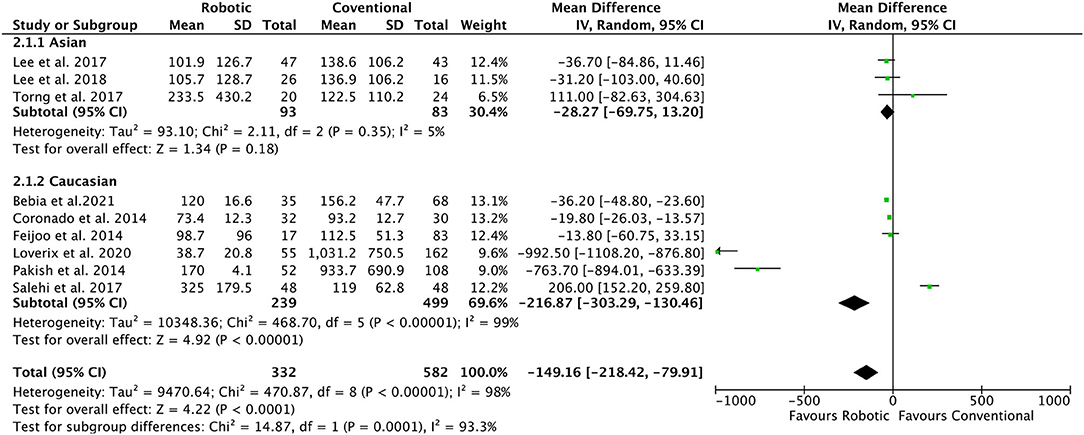
Figure 3. Forest plot of the association of total blood loss (ml) in robotic-assisted vs. conventional laparoscopy for para-aortic lymphadenectomy in gynecological malignancies.
Length of Stay
A total of seven studies (19–22, 24–26) with a total of 664 patients reported the data for the LOS in hospital (days). No significant changes in the LOS were observed in robotics as compared with the conventional laparoscopy group (MD = 0.62, 95%CI: −0.19 to 1.4; I2 = 95%) (Table 2). Subgroup analysis based on ethnicity, types of study, histological type, and lymphadenectomy approach also showed a non-significant change in LOS.
Complication Rate
A total of nine studies (8, 19–26) with 914 patients reported a non-significant change in postoperative complication rate (RR = 0.80, 95% CI:0.45 to 1.42; I2 =45%) in the robotic group as compared to the conventional laparoscopy group (Table 2). Based on ethnicity, stratified analysis also showed a non-significant change in postoperative complication rate (RR = 0.69, 95% CI:0.33 to 1.47; I2 = 56%) in both Caucasian as well as in Asian population (RR = 1.22, 95% CI:0.51 to 2.88; I2 = 0%).
Sensitivity Analysis and Publication Bias
A sensitivity analysis was performed using the leave-one-out method. This method re-evaluates the pooled effect size of the included studies by removing a single study at a time. A significant change in the effect size, measuring the association change in postoperative in the robotic group as compared to the conventional laparoscopy group, was observed when an outlier study by Salehi et al. was removed (20). No significant evidence of publication bias was found. An asymmetrical inverted funnel plot for OT, TBL, LOS, and CR was observed (Figure 4).

Figure 4. Begg's funnel plot of publication bias testing for the association of (A) operation time, (B) total blood loss, (C) length of hospital stay, and (D) complication rate in robotic-assisted vs. conventional laparoscopy for para-aortic lymphadenectomy in gynecological malignancies.
Discussion
The strengths of our study include the fact that, to our knowledge, this is the first systematic review and meta-analysis that compared the robotic vs. conventional laparoscopy approaches for PAL in gynecological maliginacies. In our meta-analysis, a significant decrease in TBL was observed in robot-assisted as compared to conventional laparoscopy. However, no significant differences were noted for OT, CR, and LOS in the overall findings. More operation time was required in the robotic group as compared with the conventional laparoscopy group for studies conducted in the Asian population vs. Caucasian Population and with a transperitoneal approach as compared to the extraperitoneal approach. Further subgroup analysis demonstrated that the robotic group had a lower OT in the mixed histological population and in studies with an extraperitoneal approach. The lower chances of TBL were observed in mixed histological populations and studies involving extraperitoneal approach, Caucasian population, and non-RCT study design. Our findings may aid surgeons in the decision-making for the best surgical approach to treat of gynecological malignancies.
Previous research on the role of extraperitoneal laparoscopic PAL in gynecologic malignancies has demonstrated that this operation is both safe and practical (7, 32, 33). This method has been proven to have few problems and a low likelihood of converting to transperitoneal laparoscopic or open lymphadenectomy (7, 32). A study by Bebia et al. (26) compared transperitoneal or extraperitoneal laparoscopic and transperitoneal robot-assisted approaches to performing PAL. Their study showed that the extraperitoneal robotic approach resulted in fewer complications, even in older patients with high BMI. All examined approaches did not show any differences in aortic lymph node count, operative time, or LOS. Elderly patients affected by gynecological cancer should benefit from individualized treatment. Data, in fact, do not support the premise that age itself is a negative prognostic factor, moreover with the objectivity that elderly patients are able to tolerate the standard of care for gynecological cancers. In this perspective, it is absolutely necessary to overcome the mental bias of not treating the elderly because they are more fragile and have a lower life expectancy than their younger counterparts (34). The advanced technology of robotic-assisted laparoscopy gives advantages for performing these difficult surgical procedures. Many studies had reported their initial experience with robotic surgery and showed its feasibility in endometrial cancer. Postoperative complications were comparable and in contrast to previous retrospective studies, the total health care cost was significantly lower for robotic surgery. The choice of surgical treatment modality will ultimately depend on patient/surgeon preference and institutional resources. Further development of robotic surgery such as intra-operative high-quality navigation and imaging systems, could open fascinating new avenues for PAL in gynecological malignancies.
Another study by Pakish et al. (8) compared the outcomes of extraperitoneal laparoscopic PAL and transperitoneal minimally invasive (laparoscopic or robotic) PAL. They also concluded that extraperitoneal PAL is associated with fewer complications and lower failure rates than transperitoneal PAL, although it is associated with longer operational periods. Our subgroup analyses showed that extraperitoneal robot-assisted approaches had a lower operative time and lesser chance of blood loss (8, 26). We couldn't perform additional analyses for the survival outcome, conversion to laparotomy, change in post-operative hemoglobin concentration and post-operative hospitalization due to the unavailability of data in the included studies (21–23). Additionally, data for the complications using different grades based on the Clavein dindo classification was available for only two studies by Loverix et al. and Salehi et al. for which analysis was not possible (20, 21).
The infrarenal para-aortic area is difficult to approach due to several limitations of the conventional laparoscopic approach, including a steep learning curve due to the unique surgical skills required, high reliance on skilled surgical assistants, the condition of the patient (morbid obesity), or significant intra-abdominal adhesions (35–37). The robotic-assisted approach took less time per infrarenal para-aortic and total lymph nodes retrieved compared to the conventional laparoscopic approach (22). The primary benefits of robotic technology in minimally invasive surgery include enhanced accuracy and precision, articulation of robotic instruments, stereoscopic picture, and surgeon's sitting position (9). Robotic-assisted and conventional laparoscopy provide similar perioperative outcomes other than lower blood loss and a higher number of aortic nodes removed (both without clinical impact) in robotic patients for the performance of extraperitoneal paraaortic lymphadenectomy in patients with locally advanced cervical cancer (24). Pelvic lymphadenectomy involves an extensive compromise of the whole pelvic lymphatic system compared to the removal of the Sentinel lymph node alone. The pelvic nodes are easily accessible using a transperitoneal technique, while the paraaortic nodes are more difficult to reach. Access to the paraaortic nodes is mostly determined by the patient's weight and the surgeon's experience. Since the intestines and omentum retain so much fat, para-aortic lymphadenectomy is more challenging in obese patients. To access the para-aortic nodes, these structures must be mobilized and retracted out of the dissection field. Even in obese patients, an extraperitoneal technique provides excellent exposure to the para-aortic nodes. However, unless additional port sites are implanted, a pelvic lymph node dissection below the level of the common iliac nodes is not conceivable (10, 38). Robotic single-site pelvic lymphadenectomy using bipolar forceps and the monopolar hook is feasible. New developments are needed to improve surgical ergonomics and additional studies should be performed to explore possible benefits of this procedure (39–41).
Our meta-analysis must be interpreted with caution as there are limitations to our findings: (1) The included papers lacked long-term follow-up results, such as the rate of local tumor recurrence or distant metastasis, and survival rate. Only two studies were RCTs, increasing the probability of substantial implementation bias. None of the studies indicated whether outcome evaluators were blinded. That may result in possible measurement bias, especially in subjective outcomes such as length of stay. (2) Sample sizes in the included studies were small. Six out of nine included studies were retrospective which significantly increases the risk of bias for under-reporting complications, especially minor complications. (3) Study participants were at diagnosed with various phases and types of gynecological malignancies and their progression, a parameter which cannot be controlled. (4) Lastly, a high degree of heterogeneity was observed in the overall analysis, possibly due to different study designs, differences in patient populations and surgeons, discharge criteria, and hospital policies regarding the post-operative stay.
Conclusions
Robotic laparoscopy has a significant advantage over the conventional laparoscopy approach for PAL in gynecological malignancies. Further prospective observational studies embedded with a large sample size are needed to validate our findings.
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found at: PubMed Central, Cochrane library, EMBASE, and MEDLINE databases from inception until May 2021 for relevant publications.
Author Contributions
ZZ and JG conceived and designed the study. KY, YZ, QH, and LW were involved in literature search and data collection. ZZ, JG, and YC analyzed the data. YC wrote the article and reviewed and edited the manuscript. All authors read and approved the final manuscript.
Funding
This study was supported by Yunnan Provincial Department of Science and Technology—Project number: 2019FE001 (-296).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.843517/full#supplementary-material
References
1. Gil-Moreno A, Magrina JF, Pérez-Benavente A, Díaz-Feijoo B, Sánchez-Iglesias JL, García A, et al. Location of aortic node metastases in locally advanced cervical cancer. Gynecol Oncol. (2012) 125:312–4. doi: 10.1016/j.ygyno.2012.02.008
2. Bogani G, Dowdy SC, Cliby WA, Ghezzi F, Rossetti D, Mariani A. Role of pelvic and para-aortic lymphadenectomy in endometrial cancer: current evidence. J Obstet Gynaecol Res. (2014) 40:301–11. doi: 10.1111/jog.12344
3. Franké O, Narducci F, Chereau-Ewald E, Orsoni M, Jauffret C, Leblanc E, et al. Role of a double docking to improve lymph node dissection: when robotically assisted laparoscopy for para-aortic lymphadenectomy is associated to a pelvic procedure. Int J Gynecol Cancer. (2015) 25:331–6. doi: 10.1097/IGC.0000000000000338
4. AlHilli MM, Mariani A. The role of para-aortic lymphadenectomy in endometrial cancer. Int J Clin Oncol. (2013) 18:193–9. doi: 10.1007/s10147-013-0528-7
5. Dargent D, Chabert P, Bretones S, Martin X. [Laparoscopic staging before treatment of advanced uterine cancer: evaluation in two stages or direct lumbar-aortic evaluation?]. Contracept Fertil Sex. (1997) 25:IV–X.
6. Dowdy SC, Aletti G, Cliby WA, Podratz KC, Mariani A. Extra-peritoneal laparoscopic para-aortic lymphadenectomy–a prospective cohort study of 293 patients with endometrial cancer. Gynecol Oncol. (2008) 111:418–24. doi: 10.1016/j.ygyno.2008.08.021
7. Nagao S, Fujiwara K, Kagawa R, Kozuka Y, Oda T, Maehata K, et al. Feasibility of extraperitoneal laparoscopic para-aortic and common iliac lymphadenectomy. Gynecol Oncol. (2006) 103:732–5. doi: 10.1016/j.ygyno.2006.04.026
8. Pakish J, Soliman PT, Frumovitz M, Westin SN, Schmeler KM, Reis RD, et al. Comparison of extraperitoneal versus transperitoneal laparoscopic or robotic para-aortic lymphadenectomy for staging of endometrial carcinoma. Gynecol Oncol. (2014) 132:366–71. doi: 10.1016/j.ygyno.2013.12.019
9. Magrina JF, Long JB, Kho RM, Giles DL, Montero RP, Magtibay PM. Robotic transperitoneal infrarenal aortic lymphadenectomy: technique and results. Int J Gynecol Cancer. (2010) 20:184–7. doi: 10.1111/IGC.0b013e3181c208e4
10. May K, Bryant A, Dickinson HO, Kehoe S, Morrison J. Lymphadenectomy for the management of endometrial cancer. Cochrane Database Syst Rev. (2010) 20:CD007585. doi: 10.1002/14651858
11. Frost JA, Webster KE, Bryant A, Morrison J. Lymphadenectomy for the management of endometrial cancer. Cochrane Database Syst Rev. (2017) 10:CD007585. doi: 10.1002/14651858.CD007585.pub4
12. Leitao MM, Bartashnik A, Wagner I, Lee SJ, Caroline A, Hoskins WJ, et al. Cost-effectiveness analysis of robotically assisted laparoscopy for newly diagnosed uterine cancers. Obstet Gynecol. (2014) 123:1031–7. doi: 10.1097/AOG.0000000000000223
13. Vizza E, Corrado G, Zanagnolo V, Tomaselli T, Cutillo G, Mancini E, et al. Neoadjuvant chemotherapy followed by robotic radical hysterectomy in locally advanced cervical cancer: A multi-institution study. Gynecol Oncol. (2014) 133:180–5. doi: 10.1016/j.ygyno.2014.02.035
14. Lavoue V, Zeng X, Lau S, Press JZ, Abitbol J, Gotlieb R, et al. Impact of robotics on the outcome of elderly patients with endometrial cancer. Gynecol Oncol. (2014) 133:556–62. doi: 10.1016/j.ygyno.2014.03.572
15. James JA, Rakowski JA, Jeppson CN, Stavitzski NM, Ahmad S, Holloway RW. Robotic transperitoneal infra-renal aortic lymphadenectomy in early-stage endometrial cancer. Gynecol Oncol. (2015) 136:285–92. doi: 10.1016/j.ygyno.2014.12.028
16. Morris B. Robotic surgery: Applications, limitations, and impact on surgical education. MedGenMed Medscape Gen Med. (2005) 7:72.
17. Stewart KI, Fader AN. New developments in minimally invasive gynecologic oncology surgery. Clin Obstet Gynecol. (2017) 60:330–48. doi: 10.1097/GRF.0000000000000286
18. Clair KH, Tewari KS. Robotic surgery for gynecologic cancers: indications, techniques and controversies. J Obstet Gynaecol Res. (2020) 46:828–43. doi: 10.1111/jog.14228
19. Torng P-L, Pan S-P, Hwang J-S, Shih H-J, Chen C-L. Learning curve in concurrent application of laparoscopic and robotic-assisted hysterectomy with lymphadenectomy in endometrial cancer. Taiwan J Obstet Gynecol. (2017) 56:781–7. doi: 10.1016/j.tjog.2017.10.014
20. Salehi S, Åvall-Lundqvist E, Legerstam B, Carlson JW, Falconer H. Robot-assisted laparoscopy versus laparotomy for infrarenal paraaortic lymphadenectomy in women with high-risk endometrial cancer: A randomised controlled trial. Eur J Cancer. (2017) 79:81–89. doi: 10.1016/j.ejca.2017.03.038
21. Loverix L, Salihi RR, Van Nieuwenhuysen E, Concin N, Han S, van Gorp T, et al. Para-aortic lymph node surgical staging in locally-advanced cervical cancer: comparison between robotic versus conventional laparoscopy. Int J Gynecol Cancer. (2020) 30:466–72. doi: 10.1136/ijgc-2019-000961
22. Lee HJ, Lee YH, Chong GO, Hong DG, Lee YS. Comparison of robotic-assisted versus laparoscopy for transperitoneal infrarenal para-aortic lymphadenectomy in patients with endometrial cancer. J Obstet Gynaecol Res. (2018) 44:547–55. doi: 10.1111/jog.13535
23. Lee HJ, Lee YH, Chong GO, Hong DG, Lee YS. Robotic-assisted Transperitoneal Infrarenal Para-aortic Lymphadenectomy for gynecological malignancies: comparison with a laparoscopic approach. Anticancer Res. (2017) 37:7087–93. doi: 10.21873/anticanres.12182
24. Díaz-Feijoo B, Gil-Ibáñez B, Pérez-Benavente A, Martínez-Gómez X, Colás E, Sánchez-Iglesias JL, et al. Comparison of robotic-assisted vs conventional laparoscopy for extraperitoneal paraaortic lymphadenectomy. Gynecol Oncol. (2014) 132:98–101. doi: 10.1016/j.ygyno.2013.11.004
25. Coronado PJ, Fasero M, Magrina JF, Herraiz MA, Vidart JA. Comparison of perioperative outcomes and cost between robotic-assisted and conventional laparoscopy for transperitoneal infrarenal para-aortic lymphadenectomy (TIPAL). J Minim Invasive Gynecol. (2014) 21:674–81. doi: 10.1016/j.jmig.2014.01.023
26. Bebia V, Gil-Moreno A, Hernández A, Gilabert-Estellés J, Franco-Camps S, de la Torre J, et al. Robot-assisted extraperitoneal para-aortic lymphadenectomy is associated with fewer surgical complications: A post hoc analysis of the STELLA-2 Randomized Trial. J Minim Invasive Gynecol. (2021) 28:2004–12.e1. doi: 10.1016/j.jmig.2021.05.009
27. Mäenpää MM, Nieminen K, Tomás EI, Laurila M, Luukkaala TH, Mäenpää JU. Robotic-assisted vs traditional laparoscopic surgery for endometrial cancer: A randomized controlled trial. Am J Obstet Gynecol. (2016) 215:588.e1–e7. doi: 10.1016/j.ajog.2016.06.005
28. Kansagara D, O'Neil M, Nugent S, Freeman M, Low A, Kondo K, et al. Quality Assessment Criteria for Observational Studies, Based on the Newcastle-Ottawa Scale (2017). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK476448/table/appc.t4/ (accessed August 16, 2021).
29. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. (1994) 50:1088–101. doi: 10.2307/2533446
30. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
31. Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. (2014) 14:135. doi: 10.1186/1471-2288-14-135
32. Dargent D, Ansquer Y, Mathevet P. Technical development and results of left extraperitoneal laparoscopic paraaortic lymphadenectomy for cervical cancer. Gynecol Oncol. (2000) 77:87–92. doi: 10.1006/gyno.1999.5585
33. Benito V, Lubrano A, Arencibia O, Andújar M, Pinar B, Medina N, et al. Laparoscopic extraperitoneal para-aortic lymphadenectomy in the staging of locally advanced cervical cancer: is it a feasible procedure at a peripheral center? Int J Gynecol Cancer. (2012) 22:332–6. doi: 10.1097/IGC.0b013e31823c241b
34. Vitale SG, Capriglione S, Zito G, Lopez S, Gulino FA, Di Guardo F, et al. Management of endometrial, ovarian and cervical cancer in the elderly: current approach to a challenging condition. Arch Gynecol Obstet. (2019) 299:299–315. doi: 10.1007/s00404-018-5006-z
35. Childers JM, Hatch KD, Tran AN, Surwit EA. Laparoscopic para-aortic lymphadenectomy in gynecologic malignancies. Obstet Gynecol. (1993) 82:741–7.
36. Querleu D. Laparoscopic paraaortic node sampling in gynecologic oncology: A preliminary experience. Gynecol Oncol. (1993) 49:24–9. doi: 10.1006/gyno.1993.1080
37. Spirtos NM, Schlaerth JB, Spirtos TW, Schlaerth AC, Indman PD, Kimball RE. Laparoscopic bilateral pelvic and paraaortic lymph node sampling: An evolving technique. Am J Obstet Gynecol. (1995) 173:105–11. doi: 10.1016/0002-9378(95)90177-9
38. Kehoe SM, Abu-Rustum NR. Transperitoneal laparoscopic pelvic and paraaortic lymphadenectomy in gynecologic cancers. Curr Treat Options Oncol. (2006) 7:93–101. doi: 10.1007/s11864-006-0044-3
39. Tateo S, Nozza A, Del Pezzo C, Mereu L. Robotic single-site pelvic lymphadenectomy. Gynecol Oncol. (2014) 134:631. doi: 10.1016/j.ygyno.2014.06.027
40. Rumolo V, Rosati A, Tropea A, Biondi A, Scambia G. Senhance robotic platform for gynecologic surgery: A review of literature. Updat Surg. (2019) 71:419–27. doi: 10.1007/s13304-018-00620-1
41. Capozzi VA, Riemma G, Rosati A, Vargiu V, Granese R, Ercoli A, et al. Surgical complications occurring during minimally invasive sentinel lymph node detection in endometrial cancer patients. A systematic review of the literature and metanalysis. Eur J Surg Oncol. (2021) 47:2142–9. doi: 10.1016/j.ejso.2021.03.253
Keywords: robotic-assisted laparoscopy, extraperitoneal paraaortic lymphadenectomy, cervical cancer, conventional laparoscopy, gynecological malignancies
Citation: Zhou Z, Ge J, Ye K, Zhang Y, Hu Q, Wang L and Chen Y (2023) Comparison of Robotic-Assisted vs. Conventional Laparoscopy for Para-aortic Lymphadenectomy in Gynecological Malignancies: A Systematic Review and Meta-Analysis. Front. Surg. 9:843517. doi: 10.3389/fsurg.2022.843517
Received: 26 December 2021; Accepted: 02 March 2022;
Published: 04 January 2023.
Edited by:
Andrea Rosati, Agostino Gemelli University Polyclinic (IRCCS), ItalyReviewed by:
Carlo Ronsini, Università degli Studi della Campania “Luigi Vanvitelli”, ItalyAntonio Simone Laganà, University of Insubria, Italy
Matteo Pavone, Agostino Gemelli University Polyclinic (IRCCS), Italy
Copyright © 2023 Zhou, Ge, Ye, Zhang, Hu, Wang and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yiwen Chen, a215d2NoZW5AMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Zhengli Zhou†
Zhengli Zhou† Yiwen Chen
Yiwen Chen