
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Surg. , 22 March 2022
Sec. Orthopedic Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.834551
This article is part of the Research Topic Advancing the Understanding of Surgical Management for Degenerative Spine Conditions View all 18 articles
Study Design: Narrative review.
Objective: The purpose of this review was to consolidate the current literature related to ponticulus posticus (PP) and to improve the systematic understanding of this anatomical variant of atlas among spine surgeons.
Methods: Articles reviewed were searched in PubMed, Ovid MEDLINE, and Embase. All articles of any study design discussing on PP were considered for inclusion. Two independent authors read article titles and abstracts and included appropriate articles. The relevant articles were studied in full text.
Results: A total of 113 literatures were reviewed and consolidated in this narrative review. These articles are roughly divided into the following five subcategories: (1) epidemiology, (2) pathology and anatomy, (3) clinical presentation, (4) surgical significance, and (5) radiographic examination.
Conclusion: The PP is non-negligible with a high prevalence. The PP compresses the V3 segment of the artery, the suboccipital nerve, and the venous plexus, consequently contributing to the incidence of neurological pathologies. When a PP is observed or suspected on a lateral radiograph, we recommend that a computed tomography (CT) scan of a patient who is about to receive a C1 lateral mass screw (C1LMS) should be performed, which could determine a safe entry point and the right trajectory of screw insertion.
Ponticulus posticus (PP) is the meaning of “little posterior bridge” in Latin, which was a variation occurring on the atlas vertebra. It was defined as a bony bridge formed between the posterior portion of the superior articular process and the lateral portion of the upper margin of the posterior arch of the atlas, surrounding all or part of the vertebral artery (VA) (1). It was first detected on imaging incidentally and was reported in the dentistry, neurosurgery, and orthopedic spinal surgery literature (2).
Ponticulus posticus has not been a matter of concern for spine surgeons until an increasing number of epidemiology studies indicated its non-negligible morbidity. More published studies showed a close connection between PP and cervicogenic headache (CGH) (3). Surgical significance of PP in the insertion of screws into the lateral mass of the atlas was also reported (4). A practical, narrative review of PP was undertaken to address the following areas: (1) epidemiology, (2) pathology and anatomy, (3) clinical presentation, (4) surgical significance, and (5) radiographic examination. Not only did it provide an extensive systematic review of all recent studies, we would rather aim to provide an updated comprehensive synthesis of the current evidence to facilitate a cogent clinical understanding of PP, which could guide spine surgeons in the condition of cervical spine disorders combined with PP.
A comprehensive literature search was performed on November 01, 2021 according to the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines. Studies published from 1950 to 2021 were chosen through relevant PubMed, Ovid MEDLINE, and Embase searches to prioritize the largest and most recent studies. The Medical Subject headings and Boolean operators employed for this search were: “ponticulus posticus” or “posticus ponticus” or “foramen arcuate” or “foramen arcuale” or “foramen sagittale” or “foramen atlantoideum posterior” or “Kimmerle's anomaly” or “foramen retroarticulare superior” or “canalis vertebralis” or “retroarticular vertebral artery ring” or “retroarticular canal” or “retrocondylar vertebral artery”. Though no strict inclusion/exclusion criteria were used, preference was given to well-known, large, multi-institution databases that represented care across many centers, in addition to larger single-center studies. All articles about study design discussing about PP were considered for inclusion. Experimental or animal studies, non-English language studies, non-peer-reviewed studies, conference abstracts, paper, letter, and unpublished manuscripts were excluded. After an initial screen of abstracts and article titles, we obtained full-text articles of all potential studies. To perfect the research, two independent researchers reviewed and evaluated the included articles, respectively. Any different opinions were discussed until a consensus was reached. Since no human subjects were directly involved in this article; hence, an IRB statement was not needed.
A total of 172 studies were identified from the initial search, of which 28 duplicates and 11 non-English language articles were removed. Titles and abstracts of the rest 133 studies were screened according to the predefined inclusion criteria, and 20 studies were excluded. In total, 113 articles were critically reviewed and consolidated for this literature review (Figure 1).
Ponticulus posticus is a normal anatomical variant of atlas vertebrae (C1), and its prevalence in population has been the focus in PP studies. In the current study, we updated the studies on the prevalence of PP in various areas of the world, and a total of 58 published studies were included in the narrative review (Table 1). According to the review, we found that the total prevalence of these studies was 5–55.7%, and there were some regional differences in the prevalence. The prevalence in East Asia was 6.2–19.0%, Europe was 14.3–34.7%, North America was 5–45.5%, and India was 10.9–37.8%, of which East Asia had the lowest incidence. These differences could be attributed to the differences in the different ethnic groups all over the world. Some scholars argued that the degenerative changes may be the cause of PP, and prevalence increases with age due to calcification, but there was no definitive evidence for association between the age and the prevalence of PP. Several recent studies did not find a statistically significant association between the age and the presence of PP (7–9). With regard to sex bias, scholars hold different views. In studies conducted by Takaaki, Paraskevas, Hong, and Saleh, the frequency of PP was higher in men (9–12). In contrast, the studies conducted by Schilling et al. (2010) and Tambawala et al. reported female predilection for this anomaly (13, 14). More studies showed that there was no statistically significant association between gender of the patient and the presence of PP (7, 8, 15, 16). The currently available literature was inconclusive in this aspect. According to Pekala's meta-analysis of 55,985 subjects, the total prevalence of the incomplete PP was 13.6%, which was higher than the complete one (9.1%) (3). However, the meta-analysis performed by Elliott and Tanweer (17) found complete PP in 9.3% of patients and incomplete PP in 8.7% of patients. The difference of study results may be attributed to the methods employed, and we could not reach a definitive conclusion in this aspect. In terms of laterality, the study conducted by Saleh et al. (9) indicated that the left sided arch has a higher rate of PP than the right one (84.7 vs. 89.2%), which was consistent with the findings made in the study of Elliott and Tanweer (17).
Ponticulus posticus is an osseous prominence formed in place of a sulcus for the VA on the posterior arch of the atlas. The atlas with a particular anatomy is composed with a short anterior arch and a longer posterior arch, which is a ring-shaped structure without vertebral body. The vertebral artery groove (VAG) is on the superior surface of the posterior arch (18, 19). PP is an aperture formed by the presence of a bony bridge on the VAG, which is placed posteriorly in relation to the anterior surface, and when the bridge is placed laterally, it is called ponticulus lateralis (PL) – a rare type of PP.
The prevalence of PL was reported to be 1.8–3.8% lower than PP (20–23). PL is difficult to be identified from anteroposterior and lateral radiographs and was rarely reported in previous literature as a result. The V3 segment of the VA travels in the VAG, which is covered by a bony ridge with the presence of PP. According to our literature review, the prevailing view was that PP compresses the V3 segment of the VA and causes alternations of the blood flow within the VAs that are ultimately responsible for a range of symptoms such as migraine and CGH. More than 50% of head rotation occurred at the atlantoaxial joint. With additional compression caused by PP, VA is more susceptible to injury when subjected to compression and extension (24). According to the study of atlas vertebrae from the population of northern Greece by Paraskevas et al., there was a high incidence of the coexistence of PP with retrotransverse forame. (11). It reported that the blood flow was directed into the small vein connecting the atlanto-occipital and the atlanto-axoidian venous sinus due to the compression of the vertebral veins in PP. This study also found that 93.5% cases of PP were accompanied by deeply excavated contralateral groove of the VA, which could be interpreted as evidence that, due to VA compression in the canal, the contralateral VA was dilated, causing an increase in the depth of the corresponding groove. In the study of cadaver conducted by Tubbs et al., all specimens with PP were also found to have gross compression of the VA as it traveled through the PP (25).
From an anatomical point of view, PP compresses the V3 segment of the artery, the suboccipital nerve, and the venous plexus, consequently contributing to the incidence of neurological pathologies such as vertigo and migraine (26). Pekala conducted a meta-analysis in 2018, finding a significant association between PP and headaches (3). Besides, the probability of complete PP resulting in headaches was higher than the incomplete ones, which in turn had a higher probability of headache compared to patients without PP. This result indicated the importance of PP in the etiology of headaches, which was supported by multiple prior studies (14, 27–29). Except for headaches, PP could cause a range of symptoms including retro-orbital pain, vasomotor disturbance of the face and recurrent disturbances of vision, swallowing, and phonation—the Barre–Lieou syndrome caused by alteration of the blood flow within the vertebral arteries, and an associated disturbance of the periarterial nerve plexus (30).
The study by Pearce (2004) introduced the ponticulus resection to treat the Barre–Lieou syndrome caused by PP (30). The patients who had surgical resection of PP during the last 10 years were reviewed and satisfactory surgical outcomes were found. However, we could not find any studies on this topic in recent years. We conjectured that few patients with the Barre–Lieou syndrome were serious enough to require surgical resection.
In addition to neurological pathologies, PP is associated with oral and maxillofacial disorders. This may be attributed to the activity of the neural crest as the common embryonic origin of the neck and shoulder skeletal development and the origin of development of tooth and midface skeletal fields (31, 32). According to the study conducted by Dadgar et al., the presence of the PP correlated with the presence of palatally displaced canines (PDC) significantly and positively (33). The study by Leonardi et al. (31) reached a converging conclusion in which 34.2% of patients with PDC showed PP as opposed to the group of normal population (20%) (34). Bayrakdar et al. found that there was a significant association between PP and cleft lip (35). In this study, the incidence of PP in the cleft-palate group was 22.2% compared to 9% in normal group.
We noticed that there were several methodologies to identify the PP in previous studies including cadaveric studies, lateral radiographs, and computed tomography (CT) scans. In our study, we found that the prevalence of PP in different studies was different, which may be contributed to the methodologies. In the radiographic examination, lateral radiographs could not identify the laterality, completeness, and sometimes even the presence of PP. In the study by Kim et al., the prevalence of PP was 26% based on the CT scans, which was only 14% in lateral radiographs (36). The difference was significant and meant that a substantial proportion of patients with PP were missed on lateral radiographs. The CT scan was still a reliable method when PP was combined with other anatomical variant. Figure 2 shows a typical case. Elgafy et al. reported a special CT finding of ipsilateral PP and high-riding VA, which were found only in 5 patients out of 100 cases (37).
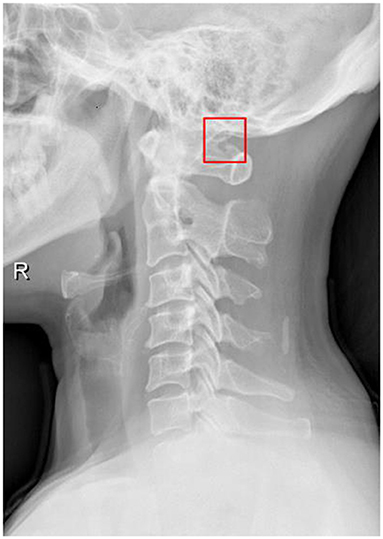
Figure 2. A 44-year-old female with migraine and normal neurologic examination. Lateral radiograph showed the right-sided partial ponticulus posticus, an anomalous bony bridge formed from the superior articulating surface of the atlas but not fused to the posterior arch of the atlas.
Radiographically, the most common classification of PP was based on the completeness of the bony bridge: none, complete, and incomplete. None type: there was no formed bony bridge; complete type: a complete bony ring was formed; and incomplete type: some portions of the bony ring were defective. However, this traditional classification neglected the laterality of PP, and there was a novel classification system introduced by Saleh et al. (9). This classification consisted of a two-letter designation for each patient, including either A, B, or C (A means no PP; B means incomplete PP; and C means complete PP). The first letter described the right-sided posterior arch, and the second letter described the left one. This classification system included 9 potential subtypes for all patients: AA, BB, CC, AB, AC, BA, BC, CA, and CB. However, we could not find a classification that combines clinical symptoms with imaging findings.
The C1 lateral mass screw (C1LMS) insertion was firstly reported by Goel and Laheri in 1994, which revolutionized the treatment of atlantoaxial instability (38). PP has gained increasing attention in recent years, and the literature has increased correspondingly as C1LMS has become increasingly popular. When the methods of inserting the C1LMS is through the posterior arch into the lateral mass, PP may be mistaken for a thickened posterior arch and may mislead the surgeon to drill the borehole too superiorly, which could cause iatrogenic injury to the V3 segment of the artery. Zhang et al. successfully inserted C1LMS in 11 patients with PP by performing preoperative three-dimensional CT reconstructive imaging, which contributed to choose an appropriate entry point and a right trajectory of screw insertion (39). Arslan et al. developed cervical column 3D models for 200 patients, of which 29 were with PP, and evaluated 3D models of both normal and PP cases (6). They found that the VA in PP cases was clearly narrower than that in normal cases, and the safe distance between lateral mass screw fixation and the bony bridge was 4 mm.
The conventional C1LMSs have been accepted as more stable approaches to avoid VA injury compared with C1LMSs inserted via the posterior arch because the screws are placed farther from the VAG. However, the study by Song et al. indicated that the latter had some anatomical feasibility and advantage with the relatively sufficient VAG height (40). In addition, the lower margin of the C1 arch could determine an appropriate entry point. The disadvantage of the conventional C1LMSs included more venous bleeding, less biomechanical stability, and postoperative C2 nerve dysfunction.
In the study conducted by Yeom et al., 9 patients with PP received C1LMS, and 3 of whom received resection of the ponticulus before the screw insertion due to wide PP and deep VAG (41). Although VA injury was not reported in this study, we did not advocate this radical surgery strategy. Notably, Lee et al. reported the notching technique (lateral mass screws inserted partially through the posterior arch), which modified the entry point to make the screw remote from the greater occipital nerve and was possible in the vast majority of patients (42).
Considering different methodologies and regional differences, the prevalence of PP is inconsistent. However, one point is certain, PP is non-negligible with a high prevalence. PP compresses the V3 segment of the artery, the suboccipital nerve, and the venous plexus, consequently contributing to the incidence of neurological pathologies. When a PP is observed or suspected on a lateral radiograph, we recommend that a CT scan of a patient who is about to receive a C1LMS should be performed, which could determine a safe entry point and a right trajectory of screw insertion. The insertion of C1LMSs via the posterior arch was applicable in the majority of cases, and the notching technique might be considered as necessary. Conventional C1LMSs should not be recommended due to the surgical risk and the postoperative complications.
MY, XX, and YZ: conceptualization, methodology, formal analysis, and writing-original draft. WM: resources and data curation. XD and JM: supervision and writing-reviewing and editing. All authors read and approved the final manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We would like to thank the reviewers for their thorough review of our manuscript, especially under the severe circumstance of worldwide epidemic COVID-19, and we wish that everybody pulls through safe and sound.
PP, ponticulus posticus; C1LMS, C1 lateral mass screw; CGH, cervicogenic headache; PDC, palatally displaced canines; PL, ponticulus lateralis; VAG, vertebral artery groove.
1. Dugdale LM. The ponticulus posterior of the atlas. Australas Radiol. (1981) 25:237–8. doi: 10.1111/j.1440-1673.1981.tb02254.x
2. Ahn J, Duran M, Syldort S, Rizvi A, D'Antoni AV, Johal J, et al. Arcuate foramen: anatomy, embryology, nomenclature, pathology, and surgical considerations. World Neurosurg. (2018) 118:197–202. doi: 10.1016/j.wneu.2018.07.038
3. Pekala PA, Henry BM, Phan K, Pekala JR, Taterra D, Walocha JA, et al. Presence of a foramen arcuale as a possible cause for headaches and migraine: systematic review and meta-analysis. J Clin Neurosci. (2018) 54:113–8. doi: 10.1016/j.jocn.2018.05.008
4. Young JP, Young PH, Ackermann MJ, Anderson PA, Riew KD. The ponticulus posticus: implications for screw insertion into the first cervical lateral mass. J Bone Joint Surg Am. (2005) 87:2495–8. doi: 10.2106/00004623-200511000-00017
5. Stubbs DM. The arcuate foramen. Variability in distribution related to race and sex. Spine. (1992) 17:1502–4. doi: 10.1097/00007632-199212000-00010
6. Arslan D, Ozer MA, Govsa F, Kitis O. The Ponticulus Posticus as Risk Factor for Screw Insertion into the First Cervical Lateral Mass. World Neurosurg. (2018) 113:e579–85. doi: 10.1016/j.wneu.2018.02.100
7. Chen CH, Chen YK, Wang CK. Prevalence of ponticuli posticus among patients referred for dental examinations by cone-beam CT. Spine J. (2015) 15:1270–6. doi: 10.1016/j.spinee.2015.02.031
8. Giri J, Pokharel PR, Gyawali R. How common is ponticulus posticus on lateral cephalograms? BMC Res Notes. (2017) 10:172. doi: 10.1186/s13104-017-2494-z
9. Saleh A, Gruber J, Bakhsh W, Rubery PT, Mesfin A. How Common Is the Ponticulus Posticus?: A Computed Tomography Based Analysis of 2917 Patients. Spine. (2018) 43:E436–41. doi: 10.1097/BRS.0000000000002400
10. Najmuddin M. Prevalence of ponticulus posticus on the posterior arch of the atlas in symptomatic and asymptomatic patients. Oral Radiol. (2022) 1–4. doi: 10.1007/s11282-021-00583-x
11. Paraskevas G, Papaziogas B, Tsonidis C, Kapetanos G. Gross morphology of the bridges over the vertebral artery groove on the atlas. Surg Radiol Anat. (2005) 27:129–36. doi: 10.1007/s00276-004-0300-9
12. Hong JT, Lee SW, Son BC, Sung JH, Yang SH, Kim IS, et al. Analysis of anatomical variations of bone and vascular structures around the posterior atlantal arch using three-dimensional computed tomography angiography. J Neurosurg Spine. (2008) 8:230–6. doi: 10.3171/SPI/2008/8/3/230
13. Tambawala SS, Karjodkar FR, Sansare K, Motghare D, Mishra I, Gaikwad S, et al. Prevalence of Ponticulus Posticus on Lateral Cephalometric Radiographs, its Association with Cervicogenic Headache and a Review of Literature. World Neurosurg. (2017) 103:566–75. doi: 10.1016/j.wneu.2017.04.030
14. Chitroda PK, Katti G, Baba IA, Najmudin M, Ghali SR, Kalmath B. Ponticulus posticus on the posterior arch of atlas, prevalence analysis in symptomatic and asymptomatic patients of gulbarga population. J Clin Diagn Res. (2013) 7:3044–7. doi: 10.7860/JCDR/2013/6795.3847
15. Cho YJ. Radiological analysis of ponticulus posticus in Koreans. Yonsei Med J. (2009) 50:45–9. doi: 10.3349/ymj.2009.50.1.45
16. Gibelli D, Cappella A, Cerutti E, Spagnoli L, Dolci C, Sforza C. Prevalence of ponticulus posticus in a Northern Italian orthodontic population: a lateral cephalometric study. Surg Radiol Anat. (2016) 38:309–12. doi: 10.1007/s00276-015-1554-0
17. Elliott RE, Tanweer O. The prevalence of the ponticulus posticus (arcuate foramen) and its importance in the Goel-Harms procedure: meta-analysis and review of the literature. World Neurosurg. (2014) 82:e335–343. doi: 10.1016/j.wneu.2013.09.014
18. Aksoy S, Yalcin B. Morphometric anatomy of the posterior aspect of the atlas and the vertebral artery groove in relation to lateral mass screw placement. J Neurol Surg A Cent Eur Neurosurg. (2021). doi: 10.1055/s-0041-1739214
19. Yeom JS, Buchowski JM, Park KW, Chang BS, Lee CK, Riew KD. Undetected vertebral artery groove and foramen violations during C1 lateral mass and C2 pedicle screw placement. Spine. (2008) 33:E942–9. doi: 10.1097/BRS.0b013e3181870441
20. Ozdemir B, Kanat A, Durmaz S, Ersegun Batcik O, Gundogdu H. Introducing a new possible predisposing risk factor for odontoid type 2 fractures after cervical trauma; Ponticulus posticus anomaly of C1 vertebra. J Clin Neurosci. (2022) 96:194–8. doi: 10.1016/j.jocn.2021.11.013
21. Le Minor JM, Trost O. Bony ponticles of the atlas (C1) over the groove for the vertebral artery in humans and primates: polymorphism and evolutionary trends. Am J Phys Anthropol. (2004) 125:16–29. doi: 10.1002/ajpa.10270
22. Kazan S, Yildirim F, Sindel M, Tuncer R. Anatomical evaluation of the groove for the vertebral artery in the axis vertebrae for atlanto-axial transarticular screw fixation technique. Clin Anat. (2000) 13:237–43. doi: 10.1002/1098-2353(2000)13:4<237::AID-CA2>3.0.CO;2-K
23. Radojevic S, Negovanovic B. The Vertebral Groove and Bone Rings of the Vertebral Artery of the Atlas (Anatomical and Radiological Study). Acta Anat (Basel). (1963) 55:186–94.
24. Isaji T, Yasuda M, Kawaguchi R, et al. Posterior inferior cerebellar artery with an extradural origin from the V3 segment: higher incidence on the nondominant vertebral artery. J Neurosurg Spine. (2018) 28:154–9. doi: 10.3171/2017.5.SPINE161286
25. Tubbs RS, Johnson PC, Shoja MM, Loukas M, Oakes WJ. Foramen arcuale: anatomical study and review of the literature. J Neurosurg Spine. (2007) 6:31–4. doi: 10.3171/spi.2007.6.1.6
26. Natsis K, Piperaki ET, Fratzoglou M, Lazaridis N, Tsitsopoulos PP, Samolis, et al. Atlas posterior arch and vertebral artery's groove variants: a classification, morphometric study, clinical and surgical implications. Surg Radiol Anat. (2019) 41:985–1001. doi: 10.1007/s00276-019-02256-1
27. Donald PM, Nagraj SK, Pallivathukkal RG, Ismail ARB. Ponticulus posticus of atlas vertebrae: an incidental finding in Malaysian orthodontic patients. BMJ Case Rep. (2017) 1–3. doi: 10.1136/bcr-2017-220851
28. Haji Ghadimi M, Amini F, Hamedi S, Rakhshan V. Associations among sella turcica bridging, atlas arcuate foramen (ponticulus posticus) development, atlas posterior arch deficiency, and the occurrence of palatally displaced canine impaction. Am J Orthod Dentofacial Orthop. (2017) 151:513–20. doi: 10.1016/j.ajodo.2016.08.024
29. Rios L, Mata-Escolano F, Blanco-Perez E, Llido S, Bastir M, Sanchis-Gimeno JA. Acute headache attributed to whiplash in arcuate foramen and non-arcuate foramen subjects. Eur Spine J. (2017) 26:1262–5. doi: 10.1007/s00586-016-4856-y
31. Putrino A, Leonardi RM, Barbato E, Galluccio G. The association between ponticulus posticus and dental agenesis: a retrospective study. Open Dent J. (2018) 12:510–9. doi: 10.2174/1874210601812010510
32. Kaya Y, Oztas E, Goymen M, Keskin S. Sella turcica bridging and ponticulus posticus calcification in subjects with different dental anomalies. Am J Orthod Dentofacial Orthop. (2021) 159:627–34. doi: 10.1016/j.ajodo.2019.11.024
33. Dadgar S, Alimohamadi M, Rajabi N, Rakhshan V, Sobouti F. Associations among palatal impaction of canine, sella turcica bridging, and ponticulus posticus (atlas arcuate foramen). Surg Radiol Anat. (2021) 43:93–9. doi: 10.1007/s00276-020-02548-x
34. Leonardi R, Barbato E, Vichi M, Caltabiano M. Skeletal anomalies and normal variants in patients with palatally displaced canines. Angle Orthod. (2009) 79:727–32. doi: 10.2319/082408-448.1
35. Bayrakdar IS, Yasa Y, Duman SB, Karaturgut UE, Ocak A, Gunen Yilmaz S. Cone beam computed tomography evaluation of ponticulus posticus in patients with cleft lip and palate: a retrospective radio-anatomic study. Folia Morphol (Warsz). (2018) 77:72–8. doi: 10.5603/FM.a2017.0076
36. Kim KH, Park KW, Manh TH, Yeom JS, Chang BS, Lee CK. Prevalence and morphologic features of ponticulus posticus in Koreans: analysis of 312 radiographs and 225 three-dimensional CT scans. Asian Spine J. (2007) 1:27–31. doi: 10.4184/asj.2007.1.1.27
37. Elgafy H, Pompo F, Vela R, Elsamaloty HM. Ipsilateral arcuate foramen and high-riding vertebral artery: implication on C1-C2 instrumentation. Spine J. (2014) 14:1351–5. doi: 10.1016/j.spinee.2014.01.054
38. Goel A, Laheri V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir (Wien). (1994) 129:47–53. doi: 10.1007/BF01400872
39. Zhang XL, Huang DG, Wang XD, Zhu JW, Li YB, He BR, et al. The feasibility of inserting a C1 pedicle screw in patients with ponticulus posticus: a retrospective analysis of eleven patients. Eur Spine J. (2017) 26:1058–63. doi: 10.1007/s00586-016-4589-y
40. Song MS, Lee HJ, Kim JT, Kim JH, Hong JT. Ponticulus posticus: Morphometric analysis and Its anatomical Implications for occipito-cervical fusion. Clin Neurol Neurosurg. (2017) 157:76–81. doi: 10.1016/j.clineuro.2017.04.001
41. Yeom JS, Kafle D, Nguyen NQ, Noh W, Park KW, Chang BS, et al. Routine insertion of the lateral mass screw via the posterior arch for C1 fixation: feasibility and related complications. Spine J. (2012) 12:476–83. doi: 10.1016/j.spinee.2012.06.010
Keywords: ponticulus posticus (PP), research progress, narrative review, clinical presentation, surgical significance
Citation: Xu X, Zhu Y, Ding X, Yin M, Mo W and Ma J (2022) Research Progress of Ponticulus Posticus: A Narrative Literature Review. Front. Surg. 9:834551. doi: 10.3389/fsurg.2022.834551
Received: 13 December 2021; Accepted: 17 February 2022;
Published: 22 March 2022.
Edited by:
Lingxiao Chen, The University of Sydney, AustraliaReviewed by:
Konstantinos Markatos, Salamina Medical Center, GreeceCopyright © 2022 Xu, Zhu, Ding, Yin, Mo and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mengchen Yin, eWlubWVuZ2NoZW4wNTEzQDEyNi5jb20=; Wen Mo, bXcyMjE4QDEyNi5jb20=; Junming Ma, anVubWluZzIzNkAxMjYuY29t
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.