- 1Department of Orthopedics, The Central Hospital of Wuhan, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430014, China
- 2Department of Orthopedics, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430022, China
Background: The purpose of this study was to compare total complications, complications stratified by type, readmissions, and reoperations at 30 and 90 days after outpatient and standard inpatient total knee and total hip arthroplasty (TKA, THA).
Methods: A literature search was conducted from the PubMed, Cochrane Library, and Embase databases for articles published before 20 August 2021. The types of studies included prospective randomized controlled trials, prospective cohort studies, retrospective comparative studies, retrospective reviews of THA and TKA registration databases, and observational case-control studies. Comparisons of interest included total complications, complications stratified by type, readmissions, and reoperations at 30 and 90 days. The statistical analysis was performed using Review Manager 5.3.
Results: Twenty studies with 582,790 cases compared relevant postoperative indicators of outpatient and inpatient total joint arthroplasty (TJA) (TKA and THA). There was a significant difference in the total complications at 30 days between outpatient and inpatient THA (p = 0.001), readmissions following TJA (p = 0.03), readmissions following THA (p = 0.001), stroke/cerebrovascular incidents following TJA (p = 0.01), cardiac arrest following TJA (p = 0.007), and blood transfusions following TJA (p = 0.003). The outcomes showed an obvious difference in 90-day total complications between outpatient and inpatient TJA (p = 0.01), readmissions following THA (p = 0.002), and surgical-related pain following TJA (p < 0.001). We did not find significant differences in the remaining parameters.
Conclusion: Outpatient procedures showed comparable and even better outcomes in total complications, complications stratified by type, readmissions, and reoperations at 30 and 90 days compared with inpatient TJA for selected patients.
Introduction
The number of total knee arthroplasty (TKA) and total hip arthroplasty (THA) procedures has increased significantly over the last two decades (1–3). The number of total joint arthroplasty (TJA) (TKA and THA) procedures is expected to reach 4 million by 2,030 in the United States (4). Advances in surgical techniques, perioperative anesthesia, multimodal pain management, and accelerated rehabilitation have led to substantial reductions in the average hospital length of stay (LOS) (5–8). TJA is increasingly being performed in outpatient settings, including hospital outpatient departments (HOPDs) and ambulatory surgery centers (ASCs), to shorten the hospital LOS, reduce the pressure from payers, control the overall cost, and allow patients to return to activities early (9–12). Although outpatient TJA is becoming more common, the frequency with which it is performed remains very low due to concerns about the safety of outpatient surgery (13–15). The acceptable outpatient TJA safety is to ensure that the rate of postoperative complications is basically the same as that in inpatients. To reduce the considerable amount of medical expenses associated with TJA, it is essential that the hospital LOS be shortened and the rate of complications be controlled. Therefore, controlling and reducing the rate of postoperative complications has been the focal point of outpatient TJA (13, 15–17). Published studies have presented conflicting results regarding postoperative complications. Several studies (13, 18, 19) have reported that outpatient TJA is associated with a high rate of perioperative complications. Some researchers have concluded that outpatient TJA is safe and feasible for selected healthy patients, with outcomes comparable to those of standard inpatient surgery (10, 20–22). Some studies have even shown that compared with inpatient TJA, outpatient TJA reduces the rate of complications and readmissions (20, 23–25). In addition, the cost savings of outpatient TJA are noteworthy (21, 26, 27). Several studies have shown that outpatient TJA can save between $4,000 and $8,000 per case (26, 28). Several studies have reported that patients have higher satisfaction with outpatient operations than with inpatient operations (24, 29, 30). We expect to conclude that outpatient procedures will have comparable total complications, complications stratified by type, readmissions, and reoperations at 30 and 90 days compared with inpatient TJA. This is the first study including the most recent literature and large-volume cases to present comprehensive information on the total complications, complications stratified by type, readmissions, and reoperations.
In this study, a meta-analysis was conducted to compare the total complications, complications stratified by type, readmissions, and reoperations at 30 and 90 days after outpatient and standard inpatient TJA. The types of studies included prospective randomized controlled trials, prospective cohort studies, retrospective comparative studies, retrospective reviews of THA and TKA registration databases, and observational case-control studies. We presumed the security of outpatient TJA to be comparable to that of inpatient surgery for selected patients.
Materials and methods
Search strategy
A literature search was conducted with the PubMed, Cochrane Library, and Embase databases. This work has been reported in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and Assessing the Methodological Quality of Systematic Reviews (AMSTAR) guidelines (31). Our work has been registered in the PROSPERO international prospective register of systematic reviews (registration number CRD42020180124). The literature search was restricted to articles published in the English language before 20 August 2021. The Cochrane Central Register of Controlled Studies was searched using the following terms: outpatient, ambulatory surgery, day surgery, inpatient, total joint arthroplasty (TJA) or total joint replacement (TJR), total knee arthroplasty (TKA) or total knee replacement (TKR), and total hip arthroplasty (THA) or total hip replacement (THR).
Inclusion and exclusion criteria
The eligibility criteria for this study were as follows:
1. Studies that included patients undergoing TKA because of a disease such as osteoarthritis, rheumatoid arthritis, or posttraumatic arthritis. Studies that included patients undergoing THA because of a disease such as femoral head necrosis, femoral neck fracture, osteoarthritis, rheumatoid arthritis, posttraumatic arthritis, or congenital hip dysplasia.
2. Prospective randomized controlled trials, prospective cohort studies, retrospective comparative studies, retrospective reviews of THA and TKA registration databases, and observational case-control studies.
3. Studies comparing outpatient procedures with inpatient TKA or THA.
4. Studies that included cohorts matched and adjusted for age, comorbidities and anesthesia grade of outpatients and inpatients without significant differences.
5. Studies that included postoperative evaluation indicators, including at least one of the following: total complications, complications stratified by type, readmissions, or reoperations.
6. A representative article was selected if several studies referred to the same database, and the remaining studies were excluded for reasons of avoiding repetition.
Data extraction
Two independent reviewers extracted the data according to the abovementioned inclusion and exclusion criteria. Disagreements between reviewers were resolved by consultation with senior reviewers. The demographics and characteristics of the studies included first author, age, year of publication, study period, country, study type or source, follow-up time, outpatient definition, type of surgery, number of total patients, number of outpatients, and number of inpatients. The comparisons of interest included total complications, complications stratified by type, readmissions, and reoperations at 30 and 90 days. The complications stratified by type included surgical site infection, pneumonia, renal insufficiency, renal failure, urinary tract infection, stroke/cerebrovascular incidents, cardiac arrest, myocardial infarction, blood transfusion, sepsis/septic shock, deep vein thrombosis, revision, periprosthetic fracture, surgical-related pain and arthrofibrosis.
Statistical analysis
The odds ratio (OR) was used to assess the effect, and the Mantel–Haenszel (MH) statistical method was selected because all data were dichotomous variables, and this study involved randomized controlled trials, prospective studies, retrospective studies, etc. A fixed-effects model was used when there was low heterogeneity among studies (p > 0.10 and I2 < 25%); otherwise, a random-effects model was used. Publication bias was evaluated by funnel plots. Sensitivity analysis was conducted by a leave-one-out analysis. The statistical analysis was performed using Review Manager 5.3 (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014), and p < 0.05 indicated a significant difference.
Results
There were 568 articles retrieved by searching the PubMed, Cochrane Library, and Embase databases, and no additional articles were found through manual searching. We removed 95 duplicate records using literature management software. A total of 357 records were excluded after the titles and abstracts were strictly screened. Finally, 20 articles (18, 19, 21, 26, 32–47) were included in our meta-analysis after the full texts were read and duplicate studies using the same source dataset were excluded. A flow chart of the study selection process is illustrated in Figure 1. A total of 582,790 patients who underwent TKA or THA were included in this study. The demographics and characteristics of the studies involved in the systematic review and meta-analysis are presented in Table 1.
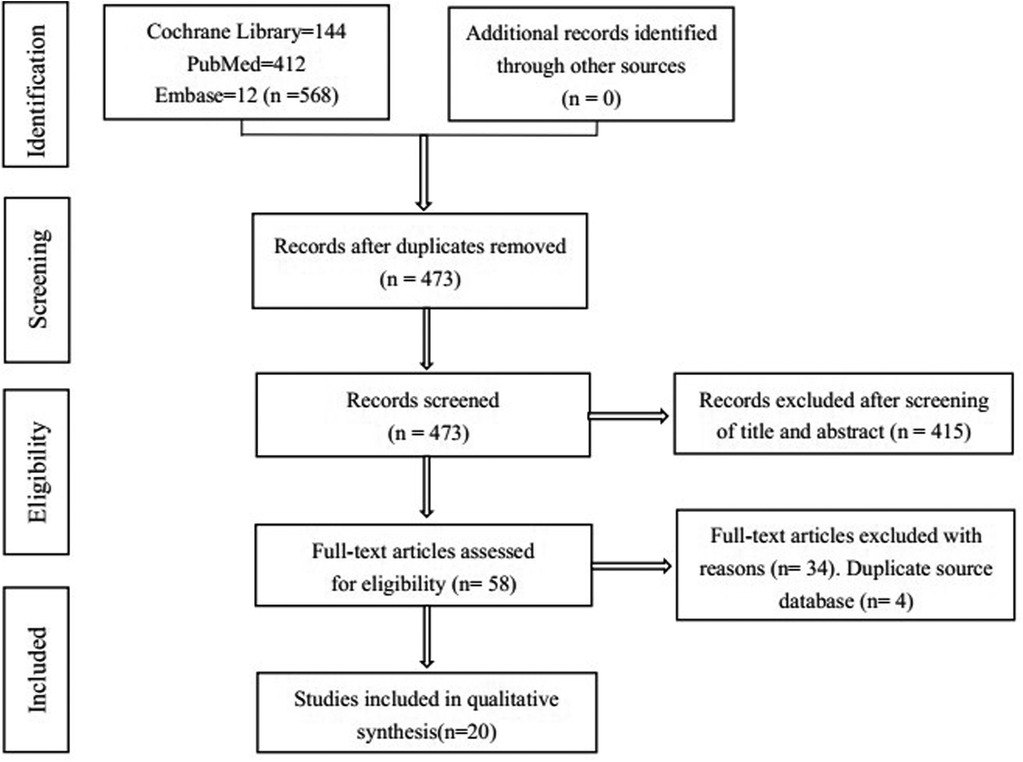
Figure 1. Flow charts of the study selection process for the meta-analysis of outpatient vs inpatient TJA.
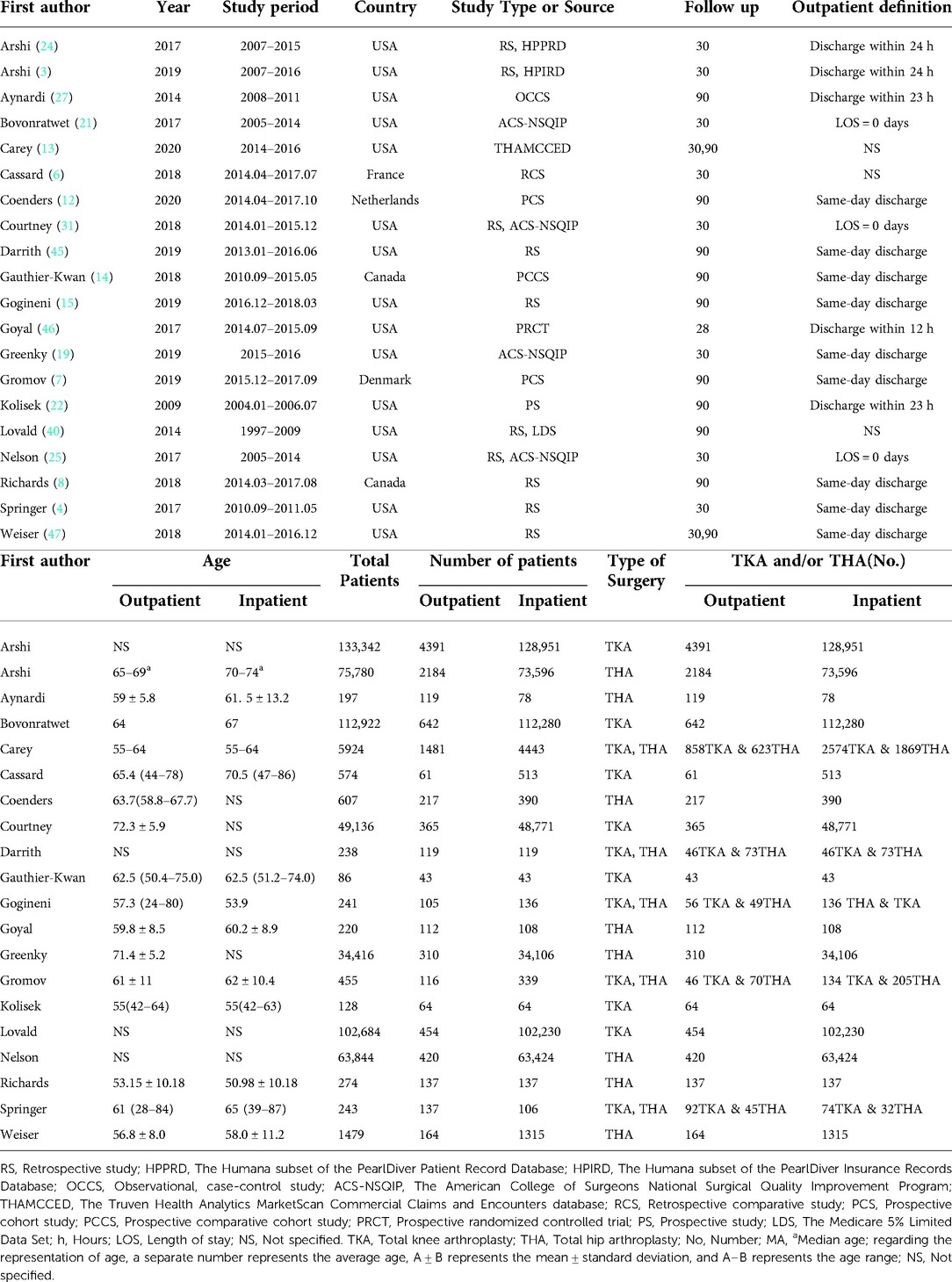
Table 1. Demographics and characteristics of the studies included in the systematic review and meta-analysis.
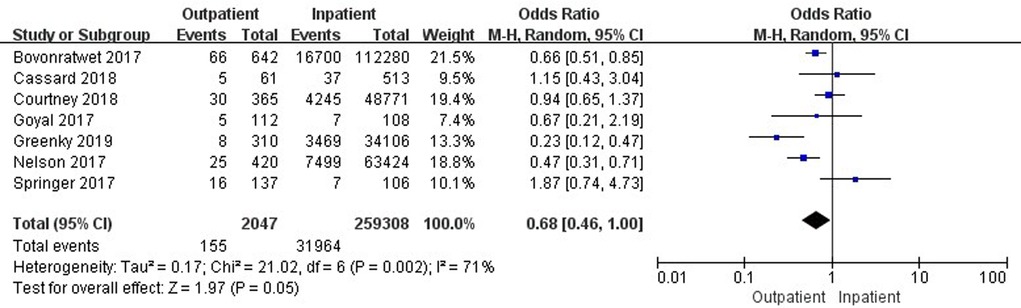
Comparison of 30-day total complications
Seven studies (19, 33, 35, 37, 41, 42, 45) involving 261,355 cases compared 30-day total complications between outpatient and inpatient TJA. The results showed no significant difference in 30-day total complications between outpatient and inpatient TJA (95% confidence interval (CI) 0.46–1.00, p = 0.05) (Figure 2). Four studies (19, 33, 35, 37) involving 162,798 cases compared 30-day total complications between outpatient and inpatient TKA. There were no significant differences in 30-day total complications between outpatient and inpatient TKA (95% CI, 0.62–1.31, p = 0.58) (Supplementary Figure S1). Four studies (19, 41, 42, 45) including 98,557 cases compared 30-day total complications between outpatient and inpatient THA. Outpatient THA showed a significant advantage, as it was associated with fewer total complications than inpatient THA (95% CI, 0.24–0.71, p = 0.001) (Figure 3).
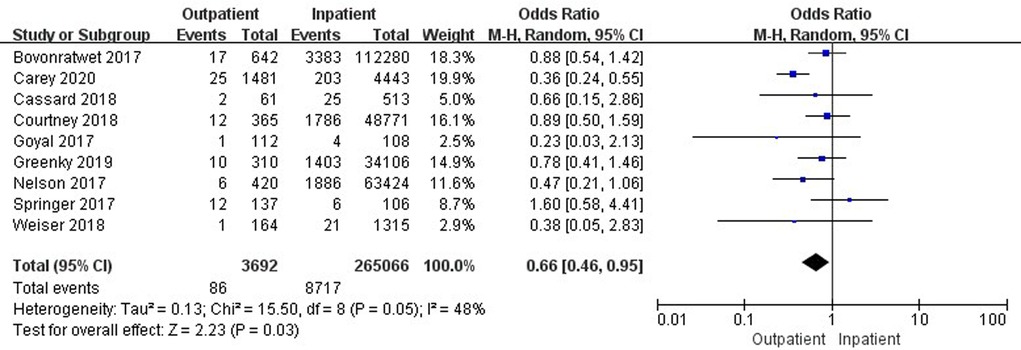
Comparison of 30-day readmissions
Nine studies (19, 33–35, 37, 41, 42, 45, 47) involving 268,758 cases compared 30-day readmissions between outpatient and inpatient TJA. Outpatient TJA presented an obvious advantage, as it was associated with fewer readmissions than inpatient TJA (95% CI, 0.46–0.95, p = 0.03) (Figure 4). Five studies (19, 33–35, 37) involving 166,230 cases compared 30-day readmissions between outpatient and inpatient TKA. There was no significant difference in 30-day readmissions between outpatient and inpatient TKA (95% CI, 0.43–1.28, p = 0.29) (Supplementary Figure S2). Six studies (19, 34, 41, 42, 45, 47) including 102,528 cases compared 30-day readmissions between outpatient and inpatient THA. Outpatient THA showed an obvious advantage, as it was associated with fewer readmissions than inpatient THA (95% CI, 0.34–0.77, p = 0.001) (Figure 5).
Comparison of 90-day total complications
Nine studies (21, 26, 34, 36, 38–40, 44, 46) involving 110,379 cases reported a comparison of 90-day total complications between outpatient and inpatient TJA. There was a significant difference in 90-day total complications between outpatient and inpatient TJA (95% CI, 0.50–0.92, p = 0.01) (Figure 6). Five studies (21, 34, 38, 39, 44) involving 106,422 cases presented a comparison of 90-day total complications between outpatient and inpatient TKA. There was no significant difference in 90-day total complications between outpatient and inpatient TKA (95% CI, 0.52–1.36, p = 0.48) (Supplementary Figure S3). Five studies (26, 34, 36, 38, 46) including 3,716 cases compared 90-day total complications between outpatient and inpatient THA. There was no significant difference in 90-day total complications between outpatient and inpatient THA (95% CI, 0.31–1.12, p = 0.11) (Supplementary Figure S4).
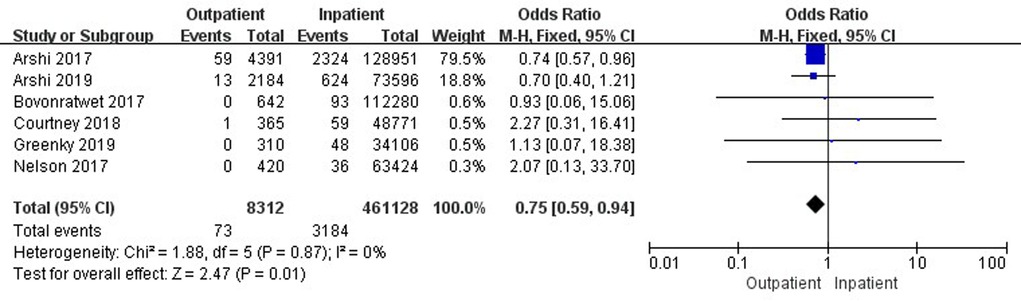
Figure 6. Comparison of 30-day stroke/cerebrovascular accidents between outpatient and inpatient TJA.
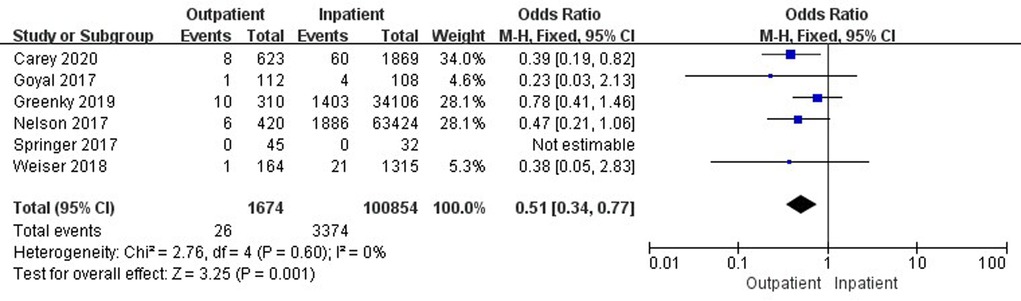
Comparison of 90-day readmissions
Eight studies (26, 34, 36, 38–40, 43, 47) involving 111,714 cases reported a comparison of 90-day readmissions between outpatient and inpatient TJA. There was no significant difference in 90-day readmissions between outpatient and inpatient TJA (95% CI, 0.25–1.30, p = 0.18) (Supplementary Figure S5). Four studies (26, 34, 38, 39) involving 106,294 cases presented a comparison of 90-day readmissions between outpatient and inpatient TKA. There was no significant difference in 90-day readmissions between outpatient and inpatient TKA (95% CI, 0.17–2.66, p = 0.57) (Supplementary Figure S6). Four studies (34, 36, 38, 47) including 4,724 cases compared 90-day readmissions between outpatient and inpatient THA. Outpatient THA showed an obvious advantage, as it was associated with fewer readmissions than inpatient THA (95% CI, 0.12–0.61, p = 0.002) (Figure 7).
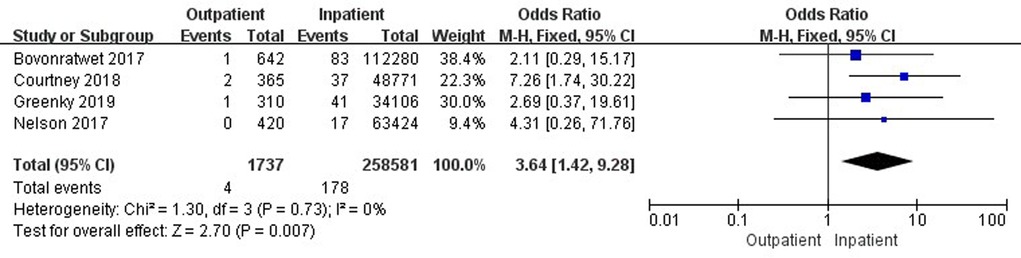
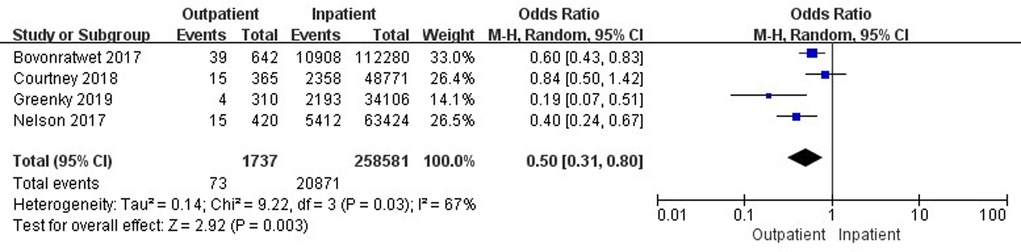
Comparison of reoperations and complications stratified by type
Six studies (18, 32, 33, 37, 42, 45) involving 469,440 cases compared 30-day stroke/cerebrovascular incidents between outpatient and inpatient TJA. There was a significant difference in 30-day stroke/cerebrovascular incidents between outpatient and inpatient TJA (95% CI, 0.59–0.94, p = 0.01) (Figure 8). Four studies (33, 37, 42, 45) involving 260,318 cases reported a comparison of 30-day cardiac arrest between outpatient and inpatient TJA. Inpatient TJA showed an obvious advantage, as it was associated with fewer cardiac arrests than outpatient TJA (95% CI, 1.42–9.28, p = 0.007) (Figure 9). Four studies (33, 37, 42, 45) involving 260,318 cases reported a comparison of 30-day blood transfusions between outpatient and inpatient TJA. Outpatient TJA showed an obvious advantage, as it was associated with fewer blood transfusions than inpatient TJA (95% CI, 0.31–0.80, p = 0.003) (Figure 10). Three studies (37, 41, 42) involving 83,772 cases reported a comparison of 30-day reoperations between outpatient and inpatient TJA. There was no significant difference in 30-day reoperations between outpatient and inpatient TJA (95% CI, 0.70–2.04, p = 0.51) (Supplementary Figure S7).
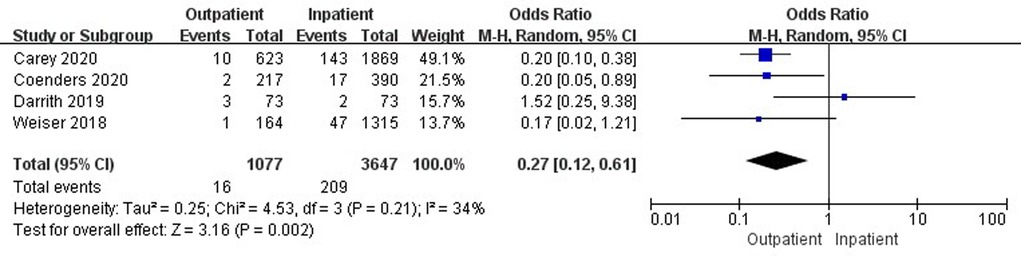
Three studies (26, 39, 46) involving 103,042 cases reported a comparison of 90-day surgical-related pain between outpatient and inpatient TJA. Outpatient TJA showed an obvious advantage, as it was associated with fewer cases of surgical-related pain than inpatient TJA (95% CI, 0.51–0.76, p < 0.001) (Figure 11). Two studies (36, 38) involving 845 cases reported a comparison of 90-day reoperations between outpatient and inpatient TJA. There was no significant difference in 90-day reoperations between outpatient and inpatient TJA (95% CI, 0.07–8.56, p = 0.82) (Supplementary Figure S8).
There were no significant differences in 30-day cases of surgical site infection (95% CI, 0.35–1.16, p = 0.14) (Supplementary Figure S9), pneumonia (95% CI, 0.15–1.50, p = 0.21) (Supplementary Figure S10), renal insufficiency (95% CI, 0.52–5.12, p = 0.39) (Supplementary Figure S11), renal failure (95% CI, 0.68–8.36, p = 0.17) (Supplementary Figure S12), urinary tract infection (95% CI, 0.51–1.42, p = 0.55) (Supplementary Figure S13), myocardial infarction (95% CI, 0.72–1.80, p = 0.59) (Supplementary Figure S14), sepsis/septic shock (95% CI, 0.09–1.51, p = 0.17) (Supplementary Figure S15), or deep vein thrombosis (95% CI, 0.29–1.85, p = 0.51) (Supplementary Figure S16) between outpatient and inpatient TJA. There were no significant differences in cases of 90-day surgical site infection (95% CI, 0.44–1.28, p = 0.29) (Supplementary Figure S17), revision (95% CI, 0.42–2.08, p = 0.87) (Supplementary Figure S18), periprosthetic fracture (95% CI, 0.14–3.37, p = 0.64) (Supplementary Figure S19), deep vein thrombosis (95% CI, 0.23–1.62, p = 0.32) (Supplementary Figure S20), or arthrofibrosis (95% CI, 0.60–1.31, p = 0.55) (Supplementary Figure S21) between outpatient and inpatient TJA.
Discussion
This study comprehensively analyzed total complications, complications stratified by type, readmissions, and reoperations at 30 and 90 days after outpatient and conventional inpatient procedures. The main finding was that outpatient procedures showed better results in THA total complications, THA readmissions, TJA readmissions, TJA stroke/cerebrovascular incidents, and TJA blood transfusion at 30 days postoperatively. Outpatient procedures presented fewer adverse events in regard to TJA total complications, THA readmissions, and TJA surgical-related pain at 90 days postoperatively compared with inpatient procedures.
There are several limitations in this study. First, the study presented significant potential bias. Outpatient protocols differed from inpatient protocols, and even outpatient protocols were not uniform. Some outpatient protocols followed enhanced recovery after surgery (ERAS) principles, while others were similar to inpatient protocols and tried to achieve same day discharge with strict patient selection. The selection criteria for outpatients and inpatients were inconsistent due to the different types of included studies. Second, according to the Improved Jadad Rating Scale score, only five prospective studies were included, and the remaining studies were retrospective or database studies. Relatively low-quality literature has limited persuasiveness. In the future, more multicenters, large-sample, randomized controlled trials will be needed to clarify the topic. Third, the definition of outpatient discharge time was inconsistent; it included same-day discharge, an LOS of 0 days, discharge within 12 h, discharge within 23 h, and discharge within 24 h. If the discharge time can be standardized, it will be of great benefit to the research on this topic.
Outpatient procedures have become a feasible treatment option and are gradually being performed more often based on substantial reductions in hospital LOS due to advances in surgical techniques, perioperative anesthesia, multimodal pain management, and accelerated rehabilitation (9–12). Common sense dictates that a prolonged LOS should provide a wider margin of security and lower the risk of complications. However, our results showed that the LOS of outpatient procedures was shortened and postoperative complications were reduced. This seemed to be slightly paradoxical. After a comprehensive analysis, we speculate that the possible reasons are as follows. First, the introduction of ERAS principles and innovation of technology and implants may lead to a shorter LOS and fewer complications in outpatient procedures (48–50). ERAS protocols require the collaboration of a multidisciplinary team, including surgeons, anesthesiologists, nurses, and physiotherapists, who follow specifically designed protocols on perioperative care and adjust their practices based on evolving scientific knowledge. Hence, it is possible for outpatients to have a shorter LOS and fewer complications than inpatients through multidisciplinary collaboration and delicacy management. Second, outpatient procedures may adhere to tighter patient selection criteria than inpatient procedures. Age is a crucial factor for outpatient and inpatient patient selection. Looking at the age comparison of the included literature, outpatient surgeons tend to choose younger patients. Another important factor is preoperative comorbidities; for example, high blood pressure, diabetes, and coronary heart disease. Outpatient surgeons tend to choose patients with fewer comorbidities. It is reasonable to consider that younger patients with fewer preoperative comorbidities could have a shorter LOS and fewer postoperative complications. Third, different anesthesia methods may affect early postoperative mobilization in outpatients and inpatients. Inpatients are more likely to receive general inhalation anesthesia, which is more likely to cause postoperative nausea, dizziness and vomiting and affect patients' early mobilization. However, outpatients generally receive spinal anesthesia, which can enable patients to mobilize early. Fourth, good preoperative education and home care are essential for the implementation of outpatient procedures. It is obvious that outpatient protocols address these two aspects better than inpatient programs.
The main obstacle to the implementation of outpatient TKA and THA came from the concerns of patients and surgeons regarding safety. The published literature showed opposite results regarding postoperative complications in outpatient and inpatient cohorts. Arshi et al. (24) showed that outpatient TKA was associated with a higher risk of postoperative 30-day complications, including surgical site infection, component failure, deep vein thrombosis, and knee stiffness, through a review of the Humana subset of the PearlDiver patient record database. However, several published studies showed that when performed in appropriately selected patients, outpatient TKA was not associated with a higher postoperative 30-day complication rate than inpatient TKA (6, 21, 31). Gogineni et al. (15) reported that outpatient TKA and THA in well-selected patients were feasible in an academic multidisciplinary tertiary care hospital, with postoperative 90-day complication rates approximating those of inpatient surgery. In addition, patients undergoing outpatient THA had no greater risk of postoperative 30-day complications than those who underwent inpatient surgery (3, 25). Some studies demonstrated that appropriately selected patients can undergo THA in an outpatient setting with no increase in complications at 90 days (8, 12, 27). Moreover, Greenky et al. (19) reported that outpatients and short-stay patients had lower 30-day complication rates than inpatients. Carey et al. (13) reported that outpatient procedures had a lower postoperative 90-day complication rate than inpatient TKA and THA. From a series of published studies, only one article reported that outpatient procedures have higher postoperative complications than inpatient surgeries, and two studies reported that the postoperative complications of outpatients are lower than those of inpatients. Most of the literature reported that outpatients and inpatients had comparable postoperative complications. After a comprehensive analysis, our results demonstrated that outpatient THA had fewer 30-day complications than the inpatient procedure, and outpatient TJA had fewer 90-day complications than inpatient surgery.
Readmission due to complications is the most direct cause of an increase in medical burden (34, 37, 42). Outpatient and inpatient TKA showed readmission rates of 1.98%–13.04% and 3.01%–8.11%, respectively, at 30 days (19, 33, 34). Outpatient and inpatient THA showed readmission rates of 0%–3.23% and 0%–4.11%, respectively, at 30 days (19, 42). Outpatient and inpatient TKA presented readmission rates of 0%–3.15% and 0%–9.87%, respectively, at 90 days (19, 34, 38). Outpatient and inpatient THA revealed readmission rates of 0.61%–4.11% and 2.74%–7.65%, respectively, at 90 days (34, 38, 47). We found an interesting phenomenon in which the maximum readmission rate at 30 days was higher than that at 90 days after TKA (13.04% vs. 9.87%). We performed a careful analysis and trusted the results. First, an inconsistency in the included articles was detected in the 30-day and 90-day groups because some articles reported the 30-day readmission data, and the other articles reported the 90-day outcomes. Second, the evidence may not be strong because of the small sample size of fewer than 100 cases (37). Therefore, a comprehensive analysis needs to be conducted in multiple studies with large sample sizes. Our study reported that outpatient TJA had fewer THA readmissions at 30 days and fewer THA readmissions at 90 days. Moreover, outpatient and inpatient TJA procedures showed comparable outcomes in TKA readmissions at 30 days and in TJA and TKA readmissions at 90 days. In summary, we conclude that outpatient TJA showed comparable and even better outcomes in readmissions at 30 and 90 days than did inpatient TJA.
Reoperations due to complications constitute the other direct cause of an increase in medical burden (37, 41, 42). Complications such as surgical site infection, periprosthetic fracture, and prosthesis dislocation are likely to require reoperation. In this study, the number of studies involving reoperations was a serious limitation, and it concluded that there was no significant difference within 30 and 90 days between the two groups. More evidence is needed to determine whether the two groups differ. Our analysis showed that outpatient TJA was associated with fewer stroke/cerebrovascular incidents than inpatient TJA. This result is possibly related to the lower average age and fewer comorbidities of outpatients (20). In this study, cardiac arrest was the only index in which outpatient TJA showed worse outcomes than inpatient TJA. This result is probably related to the lack of emergency medical support for outpatients at discharge. Our study showed that outpatient TJA required fewer blood transfusions than inpatient TJA. Same-day discharge lacks the assessment of hemoglobin and related indicators. Inpatients undergo more medical index monitoring and elaborate treatments. This study showed that outpatient TJA was associated with less surgical-related pain than inpatient TJA. We speculate that inpatients were given more detailed multimodal pain management than were same-day discharge outpatients.
Conclusion
Outpatient TJA has advantages over inpatient TJA in THA total complications, THA readmissions, TJA readmissions, TJA stroke/cerebrovascular incidents, and TJA blood transfusion at 30 days and in THA readmissions, TJA total complications, and TJA surgical-related pain at 90 days. The remaining parameters presented comparable outcomes between outpatient and inpatient TJA. Overall, outpatient total knee and hip arthroplasty provide comparable and even better clinical outcomes than inpatient operations for well-selected patients. Multicenter randomized controlled trials with large samples are needed to provide stronger evidence in the future.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author contributions
GS and XWH are responsible for the integrity and authenticity of this work. All authors have read and approved the final version of this manuscript submitted for publication. Conception and design: XWH, GS, YYH and FY. Literature search: GS, WRY, YYH and WYX. Data extraction: GS, HLZ and SWK. Data analysis: GS, WRY, and GTL.Writing and critical revision of the article: GS, XWH, FY, and YYH. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by a grant from the National Natural Science Foundation of China (No. 81672155/81974337).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.833275/full#supplementary-material.
References
1. Bertin KC. Minimally invasive outpatient total hip arthroplasty: a financial analysis. Clin Orthop Relat Res. (2005) 435:154–63. doi: 10.1097/01.blo.0000157173.22995.cf
2. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. (2009) 62(10):1006–12. 10.1016/j.jclinepi.2009.06.005 19631508
3. Arshi A, Leong NL, Wang C, Buser Z, Wang JC, SooHoo NF. Outpatient total hip arthroplasty in the United States: a population-based comparative analysis of complication rates. J Am Acad Orthop Surg. (2019) 27:61–7. doi: 10.5435/JAAOS-D-17-00210
4. Springer BD, Odum SM, Vegari DN, Mokris JG, Beaver WB Jr. Impact of inpatient versus outpatient total joint arthroplasty on 30-day hospital readmission rates and unplanned episodes of care. Orthop Clin North Am. (2017) 48:15–23. doi: 10.1016/j.ocl.2016.08.002
5. Berend KR, Lombardi AV Jr, Berend ME, Adams JB, Morris MJ. The outpatient total hip arthroplasty: a paradigm change. Bone Joint J. (2018) 100-B:31–5. doi: 10.1302/0301-620X.100B1.BJJ-2017-0514.R1
6. Cassard X, Garnault V, Corin B, Claverie D, Murgier J. Outpatient total knee arthroplasty: readmission and complication rates on day 30 in 61 patients. Orthop Traumatol Surg Res. (2018) 104:967–70. doi: 10.1016/j.otsr.2018.07.014
7. Gromov K, Jørgensen CC, Petersen PB, Kjaersgaard-Andersen P, Revald P, Troelsen A, et al. Complications and readmissions following outpatient total hip and knee arthroplasty: a prospective 2-center study with matched controls. Acta Orthop. (2019) 90:281–5. doi: 10.1080/17453674.2019.1577049
8. Richards M, Alyousif H, Kim JK, Poitras S, Penning J, Beaulé PE. An evaluation of the safety and effectiveness of total hip arthroplasty as an outpatient procedure: a matched-cohort analysis. J Arthroplasty. (2018) 33:3206–10. doi: 10.1016/j.arth.2018.05.036
9. Etkin CD, Springer BD. The American joint replacement registry-the first 5 years. Arthroplast Today. (2017) 3:67–9. doi: 10.1016/j.artd.2017.02.002
10. Vorhies JS, Wang Y, Herndon JH, Maloney WJ, Huddleston JI. Decreased length of stay after TKA is not associated with increased readmission rates in a national medicare sample. Clin Orthop Relat Res. (2012) 470:166–71. doi: 10.1007/s11999-011-1957-0
11. Huang A, Ryu J, Dervin G. Cost savings of outpatient versus standard inpatient total knee arthroplasty. Can J Surg. (2017) 60:57–62. doi: 10.1503/cjs.002516
12. Coenders MJ, Mathijssen NMC, Vehmeijer SBW. Three and a half years’ experience with outpatient total hip arthroplasty. Bone Joint J. (2020) 102-B:82–9. doi: 10.1302/0301-620X.102B1
13. Carey K, Morgan JR, Lin MY, Kain MS, Creevy WR. Patient outcomes following total joint replacement surgery: a comparison of hospitals and ambulatory surgery centers. J Arthroplasty. (2020) 35:7–11. doi: 10.1016/j.arth.2019.08.041
14. Gauthier-Kwan OY, Dobransky JS, Dervin GF. Quality of recovery, postdischarge hospital utilization, and 2-year functional outcomes after an outpatient total knee arthroplasty program. J Arthroplasty. (2018) 33:2159–64.e1. doi: 10.1016/j.arth.2018.01.058
15. Gogineni HC, Gray CF, Prieto HA, Deen JT, Boezaart AP, Parvataneni HK. Transition to outpatient total hip and knee arthroplasty: experience at an academic tertiary care center. Arthroplast Today. (2018) 5:100–5. doi: 10.1016/j.artd.2018.10.008
16. Delaney CP, Senagore AJ, Gerkin TM, Beard TL, Zingaro WM, Tomaszewski KJ, et al. Association of surgical care practices with length of stay and use of clinical protocols after elective bowel resection: results of a national survey. Am J Surg. (2010) 199:299–304. doi: 10.1016/j.amjsurg.2009.08.027
17. Otero JE, Gholson JJ, Pugely AJ, Gao Y, Bedard NA, Callaghan JJ. Length of hospitalization after joint arthroplasty: does early discharge affect complications and readmission rates? J Arthroplasty. (2016) 31:2714–25. doi: 10.1016/j.arth.2016.07.026
18. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. (2007) 89:780–5. doi: 10.2106/JBJS.F.00222
19. Greenky MR, Wang W, Ponzio DY, Courtney PM. Total hip arthroplasty and the medicare inpatient-only list: an analysis of complications in medicare-aged patients undergoing outpatient surgery. J Arthroplasty. (2019) 34:1250–4. doi: 10.1016/j.arth.2019.02.031
20. Parvizi J, Mui A, Purtill JJ, Sharkey PF, Hozack WJ, Rothman RH. Total joint arthroplasty: when do fatal or near-fatal complications occur? J Bone Joint Surg Am. (2007) 89:27–32. doi: 10.2106/JBJS.E.01443
21. Bovonratwet P, Ondeck NT, Nelson SJ, Cui JJ, Webb ML, Grauer JN. Comparison of outpatient vs. inpatient total knee arthroplasty: an ACS-NSQIP analysis. J Arthroplasty. (2017) 32:1773–8. doi: 10.1016/j.arth.2017.01.043
22. Kolisek FR, McGrath MS, Jessup NM, Monesmith EA, Mont MA. Comparison of outpatient versus inpatient total knee arthroplasty. Clin Orthop Relat Res. (2009) 467:1438–42. doi: 10.1007/s11999-009-0730-0
23. Stephen AE, Berger DL. Shortened length of stay and hospital cost reduction with implementation of an accelerated clinical care pathway after elective colon resection. Surgery. (2003) 133:277–82. doi: 10.1067/msy.2003.19
24. Arshi A, Leong NL, D'Oro A, Wang C, Buser Z, Wang JC, et al. Outpatient total knee arthroplasty is associated with higher risk of perioperative complications. J Bone Joint Surg Am. (2017) 99:1978–86. doi: 10.2106/JBJS.16.01332
25. Nelson SJ, Webb ML, Lukasiewicz AM, Varthi AG, Samuel AM, Grauer JN. Is outpatient total hip arthroplasty safe? J Arthroplasty. (2017) 32:1439–42. doi: 10.1016/j.arth.2016.11.053
26. Inacio MCS, Paxton EW, Graves SE, Namba RS, Nemes S. Projected increase in total knee arthroplasty in the United States e an alternative projection model. Osteoarthr Cartil. (2017) 25:1797–803. doi: 10.1016/j.joca.2017.07.022
27. Aynardi M, Post Z, Ong A, Orozco F, Sukin DC. Outpatient surgery as a means of cost reduction in total hip arthroplasty: a case-control study. HSS J. (2014) 10:252–5. doi: 10.1007/s11420-014-9401-0
28. Maempel JF, Walmsley PJ. Enhanced recovery programmes can reduce length of stay after total knee replacement without sacrificing functional outcome at one year. Ann R Coll Surg Engl. (2015) 97:563–7. doi: 10.1308/rcsann.2015.0016
29. Berger RA, Kusuma SK, Sanders SA, Thill ES, Sporer SM. The feasibility and perioperative complications of outpatient knee arthroplasty. Clin Orthop Relat Res. (2009) 467:1443–9. doi: 10.1007/s11999-009-0736-7
30. Kelly MP, Calkins TE, Culvern C, Kogan M, Della Valle CJ. Inpatient versus outpatient hip and knee arthroplasty: which has higher patient satisfaction? J Arthroplasty. (2018) 33:3402–6. doi: 10.1016/j.arth.2018.07.025
31. Courtney PM, Froimson MI, Meneghini RM, Lee GC, Della Valle CJ. Can total knee arthroplasty be performed safely as an outpatient in the medicare population? J Arthroplasty. (2018) 33:S28–31. doi: 10.1016/j.arth.2018.01.003
32. Kurtz SM, Ong KL, Lau E, Bozic KJ. Impact of the economic downturn on total joint replacement demand in the United States. J Bone Joint Surg Am. (2014) 96:624–30. doi: 10.2106/JBJS.M.00285
33. Hirschmann MT, Kort N, Kopf S, Becker R. Fast track and outpatient surgery in total knee arthroplasty: beneficial for patients, doctors and hospitals. Knee Surg Sports Traumatol Arthrosc. (2017) 25:2657–8. doi: 10.1007/s00167-017-4660-1
34. Memtsoudis SG, Della Valle AG, Besculides MC, Gaber L, Laskin R. Trends in demographics, comorbidity profiles, in-hospital complications and mortality associated with primary knee arthroplasty. J Arthroplasty. (2009) 24:518–27. doi: 10.1016/j.arth.2008.01.307
35. Berger RA, Sanders SA, Thill ES, Sporer SM, Della Valle C. Newer anesthesia and rehabilitation protocols enable outpatient hip replacement in selected patients. Clin Orthop Relat Res. (2009) 467:1424–30. doi: 10.1007/s11999-009-0741-x
36. Basques BA, Tetreault MW, Della Valle CJ. Same-day discharge compared with inpatient hospitalization following hip and knee arthroplasty. J Bone Joint Surg Am. (2017) 99:1969–77. doi: 10.2106/JBJS.16.00739
37. Lovecchio F, Alvi H, Sahota S, Beal M, Manning D. Is outpatient arthroplasty as safe as fast-track inpatient arthroplasty? A propensity score matched analysis. J Arthroplasty. (2016) 31:197–201. doi: 10.1016/j.arth.2016.05.037
38. Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among medicare beneficiaries, 1991-2010. JAMA. (2012) 308:1227–36. doi: 10.1001/2012.jama.11153
39. Courtney PM, Boniello AJ, Berger RA. Complications following outpatient total joint arthroplasty: an analysis of a national database. J Arthroplasty. (2017) 32:1426–30. doi: 10.1016/j.arth.2016.11.055.28034481
40. Lovald ST, Ong KL, Malkani AL, Lau EC, Schmier JK, Kurtz SM, et al. Complications, mortality, and costs for outpatient and short-stay total knee arthroplasty patients in comparison to standard-stay patients. J Arthroplasty. (2014) 29:510–5. doi: 10.1016/j.arth.2013.07.020
41. Sutton JC, Antoniou J, Epure LM, Huk OL, Zukor DJ, Bergeron SG. Hospital discharge within 2 days following total hip or knee arthroplasty does not increase major-complication and readmission rates. J Bone Joint Surg Am. (2016) 98:1419–28. doi: 10.2106/JBJS.15.01109
42. Dorr LD, Thomas DJ, Zhu J, Dastane M, Chao L, Long WT. Outpatient total hip arthroplasty. J Arthroplasty. (2010) 25:501–6. doi: 10.1016/j.arth.2009.06.005
43. Teeny SM, York SC, Benson C, Perdue ST. Does shortened length of hospital stay affect total knee arthroplasty rehabilitation outcomes? J Arthroplasty. (2005) 20:39–45. doi: 10.1016/j.arth.2005.04.025
44. Hartog YM, Mathijssen NM, Vehmeijer SB. Total hip arthroplasty in an outpatient setting in 27 selected patients. Acta Orthop. (2015) 86:667–70. doi: 10.3109/17453674.2015.1066211
45. Darrith B, Frisch NB, Tetreault MW, Fice MP, Culvern CN, Della Valle CJ. Inpatient versus outpatient arthroplasty: a single-surgeon, matched cohort analysis of 90-day complications. J Arthroplasty. (2019) 34:221–7. doi: 10.1016/j.arth.2018.10.015
46. Goyal N, Chen AF, Padgett SE, Tan TL, Kheir MM, Hopper RH Jr, et al. Otto aufranc award: a multicenter, randomized study of outpatient versus inpatient total hip arthroplasty. Clin Orthop Relat Res. (2017) 475:364–72. doi: 10.1007/s11999-016-4915-z
47. Weiser MC, Kim KY, Anoushiravani AA, Iorio R, Davidovitch RI. Outpatient total hip arthroplasty has minimal short-term complications with the use of institutional protocols. J Arthroplasty. (2018) 33:350. doi: 10.1016/j.arth.2018.07.015
48. Vendittoli PA, Pellei K, Desmeules F, Massé V, Loubert C, Lavigne M, et al. Enhanced recovery short-stay hip and knee joint replacement program improves patients outcomes while reducing hospital costs. Orthop Traumatol Surg Res. (2019) 105(7):1237–43. doi: 10.1016/j.otsr.2019.08.013
49. Pennestrì F, Maffulli N, Sirtori P, Perazzo P, Negrini F, Banfi G, et al. Blood management in fast-track orthopedic surgery: an evidence-based narrative review. J Orthop Surg Res. (2019) 14(1):263. doi: 10.1186/s13018-019-1296-5
Keywords: outpatient total knee arthroplasty, outpatient total hip arthroplasty, complications, readmissions, reoperations
Citation: Gong S, Yi Y, Wang R, Han L, Gong T, Wang Y, Shao W, Feng Y and Xu W (2022) Outpatient total knee and hip arthroplasty present comparable and even better clinical outcomes than inpatient operation. Front. Surg. 9:833275. doi: 10.3389/fsurg.2022.833275
Received: 14 January 2022; Accepted: 12 August 2022;
Published: 6 September 2022.
Edited by:
Yang Lv, Peking University Third Hospital, ChinaReviewed by:
Minwei Zhao, Peking University Third Hospital, ChinaJochen Salber, Ruhr-University Bochum, Germany
© 2022 Gong, Yi, Wang, Han, Gong, Wang, Shao, Feng and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yong Feng ZmVuZ3lvbmdAaHVzdC5lZHUuY24= Weihua Xu eHV3ZWlodWFAaHVzdC5lZHUuY24=
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
†These authors have contributed equally to this work and share first authorship.
 Song Gong
Song Gong Yihu Yi
Yihu Yi Ruoyu Wang
Ruoyu Wang Lizhi Han
Lizhi Han Tianlun Gong
Tianlun Gong Yuxiang Wang
Yuxiang Wang Wenkai Shao2
Wenkai Shao2 Yong Feng
Yong Feng Weihua Xu
Weihua Xu