
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CLINICAL TRIAL article
Front. Surg., 11 May 2022
Sec. Cardiovascular Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.826761
This article is part of the Research TopicNew Challenges with the Management of Rheumatic Heart DiseaseView all 8 articles
Background: Use of capnography as a non-invasive method during the weaning process for fast track extubation (FTE) is controversial. We conducted the present study to determine whether pulse oximetry and capnography could be utilized as alternatives to arterial blood gas (ABG) measurements in patients under mechanical ventilation (MV) following coronary artery bypass graft (CABG) surgery.
Methods: In this randomized clinical trial, 70 patients, who were candidates for CABG surgery, were randomly assigned into two equal groups (n = 35), intervention and control group. In the intervention group, the ventilator management and weaning from MV was done using Etco2 from capnography and SpO2 from pulse oximetry. Meanwhile, in the control group, weaning was done based on ABG analysis. The length of intensive care unit (ICU) stay, time to extubation, number of manual ventilators setting changes, and alarms were compared between the groups.
Results: The end-tidal carbon dioxide (ETCO2) levels in the intervention group were completely similar to the partial pressure of carbon dioxide (PaCo2) in the control group (39.5 ± 3.1 vs. 39.4 ± 4.32, p > 0.05). The mean extubation times were significantly shorter in the intervention group compared to those in the control patients (212.2 ± 80.6 vs. 342.7 ± 110.7, p < 0.001). Moreover, the number of changes in the manual ventilator setting and the number of alarms were significantly lower in the intervention group. However, the differences in the length of stay in ICU between the two groups were not significant (p = 0.219).
Conclusion: Our results suggests that capnography can be used as an alternative to ABG. Furthermore, it is a safe and valuable monitor that could be a good alternative for ABG in this population. Further studies with larger sample sizes and on different disease states and populations are required to assess the accuracy of our findings.
Clinical Trial Registration: Current Controlled Trials, IRCT, IRCT201701016778N6, Registered 3 March 2017, https://www.irct.ir/trial/7192.
Fast track extubation (FTE) is an accepted method for weaning patients from mechanical ventilation (MV) after coronary artery bypass graft (CABG) surgery. The duration of MV in patients undergoing cardiac surgery is usually between 1–6 h. Long-term MV might trigger certain complications, such as infection, atelectasis, and increased mortality (1, 2). With a proper management and early withdrawal of the endotracheal tube, the complications and costs would reduce (1, 3). FTE can decrease health care costs following CABG surgery up to 50% (4). Utilizing a proper anesthesia technique during surgery and post-surgery management, FTE can be applied in patients undergoing CABG surgery without any specific complications (5).
The readiness of patients for weaning is usually assessed by arterial blood gas (ABG) sampling. ABG is the gold standard for the monitoring of oxygenation and ventilation during the postoperative MV (6). Arterial line cannulation is employed in the operating room and ICU settings to provide easy access for continuous and real-time systemic blood pressure measurements, blood gas analysis, and other laboratory measurements. However, based on evidence, this process is not without risk factors (7). The process of inserting arterial line (over 48 or 72 h) is an invasive procedure with several complications, for instance infection, local hematoma, vascular injury, thrombosis, disseminated intravascular coagulation, and reduced cardiac output (8–10). On the other hand, Iran, as a developing country with sanctions, cannot access advanced medical equipment, such as ABG analyzers. Therefore, in order to minimize these complications and having easier access, finding an alternative non-invasive method seems to be reasonable.
The use of pulse oximetry as a valid non-invasive tool for oxygenation monitoring has been agreed upon by the public for many years (11). In several cases, the pulse oximetry is used as the only criterion to check oxygenation and to make oxygenation-associated changes in MV. The utilization of a capnography is also recommended under different clinical conditions (12). Capnography is a method in which the infrared radiation is employed to measure the carbon dioxide (CO2) in exhaled air. This method includes the non-invasive measurement of CO2, providing information on ventilation (effectiveness of CO2 elimination), perfusion (CO2 transportation in vasculature), and metabolism (production of CO2 via cellular metabolism) in intubated and spontaneously breathing patients (13, 14). Capnography in certain conditions, for instance confirmation of the correct place of the endotracheal tube, is recommended as the standard of care (15). Yet in some other circumstances, such as cardiopulmonary resuscitation and changing the MV settings, there are numerous differences between the existing data and there are no similar recommendations (16–18). Certain studies have mentioned the lack of correlation between these variables and have considered the difference between them high (19). On the other hand, some other studies have reported an equal role for these two parameters in monitoring the level of CO2 (14, 20).
The substantial debate is that whether capnography and pulse oximetry could be efficient alternatives for ABG analysis during the process of weaning from mechanical ventilation (MV). Therefore, capnography and pulse oximetry are used in this study for monitoring during the MV and management of the ventilator setting. The current study aimed to assess the feasibility and safety of non-invasive monitoring techniques during the weaning process in patients undergoing the CABG surgery.
This study was a randomized controlled clinical trial conducted between February and March 2018 with Trial Registration Number (IRCT201701016778N6) in Iranian Registry of Clinical Trials (IRCT). The study protocol was reviewed and approved by the Ethics Committee of Baqiyatallah University of Medical Sciences, Tehran, Iran, under code IR.BMSU.REC.1395.141, in accordance with the Declaration of Helsinki of the World Medical Association (21). In addition, one day ahead of the operation, we explained the objectives of this study to the participants and obtained the informed consent. The study was conducted and reported in accordance with the recommendations of the Consolidated Standards of Reporting Trials (CONSORT) statement (22).
We conducted this research on 70 patients, who underwent CABG surgery at Jamaran Heart Hospital in Tehran, Iran. The patients who met the inclusion criteria were selected through convenient sampling and randomly assigned into two equal groups (n = 35); the intervention group and the control group. Due to the nature of this clinical trial study, which compared two different methods, there was no possibility of blinding. Randomization sequence was created with Excel 2007 (Microsoft, Redmond, WA, USA) with a 1:1 allocation, using random block sizes of 2 and 4 by an investigator with no clinical involvement in the trial. The eligible participants in this study were those with a negative history of stroke or other severe neurologic disorders, chronic obstructive pulmonary disease, and ejection fraction (EF) less than 30%. On the other hand, patients below the age of 18 or over 80, with chest tube drainage >400 mL/h at the first 4 h after surgery, hemodynamic instability (requiring intra-aortic balloon pump or high dose inotrope), loss of consciousness, and Those who were expected to require MV more than 24 h were excluded.
We calculated the sample size of this study based on the Altman’s nomogram for the two-sided hypothesis with a power of 90% and α = 0.05 and according to similar studies for the weaning time variable (p = 0.03 and the effect size = 1.3) (23). Based on the nature of the clinical trial study and the probability of sample size drop, 10% drop was considered as the attrition rate and the final sample size for each group was considered to be 35 subjects.
Our center is a single specialty heart center with a multi-disciplinary team including cardiac surgeon, cardiac anesthesiologist, nurses, internal medicine, echocardiographist, perfusionist, electro-physiologist, interventionist, and cardiac rehabilitation specialist. Patients who are candidate for surgery are assessed by anesthesiologist before surgery. Also, all patients above 60 years old are screened by pulmonologist and based on comorbidities, patients are screened by nephrologist, neurologist, endocrinologist and hematologist. Our ICU is a 10-bed ICU which is designed for cardiac surgical procedures. The ICU and operation room are in the same environment and on two floors. After the surgery, patients are transferred directly to the ICU and managed by experienced nurses. Usually, patients remain in ICU for two days, and the enhanced recovery after surgery protocols, including fast tract extubation, early mobilization, and minimal sedation strategy, are utilized. Sedation infusion and also using from bolus doses of sedatives such as midazolamis discouraged and patients are oriented as soon as possible. Fast tract extubation is the routine procedure during the weaning and extubation.
Anesthesia and surgical protocols were similar in both groups. Anesthesia was induced and maintained using midazolam, fentanyl, and propofol, and paralysis was achieved by atracurium. The patients were intubated after anesthesia induction and ventilated during the surgery. The following setting was applied in the operating room: tidal volume of 8–10 mL/kg, positive end-expiratory pressure (PEEP) of 5 cmH2O, and respiratory rate (RR) of 12 breaths per minute. During cardiopulmonary bypass, ventilation was stopped and continuous positive airway pressure of 5 cmH2O was applied. We performed the surgery using the standard procedure through median sternotomy (24). Following the surgery, adaptive support ventilation (ASV) was applied for mechanical ventilation management. A Galileo with software version GBC 01.202 (Hamilton Medical AG, Rhäzüns, Switzerland) was employed for managing the patient during the MV. Although weaning and extubation is a clinical decision made at the bedside, it is based on many factors including wakefulness, comfort, and the patient’s ability to cough and secrete. In both groups, the MV weaning criteria were MIN VOL% 60–65%, F control (number of controlled breathes) zero, f Spont >10 (number of spontaneous breathes), p insp <8 (the amount of automatically adjusted pressure support). Figure 1 represents standard weaning process algorithms in ASV mode (25).
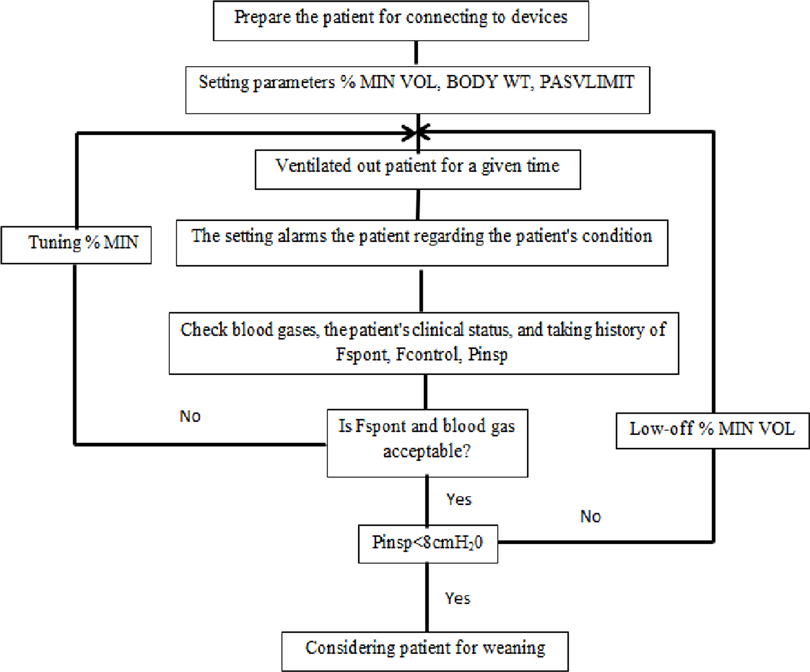
Figure 1. Standard weaning process algorithm in adaptive support ventilation (ASV) mode. MIN VOL, minute volume; WT, weight; F spont, frequency of spontaneous breathing; F control, frequency of controlled breathing; P insp, inspiratory pressure.
In both groups, the initial ventilator settings were minute volume 100%, oxygen inspiratory fraction (Fio2) of 100%, positive end-expiratory pressure of 5 cm H2O, and flow trigger sensitivity of 4 L/min. Following 10 min, we performed an ABG analysis. Simultaneously, the ETCO2 and SPO2 were measured. The goal for PaCO2 was 38–43 mmHg. Based on our clinical pilot, the Etco2 was 2–4 mmHg lower than PaCO2. Therefore, this difference was considered in all the settings and interpretations regarding PaCO2. If the PaCO2 was greater than 45 the minute volume increased by 10%–20%, and if it was lower than 35 the minute volume decreased 10%–20%. In the intervention group, the trend was monitored with capnography and in the control group, another ABG analysis was performed 10–20 min after any changes in the setting. In the intervention group point by point changes were made in ventilation and oxygenation based on continuous monitoring of capnography and pulse oximetry. The capnography and pulse oximetry, used in this study provided by Pooyandegan Rah Saadat Company. The capnography device was a main wave form of capnography. The FIO2 was changed to target oxygen saturation about 95%. This was measured in the control group with ABG or pulse oximetry and in the intervention group with pulse oximetry. Equal basic settings were employed on both groups and Fast-track extubation was employed for all the patients.
Adaptive Support Ventilation (ASV) is an intelligent advanced closed-loop ventilation mode that maintains constant minimum mandatory ventilation based on preset minute volume% and ideal body weight. Depending on patients’ status, this mode provides a range of ventilation support including Pressure Controlled Ventilation (PCV), Synchronized Intermittent Mandatory Ventilation (SIMV), or Pressure Support Ventilation (PSV). Ventilator switches between these forms automatically. ASV adjusts respiratory rate, tidal volume, and inspiratory time continuously and it depends on the mechanism of the lung and the efforts of the patients (26, 27). The controlled settings of this mode included the following items: patients’ ideal body weight (IBW), the value of minute respiratory volume in percentage (Min volume), positive end expiratory pressure (PEEP), fraction of inspired oxygen (Fio2), the level of ventilator sensitivity for the breath of the patient (Trigger), and the maximum pressure that must be applied (cmH2o). The most important settings in ASV are ideal body weight and Minute volume. The ventilator uses the Otis equation for determining the appropriate rate and volume based on measuring patients’ respiratory compliance and resistances during the initial five breaths. By improving the patient situation, ventilator switches from controlled breaths to spontaneous breaths. During the spontaneous breathing, gradually by improving the patient situation, the inspiratory pressure support decreases. Ventilator continuously adapts the settings and supports patients’ needs.
In spite of published data about capnography, it is not used widely in Iranian clinical practice. For this reason, in order to reduce the staff, fear of its accuracy a 4-hour training class was conducted for ICU staff with clinical work in the pilot phase for one month. In those sessions, the data from the capnography and ABG were compared and the results were presented to them. Based on our data, the Etco2 was usually 2–4 mmHg lower than PaCO2. Thus, this difference was considered in all the settings and interpretation regarding PaCO2.
Categorical variables were described as frequency rates and percentages, and continuous variables were described using mean ± standard deviation (SD) values. The comparison of demographic characteristics and baseline measures between the two groups herein were done with independent t-test for continuous variables and Chi-square test or Fisher’s exact test (in case of low sample) for categorical variables. The normality of the numeric variables was checked employing Kolmogorov-Smirnov test. The repeated measures analysis of variance (RMANOVA) was used to compare the vital signs and ABG measurements between the groups. Furthermore, we did pairwise comparisons with Sidak post hoc test. The assumption of sphericity was addressed utilizing Mauchly’s test of sphericity. Once the assumption was not satisfied (p < 0.05), the Greenhouse-Geiser correction of p-value was utilized. To assess the effect of intervention, we used the analysis of covariance (ANCOVA) after controlling for baseline measures and confounders in the main effect model. All the data were analyzed using the Statistical Package for the Social Sciences (SPSS) 21.0 statistical package (Chicago, IL, USA); two-side p < 0.05 indicated a statistically significant difference.
A total of 70 patients enrolled in the current study according to the inclusion and exclusion criteria. Three patients were excluded due to hemodynamic instability (1 subject from the intervention group) and bleeding (2 subjects from the control group). Therefore, the analyses were performed in the remaining 67 patients (34 patients in the intervention group and 33 patients in the control group). Figure 2 depicts the patients’ flowchart of the study.
The mean ± SD ages of patients in the intervention and control groups were 58.1 ± 9.6 and 60.8 ± 9.3 years, respectively. There were no significant differences between the groups in terms of age (p = 0.244). In terms of gender, 19 participants (55.9%) in the intervention group and 22 (66.7%) in the control group were male (p = 0.365). Baseline demographic and clinical characteristics of the participants in the two groups are presented in Table 1. Based on our findings, there were no significant differences between the groups regarding the demographic characteristics and baseline ABG measurements (p > 0.05). However, in terms of intraoperative parameters, the duration of the surgery (based minutes) in the control group was significantly lower than that in the intervention group (235.7 ± 49.2 min vs. 259 ± 39.8 min, p = 0.035).
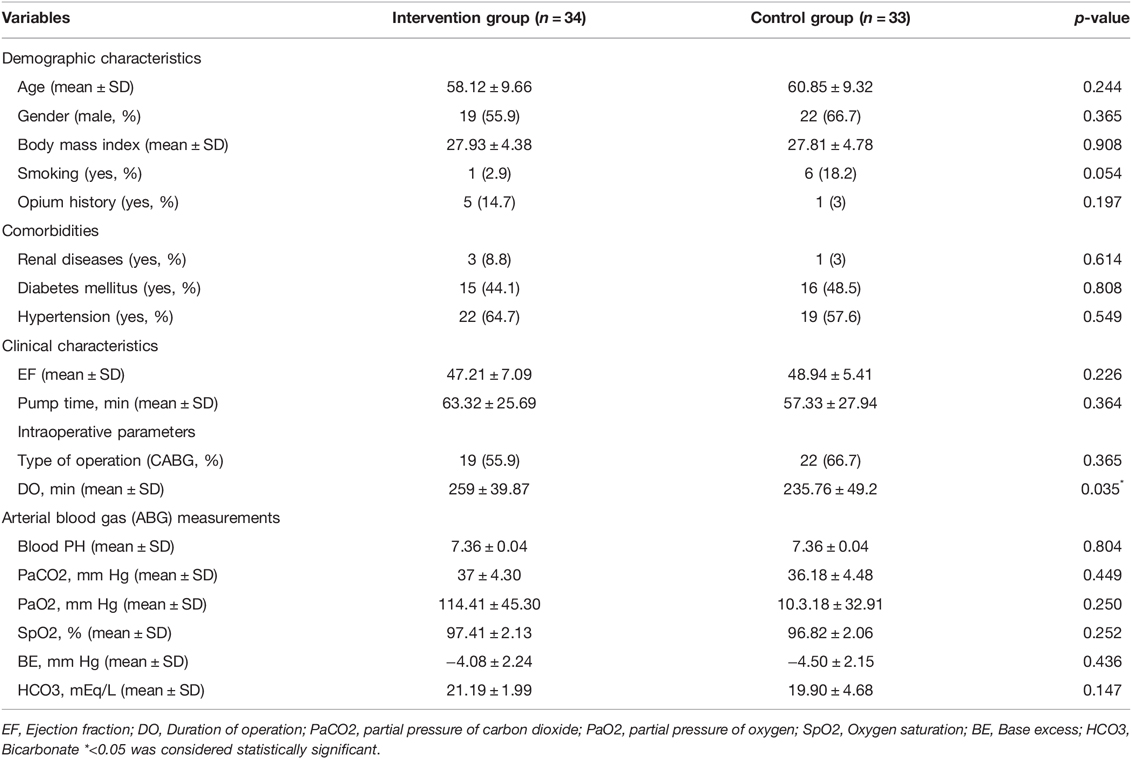
Table 1. Baseline demographic and clinical characteristics of the participants in two groups of study.
Comparisons of hemodynamic parameters and vital signs of the patients on different times between the two groups and within group are respectively presented in Tables 2 and 3. There were significant differences between the intervention and control groups concerning tidal volume (VT) p = 0.016, inspiratory pressure (Pi) p = 0.006, and fraction of inspired oxygen (Fio2) p = 0.002. Nevertheless, the differences of other characteristics between the two groups were not significant (p > 0.05).
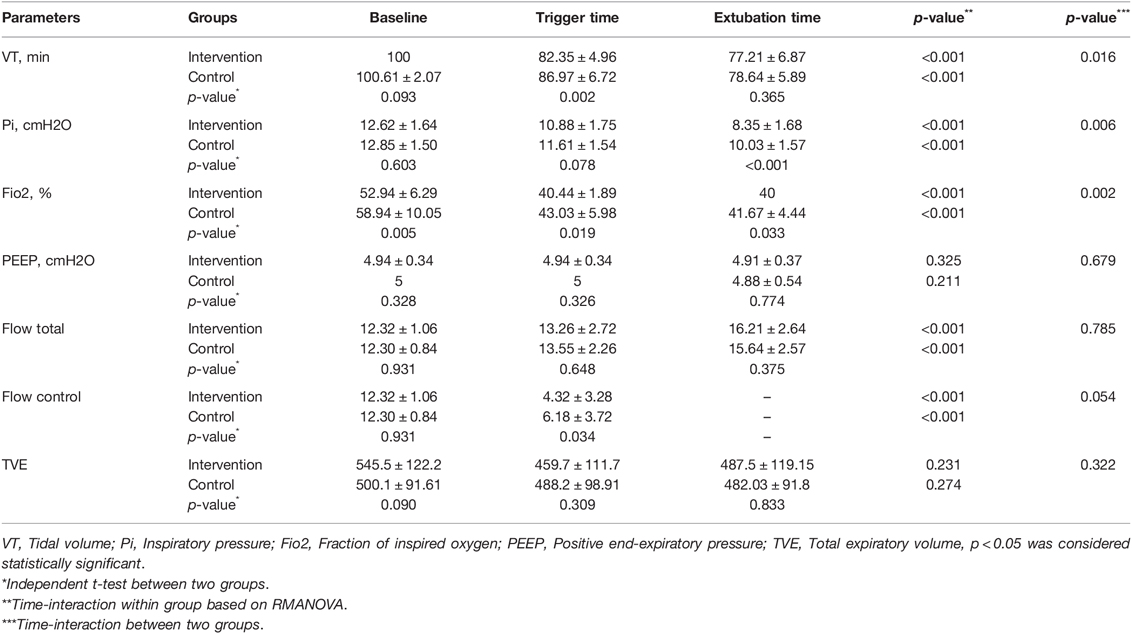
Table 2. Comparison of ventilator and respiratory in three different times between the intervention and control groups.
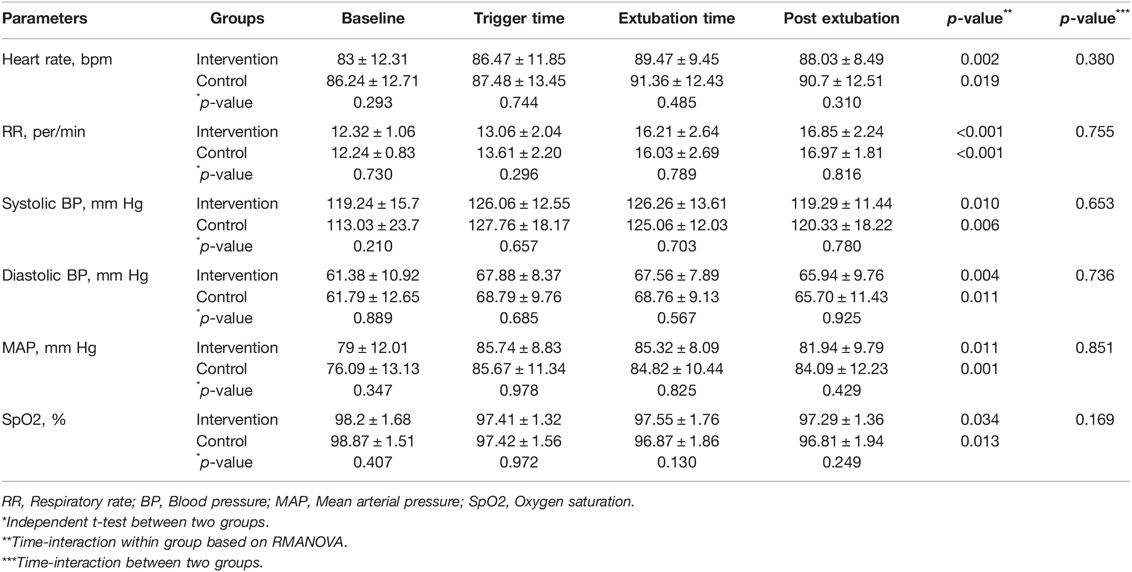
Table 3. Comparison of vital signs of patients on different times between the intervention and control groups.
Figure 3 shows ETCO2 level distribution of patients in intervention group compare with the PaCO2 in control group at extubation time. The mean of ETCO2 in the intervention group was compared to the PaCO2 in the control group at extubation time. The data indicated no statistically significant differences between them (39.5 ± 3.0 vs. 39.4 ± 4.3, 95% CI, −1.7–1.8, p = 0.935).
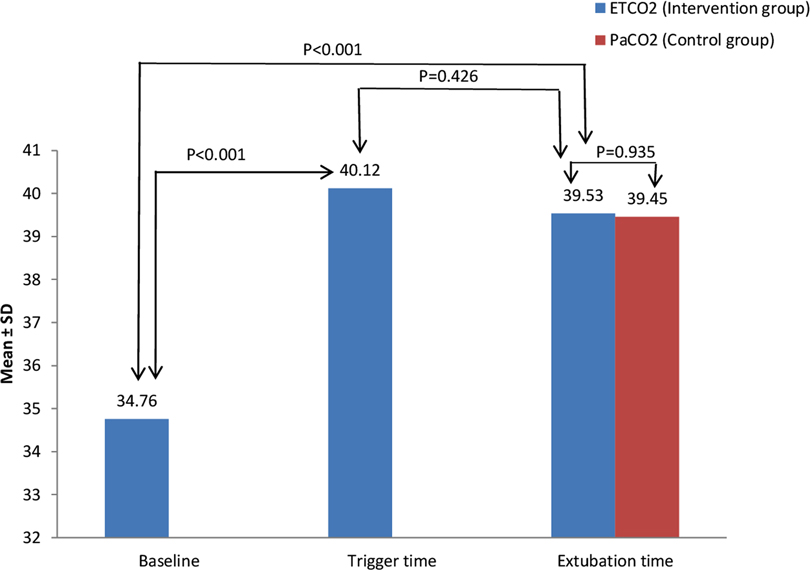
Figure 3. ETCO2 level distribution in the intervention group compare with PaCO2 in the control group at extubation time
The mean duration of MV was 212.2 ± 80.6 (min) and 342.7 ± 110.7 (min) in the intervention and control groups, respectively (p < 0.001). FTE (MV duration <6 hours) was observed in 33 (97.1%) of the patients in the intervention group and 18 (54.5%) of the patients in the control group. The intervention group was of 4.8 (95% CI, 1.4–15.5; p = 0.008) times more chance than the control group from FTE perspective. However, the differences in the length of stay in ICU between the two groups was not significant (p = 0.219). The number of alarms (p < 0.001) and manual ventilator setting changes (p = 0.027) were significantly lower in the intervention group. In addition, no significant differences were observed in compliance between the groups (p = 0.289). Meanwhile, the differences in the mean of airway resistant between the two groups was significant (p = 0.045). Comparison of extubation time, length of ICU stays, airway resistance, and compliance are listed in Tables 4 and 5.
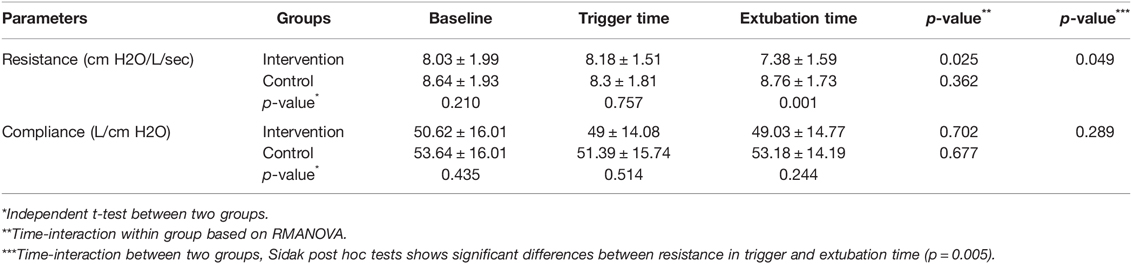
Table 4. Comparison of airway resistance and compliance in different times between the intervention and control groups.
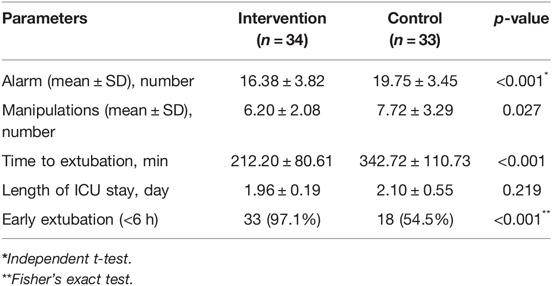
Table 5. Comparison of extubation time and length of ICU stay between the intervention and control groups.
In this study, the use of non-invasive monitoring including capnography and pulse oximetry accelerated the weaning process and increased the number of FTE in intervention group. According to the results of the present study, in terms of vital signs and the amount of arterial oxygen saturation (SpO2), there were no significant differences between the intervention and control groups. However, there was a significant difference between the two groups regarding tidal volume (VT), inspiratory pressure (Pi), and fraction of inspired oxygen (Fio2). In the current study, the number of manual setting changes of ventilator and alarms in the intervention group significantly decreased compared to the control group. The reduction in both alarm and manual setting changes is of great importance. In fact, the increase in the number of alarms may lead to alarm fatigue, which is an important concern for patients’ safety (28–30).
In addition, our data revealed no significant differences between the values of PaCO2 and ETCO2 at the weaning time; however, we observed a statistically significant linear relationship between them (p < 0.001). PaCO2 and ETCO2 had a strongly positive correlation (r = 0.918), meaning that these variables tend to increase together. In other words, ETCO2 could be used instead of PaCO2 for monitoring. In this regard, the results of the present study are consistent with those of the studies conducted by Taghizadeh et al. (10), Aminiahidashti et al. (31), McSwain et al. (32), Moses et al. (33), and Garcia et al. (34). They all reported the same results in terms of the correlation between ETCO2 and PaCO2 and suggested that capnography could be employed as a non- invasive method, and it is a surrogate for PaCO2 which if high, signals a respiratory acidosis or if low, a respiratory alkalosis or when combined with pH and serum bicarbonate, a compensatory mechanism. In contrast to our results, certain studies have reported that the correlation between these variables is not sufficient (35–37). A pilot study by Drew et al. (38), in which they used non-invasive methods during the weaning process, exhibited that the hypothesis that capnography would allow more rapid weaning from MV, and requires fewer ABGs during the process, was not true. Moreover, in a study by Casati et al. (39), the role of capnography was reported to be inappropriate in patients with spontaneous breathing. This contradiction may be attributed to the different research methods or different populations. For example, some studies have generally not included a comprehensive statistical analysis accounting for the differences in physiologic dead space ventilation and the resulting gradient between ETCO2 and PaCO2. In addition, some other studies have been reviewed in patients with critical conditions.
The results of this work revealed that the use of capnography and pulse oximetry accelerated the weaning process in the patients undergoing CABG surgery. FTE is found to be the best practice for management of cardiac surgery patients, which improves the recovery and reduces the complications (40). In this study 97.1% of the intervention group and 54.5% of the control group had FTE, which was reported 49.5% FTE in a study by Akhtar et al. (5). Our results showed that the use of capnography could improve the FTE by the identification of hypercapnic episodes during the weaning process. In some centers, due to the fear of hypercapnic episodes, the FTE is delayed. Hence, using ETCO2 with continuous monitoring can reduce this fear. On the other hand, one of the uses of capnography is the discovery of hypercapnic episodes (41).
In some studies, changes in ETCO2 was observed from breath to breath and from the controlled to the spontaneous breathing (6). Therefore, the momentary monitoring is not reliable and the ETCO2 should be monitored continuously during the weaning process. Due to the importance of FTE in cardiac surgery, various changes are made to MV settings in a short time. Due to some restrictions such as limited access to ABG analyzers in developing countries and the fact that ABG method is an invasive method, a non-invasive monitor, which is easily accessible, inexpensive, and accurate, is very useful. The available data showed that both capnography and pulse oximetry have the above-mentioned features.
Despite the availability of capnography in many ICUs, it is not frequently used in the routine practice. One of the reasons might be the medical staff’s fear of the risks and the proper linkage between the PaCO2 and ETCO2 (42, 43). As mentioned in the method section, we had a 4-hour class with a pilot clinical phase for assuring the staff of the accuracy of Etco2. This increased the trust of ICU staff.
The principal strength of this study is being conducted in a real-world setting. All the patients were screened by a pulmonologist and the medical staffs in our center were trained. The limitation of this study is the sample size which was small; therefore, it was not possible to determine the cutting point for ETCO2. Accordingly, a larger sample size study is recommended to determine the cutting point.
Using the non-invasive monitors including capnography and pulse oximetry enhances the rate of FTE in cardiac surgery. It is also a safe and correct monitor and could be a good alternative for ABG in this population. Nevertheless, the fact that in some conditions the relationship between ETCO2 and PaCO2 was not well described primarily necessitates the determination of a capnography on which patients could rely. Precautions should be taken and other respiratory parameters, including tidal volume and respiratory rate, should be taken into consideration. In addition, further studies are required with larger sample sizes in different disease status and populations for the assessment of the accuracy of our findings.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by Ethics Committee of Baqiyatallah University of Medical Sciences, Tehran, Iran, “IR.BMSU.REC.1395.141”. The patients/participants provided their written informed consent to participate in this study.
AV-A developed the study concept. All authors contributed to the study design. Testing and data collection were performed by STM, FB and AV-A. The data analysis and interpretation was performed by FB and MSG under the supervision of AV-A. All authors contributed to the article and approved the submitted version.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Thanks to guidance and advice from the “Clinical Research Development Unit of Baqiyatallah Hospital”.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Badhwar V, Esper S, Brooks M, Mulukutla S, Hardison R, Mallios D, et al. Extubating in the operating room after adult cardiac surgery safely improves outcomes and lowers costs. J Thorac Cardiovasc Surg. (2014) 148:3101–9.e1. doi: 10.1016/j.jtcvs.2014.07.037
2. Cheng DC, Karski J, Peniston C, Asokumar B, Raveendran G, Carroll J, et al. Morbidity outcome in early versus conventional tracheal extubation after coronary artery bypass grafting: a prospective randomized controlled trial. J Thorac Cardiovasc Surg. (1996) 112:755–64. doi: 10.1016/s0022-5223(96)70062-4
3. García-Delgado M, Navarrete-Sánchez I, Colmenero M. Preventing and managing perioperative pulmonary complications following cardiac surgery. Curr Opin Anaesthesiol. (2014) 27:146–52. doi: 10.1097/aco.0000000000000059
4. Reis J, Mota JC, Ponce P, Costa-Pereira A, Guerreiro M. Early extubation does not increase complication rates after coronary artery bypass graft surgery with cardiopulmonary bypass. Eur J Cardiothorac Surg. (2002) 21:1026–30. doi: 10.1016/s1010-7940(02)00121-5
5. Akhtar MI, Hamid M. Success and failure of fast track extubation in cardiac surgery patients of tertiary care hospital: one year audit. J Pak Med Assoc. (2009) 59:154–6. http://ecommons.aku.edu/pakistan_fhs_mc_surg_cardiothoracic/21
6. Gerdung CA, Adeleye A, Kirk VG. Noninvasive monitoring of CO2 during polysomnography: a review of the recent literature. Curr Opin Pulm Med. (2016) 22:527–34. doi: 10.1097/mcp.0000000000000320
7. Lakhal K, Robert-Edan V. Invasive monitoring of blood pressure: a radiant future for brachial artery as an alternative to radial artery catheterisation? J Thorac Dis. (2017) 9:4812–6. doi: 10.21037/jtd.2017.10.166
8. Sood P, Paul G, Puri S. Interpretation of arterial blood gas. Indian J Crit Care Med. (2010) 14:57–64. doi: 10.4103/0972-5229.68215
9. Long B, Koyfman A, Vivirito MA. Capnography in the emergency department: a review of uses, waveforms, and limitations. J Emerg Med. (2017) 53:829–42. doi: 10.1016/j.jemermed.2017.08.026
10. Taghizadieh A, Pouraghaei M, Moharamzadeh P, Ala A, Rahmani F, Basiri Sofiani K. Comparison of end-tidal carbon dioxide and arterial blood bicarbonate levels in patients with metabolic acidosis referred to emergency medicine. J Cardiovasc Thorac Res. (2016) 8:98–101. doi: 10.15171/jcvtr.2016.21
11. Nitzan M, Romem A, Koppel R. Pulse oximetry: fundamentals and technology update. Med Devices (Auckl). (2014) 7:231–9. doi: 10.2147/mder.s47319
12. Cambra Lasaosa FJ, Pons Odena M. [Pulse oximetry and capnography]. An Pediatr (Barc). (2003) 59:259–64. doi: 10.1016/s1695-4033(03)78176-4
13. Nassar BS, Schmidt GA. Capnography during critical illness. Chest. (2016) 149:576–85. doi: 10.1378/chest.15-1369
14. Kugelman A, Zeiger-Aginsky D, Bader D, Shoris I, Riskin A. A novel method of distal end-tidal CO2 capnography in intubated infants: comparison with arterial CO2 and with proximal mainstream end-tidal CO2. Pediatrics. (2008) 122:e1219–24. doi: 10.1542/peds.2008-1300
15. Cumming C, McFadzean J. A survey of the use of capnography for the confirmation of correct placement of tracheal tubes in pediatric intensive care units in the UK. Paediatr Anaesth. (2005) 15:591–6. doi: 10.1111/j.1460-9592.2005.01490.x
16. Turle S, Sherren PB, Nicholson S, Callaghan T, Shepherd SJ. Availability and use of capnography for in-hospital cardiac arrests in the United Kingdom. Resuscitation. (2015) 94:80–4. doi: 10.1016/j.resuscitation.2015.06.025
17. Pantazopoulos C, Xanthos T, Pantazopoulos I, Papalois A, Kouskouni E, Iacovidou N. A review of carbon dioxide monitoring during adult cardiopulmonary resuscitation. Heart Lung Circ. (2015) 24:1053–61. doi: 10.1016/j.hlc.2015.05.013
18. Rasera CC, Gewehr PM, Domingues AM. PET(CO2) measurement and feature extraction of capnogram signals for extubation outcomes from mechanical ventilation. Physiol Meas. (2015) 36:231–42. doi: 10.1088/0967-3334/36/2/231
19. Warner KJ, Cuschieri J, Garland B, Carlbom D, Baker D, Copass MK, et al. The utility of early end-tidal capnography in monitoring ventilation status after severe injury. J Trauma. (2009) 66:26–31. doi: 10.1097/TA.0b013e3181957a25
20. Kerr ME, Zempsky J, Sereika S, Orndoff P, Rudy EB. Relationship between arterial carbon dioxide and end-tidal carbon dioxide in mechanically ventilated adults with severe head trauma. Crit Care Med. (1996) 24:785–90. doi: 10.1097/00003246-199605000-00010
21. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. (2013) 310:2191–4. doi: 10.1001/jama.2013.281053
22. Jayaraman J. Guidelines for reporting randomized controlled trials in paediatric dentistry based on the CONSORT statement. Int J Paediatr Dent. (2020) 31(Suppl 1):38–55. doi: 10.1111/ipd.12733
23. Salmani F, Yazdannik A. Evaluation of nurse’s participation in patient weaning from mechanical ventilation on the outcoms. Iran J Med Surgl Nurs. (2013) 1:6.
24. Aybek T, Dogan S, Neidhart G, Kessler P, Matheis G, Wimmer-Greinecker G, et al. Coronary artery bypass grafting through complete sternotomy in conscious patients. Heart Surg Forum. (2002) 5:17–20; discussion -1. https://pubmed.ncbi.nlm.nih.gov/11937456/
25. Fernández J, Miguelena D, Mulett H, Godoy J, Martinón-Torres F. Adaptive support ventilation: state of the art review. Indian J Crit Care Med. (2013) 17:16–22. doi: 10.4103/0972-5229.112149
26. Arnal J-M, Wysocki M, Nafati C, Donati S, Granier I, Corno G, et al. Automatic selection of breathing pattern using adaptive support ventilation. Intensive Care Med. (2008) 34:75–81. doi: 10.1007/s00134-007-0847-0
27. Moradian ST, Saeid Y, Ebadi A, Hemmat A, Ghiasi MS. Adaptive support ventilation reduces the incidence of atelectasis in patients undergoing coronary artery bypass grafting: a randomized clinical trial. Anesthesiol Pain Medicine. (2017) 7. doi: 10.5812/aapm.44619
28. Ruskin KJ, Hueske-Kraus D. Alarm fatigue: impacts on patient safety. Curr Opin Anaesthesiol. (2015) 28:685–90. doi: 10.1097/aco.0000000000000260
29. Sendelbach S, Funk M. Alarm fatigue: a patient safety concern. AACN Adv Crit Care. (2013) 24:378–86; quiz 87–8; doi: 10.1097/NCI.0b013e3182a903f9
30. Jones K. Alarm fatigue a top patient safety hazard. CMAJ. (2014) 186:178. doi: 10.1503/cmaj.109-4696
31. Aminiahidashti H, Shafiee S, Zamani Kiasari A, Sazgar M. Applications of end-tidal carbon dioxide (ETCO2) monitoring in emergency department; a narrative review. Emergency (Tehran, Iran). (2018) 6:e5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5827051/
32. McSwain SD, Hamel DS, Smith PB, Gentile MA, Srinivasan S, Meliones JN, et al. End-tidal and arterial carbon dioxide measurements correlate across all levels of physiologic dead space. Respir Care. (2010) 55:288–93. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2837928/
33. Moses JM, Alexander JL, Agus MS. The correlation and level of agreement between end-tidal and blood gas pCO2 in children with respiratory distress: a retrospective analysis. BMC Pediatr. (2009) 9:20. doi: 10.1186/1471-2431-9-20
34. Garcia E, Abramo TJ, Okada P, Guzman DD, Reisch JS, Wiebe RA. Capnometry for noninvasive continuous monitoring of metabolic status in pediatric diabetic ketoacidosis. Crit Care Med. (2003) 31:2539–43. doi: 10.1097/01.ccm.0000090008.79790.a7
35. Kugelman A, Bromiker R, Riskin A, Shoris I, Ronen M, Qumqam N, et al. Diagnostic accuracy of capnography during high-frequency ventilation in neonatal intensive care units. Pediatr Pulmonol. (2016) 51:510–6. doi: 10.1002/ppul.23319
36. Cantó EG, Laso AG, Macián I, Pérez AA, Sopena FM. [The value of capnography and exhaled CO2 in neonatal intensive care units]. An Esp Pediatr. (1997) 47:177–80. https://pubmed.ncbi.nlm.nih.gov/9382351/
37. Heines SJ, Strauch U, Roekaerts PM, Winkens B, Bergmans DC. Accuracy of end-tidal CO2 capnometers in post-cardiac surgery patients during controlled mechanical ventilation. J Emerg Med. (2013) 45:130–5. doi: 10.1016/j.jemermed.2012.11.019
38. Drew K, Brayton M, Ambrose A, Bernard G. End-tidal carbon dioxide monitoring for weaning patients: a pilot study. Dimens Crit Care Nurs. (1998) 17:127–34. doi: 10.1097/00003465-199805000-00002
39. Casati A, Gallioli G, Scandroglio M, Passaretta R, Borghi B, Torri G. Accuracy of end-tidal carbon dioxide monitoring using the NBP-75 microstream capnometer. A study in intubated ventilated and spontaneously breathing nonintubated patients. Eur J Anaesthesiol. (2000) 17:622–6. doi: 10.1046/j.1365-2346.2000.00731.x
40. Gutsche JT, Erickson L, Ghadimi K, Augoustides JG, Dimartino J, Szeto WY, et al. Advancing extubation time for cardiac surgery patients using lean work design. J Cardiothorac Vasc Anesth. (2014) 28:1490–6. doi: 10.1053/j.jvca.2014.05.024
41. Saura P, Blanch L, Lucangelo U, Fernández R, Mestre J, Artigas A. Use of capnography to detect hypercapnic episodes during weaning from mechanical ventilation. Intensive Care Med. (1996) 22:374–81. doi: 10.1007/bf01712151
42. Georgiou AP, Gouldson S, Amphlett AM. The use of capnography and the availability of airway equipment on Intensive Care Units in the UK and the Republic of Ireland. Anaesthesia. (2010) 65:462–7. doi: 10.1111/j.1365-2044.2010.06308.x
Keywords: airway extubation, coronary artery bypass, capnography, blood gas analysis, pulse oximetry
Citation: Moradian ST, Beitollahi F, Ghiasi MS and Vahedian-Azimi A (2022) Capnography and Pulse Oximetry Improve Fast Track Extubation in Patients Undergoing Coronary Artery Bypass Graft Surgery: A Randomized Clinical Trial. Front. Surg. 9:826761. doi: 10.3389/fsurg.2022.826761
Received: 1 December 2021; Accepted: 21 April 2022;
Published: 11 May 2022.
Edited by:
Pilly Chillo, Muhimbili University of Health and Allied Sciences, TanzaniaReviewed by:
Rhodri Saunders, Coreva Scientific, GermanyCopyright © 2022 Moradian, Beitollahi, Ghiasi and Vahedian-azimi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amir Vahedian-Azimi Amirvahedian63@gmail.com
Specialty section: This article was submitted to Heart Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.