- Department of General Surgery, Tianjin Medical University General Hospital, Tianjin, China
Background: Solitary cecal ulcer is a rare disease. Its etiology is unknown and there are no pathognomonic symptoms. There are rare reports mimicking carcinoma as seen in this case.
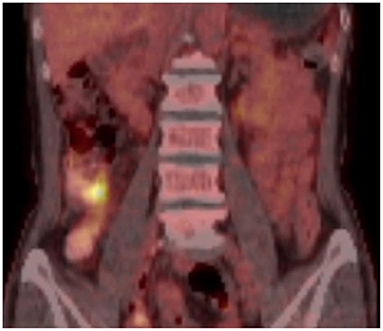
Case Presentation: A 64 year-old woman presented with a history of intermittent right lower abdominal pain for 20 years and worsening for 1 year. Colonoscopy revealed an enormous cecal ulcer. The PET-CT showed increased metabolism of the lesion. She underwent a right hemicolectomy. Histopathological examination revealed chronic non-specific inflammation. A rare diagnosis of the solitary cecal ulcer was ultimately made.
Conclusion: Solitary cecal ulcer is a rare, idiopathic entity. It mimics inflammatory bowel disease, malignancy, infection, etc. The comprehensive images of this case describe the characteristics of the disease.
Introduction
Solitary cecal ulcer is rare. Its etiology is unknown, and there are no pathognomonic symptoms. Its clinical presentation is varied, but abdominal pain is common. The PET-CT or CT may suggest a carcinoma. The definitive diagnosis is made only on histopathological examinations. We describe comprehensive images including PET-CT, colonoscopy, specimen, and pathology. These images describe the characteristics of the disease. Meanwhile, we review pieces of literature on this rare disease.
Case Presentation
A 64 year-old woman presented to the outpatient department with a history of intermittent right lower abdominal pain for 20 years and worsening for 1 year with no weight loss. She was a non-smoker and had unremarkable medical and family medical histories. Recently, she took mesarazine intermittently without marked remission. A physical examination was notable for a palpable mass and tenderness on the right lower abdomen. The laboratory studies showed no abnormality, except for a c-reactive protein level of 2.58 mg per deciliter (reference range, <0.8). The CT imaging showed that the ileocecal intestinal wall was thickened (Figure 1). Colonoscopy revealed a cecal enormous ulcer (Figure 2). The pathology reminded of nothing except for non-specific inflammation, so a PET-CT was arranged and showed the increased metabolism (Figure 3, SUVmax: 9.3) of the lesion. She underwent a right hemicolectomy in case of a malignancy. An isolated, well-circumscribed ileocecal ulcer could be seen with a size of about 2*2 cm (Figure 4A). The histopathological examination (Figure 4B) revealed chronic inflammation and significant fibrosis at the edges and bottom of the ulcer, lymphocyte hyperplasia, and several lymph nodes were benign. The mucous crypt was normal with no evidence of granulomas, cancer. After exclusion of other possible diagnoses, the rare diagnosis of the solitary cecal ulcer was ultimately made. The patient remained well a year after surgery.
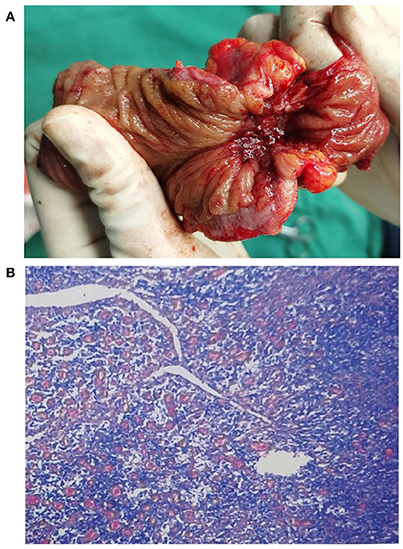
Figure 4. (A) An isolated, well-circumscribed ileocecal ulcer could be seen in the surgical specimen; (B) The post-operative pathological analysis revealed chronic non-specific inflammation (hematoxylin and eosin, original magnification 20 ×).
Discussion
Solitary ulcer in the colon is rare. Only a few cases in the literature describe the characteristics of solitary cecal ulcer. McCarthy and Beveridge (1) and Last and Lavery (2) reported a case of solitary cecal ulcer with hemorrhage separately. Yeom et al. (3) reported a case of multiple pyogenic liver abscesses caused by the micro-perforation of idiopathic cecal ulcer. González-Urquijo et al. (4) reported a case of a patient presenting with a solitary cecal ulcer associated with non-steroidal anti-inflammatory drugs (NSAIDs) intake, mimicking a malignant lesion, and a laparoscopy right colectomy was performed. In addition, conditions that mimic appendicitis (5) and coexists appendix carcinoid tumors (6) have been reported. Ong et al. (7) described the experience of 10 patients with benign caecal ulcers.
The signs and symptoms of solitary cecal ulcers are non-specific, and the disease has no pathognomonic signs, which leads to the fact that the solitary cecal ulcer is often misdiagnosed as acute appendicitis (8). The most common symptom is right lower abdominal pain, but other symptoms include melena, constipation, diarrhea, and weight loss (5, 8, 9). Diagnosis is difficult to make preoperatively and intraoperatively, and definitive diagnosis is usually obtained by surgical and/or colonoscopic histological biopsy (10, 11).
Solitary cecal ulcer has a small incidence. They can appear in every age group but have a slightly higher incidence in patients aged 40–60 years and are more common in women (12, 13). The etiology is unknown, and other than the leading cause being consumption of non-steroid anti-inflammatory drugs (9, 14, 15), there are others such as the Solitary Rectal Ulcer Syndrome, sterocoraceus ulcer, ischemic ulcer, or ulcers caused by infections, among other even less common causes (9, 13). These etiologies are most commonly found in the left colon and rectum, and NSAIDs ulcers are mainly found in the cecum and right colon.
The CT scan of a chronic solitary cecal ulcer is very similar to those of a cecal carcinoma, with the colonic wall thickening by edema in the sub-serous layer, striations in the pericolonic adipose tissue (9). This is consistent with the findings in our patient. This is a key element to explain our decision of the pathology reminded nothing except for non-specific inflammation, and the PET-CT showed characteristics mimicking carcinoma. Diagnosis relies on colonoscopy with a biopsy taken from the ulcer to rule out malignant lesions. In patients with a possible diagnosis of inflammatory bowel disease, random samples should be taken from the entire colon (9, 13).
The treatment should consist of the immediate discontinuation of NSAID therapy, a high fiber diet to avoid constipation, and conservative care at first (9). An operation should be considered when the symptoms persist, severe gastrointestinal bleeding secondary to cecal ulceration or a malignant lesion cannot be ruled out (7).
Conclusion
In summary, solitary cecal ulcer is rare. Its etiology is unknown. It needs to be differentiated from malignant lesions, infection and inflammatory bowel diseases, etc. An operation should be considered when the symptoms persist, severe gastrointestinal bleeding secondary to cecal ulceration or a malignant lesion cannot be ruled out.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
CL and A-QH wrote the manuscript and were assistants in surgery. GL was the chief operating surgeon. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. McCarthy JH, Beveridge BR. Solitary caecal ulcer as a cause of gastrointestinal bleeding. Med J Aust. (1984) 141:530–1. doi: 10.5694/j.1326-5377.1984.tb132913.x
2. Last MD, Lavery IC. Major hemorrhage and perforation due to a solitary cecal ulcer in a patient with end-stage renal failure. Dis Colon Rectum. (1983) 26:495–8. doi: 10.1007/BF02563737
3. Yeom DH, Sohn KC, Chu MS, Jo DH, Cho EY, Kim HC. Multiple pyogenic liver abscesses caused by microperforation of an idiopathic cecal ulcer. Korean J Gastroenterol. (2016) 67:44–8. doi: 10.4166/kjg.2016.67.1.44
4. González-Urquijo M, Rojas-Méndez J, Tijerina-Gomez LO. Solitary ulcer in cecum, mimicking a carcinoma: a case report. Ann Med Surg. (2017) 21:45–8. doi: 10.1016/j.amsu.2017.07.041
5. Atila K, Güler S, Gönen C, Sarioglu S, Bora S. Benign solitary cecal ulcer: a condition that mimics plastron appendicitis. Ulus Travma Acil Cerrahi Derg. (2010) 16:579–81.
6. Ince V, Barut B, Karakaş S. Co-existence of idiopathic cecal ulcer and incidental appendix carcinoid tumor. Ulus Cerrahi Derg. (2015) 32:285–6. doi: 10.5152/UCD.2015.2861
7. Ong J, Lim KH, Lim JF, Eu KW. Solitary caecal ulcer syndrome: our experience with this benign condition. Colorectal Dis. (2011) 13:786–90. doi: 10.1111/j.1463-1318.2010.02261.x
8. Chi KD, Hanauer SB. Benign solitary cecal ulcer: a case report and review of the literature. Dig Dis Sci. (2003) 48:2207–12. doi: 10.1023/B:DDAS.0000004527.77947.fd
9. Davies NM. Toxicity of nonsteroidal anti-inflammatory drugs in the large intestine. Dis Colon Rectum. (1995) 38:1311–21. doi: 10.1007/BF02049158
10. Agha RA, Fowler AJ, Saeta A, Barai I, Rajmohan S, Orgill DP. The SCARE statement: consensus-based surgical case report guidelines. Int J Surg. (2016) 34:180–6. doi: 10.1016/j.ijsu.2016.08.014
11. Castillo Contreras O, Salazar Muente F, Young Tabusso F. Benign solitary cecal ulcer. Indian J Gastroenterol. (2014) 33:495. doi: 10.1007/s12664-013-0399-x
12. Ona FV, Allende HD, Vivenzio R, Zaky DA, Nadaraja N. Diagnosis and management of nonspecific colon ulcer. Arch Surg. (1982) 117:888–94. doi: 10.1001/archsurg.1982.01380310014004
13. Smithwick W III, Anderson RP, Ballinger WF II. Nonspecific ulcer of the colon. Arch Surg. (1968) 97:133–8. doi: 10.1001/archsurg.1968.01340010163022
14. Jenkins AP, Trew DR, Crump BJ, Nukajam WS, Foley JA, Menzies IS, et al. Do non-steroidal anti-inflammatory drugs increase colonic permeability? Gut. (1991) 32:66–9. doi: 10.1136/gut.32.1.66
Keywords: cecal ulcer, colonic neoplasms, inflammatory bowel disease, colorectal diseases, abdominal pain
Citation: Li CQ, He A-Q and Liu G (2022) Solitary Cecal Ulcer: A Case Report. Front. Surg. 9:819519. doi: 10.3389/fsurg.2022.819519
Received: 21 November 2021; Accepted: 21 February 2022;
Published: 01 April 2022.
Edited by:
Vincenzo Neri, University of Foggia, ItalyCopyright © 2022 Li, He and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gang Liu, bGcxMDU5JiN4MDAwNDA7dG11LmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
 Chun Qiang Li†
Chun Qiang Li† Gang Liu
Gang Liu