- 1Department of Orthopaedics, Beijing Ditan Hospital, Capital Medical University, Beijing, China
- 2Department of Respiratory and Critical Care Medicine, The Affiliated Hospital of Qingdao University, Qingdao, China
- 3Department of Hematology, The Affiliated Hospital of Qingdao University, Qingdao, China
- 4Department of Spinal Surgery, The Affiliated Hospital of Qingdao University, Qingdao, China
Objective: This study aimed to explore the main risk factors affecting Total Knee Arthroplasty (TKA) patients and develop a predictive nomogram of hospital stay.
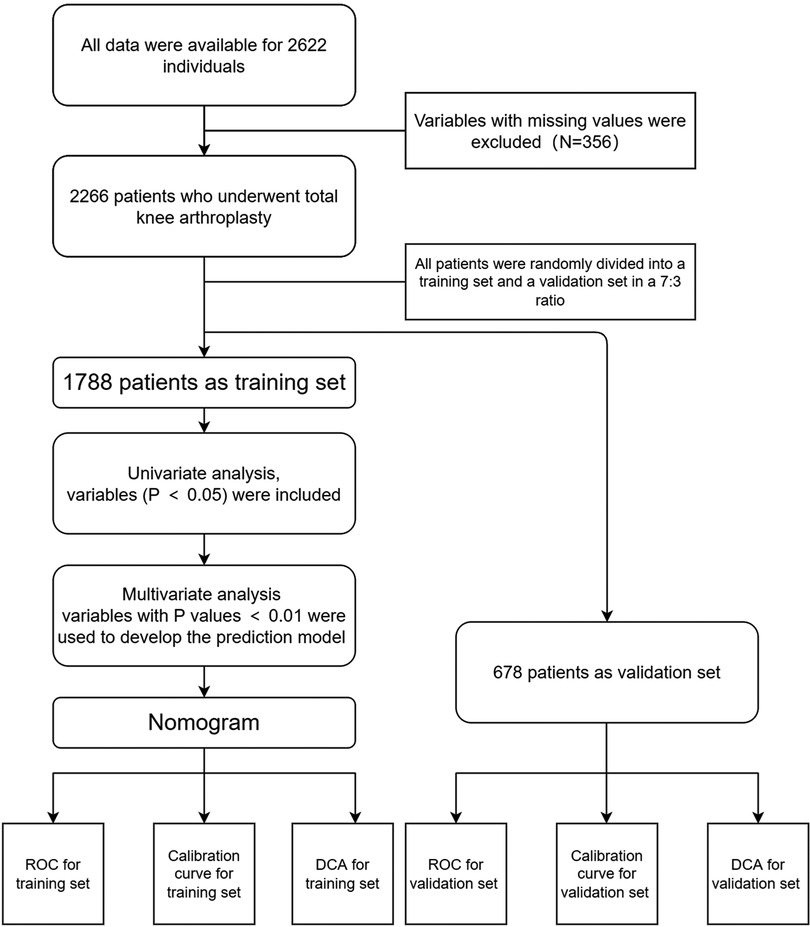
Methods: In total, 2,622 patients undergoing TKA in Singapore were included in this retrospective cohort study. Hospital extension was defined based on the 75% quartile (Q3) of hospital stay. We randomly divided all patients into two groups using a 7:3 ratio of training and validation groups. We performed univariate analyses of the training group, in which variables with P-values < 0.05 were included and then subjected to multivariate analysis. The multivariable logistic regression analysis was applied to build a predicting nomogram, using variable P-values < 0.01. To evaluate the prediction ability of the model, we calculated the C-index. The ROC, Calibration, and DCA curves were drawn to assess the model. Finally, we verified the accuracy of the model using the validation group and by also using the C-index. The ROC curve, Calibration curve, and DCA curve were then applied to evaluate the model in the validation group.
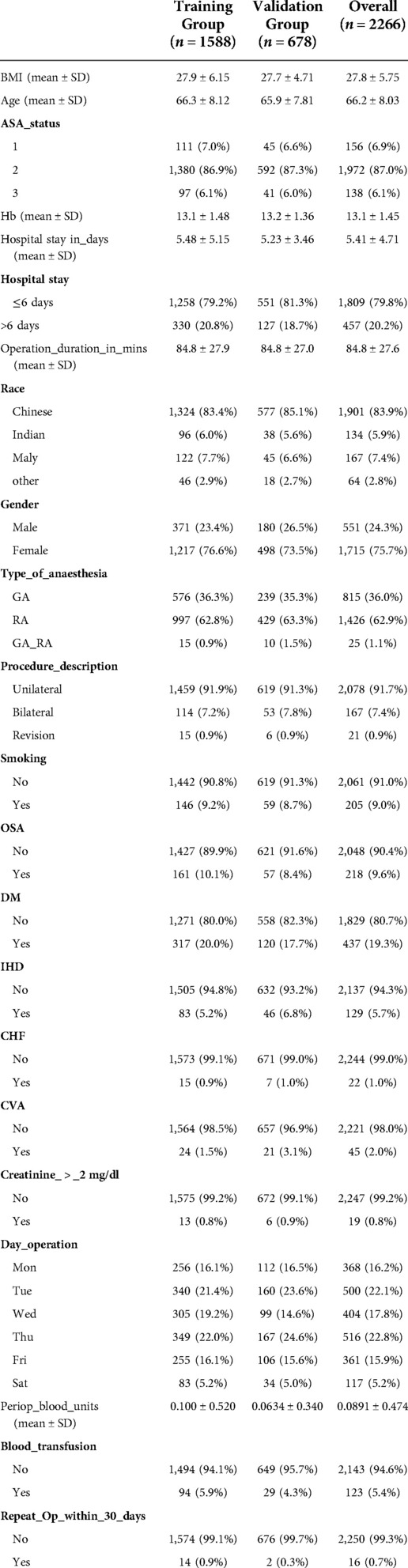
Results: The final study included 2,266 patients. The 75% quartile (Q3) of hospital stay was six days. In total, 457 (20.17%) patients had hospital extensions. There were 1,588 patients in the training group and 678 patients in the validation group. Age, Hb, D.M., Operation Duration, Procedure Description, Day of Operation, Repeat Operation, and Blood Transfusion were used to build the prediction model. The C-index was 0.680 (95% CI: 0.734–0.626) in the training group and 0.710 (95% CI: 0.742–0.678) for the validation set. The calibration curve and DCA indicated that the hospital stay extension model showed good performance in the training and validation groups.
Conclusion: To identify patients' risk factors early, medical teams need to plan a patient’s rehabilitation path as a whole. Its advantages lie in better resource allocation, maximizing medical resources, improving the functional recovery of patients, and reducing the overall cost of hospital stay and surgery, and will help clinicians in the future.
Introduction
Total Knee Arthroplasty (TKA) is the primary surgical procedure for treating severe knee disorders, relieving knee pain, and reestablishing knee function (1). It can help patients restore knee joint function and improve their quality of life (2). The increased life expectancy and aging of society have led to a dramatic increase in the number of patients with knee disorders. TKA is currently the most important and effective way to solve knee disorders, indicating that the demand for TKA will increase dramatically (3, 4). It is estimated that more than 700,000 TKA surgeries are performed in the United States annually and that this number will increase to nearly 3.5 million by 2030. It is therefore important that TKA is performed economically and effectively (5).
The costs of surgical procedures, inpatient care, and postoperative care have substantially increased due to enhanced intra- and peri-operative management (6). Meanwhile, there has been a noticeable decline in the global economy, and medical insurance expenditure has increased significantly. Some countries have removed TKA from the List of Medicare Outpatient Payment System Rules (7). The main focus of attempts to reduce hospitalization costs is to minimize hospital stays as shortening them will reduce medical expenses and society's medical burden (8).
TKA surgery may be accompanied by severe complications, which affect patients' prognosis and increase the possibility of disability and death (9). However, an extended hospital stay is a risk factor for postoperative complications. It is essential to reduce postoperative complications such as postoperative infection, thromboembolism, postoperative delirium, and cognitive dysfunction (10). The main factors of hospital stay, the incidence of surgical complications, hospitalization expenses, and medical resources are intractable issues that should be solved as soon as possible. This study aimed to explore the main risk factors and establish a predictive nomogram of Hospital Stay in undergoing Total Knee Arthroplasty (TKA).
Patients and methods
Patient and dates
Our secondary analysis was based on a single-center retrospective cohort study of patients who underwent TKA at Singapore General Hospital from January 2013 to June 2014 (11). We downloaded the raw data uploaded at the “DATADRYAD” website (www.datadryad.org). Abdullah et al. (11) shared the original data to the dryad database. We utilized these data for secondary analysis on a different hypothesis without violating the authors' rights.
The Beijing Ditan Hospital of Capital Medical University Ethics Committee approved our study. The Ethics Committee confirmed that informed consent was not required because the data are available publicly via the “DATADRYAD” Website (www.datadryad.org), and data were analyzed anonymously. The ethics committee waived the requirement for informed consent from all patients.
Methods
The study included 2,622 patients undergoing TKA in Singapore in a retrospective cohort study. We removed patients whose variables contained missing values, for example, BMI, D.M., D.M. on insulin, etc, which meant that 2,266 patients met the criteria and were included in the study. The prolonged hospital stay was defined as over the 75% quartile (Q3) of hospital stay (12–14). We randomly divided all patients into two groups in a 7:3 ratio: training and validation groups. We performed a univariate analysis in the training group, in which variables with P-values < 0.05 were included and then subjected to multivariate analysis. Multivariable logistic regression analysis was then applied to build a predicting nomogram using the variables the P-values were < 0.01. Furthermore, ROC, Calibration, and DCA curves were drawn to assess the model in the training and validation group.
Statistical analysis
R software (version 4.1.2) was used for all statistical analyses. (https://www.R-project.org). Using the R package “tableone”, Chi-squared tests (categorical variables) and one-way analysis of variance, or K–W test (continuous variables of a normal distribution or skewed distribution) we verified significant differences between different groups. Using the R package “caret”, we randomly divided all patients into two groups, using a 7:3 ratio for the training and validation groups. We first conducted univariate analysis, then multivariable regression under the package “rms”. P-value < 0.05 (bilateral) was considered statistically significant in the univariate analysis, and a P-value < 0.01 (bilateral) was considered statistically significant in the multivariable logistic regression. Predictors with a P-value < 0.01 were applied to develop the model that predicted the prolonged hospital stay.
The C-index (the concordance index) was used to evaluate the model's predictive ability. The C-index refers to the proportion of all patients whose predicted outcome is concordant with the actual result. Similarly, the ROC curve was used for the prediction accuracy of X to Y, enabling us to judge whether a specific factor has a diagnostic value for identifying a particular disease. The ROC curve reflects the relationship between sensitivity and specificity (package = “ROCR”). The DCA curve was performed by quantifying the net benefit at different threshold probabilities (package = “rmda”). Furthermore, the ROC curve, the calibration, and the decision curve analysis were used to evaluate the nomograms in the validation group.
Results
The demographic characteristics of patients who underwent TKA
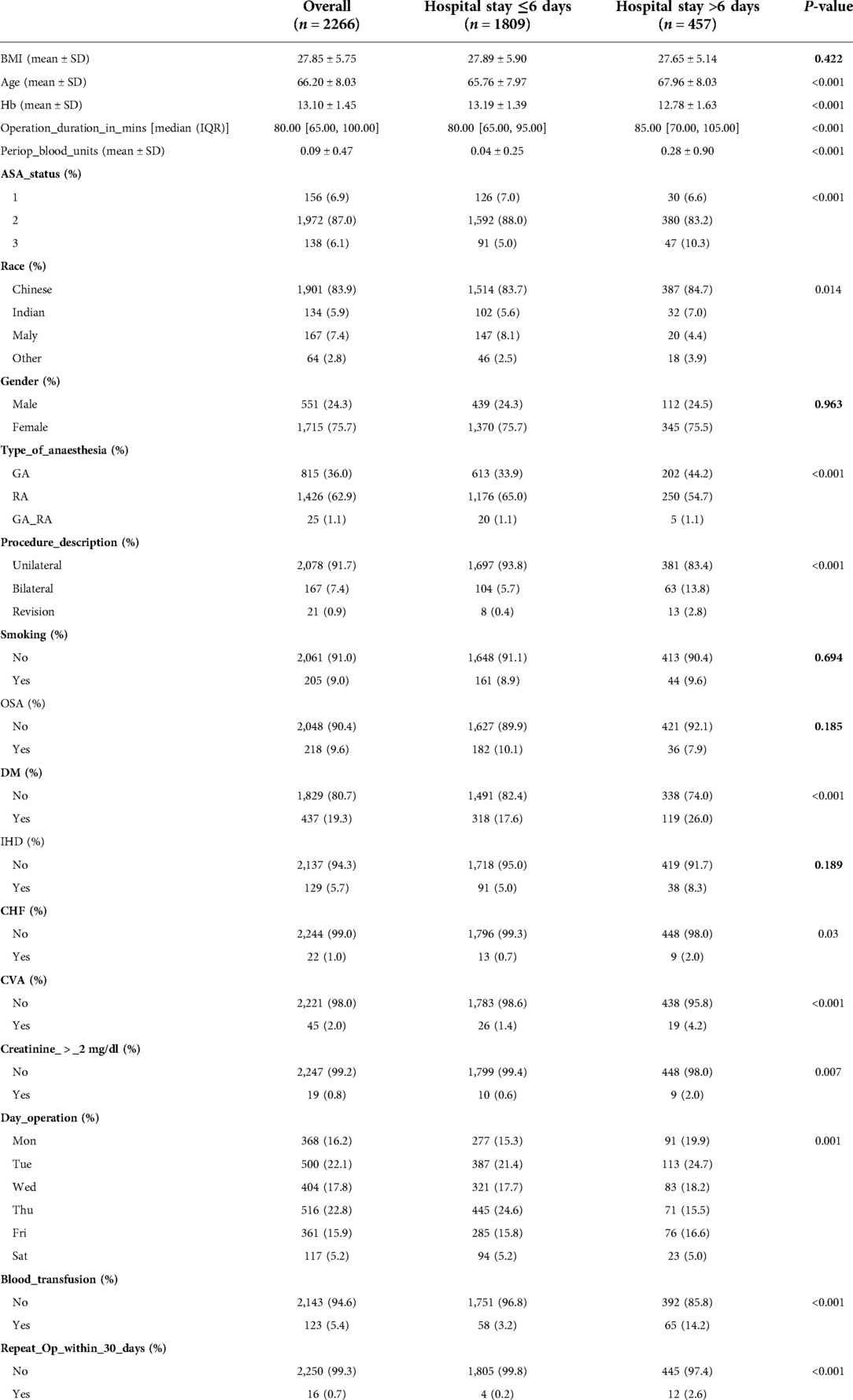
In total 2,266 of the patients who underwent TKA between January 2013 and June 2014 in the retrospective cohort were included, and 356 patients were excluded because the variable had a missing value (Figure 1). The two groups had no significant differences in BMI, Gender, Smoking habits, and OSA distribution. However, patients had a higher ASA score, longer operation time, higher ratio of bilateral TKA, higher incidence of anemia, higher risk of Blood Transfusion, repeated operation, and general anesthesia in the extended hospital stay group (Table 1). We randomized 1,788 patients into the training group and 678 patients into the validation group. The 75% quartiles (Q3) of hospital stays were six days, with 457 patients (20.17%) hospitalized for over six days (Tables 2, 3).
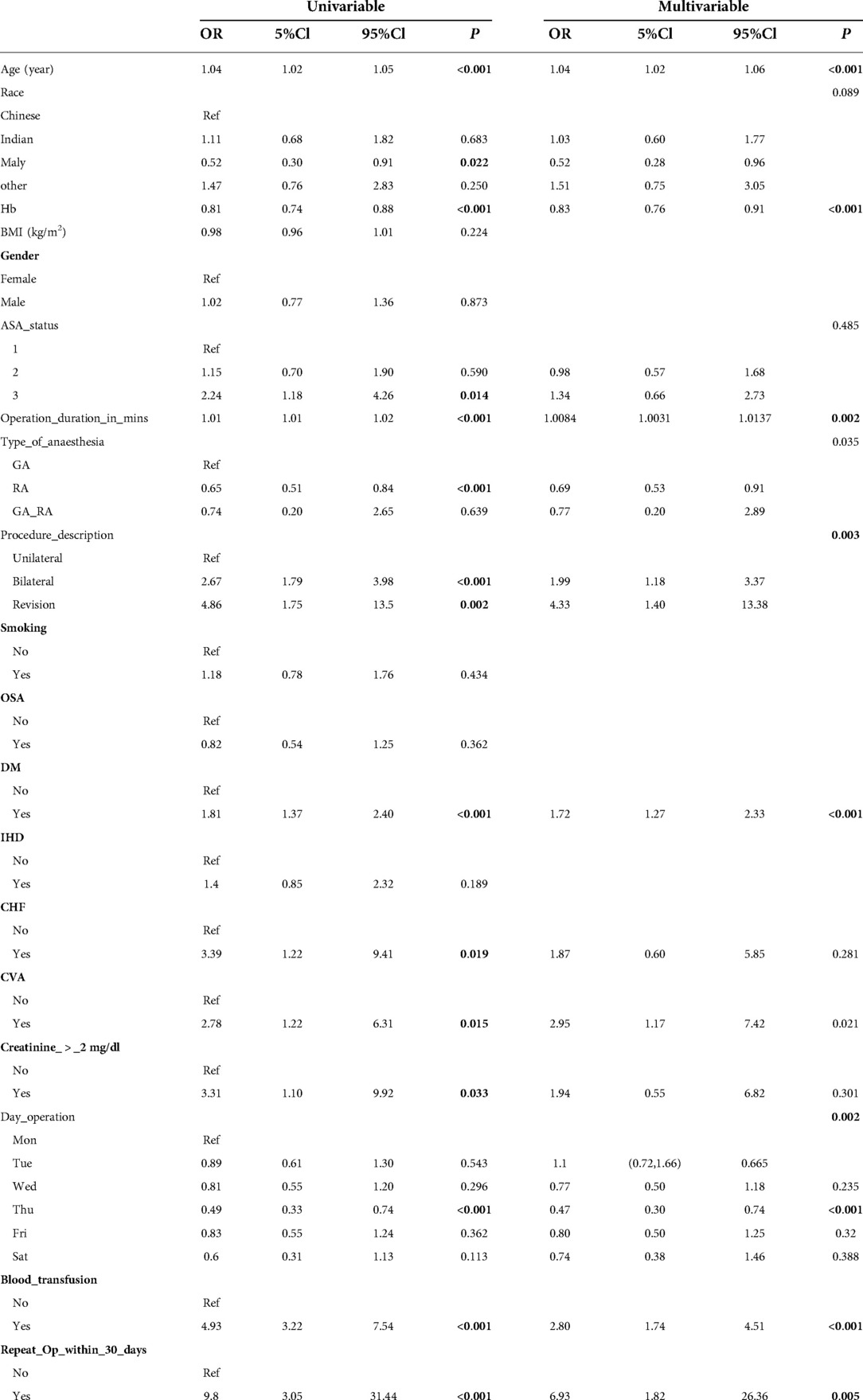
Table 3. Univariate and multivariate analysis of prolonged hospital stay in undergoing TKA patients.
The result of univariate and multivariate analysis for prolonged hospital stay patients
We used univariate logistic analysis to identify variables associated with a prolonged hospital stay in patients who underwent TKA, and 19 predictive factors were analyzed. The results showed that 14 predictive factors were associated with a prolonged hospital stay in patients who underwent TKA. Our study showed that Age, Hb, ASA Status, Operation Duration, Race, Type of Anaesthesia, Procedure Description, D.M., CHF, CVA, Creatinine, Day operation, Blood transfusion, and reoperation were the predictor risk factors for prolonged hospital stay in patients who underwent TKA (Table 2).
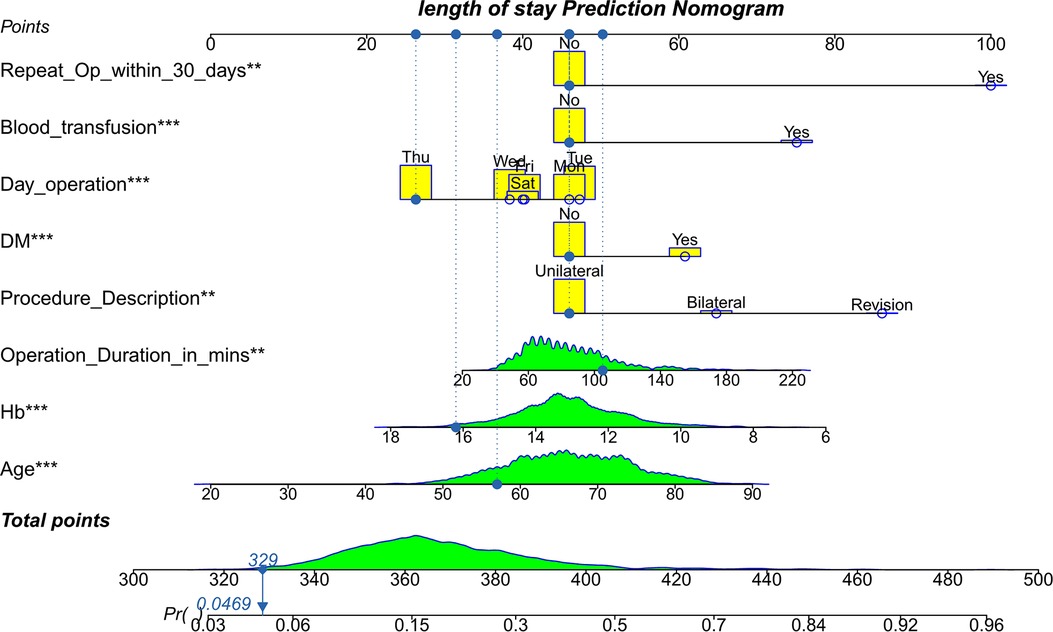
The multivariate logistics regression model was also performed to screen for independent risk factors. The results showed that Age (P ≤ 0.001), Hb (P ≤ 0.001), Operation Duration in mins (P ≤ 0.001), Procedure Description (P ≤ 0.001), D.M. (P ≤ 0.001), Day operation (P ≤ 0.001), Blood transfusion (P ≤ 0.001), Repeat Op within 30 days (P ≤ 0.001) were independent prognostic factors of prolonged hospital stay (Table 2).
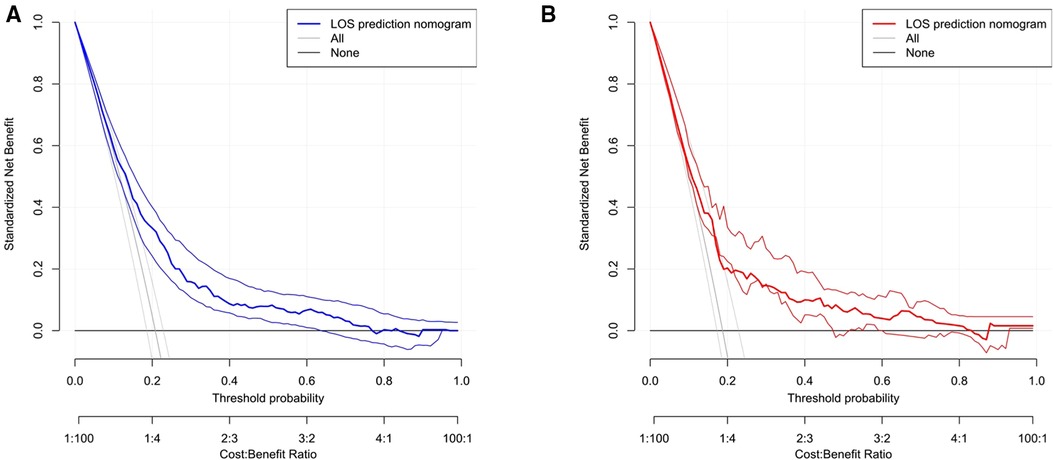
Development of the prediction model and evaluation of the accuracy of the nomogram in the training group
Based on eight independent risk factors, we established a nomogram for prolonged hospital stay in TKA patients (Figure 2). Meanwhile, the area under the ROC curve was 0.710 in the training group (Figure 3A). This indicated that the prediction model established based on the results of multivariate logistics regression analysis had a high predictive value. In addition, we also plotted the calibration curve and DCA for the nomogram in the training sets. The results showed that the nomogram could be a good tool for predicting prolonged hospital stay in TKA patients (Figures 4A, 5A).
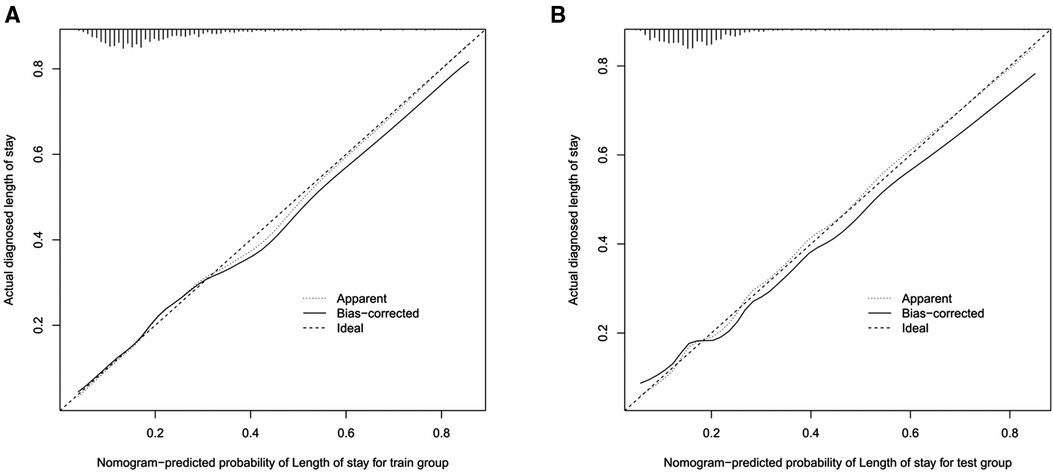
Figure 4. The Calibration curves of prolonged hospital stay in the training set (A) and validation set (B).
Evaluating the accuracy of the nomogram in the validation group
The ROC curve shows that the rosette has high predictive performance, and its AUC is 0.680 (Figure 3B). It indicates that the prediction model has a strong prediction ability. The calibration curves used to predict the prolonged hospital stay in the validation cohort showed good consistency and prediction ability (Figure 4B). The DCA of prolonged hospital stay indicated that this nomogram could be an excellent diagnostic tool for patients undergoing TKA (Figure 5B).
Discussion
Our study aimed to develop and validate a prolonged hospital stay risk prediction model for TKA patients. The risk factors were Age, Hb, Operation Duration, Procedure Description, D.M., Day operation, Blood transfusion, and Repeat Operation within 30 days. We built the nomogram using the above risk factors for prolonged hospital stay in TKA patients. The nomogram transforms the complex regression equation into a visual graph, making the prediction model's results more readable and convenient for clinicians. Because of the intuitive and easy-to-understand characteristics of the nomogram, it has gradually received more attention and has been applied in medical research and clinical practice.
Our study found that age was an independent risk factor for prolonged hospitalization after TKA. This might be because elderly patients are at high risk and prone to many diseases. Factors such as poor autoimmune ability, health status, and other reasons, coupled with the increased risk of infection due to blood loss during surgery, contribute to increasing their hospital stay. Davide Tornese et al. (15) found that the average LOS was 5.08 ± 2.52 days in the Department of Orthopedic Surgery, and the age was predictive of a more extended stay. In Corentin Roger et al. (16) study, the predictors of LOS were identified using a survival model that considered age as a continuous variable, individual comorbidities, and the discharge destination.
This study shows that preoperative hemoglobin is related to hospital stay. The hospitalization time decreased with the increase in hemoglobin value (17). We suggest that anemia be corrected before the operation to shorten hospital stays. Raut et al. (18) found a negative correlation between the level of Hb and LOS before and on the first day after the operation. However, there was still no correlation between the level of Hb decline and LOS, emphasizing the importance of improving the level of Hb before the operation.
Similarly, the longer the operative time, the higher the risk of prolonged patient hospitalization. Cregar (19) and Garbarino (20) indicated that less time spent in the operating theatre could lead to shorter LOS for revision and primary TKA patients. Lu (21) found that Total knee arthroplasty (TKA) frequently results in significant blood loss with accompanying hemoglobin loss and potentially increased transfusion rates. Unfortunately, transfusions have associated risks, including postoperative confusion, infection, cardiac arrhythmias, fluid overload, prolonged hospital stay, and increased mortality.
The highest risk score in the independent predictor was blood transfusion, many studies have come to the same conclusion, and the transfusion rate was directly related to the hospital stay (22–24). Autologous blood transfusion is often required when the blood loss is between 1000 and 1500 ml. Research shows that the total blood loss after TKA may be as high as 2000 ml, and the proportion of blood transfusion may be as high as 67% (25, 26). In a cohort of 228,316 TKA patients at 922 hospitals, the mean predicted probability of TKA transfusion was 7.9%, with 60% (95% CI, 36%–87%) of patients having hospital stays of more than three days (22). In a cross-sectional study of 4,544,999 patients who received TKA between January 2000 and December 2009, blood transfusions were associated with in-hospital mortality, and hospital stay increased by 0.71 ± 0.01 days (23). In addition, Danninger et al. (24) showed a significantly higher rate of significant complications in patients receiving transfusion (19.1% vs. 11.2%, P < 0.0001), and the mean length of hospital stay was significantly increased.
Our study found that the operation date was a significant factor in predicting the risk of hospital stays after blood transfusion. Similarly, studies demonstrated that operation procedures or factors related to doctors and nurses provide clinically relevant improvements in explaining hospital stay and patient-related risk factors (7). In a prospective cohort study of 4,509 patients who underwent initial TKA at four hospitals between January 1, 2016, and September 30, 2017, who received surgery later in the day were predicted to have a more extended hospital stay, with patients who had surgery on Friday having a significantly longer hospital stay than patients who had surgery on Monday (7). Our study showed that the risk prediction scores of operations on Monday, Tuesday, and Friday were much higher than those on Thursday. The length of hospital stay was related to operation data. Possible reasons for this result include patients coming from different countries, surgical hospital systems, and doctors' moods and preferences.
Diabetes is a chronic disease that can lead to multiple systemic comorbidities. This study found that the higher the comorbidity index, the longer the hospital stays were. Swain et al. (27) showed that 67% of patients with osteoarthritis had at least one other chronic condition, 20% more than those without osteoarthritis. The DM was the independent predictor of prolonged hospital stay. Similarly, other previous studies have suggested that TKA patients with comorbidities had prolonged hospital stays (28–31). Higuera et al. (30) showed that chronic heart failure was associated with extended hospital stays and increased rates of major postoperative complications in TKA patients. In a study of 15,321 TKA patients, 18.2% had a medical comorbidity D.M., with a 300% increase in overall mortality. Belmont et al. (31) found that DM was an independent predictor of hospitalization for four days or more.
Our study found that unilateral TKA under epidural anesthesia is economical, efficient, and has an ideal surgical effect for patients with osteoarthritis. For patients with bilateral knee arthritis, a comprehensive health assessment should be conducted before surgery. For high-risk patients, especially those with severe cardiovascular diseases, simultaneous bilateral total knee replacement should be avoided as far as possible (32–35). The reasons for reoperation TKA were that the patients had cardiac complications, pulmonary complications, and renal and cerebrovascular complications before the operation. The local complications of patients after operation include non-infection-related complications, wound infection, and peripheral nerve injury. Furthermore, we also found that the causes of revision surgery were periprosthetic infection, aseptic loosening, osteolysis, abrasion, joint dislocation, periprosthetic fracture, and patellar-related complications. These factors will lead to prolonged hospitalization (16, 36–38).
There are still some limitations to our study. First, this study is retrospective, using clinical data from a single center. Therefore, there may be differences in treatment strategies and race, etc. Second, because of differences in healthcare settings and practices, the predictive models developed in one country are unlikely to be directly applicable in another, requiring external validation and an updating of the predictive performance of models in other new patients. Finally, some influencing factors may not be included in this paper, including patient income, medical expenses, medical insurance, hospital location, etc. Potential factors not included may also have some influence on the results.
Conclusion
To make better use of these factors and identify patients' risk factors early, the medical team should plan a patient's rehabilitation path as a whole. Advantages of this approach include better resource allocation, maximizing medical resources, improving the functional recovery of patients, and reducing the overall cost of hospital stay and surgery. We also hope that these results will help clinicians in the future.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://datadryad.org/stash/dataset/doi:10.5061/dryad.73250.
Ethics statement
This study was approved by the Ethics Committee of Beijing Ditan Hospital, Capital Medical University. The Ethics Committee approved that informed consent was not required because the DRYAD was supported and data were analyzed anonymously. The ethics committee waived the requirement for informed consent from all patients.
Author contributions
BL performed the data analysis. BL, CXZ wrote the manuscript. BL, CXZ, and YJM. contributed to the manuscript revision. YJM contributed to the literature search and data extraction. BL, ZJW, and QZ Conceived and designed the study. All authors have read and approved the final version of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
l claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
TKA, total knee arthroplasty; ROC, receiver operating characteristic; OR, odds ratio; AUC, area under the curve; CI, confidence interval; DM, diabetes Mellitus; IHD, ischemic heart disease; CHF, congestive hearts failure; SE, standard error.
References
1. Ji X, Ke W. Two types of anaesthesia and length of hospital stay in patients undergoing unilateral total knee arthroplasty (TKA): a secondary analysis based on a single-centre retrospective cohort study in Singapore. BMC Anesthesiol. (2021) 21(1):242. doi: 10.1186/s12871-021-01459-7
2. Ethgen O, Bruyère O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. (2004) 86(5):963–74. doi: 10.2106/00004623-200405000-00012
3. Kim SH. Morbid obesity and excessive hospital resource consumption for unilateral primary hip and knee arthroplasty. J Arthroplasty. (2010) 25(8):1258–66. doi: 10.1016/j.arth.2009.09.005
4. Losina E, Thornhill TS, Rome BN, Wright J, Katz JN. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am. (2012) 94(3):201–7. doi: 10.2106/jbjs.J.01958
5. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. (2007) 89(4):780–5. doi: 10.2106/jbjs.F.00222
6. Belatti DA, Pugely AJ, Phisitkul P, Amendola A, Callaghan JJ. Total joint arthroplasty: trends in medicare reimbursement and implant prices. J Arthroplasty. (2014) 29(8):1539–44. doi: 10.1016/j.arth.2014.03.015
7. Cleveland Clinic Orthopaedic Arthroplasty G. The main predictors of length of stay after total knee arthroplasty: patient-related or procedure-related risk factors. J Bone Joint Surg Am. (2019) 101(12):1093–101. doi: 10.2106/JBJS.18.00758
8. Molloy IB, Martin BI, Moschetti WE, Jevsevar DS. Effects of the length of stay on the cost of total knee and total hip arthroplasty from 2002 to 2013. J Bone Joint Surg Am. (2017) 99(5):402–7. doi: 10.2106/JBJS.16.00019
9. Parvizi J, Mui A, Purtill JJ, Sharkey PF, Hozack WJ, Rothman RH. Total joint arthroplasty: when do fatal or near-fatal complications occur? J Bone Joint Surg Am. (2007) 89(1):27–32. doi: 10.2106/jbjs.E.01443
10. Kehlet H. Fast-track hip and knee arthroplasty. Lancet. 2013;381(9878):1600–2. doi: 10.1016/s0140-6736(13)61003-x
11. Abdullah HR, Sim YE, Hao Y, Lin GY, Liew GHC, Lamoureux EL, et al. Association between preoperative anaemia with length of hospital stay among patients undergoing primary total knee arthroplasty in Singapore: a single-centre retrospective study. BMJ Open. (2017) 7(6):e016403. doi: 10.1136/bmjopen-2017-016403
12. Klemt C, Tirumala V, Barghi A, Cohen-Levy WB, Robinson MG, Kwon YM. Artificial intelligence algorithms accurately predict prolonged length of stay following revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. (2022) 30(8):2556–64. doi: 10.1007/s00167-022-06894-8
13. Ong PH, Pua YH. A prediction model for length of stay after total and unicompartmental knee replacement. Bone Joint J. (2013) 95-b(11):1490–6. doi: 10.1302/0301-620x.95b11.31193
14. Papalia R, Torre G, Alifano AM, Albo E, Papalia GF, Bravi M, et al. Length of hospital stay after total knee arthroplasty: a correlation study on 1200 patients. J Clin Med. (2022) 11(8). doi: 10.3390/jcm11082114
15. Tornese D, Robustelli A, Ricci G, Rancoita PMV, Maffulli N, Peretti GM. Predictors of postoperative hospital length of stay after total knee arthroplasty. Singapore Med J. (2021). doi: 10.11622/smedj.2021142
16. Roger C, Debuyzer E, Dehl M, Bulaïd Y, Lamrani A, Havet E, et al. Factors associated with hospital stay length, discharge destination, and 30-day readmission rate after primary hip or knee arthroplasty: retrospective cohort study. Orthop Traumatol Surg Res. (2019) 105(5):949–55. doi: 10.1016/j.otsr.2019.04.012
17. Zhang S, Huang Q, Xie J, Xu B, Cao G, Pei F. Factors influencing postoperative length of stay in an enhanced recovery after surgery program for primary total knee arthroplasty. J Orthop Surg Res. (2018) 13(1):29. doi: 10.1186/s13018-018-0729-x
18. Raut S, Mertes SC, Muniz-Terrera G, Khanduja V. Factors associated with prolonged length of stay following a total knee replacement in patients aged over 75. Int Orthop. (2012) 36(8):1601–8. doi: 10.1007/s00264-012-1538-1
19. Cregar WM, Goodloe JB, Lu Y, Gerlinger TL. Increased operative time impacts rates of short-term complications after unicompartmental knee arthroplasty. J Arthroplasty. (2021) 36(2):488–94. doi: 10.1016/j.arth.2020.08.032
20. Garbarino LJ, Gold PA, Sodhi N, Anis HK, Ehiorobo JO, Boraiah S, et al. The effect of operative time on in-hospital length of stay in revision total knee arthroplasty. Ann Transl Med. (2019) 7(4):66. doi: 10.21037/atm.2019.01.54
21. Lu Q, Peng H, Zhou GJ, Yin D. Perioperative blood management strategies for total knee arthroplasty. Orthop Surg. (2018) 10(1):8–16. doi: 10.1111/os.12361
22. Menendez ME, Lu N, Huybrechts KF, Ring D, Barnes CL, Ladha K, et al. Variation in use of blood transfusion in primary total hip and knee arthroplasties. J Arthroplasty. (2016) 31(12):2757–2763.e2. doi: 10.1016/j.arth.2016.05.022
23. Klika AK, Small TJ, Saleh A, Szubski CR, Chandran Pillai ALP, Barsoum WK. Primary total knee arthroplasty allogenic transfusion trends, length of stay, and complications: nationwide inpatient sample 2000–2009. J Arthroplasty. (2014) 29(11):2070–7. doi: 10.1016/j.arth.2014.06.018
24. Danninger T, Rasul R, Poeran J, Stundner O, Mazumdar M, Fleischut PM, et al. Blood transfusions in total hip and knee arthroplasty: an analysis of outcomes. ScientificWorldJournal. (2014) 2014:623460. doi: 10.1155/2014/623460
25. Rosencher N, Kerkkamp HE, Macheras G, Munuera LM, Menichella G, Barton DM, et al. Orthopedic surgery transfusion hemoglobin European overview (OSTHEO) study: blood management in elective knee and hip arthroplasty in Europe. Transfusion. (2003) 43(4):459–69. doi: 10.1046/j.1537-2995.2003.00348.x
26. Bong MR, Patel V, Chang E, Issack PS, Hebert R, Di Cesare PE. Risks associated with blood transfusion after total knee arthroplasty. J Arthroplasty. (2004) 19(3):281–7. doi: 10.1016/j.arth.2003.10.013
27. Swain S, Sarmanova A, Coupland C, Doherty M, Zhang W. Comorbidities in osteoarthritis: a systematic review and meta-analysis of observational studies. Arthritis Care Res. (2020) 72(7):991–1000. doi: 10.1002/acr.24008
28. Jans Ø, Jørgensen C, Kehlet H, Johansson PI. Role of preoperative anemia for risk of transfusion and postoperative morbidity in fast-track hip and knee arthroplasty. Transfusion. (2014) 54(3):717–26. doi: 10.1111/trf.12332
29. Mathijssen NM, Verburg H, van Leeuwen CC, Molenaar TL, Hannink G. Factors influencing length of hospital stay after primary total knee arthroplasty in a fast-track setting. Knee Surg Sports Traumatol Arthrosc. (2016) 24(8):2692–6. doi: 10.1007/s00167-015-3932-x
30. Higuera CA, Elsharkawy K, Klika AK, Brocone M, Barsoum WK. 2010 Mid-America orthopaedic association physician in training award: predictors of early adverse outcomes after knee and hip arthroplasty in geriatric patients. Clin Orthop Relat Res. (2011) 469(5):1391–400. doi: 10.1007/s11999-011-1804-3
31. Belmont PJ J, Goodman GP, Waterman BR, Bader JO, Schoenfeld AJ. Thirty-day postoperative complications and mortality following total knee arthroplasty: incidence and risk factors among a national sample of 15,321 patients. J Bone Joint Surg Am. (2014) 96(1):20–6. doi: 10.2106/JBJS.M.00018
32. Shah K, Smith J, Jones B, Hullin M. Bilateral total knee replacement under a single anaesthetic, using a cementless implant is not unsafe. Knee Surg Sports Traumatol Arthrosc. (2007) 15(3):269–75. doi: 10.1007/s00167-006-0196-5
33. Alghadir AH, Iqbal ZA, Anwer S, Anwar D. Comparison of simultaneous bilateral versus unilateral total knee replacement on pain levels and functional recovery. BMC Musculoskelet Disord. (2020) 21(1):246. doi: 10.1186/s12891-020-03269-3
34. Oakes DA, Hanssen AD. Bilateral total knee replacement using the same anesthetic is not justified by assessment of the risks. Clin Orthop Relat Res. (2004) 428:87–91. doi: 10.1097/01.blo.0000147133.75432.86
35. Warren JA, Siddiqi A, Krebs VE, Molloy R, Higuera CA, Piuzzi NS. Bilateral simultaneous total knee arthroplasty may not be safe even in the healthiest patients. J Bone Joint Surg Am. (2021) 103(4):303–11. doi: 10.2106/jbjs.20.01046
36. Jensen CB, Petersen PB, Jørgensen CC, Kehlet H, Troelsen A, Gromov K. Length of stay and 90-day readmission/complication rates in unicompartmental versus total knee arthroplasty: a propensity-score-matched study of 10,494 procedures performed in a fast-track setup. J Bone Joint Surg Am. (2021) 103(12):1063–71. doi: 10.2106/jbjs.20.01287
37. Wilson HA, Middleton R, Abram SGF, Smith S, Alvand A, Jackson WF, et al. Patient relevant outcomes of unicompartmental versus total knee replacement: systematic review and meta-analysis. BMJ. (2019) 364:l352. doi: 10.1136/bmj.l352
Keywords: total knee arthroplasty, hospital stay, the risk factor, nomogram, predictive model, a cohort study
Citation: Liu B, Ma Y, Zhou C, Wang Z and Zhang Q (2023) A novel predictive model of hospital stay for Total Knee Arthroplasty patients. Front. Surg. 9:807467. doi: 10.3389/fsurg.2022.807467
Received: 2 November 2021; Accepted: 14 October 2022;
Published: 6 January 2023.
Edited by:
Sujit Kumar Tripathy, All India Institute of Medical Sciences Bhubaneswar, IndiaReviewed by:
Richard Amdur, George Washington University, United StatesBjörn Rath, Klinikum Wels-Grieskirchen, Austria
© 2023 Liu, Ma, Zhou, Wang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhijie Wang c2ltb253YW5nMTk2OUAxNjMuY29t Qiang Zhang emhhbmdkdHpxQHNpbmEuY29t
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Bo Liu
Bo Liu Yijiang Ma2
Yijiang Ma2