- 1Department of vascular surgery, West China Hospital, Sichuan University, Chengdu, China
- 2Department of ambulatory center, West China Hospital, Sichuan University, Chengdu, China
Objectives: The effects of body mass index (BMI) on the outcome of high ligation and stripping (HLS) in an ambulatory center remain unclear. This study aims to investigate the outcomes of HLS in an ambulatory center based on BMI in the Chinese population.
Design: This was a prospective cohort study with mid-term follow-up.
Materials and Methods: 170 eligible patients were included in the study and the data of Clinical, Etiology, Anatomy, and Pathophysiology (CEAP) classification, Venous Clinical Severity Score (VCSS), Visual Analogue Score (VAS), Aberdeen Varicose Veins Questionnaire (AVVQ), Quality of Recovery (QoR-15), and postoperative complications at predetermined time points were collected.
Results: A total of 170 patients (236 limbs) with a mean age of 53.87 ± 9.96 years (range, 24–80 years) and a mean BMI of 23.86 ± 2.96 kg/m2 were included. Of the group, 50.6% were women, and 66 patients received bilateral procedures. Through curve fitting, a BMI less than 28 and a BMI of 28 or higher were found to have a negative [−0.1 (−0.3, 0.1) 0.296] and positive [0.7 (0.2, 1.2) 0.006] relationship trend, respectively, with the improvement of VCSS at 6 weeks after surgery. Through smooth curve fitting, BMI was shown to have a negative relationship trend on the improvement of VCSS at 6 months after surgery. After multivariable risk adjustment for potential confounding factors, BMI was not found to be associated with the improvement of VCSS and AVVQ at 6 weeks after surgery, as well as the improvement of AVVQ at 6 months after surgery (all p-values >0.05). Six months after surgery, BMI was shown to have a negative relationship trend on the improvement of VCSS, and obese patients showed lower VCSS improvement than patients of normal BMI [−1.3 (−1.9, −0.7) <0.0001]. Six weeks after surgery, postoperative complications such as paresthesia were found to be significantly higher in the obese group than in the non-obese group (p < 0.05). At 6 months after surgery, the obese group showed significantly higher complications of the legs compared with the normal BMI group (p < 0.05).
Conclusions: Our results showed that obesity is a risk factor for prognosis and postoperative complications following ambulatory HLS.
Introduction
Varicose vein disease is a common condition presenting to physicians globally, and approximately 25 to 40% of the world’s population is affected by it (1–4). The Society for Vascular Surgery/American Venous Forum evidence-based guidelines recommend endovenous laser ablation (EVLA)/radiofrequency ablation (RFA) as the primary treatment (1 B) (5). However, due to factors such as its cost, partial coverage by medical insurance, ineffectiveness for severely distorted veins, and the need for expensive equipment, EVLA/RFA has not been widely used, especially in developing countries. High ligation and stripping (HLS), on the other hand, is a classic treatment that has numerous advantages and is widely used, especially in developing countries (6). Numerous studies have reported that HLS performed in ambulatory centers is just as safe and feasible as HLS performed in hospitals (7–9). In particular, HLS performed in ambulatory centers has several advantages, including lower costs, quicker recovery, improved patient satisfaction and comfort, and much shorter hospitalization time (10–12).
Some studies have reported that overweight patients undergoing HLS have a higher rate of lymphatic complications and wound infections (13–14), and should be monitored closely in the perioperative period. Another study also demonstrated that moderate and severe obesity were associated with an increased incidence of postoperative complications and unplanned admissions in major ambulatory centers (13–15). Despite some evidence suggesting that increased weight can promote the incidence of lower limb varicose veins, there are few studies focusing on the effects of weight on patients after HLS in ambulatory centers. According to the World Health Organization criteria (16), a body mass index (BMI) of 25.0 kg/m2 or higher is defined as overweight; however, this cut-off point may not be appropriate for Asian populations. According to the Chinese national standard (17), a BMI of 24.0 kg/m2 or higher is defined as overweight and a BMI of 28.0 kg/m2 or higher is defined as obesity. Thus, the study aimed to prospectively investigate the early and mid-term outcomes based on the BMI in a Chinese tertiary-care institution, and determine the correlation between BMI and the prognosis of HLS performed in an ambulatory center. Our hypothesis was that overweight and obese patients had worse clinical outcomes after HLS in an ambulatory center.
Materials and Methods
A prospective cohort study was performed with 170 eligible patients who underwent their first HLS for varicose veins in an ambulatory center from November 2016 to October 2017 in our hospital. Our research protocol was approved by the West China Hospital Ethics Committee and was in accord with the ethical guidelines of the Declaration of Helsinki.
We included patients with C2-4 classes of venous disease (advanced CEAP classification), who were less than 85 years of age, diagnosed with varicose veins by ultrasound, and willing to sign an informed consent. Patients are routinely examined in the standing position and reverse flow of greater than 0.5 m/s following a compression of the calf or valsalva manoeuvre is considered pathological reflux. Patients with any of the following criteria were excluded from this study: 1. Great saphenous varicose vein recurrence; 2. secondary varicose veins (post-thrombotic syndrome); 3. small saphenous varicose veins; 4. acute deep vein thrombosis; 5. superficial phlebitis; 6. Incompetent perforating vein; 7. varicose veins from trauma; and 8. severe comorbidity.
We collected data on the Venous Clinical Severity Score (VCSS) (18), the Aberdeen Varicose Veins Questionnaire (AVVQ) (19), Visual Analogue Score (VAS) (20), Quality of Recovery-15 (QoR-15, QoR15 consists of part QOR15-part A and part QOR15-part B) (21), and the Clinical, Etiology, Anatomy, and Pathophysiology (CEAP) classification (22) before surgery and during postoperative follow-up. The improvement in VCSS and AVVQ were our primary endpoints. The incidence of systemic and leg-specific complications in both groups were our secondary endpoints and were recorded at 6 weeks and 6 months post-procedure. All outcomes were assessed by the same certified specialists in the study team. Our research protocol was approved by the local committee and was in accord with the ethical guidelines of the Declaration of Helsinki. All patients provided written informed consent. Meanwhile, our research was registered in the Chinese Clinical Trial Registry (ChiCTR-ORC-17011614).
Surgical Procedure
The standard HLS procedure was performed under general anesthesia (without tumescent anesthesia) by the same group of surgeons (chief physicians). The micro-incisions (2–3 cm) were made parallel to the dermatoglyphics with a proximal oblique incision in the groin and a distal transverse incision in the medial malleolus, when deemed necessary (i.e., when the great saphenous vein (GSV) was dilated with severe reflux all the way distally). The trunk and tributaries were systematically and thoroughly treated by ligation. A standard stripper was inserted in the GSV and the vein was stripped from the top down to just below the knee. Another small stripper was inserted in the distal transverse incision of the GSV in the medial malleolus and the vein was stripped from the bottom upward to near the knee, when deemed necessary (i.e., when the GSV was dilated with severe reflux all the way distally). When indicated, phlebectomy of the marked varicose branches and ligation of the grossly incompetent perforators were performed simultaneously. The groin and distal incisions were closed by an intradermal continuous suture (Monocryl@ 5/0, Ethicon, Johnson & Johnson, Neuchâtel, Switzerland). At the end of the surgical procedure, the leg was wrapped in sterile absorbent gauze and covered with a single-layer elastic bandage. After 48 h, the patient could remove the bandage and was allowed to walk as soon as possible. A Class II (30 mmHg) below-knee elastic stocking was used for 3 months during the daytime only. No thermal ablation or sclerotherapy was performed during the surgical procedure. Any additional procedures during the follow-up, such as surgery, thermal ablation, or sclerotherapy, were considered a failure, and these patients were not included in the study. We do not routinely use heparin after ambulatory HLS; only patients with a high risk of thrombosis (Caprini score ≥3) receive heparin (subcutaneous injection of low-molecular-weight heparin 4,000 IU/day) to prevent thrombosis (23). We routinely used early ambulation and compression therapy to prevent thrombosis.
Follow-up
All the patients were seen twice: at 6 weeks and 6 months after the procedure. Postoperative complications (systemic and leg-specific complications), CEAP class, VCSS score, AVVQ score, VAS score, and QOR-15 score were evaluated and recorded. Follow-up methods included outpatient visits, interviews by telephone and email, and online forums.
Statistical Analysis
We first described the demographics and general characteristics of the study participants. Then, univariate analysis and stratified analysis were performed to detect the risk variables associated with the BMI group and the improvement of VCSS, as well as AVVQ, at 6 weeks and 6 months after surgery. We further applied a two-piecewise linear regression model to examine the threshold effect of the BMI on the improvement of VCSS and AVVQ at 6 weeks and 6 months after surgery using a smoothing function. The threshold level (i.e., turning point) was determined using trial and error, including a point that gave the maximum model likelihood. We also conducted a log-likelihood ratio test comparing the one-line regression model with a two-piecewise linear model. The Pearson test was used for analysis of the correlation between BMI and the improvement of VCSS and AVVQ. Finally, multivariate regression analysis was performed between the BMI groups. All data were double entered and then exported to tab-delimited text files. The qualitative variables were presented as numbers and percentages, and the quantitative variables were expressed as mean and standard deviation (SD). A p-value of <0.05 was considered statistically significant. All the analyses were performed with R (http://www.R-project.org) and EmpowerStats software (www.empowerstats.cm, X&Y solutions, Boston, MA, USA).
Results
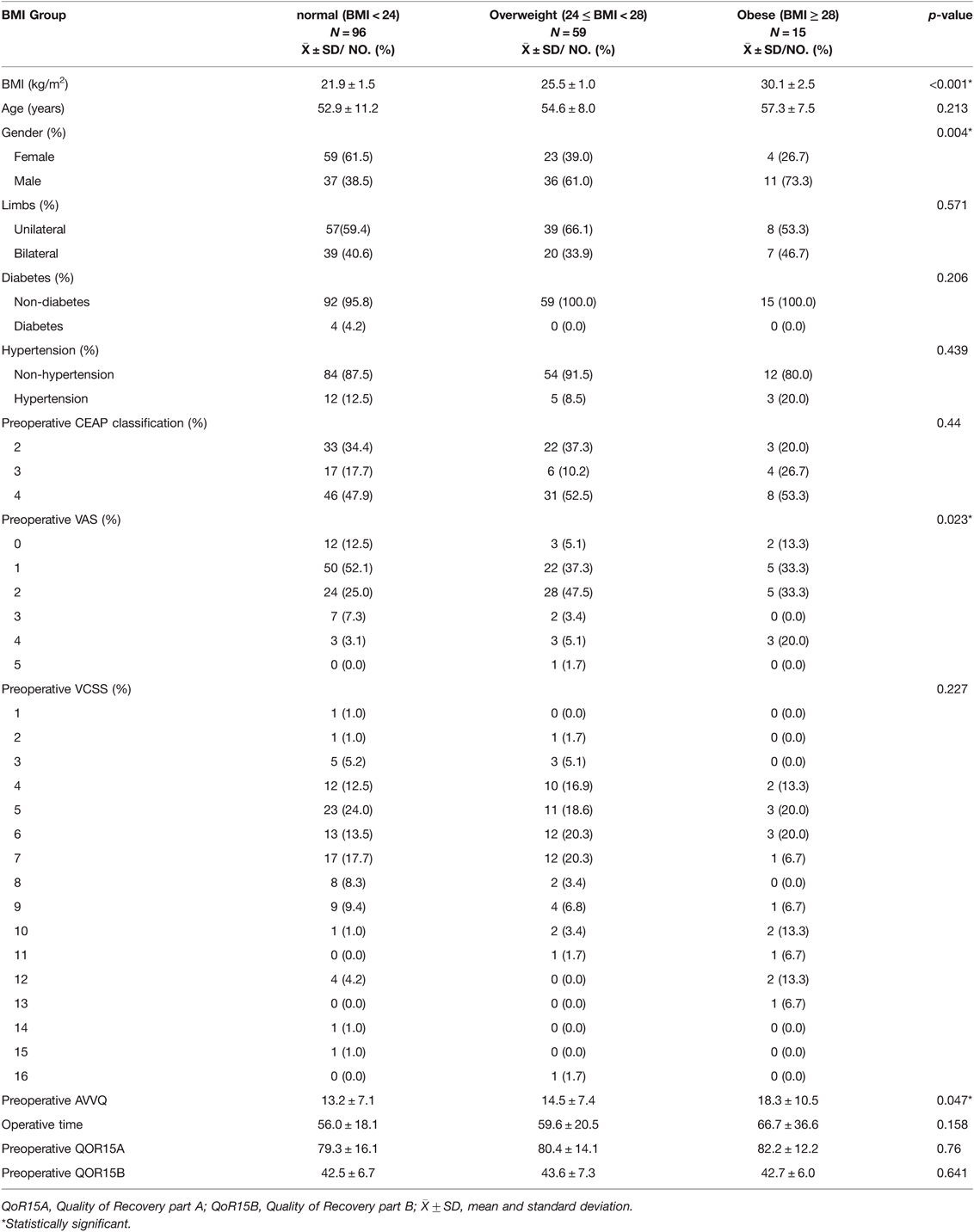
A total of 204 ambulatory HLS procedures were performed from January 2016 to December 2017 and 170 eligible patients were enrolled in this study. We excluded 21 patients for additional procedures (e.g., foam sclerotherapy/endovascular radiofrequency ablation) and 13 patients who were lost to follow-up. The mean age of the patients was 53.87 ± 9.96 years (range, 24–80 years), and the mean BMI was 23.86 ± 2.96 kg/m2. Of the patient group, 50.6% were women, and 66 patients received bilateral procedures. The proportion of men in the high BMI group was significantly higher than that of women (p = 0.004). The overweight group and obese group had higher VAS (p = 0.023) and AVVQ scores than the normal group (p = 0.047). Apart from these three factors, there were no significant differences in the basic characteristics of the BMI groups (Table 1).
We performed univariate analysis to detect the effects of BMI risk factors on the improvement of AVVQ and VCSS at 6 weeks and 6 months after surgery. The univariate regression analysis showed that the improvement of AVVQ at 6 weeks and 6 months after surgery was significantly correlated with bilateral HLS and CEAP classification 4 (all p < 0.05). Preoperative QoR15B had a negative relationship trend on the improvement of VCSS at 6 weeks and 6 months after surgery, especially in the group with high preoperative QoR15B scores (Table 2). A positive relationship trend was found between CEAP classification and the improvement of VCSS at 6 weeks and 6 months after surgery (Table 2). In the overweight group, we found that BMI had a positive relationship trend on the improvement of AVVQ at 6 months after surgery [4.8 (0.5, 9.0) 0.0298].

Table 2. Effects of risk factors of BMI on the improvement of AVVQ and VCSS at six weeks and six months after surgery by univariate analysis.
We further applied a two-piecewise linear regression model to examine the threshold effect of BMI on the improvement of VCSS at 6 weeks and 6 months after surgery using a smoothing function (Table 3 and Figure 1). Through curve fitting, a negative relationship trend was found between BMI less than 28 and the improvement of VCSS at 6 weeks after surgery [−0.1 (−0.3, 0.1) 0.296]. Conversely, a positive relationship trend was found between BMI of 28 or higher and the improvement of VCSS at 6 weeks [0.7 (0.2, 1.2) 0.006], (the P value of log-likelihood ratio (PLLR): p = 0.007, indicating a nonlinear relationship between BMI and the improvement of VCSS at 6 weeks after surgery) (Table 3). Through smooth curve fitting, BMI was shown to have a negative relationship trend on the improvement of VCSS at 6 months after surgery (Figure 1).

Figure 1. Smooth curve fitting for the relationship between BMI and the improvement of VCSS at 6 weeks and 6 months after surgery *. *: Adjust I adjust for: Gender; Years; Limbs; Preoperative CEAP; Preoperative AVVQ; Preoperative VAS; Preoperative QoR15-A; Preoperative QoR15-B.
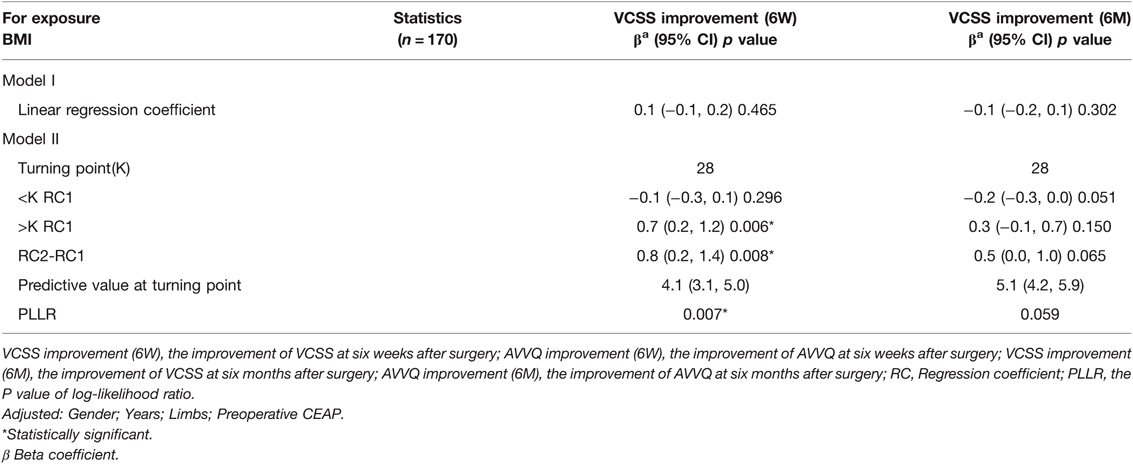
Table 3. Threshold analysis for the relationship between BMI and the improvement of VCSS and AVVQ at six weeks and six months after surgery.
After multivariable risk adjustment for potential confounding factors (Table 4), we found that the BMI was not associated with the improvement of VCSS and AVVQ at 6 weeks after surgery, as well as the improvement of AVVQ at 6 months after surgery (all p-values >0.05). At 6 months after surgery, we found that the BMI had a negative relationship trend on the improvement of VCSS, and obese patients showed a lower VCSS improvement than patients with normal BMI [−1.3 (−1.9, −0.7) <0.0001].
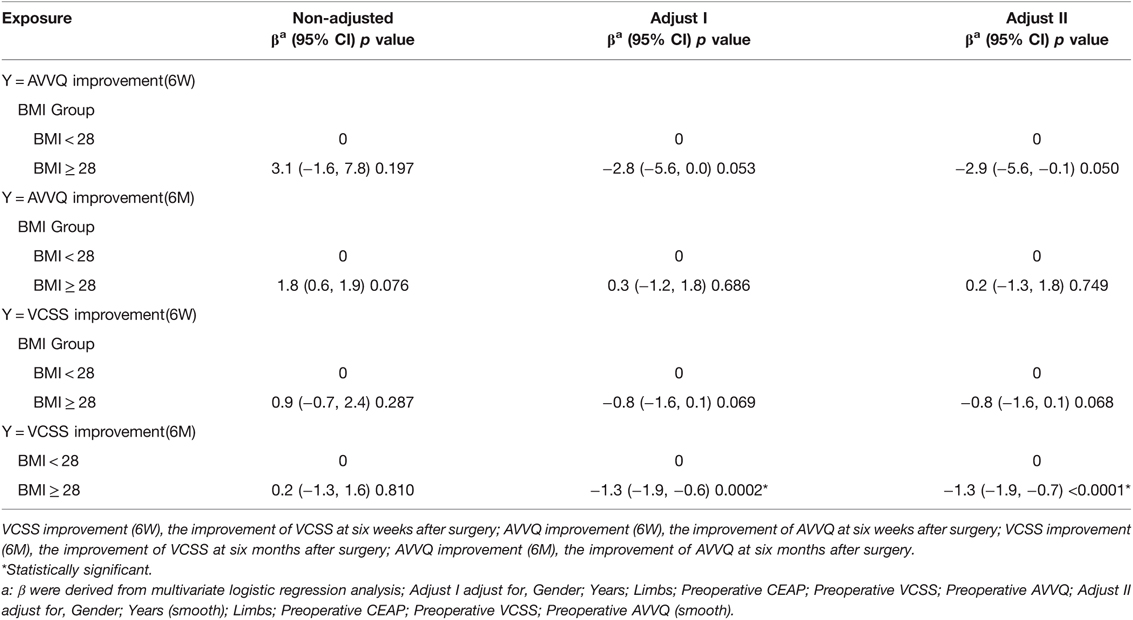
Table 4. Multivariate logistic regression model for risk factors associated with the improvement of AVVQ and VCSS at six weeks and six months after surgery.
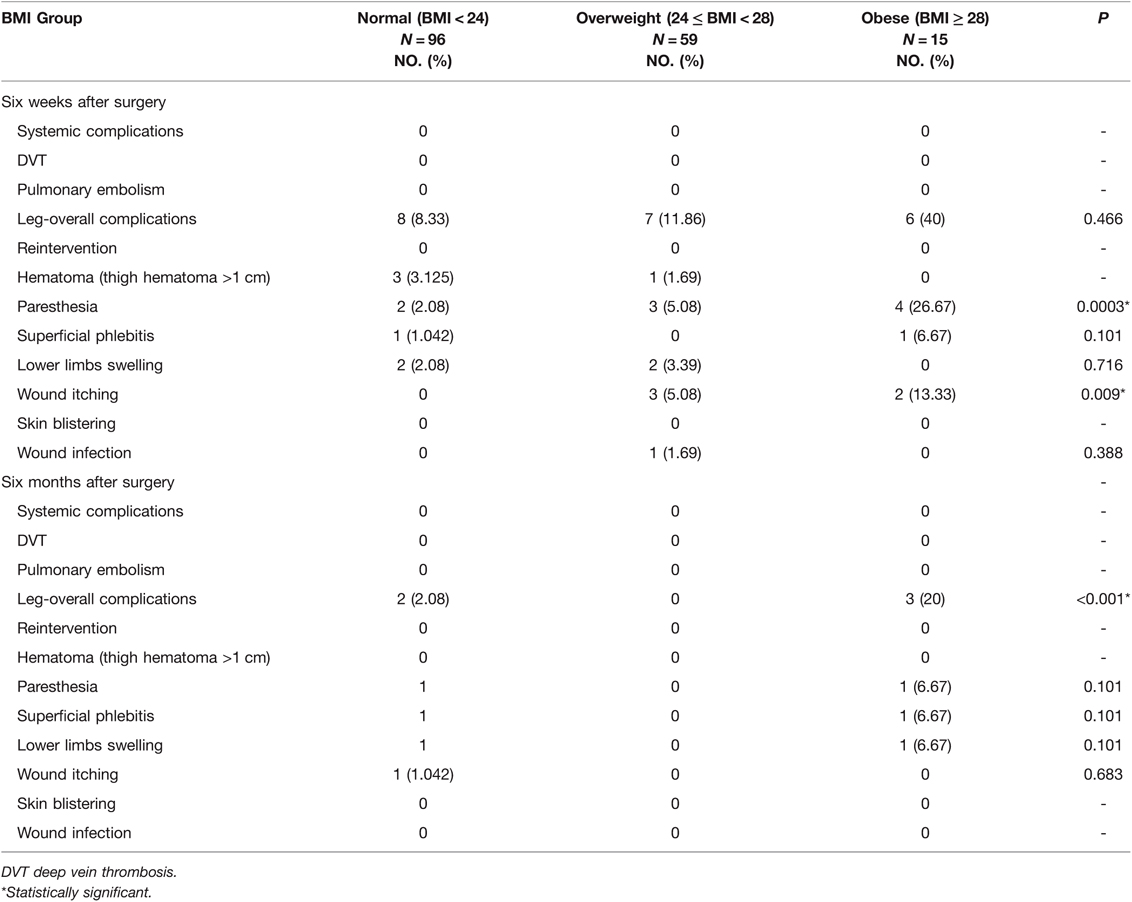
Postoperative Complications
During the observation period of our study, there were no systemic complications, and no patients received reintervention (Table 5). Meanwhile, there was a very low incidence of leg-specific postoperative complications. Paresthesia was the most common complication in the three groups, followed by wound itching (Table 5). Six weeks after surgery, the BMI groups were compared for overall or specific-aspect postoperative complications, and paresthesia was found to be significantly higher in the obese group compared with the normal BMI/overweight group (p-value = 0.00032). At 6 months after surgery, although there were no significant differences in the specific-aspect complications between the BMI groups, the overall complications of the legs were significantly higher in the obese group than in the normal BMI group (p-value < 0.001) (Table 5).
Discussion
Previously, numerous studies have examined the relationship between BMI and the incidence of varicose veins (24–27). A few studies have showed the relationship between BMI and the prognosis of varicose veins after ambulatory HLS surgery. In our prospective cohort study, after multivariable risk adjustment for potential confounding factors, we found that the BMI was independent of VCSS improvement and AVVQ improvement at 6 weeks after surgery, as well as the improvement of AVVQ at 6 months after surgery. At 6 months after surgery, we found that the improvement of VCSS in obese patients was significantly lower than that of the normal BMI or overweight groups. We also found that BMI was negatively correlated with the improvement of VCSS in the non-obese group at 6 weeks or 6 months after surgery. While BMI was positively correlated with the improvement of VCSS in obese patients at 6 weeks after surgery and was negatively correlated with the improvement of VCSS in obese patients at 6 months after surgery.
This result seems to be contradictory, but in fact it is reasonable. The BMI was independent of VCSS improvement and AVVQ improvement at 6 weeks after surgery, we believe that an explanation for this anomaly could be that obese patients have an obvious improvement of preoperative discomfort symptoms after surgery that resulting in no significant difference in AVVQ and VCSS scores. In the same way, this can explain why smooth curve fitting showed that BMI of 28 or higher had a positive relationship trend on the improvement of VCSS at 6 weeks after surgery. The VCSS score of obese patients was higher before surgery and the disappearance of postoperative symptoms made the VCSS score was lower, which leading to the improvement of VCSS at 6 weeks after surgery have an obvious improvement, which needs to be further confirmed by larger well-designed studies. Through curve fitting, we observed that the BMI had a negative relationship trend on the improvement of VCSS at 6 weeks after surgery in the non-obese group, although there was no statistical difference in multivariate analysis, which was consistent with the findings by Casana et al. (28). At six months after surgery, a negative correlation between BMI and the improvement of VCSS was confirmed by multivariate analysis and smoothing curves, which was also consistent with currently reports. Currently, the relationship between BMI and the prognosis of varicose veins surgery is controversial. The possible explanations for these inconsistent results were as follows: (a) different cut-off for BMI values in different investigations; (b) different age of individuals enrolled in different studies; (c) racial heterogeneity of BMI; (d) other factors. That needs to be further confirmed by larger well-designed studies.
Despite our efforts to optimize the experimental design, there are still some deficiencies. First, given the prospective design of our study, our sample size was relatively small. Larger well-designed cohort studies are warranted in the future. Second, our study only illustrates the early and midterm outcomes and does not include the long-term outcomes. Last, we did not include ultrasound follow-up data of the patients, which would have shed more light on the postoperative changes of the vein systems.
Conclusions
The BMI had no significant effect on the early prognosis of HLS performed in an ambulatory center. The mid-term results showed that the BMI had a negative relationship trend on the prognosis of HLS performed in an ambulatory center. Further, patients with high BMI who received ambulatory HLS for varicose veins had a higher risk of postoperative complications compared with patients with low BMI.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author’s.
Ethics statement
The studies involving human participants were reviewed and approved by Chinese Clinical Trial Registry. http://www.chictr.org.cn/. The patients/participants provided their written informed consent to participate in this study.
Author contributions
CWC and YTC are joint first authors and performed the majority of experiments. Conceptualization: JCZ, YKM, BH. Data curation: CWC, YTC, ZPW, YL, JRW. Formal analysis: CWC, YTC, YL, JRW. Methodology: CWC, YTC, DY, BH, JCZ, YKM. Project administration: JCZ and BH. Software: YY and BH. Supervision: DY, YY, BH, JCZ, YKM. Writing – original draft: CWC and YTC. Writing – review & editing: CWC, YTC, DY, YKM. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Evans CJ, Fowkes FG, Ruckley CV, Lee AJ. Prevalence of varicose veins and chronic venous insufficiency in men and women in the general population: Edinburgh Vein Study. J Epidemiol Community Health. (1999) 53(3):149–53. doi: 10.1136/jech.53.3.149
2. Rabe E, Berboth G, Pannier F. Epidemiology of chronic venous diseases. Wien Med Wochenschr. (2016) 166(9-10):260–3. doi: 10.1007/s10354-016-0465-y
3. Pannier-Fischer F, Rabe E. Epidemiology of chronic venous diseases. Hautarzt. (2003) 54(11):1037–44. doi: 10.1007/s00105-003-0616-0
4. Beebe-Dimmer JL, Pfeifer JR, Engle JS, Schottenfeld D. The epidemiology of chronic venous insufficiency and varicose veins. Ann Epidemiol. (2005) 15(3):175–84. doi: 10.1016/j.annepidem.2004.05.015
5. Gloviczki P, Comerota AJ, Dalsing MC, Eklof BG, Gillespie DL, Gloviczki ML, et al. The care of patients with varicose veins and associated chronic venous diseases: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. (2011) 53(5 Suppl):2S–48S. doi: 10.1016/j.jvs.2011.01.079
6. Zhang MY, Qiu T, Bu XQ, Li X, Liang G, Zhang H, et al. A national survey on management of varicose veins in China. J Vasc Surg-Venous L. (2018) 6(3):338–46.e1. doi: 10.1016/j.jvsv.2017.10.018
7. Yoh T, Okamura R, Nakamura Y, Kobayashi A. Divided saphenectomy for varicose vein in ambulatory surgery. Ann Vasc Dis. (2014) 7(2):195–8. doi: 10.3400/avd.hdi.14-00030
8. de Roos KP, Nieman FH, Neumann HA. Ambulatory phlebectomy versus compression sclerotherapy: results of a randomized controlled trial. Dermatol Surg. (2003) 29(3):221–6. doi: 10.1046/j.1524-4725.2003.29053.x
9. de Roos KP, Nieman F, Neumann HA. Patient satisfaction after ambulatory phlebectomy of varicose veins in the foot. Dermatol Surg. (2002) 28(11):1027–30. doi: 10.1046/j.1524-4725.2002.02080.x
10. Almeida JI, Raines JK. Ambulatory phlebectomy in the office. Perspect Vasc Surg Endovasc Ther. (2008) 20(4):348–55. doi: 10.1177/1531003508325054
11. Sadick NS. Advances in the treatment of varicose veins: ambulatory phlebectomy, foam sclerotherapy, endovascular laser, and radiofrequency closure. Dermatol Clin. (2005) 23(3):443–55, vi. doi: 10.1016/j.det.2005.03.005
12. Rasmussen LH, Bjoern L, Lawaetz M, Blemings A, Lawaetz B, Eklof B. Randomized trial comparing endovenous laser ablation of the great saphenous vein with high ligation and stripping in patients with varicose veins: short-term results. J Vasc Surg. (2007) 46(2):308–15. doi: 10.1016/j.jvs.2007.03.053
13. Pittaluga P, Chastanet S. Lymphatic complications after varicose veins surgery: risk factors and how to avoid them. Phlebology. (2012) 27(Suppl 1):139–42. doi: 10.1258/phleb.2012.012s12
14. Carruthers TN, Farber A, Rybin D, Doros G, Eslami MH. Interventions on the superficial venous system for chronic venous insufficiency by surgeons in the modern era: an analysis of ACS-NSQIP. Vasc Endovascular Surg. (2014) 48(7-8):482–90. doi: 10.1177/1538574414561226
15. Yeung TM, Cope AC, Whittome N, Lintott P. Raised BMI is an independent risk factor for groin surgical site infections in patients undergoing varicose vein surgery. Am J Infect Control. (2008) 36(2):152–3. doi: 10.1016/j.ajic.2007.08.002
16. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. (2000) 894:i–xii, 1–253. doi: 10.1002/jps.3080150106
17. Zhou BF. Cooperative Meta-Analysis Group of the Working Group on Obesity in C. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults–study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. (2002) 15(1):83–96. PMID: 12046553
18. Vasquez MA, Rabe E, McLafferty RB, Shortell CK, Marston WA, Gillespie D, et al. Revision of the venous clinical severity score: venous outcomes consensus statement: special communication of the American Venous Forum Ad Hoc Outcomes Working Group. J Vasc Surg. (2010) 52(5):1387–96. doi: 10.1016/j.jvs.2010.06.161
19. Staniszewska A, Tambyraja A, Afolabi E, Bachoo P, Brittenden J. The Aberdeen varicose vein questionnaire, patient factors and referral for treatment. Eur J Vasc Endovasc Surg. (2013) 46(6):715–8. doi: 10.1016/j.ejvs.2013.08.019
20. Knop C, Oeser M, Bastian L, Lange U, Zdichavsky M, Blauth M. Development and validation of the Visual Analogue Scale (VAS) Spine Score. Unfallchirurg. (2001) 104(6):488–97. doi: 10.1007/s001130170111
21. Stark PA, Myles PS, Burke JA. Development and psychometric evaluation of a postoperative quality of recovery score: the QoR-15. Anesthesiology. (2013) 118(6):1332–40. doi: 10.1097/ALN.0b013e318289b84b
22. Eklöf B, Rutherford RB, Bergan JJ, Carpentier PH, Gloviczki P, Kistner RL, et al. Revision of the CEAP classification for chronic venous disorders: consensus statement. J Vasc Surg. (2004) 40(6):1248–52. doi: 10.1016/j.jvs.2004.09.027
23. Caprini JA. Thrombosis risk assessment as a guide to quality patient care. Dis Mon. (2005) 51(2–3):70–8. doi: 10.1016/j.disamonth.2005.02.003
24. Labropoulos N, Kokkosis AA, Spentzouris G, Gasparis AP, Tassiopoulos AK. The distribution and significance of varicosities in the saphenous trunks. J Vasc Surg. (2010) 51(1):96–103. doi: 10.1016/j.jvs.2009.08.069
25. Iannuzzi A, Panico S, Ciardullo AV, Bellati C, Cioffi V, Iannuzzo G, et al. Varicose veins of the lower limbs and venous capacitance in postmenopausal women: relationship with obesity. J Vasc Surg. (2002) 36(5):965–8. doi: 10.1067/mva.2002.128315
26. Padberg F Jr, Cerveira JJ, Lal BK, Pappas PJ, Varma S, Hobson RW 2nd. Does severe venous insufficiency have a different etiology in the morbidly obese? Is it venous? J Vasc Surg. (2003) 37(1):79–85. doi: 10.1067/mva.2003.61
27. Danielsson G, Eklof B, Grandinetti A, Kistner RL. The influence of obesity on chronic venous disease. Vasc Endovascular Surg. (2002) 36(4):271–6. doi: 10.1177/153857440203600404
Keywords: varicose vein, high ligation and stripping, body mass index, ambulatory care center, great saphenous vein, prospective cohort study
Citation: Chen CW, Cai YT, Wang JR, Wu ZP, Liu Y, Huang B, Yang Y, Yuan D, Ma YK and Zhao JC (2022) The Effect of Body Mass Index on Outcome Following Ambulatory High Ligation and Stripping for Lower Varicose Veins: A Prospective Cohort Study. Front. Surg. 9:801729. doi: 10.3389/fsurg.2022.801729
Received: 25 October 2021; Accepted: 21 March 2022;
Published: 4 April 2022.
Edited by:
Faisal Aziz, Penn State Milton S. Hershey Medical Center, USAReviewed by:
Joseph Raffetto, VA Boston Healthcare System, Veterans Health Administration, United States Department of Veterans Affairs, USAYung-Wei Chi, University of California, Davis, USA
Copyright: Copyright © 2022 Chen, Cai, Wang, Wu, Liu, Huang, Yang, Yuan, Ma and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ji C. Zhao zhaojc3@163.com Yu K. Ma hxyymyk@126.com Bin Huang hxxgwkhb@126.com
Speciality section: This article was submitted to Vascular Surgery, a section of the journal Frontiers in Surgery
 Chu Wen Chen1
Chu Wen Chen1 Yu K. Ma
Yu K. Ma Ji C. Zhao
Ji C. Zhao