- Nuffield Department of Surgical Sciences, University of Oxford, Oxford, United Kingdom
Introduction: Paediatric burns are a common clinical presentation. The long-term scar outcomes in paediatric burns patients are relatively unknown as most are discharged after 6 weeks follow up, apart from the small number that are followed up by scar services depending on geographical availability. We aimed to determine whether the long-term scarring outcomes are significantly different in those who had surgical treatment with Versajet® debridement and Biobrane®, vs. those treated conservatively with non-adherent Mepitel® and Acticoat® dressings, in a cohort of paediatric burns patients.
Methods: The parents of all paediatric burns patients admitted to Stoke Mandeville Hospital from October 2014 to September 2017 were contacted by telephone to fill in the paediatric Brisbane Burn Scar Impact Profile (BBSIP), the only patient reported outcome measure (PROM) specifically aimed at children. The results from the questionnaires underwent statistical analysis to see if there was a significant difference in questionnaire scores between children treated surgically vs. those treated conservatively.
Results: A total of 107 children were admitted in the timeframe, responses were received from 34 patients with 13 having been treated surgically and 21 having been treated conservatively. In all 58 questions that make up the BBSIP, there was no statistically significant difference observed in the scores of those treated surgically vs. those treated conservatively. For 31 questions on the BBSIP, the lowest score indicating the best outcome was observed in all patients in both groups.
Discussion: Surgical management for burns is always the last resort. Our results could be interpreted to suggest clinicians need not fear the longer-term impact a scar may have when deciding whether to treat a paediatric burns patient surgically or conservatively. This study is the first to assess longer-term scar outcomes using the BBSIP. A larger data set and comparison with other burn units in the UK may help to provide more information on scar outcomes between different methods of surgical and conservative treatment. We found no statistically significant difference in the long-term scar outcomes as assessed by the BBSIP in paediatric burn patients treated with Versajet® debridement and Biobrane®, vs. those treated conservatively with non-adherent Mepitel® and Acticoat® dressings.
Introduction
The global number of pediatric burns presenting to hospitals in 2005 was 505,276, with a then pediatric population of 1.843 billion (1). There is no defined “gold standard” for treating pediatric partial thickness burns. First aid involves cooling the site with water to dissipate any thermal energy followed by providing a moist wound environment, physiologically stabilizing the patient, removing exudate, preventing infection, and minimizing pain (2, 3).
The Stoke Mandeville Hospital Burns unit receives approximately 450 pediatric burns referrals per year. The most common presentation is of scald injuries to the chest, typically from hot drinks. The thinner dermis in younger children can often result in a deeper more substantial burn compared to a similar injury in adults (2). The majority of patients can be treated conservatively, although those with deeper burns may require surgical intervention.
Depending on the depth of the burn, a surgical approach may be required to remove necrotic non-viable tissue. An issue with this surgical debridement is removal of normal healthy viable tissue along with non-viable tissue which can result in worse scarring (4, 5). The Versajet® (Smith and Nephew, Key Largo FL, USA) hydrosurgery system has been used as a burn debridement method for 12 years (6). Its mechanism is to use high pressure sterile saline to create a controlled cutting field with a built in suction system. Due to its ability to debride in a controlled manner, it is regarded as a useful tool for debriding burned tissue whist preserving the dermis (7). The thinner dermis observed in the pediatric population means this greater level of control is advantageous (5). Cubison et al 2006 reported using Versajet® debridement and subsequent Biobrane® dressings in pediatric patients with good healing and scar outcomes (5).
After the burn has healed, injuries that have gone beyond 33.1% of skin depth will typically leave a scar (8). Scars can be itchy, painful, tight, functionally restrictive, and cosmetically disfiguring. Many studies have reported on the short term outcomes of pediatric burn wounds focusing on factors such as hospital stay, time to healing and cost-effectiveness of treatment (2, 3, 9–11). Longer term scar outcomes are less commonly described, with discharge from outpatient clinic reported as a common contributory factor (2). Fan et al 2018 commented on the longer term scarring outcomes of pediatric burns treated with Biobrane® compared to those treated with silver based dressings (9). No difference in outcomes was observed when using the patient reported outcome section of the Patient Observer Scar Assessment Scale (POSAS) (9). The POSAS is a scar specific assessment tool comprised of an observer section, typically filled in by a clinician; and a patient reported section for scar symptoms and appearance. For Versajet® debridement, there is limited literature observing the longer term scarring outcomes in pediatric burn patients. Legemate et al 2018 put forward a research protocol to compare the longer-term scarring outcomes in patients of all ages with burns treated with conventional surgical debridement vs. Versajet® debridement (12). Although results have not been published yet, they will be following up patients at 12 months post-surgery using the POSAS as the primary outcome measure.
The novel BBSIP is a PROM developed to assess scar outcomes based on elements related to quality of life in patient with scars from burn injuries (13). The BBSIP has been further developed to create versions dedicated to young children aged 8 to 18 (BBSIP8–18) and the caregivers of younger children aged 0 to 8 (BBSIP0–8) (14, 15). A recent study measured the internal consistency, test-retest reliability, longitudinal validity and responsiveness of the BBSIP in post-acute burn period (15). The content and construct validity had been reported in another study (13, 16). The authors concluded that the BBSIP is a suitable PROM in the post-acute burn period and that future studies will help evaluate its use as a longer term scar outcome tool (15). The POSAS is also considered to be a well validated PROM for scarring. The observer element filled in by an assessor has demonstrated acceptable reliability for the vascularity section and total score; along with internal consistency and construct validation (17, 18). Test-retest reliability of the POSAS has been reported as acceptable for all items (except vascularity and relief) in the observer section and the pain section of the patient version (19). The internal consistency for the patient scale has been reported as generally acceptable (17).
There is little data on the outcomes of the scar in children treated conservatively vs. surgically for burns. By utilizing a purpose created paediatric burn scar assessment tool; the aim of this study was to determine if there were any long-term differences in scarring outcomes of pediatric burn patients treated with surgical Versajet® and Biobrane® compared to conservative Acticoat® and non-adherent dressings. By comparing the two, we hoped to determine if there would be superior scarring outcomes in either group.
Materials and methods
A retrospective review was performed of all pediatric burns patients admitted to the Stoke Mandeville Burns Unit from October 2014 to September 2017. At the time of this study, the unit's policy for superficial partial thickness burn conservative burn treatment was non-adherent dressing Mepitel® and Acticoat® after cleansing with aqueous chlorhexidine. Surgical management for superficial partial thickness burns was with Versajet® debridement and Biobrane® dressings.
Established for over 30 years, Biobrane® (UDL Laboratories, Rockford, IL, USA) is a popular treatment choice for superficial and partial thickness burns. It consists of a semipermeable silicone membrane combined with a Type I collagen (of porcine origin) coated nylon mesh. Multiple studies have demonstrated that Biobrane® can protect against infection, reduce pain, improve healing time resulting in a shorter inpatient stay, reduced dressing changes and better cost-effectiveness (10, 20–25) These qualities have made it a popular dressing choice around the UK. Despite its widespread use, there is a lack of data on longer term scar outcomes of patients treated with Biobrane (10).
Silver sulfadiazine and silver nitrate impregnated dressings such as Acticoat®, are another popular treatment for partial thickness burns (22, 23, 26). The silver is reported to provide an anti-microbial surface helping to reduce the risk of infection of the burn wound (27). Acticoat® is a popular choice in UK burn centers, consisting of a silver nano-crystalline mesh that can be manipulated over the burn site (27, 28). Other reported benefits of Acticoat® include fewer inflammatory reactions compared to silver sulfadiazine and prolonged silver release (27, 28). There is conflicting information between topical silver dressings compared with Biobrane®, but the few available studies report no observed differences in longer term outcomes (9, 11, 26).
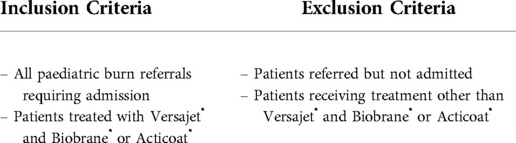
A total of 107 patients satisfied our inclusion and exclusion criteria (Table 1) and were included in the study. The data collected from the patients' online medical records included: age, gender, Total Body Surface Area (TBSA), mechanism of burn (e.g., scald), number of follow up appointments, further treatments, the location of the burn, injury date, assessment date, admission date and treatment received. As the focus was on longer term scar outcomes, many patients were no longer being followed up in outpatient clinic and so scar evaluation was conducted via telephone interview using the age-appropriate version of the BBSIP. The 107 patients were contacted a maximum of 3 times using telephone numbers from their records.
Data were analyzed using IBM SPSS Statistics for Windows version 26 (IBM Corp, New York USA) and are presented as mean ± standard deviation. A two-tailed Student's t-test was performed for the continuous variables; for categorical response variables a Fisher's exact test was used. The study was supported by Buckinghamshire NHS Trust as a service evaluation study. Research ethics was not required as previous treatments that followed trust protocol were being evaluated.
Results
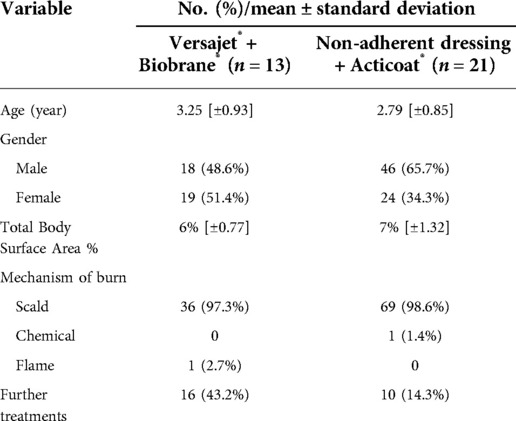
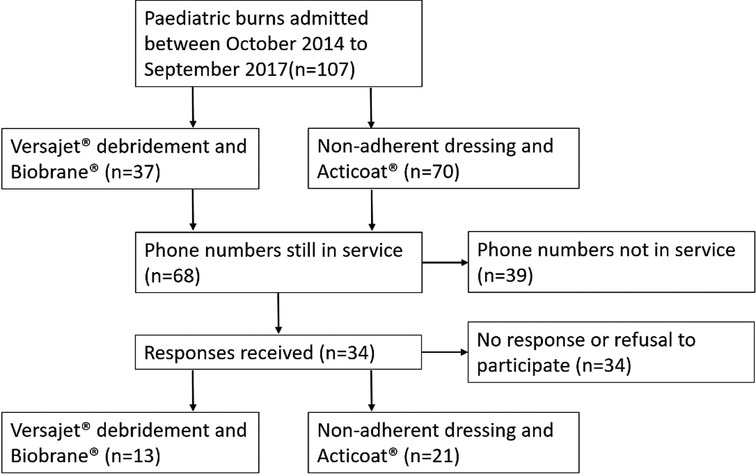
The dataset included all children admitted to the ward with a burn injury between October 2014 and September 2017. All 107 children admitted met our inclusion criteria. There were 37 patients (34.6%) treated surgically with Versajet® debridement and Biobrane® dressings; and 70 (65.4%) patients treated conservatively with Mepitel® and Acticoat®. Most of the pediatric patients in our study were pre-school (Versajet® and Biobrane® vs. Mepitel® and Acticoat®: mean age 3.25[±0.93] vs. 2.79[±0.85]). The overwhelming majority (n = 105 98.1%) had scalds whilst one patient had flame burns and another chemical burns (Table 2).
Telephone interviews resulted in a total of 34 responses (Versajet® and Biobrane® vs. Acticoat®: 13 vs. 21); 39 of the phone numbers contacted were no longer in service and a further 34 phone numbers resulted in no response or declined to participate (Figure 1).
For the responses received by telephone interview, the average interval post-injury was three years (Versajet® and Biobrane® vs. Acticoat®: 34.19[±7.71 months] vs. 36.85[±7.36 months]). As all patients were 8 years old or younger, the BBSIP0–8 was used (see Appendix).
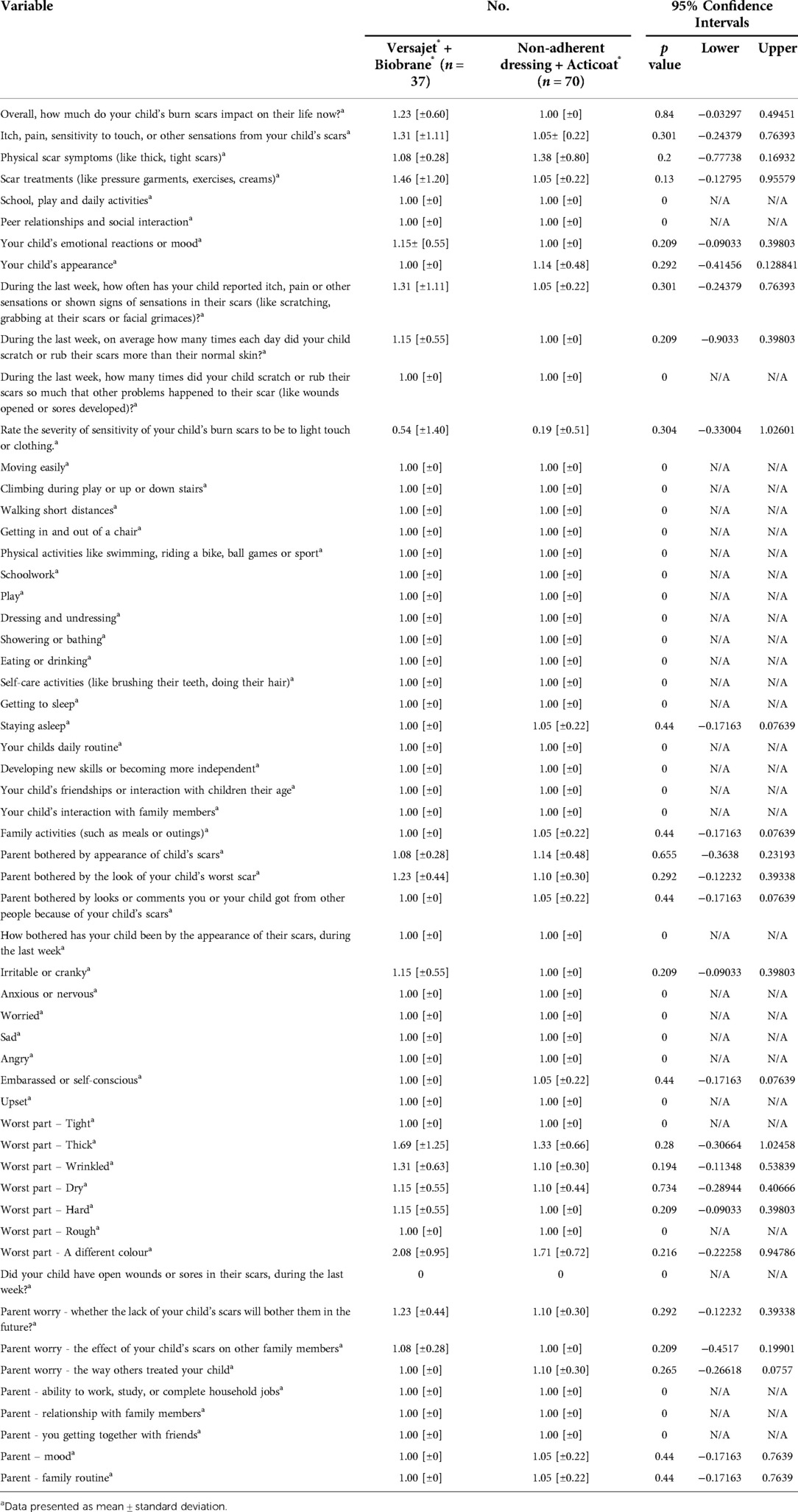
Of the 58 questions that make up the BBSIP0–8, a two-tailed students t-test was performed on the results from 57 of them (Table 3). For 31 of the 57 questions, both treatment groups scored the same lowest possible score indicating no impact on the child's life/best possible outcome. For the remaining 26 questions, there was no statistically significant difference observed between the groups. The lower and upper 95% confidence intervals spanned across zero in all questions.
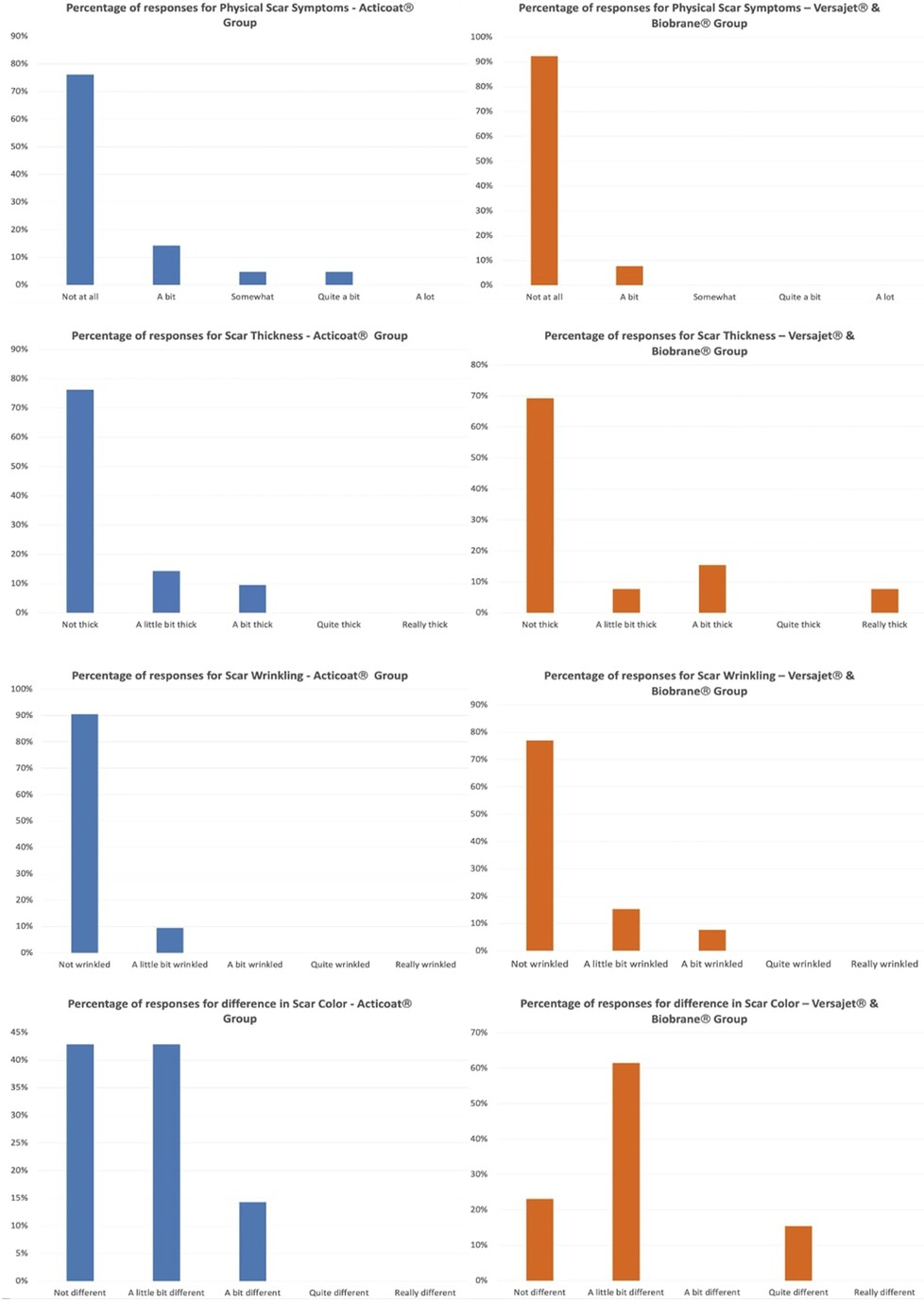
Part 7 of the BBSIP focuses on physical symptoms with question 15 asking caregivers to rate how much the child's worst area of scar was affected by a physical property in the last week.
Physical properties of thickness (question 15B), wrinkling (question 15C) and difference in color (question 15G) demonstrated the larger differences (Figure 2). Responses for question 15B relating to scar thickness in the conservative treatment group were: 16 (76%) conservative vs. 9 (69%) surgical reported not thick, 3 (14%) conservative vs. 1 (8%) surgical reported a little bit thick, 2 (10%) reported a bit thick in conservative and 1 (8%) reported really thick in surgical. Question 15C focused on wrinkling with responses as; 19 (91%) conservative, vs. 10 (77%) surgical reported not wrinkled, 2 (9%) conservative vs. 2 (15%) reported a little bit wrinkled with 1 (8%) report of a bit wrinkled in the surgical group. Scar colour asked in question 15G had the largest difference in responses; 9 (43%) conservative vs. 3 (23%) surgical reported not different, 9 (43%) conservative vs. 8 (62%) surgical reported a little bit different, 3 (14%) conservative reported a bit different and 2 (15%) surgical reported quite different. In the surgical treatment group, 6 of the 13 had further treatments in clinic, whilst 3 of the 21 children in the conservative group had further treatments. Question 14 in part 7 of the BSIP0–8 asked to describe the worst part of the child's scar by anatomical location. The Fishers exact test was used for any correlation between worst areas of burn and treatment group. No statistically significant difference was demonstrated between the two groups (Fishers Exact Test = 0.817).
Discussion
This study did not identify any statistically significant differences in longer-term scar outcomes as assessed by the BBSIP0–8 in pediatric burn patients treated with surgical Versajet® debridement and Biobrane® vs. those treated conservatively with Acticoat® and non-adherent dressings. For over half of the questions asked as part of the BBSIP, all responses in both groups were the lowest possible score indicating the least/no impact of the scar on the child's life. For part 3 of the BBSIP0–8 which focuses on school, play and daily activities, 14 of the 15 questions in this section all scored the lowest possible score in both groups. Part 6 of the BBSIP0–8 focuses on emotional reactions; we found that 5 out of the 7 questions in the sections had scored the lowest possible score in both groups (irritable or cranky and self-conscious). The area that had the most variation was part 7 of the BBSIP0–8 which focuses on physical symptoms. Questions focused on the worst areas of scar tightness and roughness scored the lowest possible in both groups. Thickness, wrinkling, dryness, hardness and difference in color all had the greater variety of responses in both groups. These properties are assessed as part of the POSAS patient scale referred to as scar color, stiffness, thickness and irregularity. From our data, we can conclude that between both treatment groups there is no significant long-term difference in the scarring outcome; with most variation observed in differences in scar colour, thickness, hardness, stiffness and irregularity compared to normal skin.
Burns specialists will use clinical judgement to determine whether or not to debride a burn, weighing up the risks of treating surgically vs. conservatively. There can be some flexibility to choose whichever approach will get the child healed fastest, acknowledging that the longer-term scarring outcomes would likely be the same. One of the caveats of the study is that potentially the children treated through different methodologies had different depths, although this is something that we aimed to control for. Our results revealed that a higher proportion of the children treated surgically underwent further treatments in scar clinic compared to those treated conservatively. This could be due to deeper, more severe burns in those treated surgically. Despite this, longer term scarring outcomes were similar.
There are multiple subjective outcome measures to assess the results of a scar. The most commonly used in academic literature include the VSS and its various modifications, the MSS and the POSAS; however, none of these are specifically targeted at children. The POSAS is a unique outcome assessment tool as it includes both an assessor score and a patient reported score and has been used in pediatric longer-term burn scar studies by conducting telephone interviews with the parents of children (9). The POSAS patient section assesses the scars on pain, itch, color, stiffness, thickness and irregularity. The defined criteria for a PROM's quality is based on content validity, internal consistency, criterion validity, construct validity, reproducibility, longitudinal validity, responsiveness, floor and ceiling effects and interpretability (29). The defined COSMIN criteria can be used to assess the methodological quality of studies assessing a PROM (30). A suitable PROM for children with burn scars would include assessment of how the scar affects all elements related to quality of life (physical, mental and social well-being) (16). Pediatric specific PROMs would ideally use language that is age-appropriate, not include elements irrelevant to children (such as driving and financial) and be focused on factors important in a child's development such as play. For younger children with a burn injury, the PROM would be more appropriate to be aimed at the primary caregiver of the child. Given the aesthetic as well as functional impact of scarring, a suitable PROM would be able to distinguish from patients that have undergone surgery and those that haven't (31, 32). It would additionally allow for comparison of techniques and identify patients likely to benefit from the procedure (32).
This study is the first to utilize the BBSIP0–8 as a longer-term scar outcome tool. Tyack et al 2019 described the value of the BBSIP0–8 in the acute post burn phase and that more studies would be required to establish the BBSIP0–8 role for longer term scar outcomes (15). The small sample size means the study may not be adequately powered and is potentially at risk of type II error. The clinical entries used as part of the data collection would not always include the depths of the burn injury and language used to describe depth was not uniform. Additionally, there is a degree of subjectivity when assessing depths of burns clinically. Telephone interviews have generally been regarded as less-attractive than face-to-face interviews and physical questionnaires (33). Negatives of telephone interviews in research have been reported as a lack of visual cues can result in a loss of contextual and non-verbal data which in turn may lead to lower quality data (33). The BBSIP0–8 is a physical questionnaire designed to be filled in by the caregiver of the patient. Whether or not telephone interviews result in lower quality data compared to physical interviews or questionnaires remains a matter of debate (33).
In conclusion, no difference was found in the long term scar outcomes as assessed by the BBSIP0–8 in those treated surgically with Versajet® debridement and Biobrane® compared to those treated conservatively with Acticoat® and non-adherent dressings. The BBSIP and its various versions are the only full PROM for burns scars widely available. It has value as a longer-term scar assessment tool, but a shorter more focused version may be of more value in clinic.
Contribution to the field statement
Burn injuries in children are a common occurrence accounting for approximately ¼ of all burn presentations. The general initial aim of burn management is to resuscitate if necessary and reduce the TBSA/depth of the burn by cooling the area down. Following this, a decision based upon clinical assessment is made on whether the burn can be treated conservatively with dressings or whether surgical intervention is required. The decision to operate is based upon the depth of the burn and what will likely cause the burn to heal fastest. As children are often discharged after a six week follow up the long-term appearance of the scar is relatively unknown unless they re-present with a problematic scar. By using the world's only available patient reported outcomes measure specifically aimed at assessing pediatric burn scars; we have demonstrated there is no statistically significant difference in the long-term scarring outcomes in pediatric burns treated conservatively with Mepitel® and Acticoat® vs. those treated surgically with Versajet® debridement and Biobrane®. The Brisbane Burn Scar Impact Profile aimed at children has value in assessing long-term scars, but a limitation is the length of the questionnaire. We propose that a shorter more focused version may be more valid in a time pressured clinical environment.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the participants’ legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
RM - first author. FI - second author. All authors contributed to the article and approved the submitted version. All authors contributed to the article and approved the submitted version.
Acknowledgments
I would like to thank Miss Alexandra Murray for her support with this research, along with the Stoke Mandeville Hospital Plastic Surgery Department.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Burd A, Yuen C. A global study of hospitalized paediatric burn patients. Burns. (2005) 31:432–8. doi: 10.1016/j.burns.2005.02.016
2. Vloemans AF, Hermans MH, van der Wal MB, Liebregts J, Middelkoop E. Optimal treatment of partial thickness burns in children: a systematic review. Burns. (2014) 40:177–90. doi: 10.1016/j.burns.2013.09.016
3. Kim LK, Martin HC, Holland AJ. Medical management of paediatric burn injuries: best practice. J Paediatr Child Health. (2012) 48:290–5. doi: 10.1111/j.1440-1754.2011.02128.x
4. Orgill DP. Excision and skin grafting of thermal burns. N Engl J Med. (2009) 360:893–901. doi: 10.1056/NEJMct0804451
5. Cubison TC, Pape SA, Jeffery SL. Dermal preservation using the Versajet hydrosurgery system for debridement of paediatric burns. Burns. (2006) 32:714–20. doi: 10.1016/j.burns.2006.01.023
6. Gravante G, Esposito G, Di Fede MC, Delogu D, Montone A. Versajet hydrosurgery in burn wound debridement: a preliminary experience. Burns. (2007) 33:401. doi: 10.1016/j.burns.2006.08.043
7. Kimble RM, Mott J, Joethy J. Versajet® hydrosurgery system for the debridement of paediatric burns. Burns. (2008) 34:297–8. doi: 10.1016/j.burns.2007.08.018
8. Dunkin CS, Pleat JM, Gillespie PH, Tyler MP, Roberts AH, McGrouther DA. Scarring occurs at a critical depth of skin injury: precise measurement in a graduated dermal scratch in human volunteers. Plast Reconstr Surg. (2007) 119:1722–32; discussion 1733–4. doi: 10.1097/01.prs.0000258829.07399.f0
9. Fan C, Pek CH, Por YC, Lim GJS. Biobrane dressing for paediatric burns in Singapore: a retrospective review. Singapore Med J. (2018) 59:360–5. doi: 10.11622/smedj.2017116
10. Mandal A. Paediatric partial-thickness scald burns – is Biobrane the best treatment available? Int Wound J. (2007) 4:15–9. doi: 10.1111/j.1742-481X.2006.00279.x
11. Selvarajah D, Bollu BK, Harvey J, Jacques M, Jehangir S, Fuller ES, et al. Acticoat versus biobrane: a retrospective review on the treatment of paediatric mid-dermal torso burns. Int J Burns Trauma. (2019) 9:82–7. PMID: 31523483, PMCID: 6737381
12. Legemate CM, Goei H, Middelkoop E, Oen IMMH, Nijhuis THJ, Kwa KAA, et al. Long-term scar quality after hydrosurgical versus conventional debridement of deep dermal burns (HyCon trial): study protocol for a randomized controlled trial. Trials. (2018) 19:239. doi: 10.1186/s13063-018-2599-2
13. Tyack Z, Ziviani J, Kimble R, Plaza A, Jones A, Cuttle L, et al. Measuring the impact of burn scarring on health-related quality of life: development and preliminary content validation of the Brisbane Burn Scar Impact Profile (BBSIP) for children and adults. Burns. (2015) 41:1405–19. doi: 10.1016/j.burns.2015.05.021
14. Simons M, Kimble R, McPhail S, Tyack Z. The brisbane burn scar impact profile (child and young person version) for measuring health-related quality of life in children with burn scars: a longitudinal cohort study of reliability, validity and responsiveness. Burns. (2019) 45:1537–52. doi: 10.1016/j.burns.2019.07.012
15. Simons M, Kimble R, McPhail S, Tyack Z. The longitudinal validity, reproducibility and responsiveness of the Brisbane Burn Scar Impact Profile (caregiver report for young children version) for measuring health-related quality of life in children with burn scars. Burns. (2019) 45:1792–809. doi: 10.1016/j.burns.2019.04.015
16. Simons M, Price N, Kimble R, Tyack Z. Patient experiences of burn scars in adults and children and development of a health-related quality of life conceptual model: a qualitative study. Burns. (2016) 42:620–32. doi: 10.1016/j.burns.2015.11.012
17. Draaijers LJ, Tempelman FRH, Botman YAM, Tuinebreijer WE, Middelkoop E, Kreis RW, et al. The patient and observer scar assessment scale: a reliable and feasible tool for scar evaluation. Plast. Reconstr. Surg. (2004) 113:1960–5. doi: 10.1097/01.prs.0000122207.28773.56
18. Tyack Z, Simons M, Spinks A, Wasiak J. A systematic review of the quality of burn scar rating scales for clinical and research use. Burns. (2012) 38:6–18. doi: 10.1016/j.burns.2011.09.021
19. Tyack Z, Kimble R, McPhail S, Plaza A, Simons M. Psychometric properties of the Brisbane Burn Scar Impact Profile in adults with burn scars. PloS one. (2017) 12:e0184452. doi: 10.1371/journal.pone.0184452
20. Lal S, Barrow RE, Wolf SE, Chinkes DL, Hart DW, Heggers JP, et al. Biobrane improves wound healing in burned children without increased risk of infection. Shock (Augusta, Ga.). (2000) 14:314–8; discussion 318–9. doi: 10.1097/00024382-200014030-00013
21. Zachary L, Heggers JP, Robson MC, Leach A, Ko F, Berta M. The use of topical antimicrobials combined with Biobrane in burn wound infections. J Trauma Acute Care Surg. (1982) 22:533–6. doi: 10.1097/00005373-198210000-00005
22. Gerding RL, Emerman CL, Effron D, Lukens T, Imbembo AL, Fratianne RB. Outpatient management of partial-thickness burns: Biobrane® versus 1% silver sulfadiazine. Ann Emerg Med. (1990) 19:121–4. doi: 10.1016/S0196-0644(05)81793-7
23. Gerding RL, Imbembo AL, Fratianne RB. Biosynthetic skin substitute vs. 1% silver sulfadiazine for treatment of inpatient partial-thickness thermal burns. J Trauma. (1988) 28:1265–9. doi: 10.1097/00005373-198808000-00022
24. Pruitt BA, Levine NS. Characteristics and uses of biologic dressings and skin substitutes. Arch Surg. (1984) 119:312–22. doi: 10.1001/archsurg.1984.01390150050013
25. Muganza A, Cullingworth L. A prospective single-centre randomised controlled study to compare the time to healing of partial thickness burn wounds treated with versajet, biobrane and acticoat to conventional therapy. Glob J Med Res. (2015) 14(6):5–12. Online ISSN: 2249-4618 / Print ISSN: 0975-5888.
26. Barret JP, Dziewulski P, Ramzy PI, Wolf SE, Desai MH, Herndon DN. Biobrane versus 1% silver sulfadiazine in second-degree pediatric burns. Plast Reconstr Surg. (2000) 105:62–5. doi: 10.1097/00006534-200001000-00010
27. Khundkar R, Malic C, Burge T. Use of Acticoat™ dressings in burns: what is the evidence? Burns. (2010) 36:751–8. doi: 10.1016/j.burns.2009.04.008
28. Dunn K, Edwards-Jones V. The role of Acticoat with nanocrystalline silver in the management of burns. Burns. (2004) 30(Suppl 1):S1–9. doi: 10.1016/S0305-4179(04)90000-9
29. Terwee CB, Bot SDM, de Boer MR, van der Windt DAWM, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. (2007) 60:34–42. doi: 10.1016/j.jclinepi.2006.03.012
30. Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, et al. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual Life Res. (2010) 19:539–49. doi: 10.1007/s11136-010-9606-8
31. Harrison CJ, Rae C, Tsangaris E, Wong Riff KWY, Swan MC, Goodacre TEE, et al. Further construct validation of the CLEFT-Q: ability to detect differences in outcome for four cleft-specific surgeries. J Plast Reconstr Aesthet Surg. (2019) 72:2049–55. doi: 10.1016/j.bjps.2019.07.029
32. Kosowski TR, McCarthy C, Reavey PL, Scott AM, Wilkins EG, Cano SJ, et al. A systematic review of patient-reported outcome measures after facial cosmetic surgery and/or nonsurgical facial rejuvenation. Plast Reconstr Surg. (2009) 123:1819–27. doi: 10.1097/PRS.0b013e3181a3f361
Keywords: scarring, paediatric, surgery, conservative treatment, long term outcome
Citation: Mistry R and Issa F (2022) No statistically significant difference in long term scarring outcomes of pediatric burns patients treated surgically vs. those treated conservatively. Front. Surg. 9:727983. doi: 10.3389/fsurg.2022.727983
Received: 20 June 2021; Accepted: 23 August 2022;
Published: 9 September 2022.
Edited by:
Arshad R. Muzaffar, University of Missouri, United StatesReviewed by:
Fatih Zor, Wake Forest School of Medicine, United StatesBjörn Behr, Ruhr University Bochum, Germany
© 2022 Mistry and Issa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Riyam Mistry cml5YW1taXN0cnlAbmhzLm5ldA==
Specialty Section: This article was submitted to Reconstructive and Plastic Surgery, a section of the journal Frontiers in Surgery
 Riyam Mistry
Riyam Mistry Fadi Issa
Fadi Issa