- 1Department of Orthopaedics, First Affiliated Hospital of Dalian Medical University, Dalian, China
- 2Key Laboratory of Molecular Mechanism for Repair and Remodeling of Orthopaedic Diseases, Dalian, China
- 3Department of Medical Engineering, The 967th Hospital of Chinese People's Liberation Army, Dalian, China
- 4Department of Orthopedics, Southwest Hospital, Army Medical University, Chongqing, China
Background: Depression is a highly prevalent mental disorder, and we found that patients with preoperative depression had worse postoperative improvement in lumbar fusion. Are mental factors related to the prognosis of laminoplasty?
Objective: To analyze the relationship between depression and clinical outcomes after laminoplasty for the treatment of multilevel CSM.
Methods: In this retrospective study, 115 patients with multilevel cervical spondylotic myelopathy (CSM), who underwent laminoplasty and were followed up for more than 1 year, were enrolled in this study from October 2018 to October 2021. Patients with the scores of 21-item Beck Depression Inventory (BDI) ≥ 15 or Hamilton Depression Scale-24 (HAMD-24) > 20 were included in the depression group. The clinical outcomes were evaluated by the changes and recovery rate (RR) of Japanese Orthopaedic Association Scores (JOA) and Neck Disability Index (NDI) respectively. Univariate and multiple linear regression analyses were performed to reveal the relationship between preoperative depressive states and clinical outcomes.
Results: Fourteen patients were diagnosed with depression by BDI and twenty-nine by HAMD-24. Between the depression group and the non-depression group, the age, gender, smoking history, and duration of symptoms were statistically significant (P < 0.05). Multiple linear regression showed that the BDI scores had a negative relationship with the changes and RR of JOA and NDI, and the HAMD-24 scores had a negative relationship with the changes and RR of JOA.
Conclusions: Preoperative depression in patients with multilevel CSM can lead to worse prognosis. In order to improve the curative effect of the operation, we should pay attention to the psychological state monitoring and intervention of patients before they receive laminoplasty.
Introduction
Cervical spondylotic myelopathy (CSM) is a disease with cervical spinal cord damage as the main manifestation due to cervical degenerative changes (1). Multilevel CSM is often accompanied by a variety of serious symptoms, and conservative treatment is often not easy to alleviate. Surgical treatment is particularly important for patients with failed conservative treatment of multilevel CSM. There are two options for the surgical approach, anterior and posterior. Anterior approach includes anterior cervical discectomy and fusion (ACDF) and anterior cervical subtotal corpectomy and fusion (ACCF), while posterior approach includes laminoplasty and laminectomy (1–3). Compared with anterior approach, posterior approach can avoid postoperative complications such as dysphagia, hoarseness, postoperative cervical instability, kyphosis, and delayed deterioration of neurological function (4–7). In posterior approach, laminoplasty is suitable for most patients, especially the elderly patients. At the same time, due to the preservation of vertebral lamina, laminoplasty can maintain the overall stability of cervical spine and reduce the incidence of postoperative complications such as axial pain and scar formation (8–10). The postoperative outcome of patients not only depends on the approach of operation, but also relates to many factors, including patient's age, duration of symptoms, neurological status and so on (11–15).
Depression is a highly prevalent mental disorder. There are about 322 million patients with depression worldwide, and the prevalence rate is about 4.4% (16). As many as 40% of people have depression symptoms at a young age, and the incidence rate of depression reaches a peak between 50 and 60 years old (17). In daily life, psychosocial and biological stressors are both the causes of depression (17, 18). At least one of the symptoms of depression must be either depressed mood or decreased positive affect (19). Depression is a common comorbidity among patients with musculoskeletal pain, and patients who are depressed complain more physical symptoms than patients who are not (20). At present, there are many screening tools for the diagnosis of depression, including the 21-item Beck Depression Inventory (BDI) (21), Hamilton Depression Scale-24 (HAMD-24) (22), the Patient Health Questionnaire-9 (23), and the Depression in the Medically ill (DMI) (24). The BDI is widely used in depression screening in view of their sensitivity, specificity and diagnostic validity (25).
In our previous study, we found that patients with preoperative depression had worse postoperative improvement in lumbar fusion (26). Are mental factors related to the prognosis of laminoplasty? In order to explore the relationship between preoperative mental disorders and postoperative effect in patients with multilevel CSM, we conducted a retrospective study to investigate the impact of preoperative depression assessed using both BDI and HAMD-24 on clinical outcomes following laminoplasty. We reviewed the literature and found that there was no study to analyze this relationship between depression and the prognosis of laminoplasty, and this study might be the first study to analyze this relationship using BDI and HAMD-24 scales.
Materials and methods
Patient population
This was a retrospective clinical study. This study was approved by the ethics statement of our hospital (First Affiliated Hospital of Dalian Medical University, Dalian). Between October 2018 and October 2021, 121 patients with multilevel CSM, who underwent laminoplasty took part in the study. The inclusion criteria were: (1) age ≥ 18 years old; (2) diagnosed as multilevel CSM; (3) posterior cervical approach was underwent; (4) the follow-up time was > 1 year. The exclusion criteria were: (1) previous spine surgery history; (2) postoperative surgical site infection or reoperation; (3) severe postoperative complications occurred; (4) severe mental disorder or confusion; (5) with serious underlying diseases.
Data collection and outcome evaluations
The data collected included the patient's age, gender, body mass index (BMI), smoking history, drinking history, comorbidities (diabetes, hypertension, rheumatism), symptom duration, and surgical levels. All patients were evaluated for depressive symptoms by BDI and HAMD-24 before operation. The BDI scores ≥15 or HAMD-24 scores >20 were diagnosed as depression. BDI is widely used in clinical epidemiological investigation. It consists of 21 items, including a series of indicators such as self, environment, work, life, and future, etc. The total scores rank from 0 to 39. The higher the scores, the more serious the depressive symptoms are. BDI is a comprehensive depression assessment tool. HAMD-24 is the most widely used scale in clinical evaluation of depression, which includes 24 indexes. The HAMD-24 evaluation method is simple and the standard is clear. The total scores of HAMD-24 can reflect the severity of the disease, and can be used to evaluate the depressive symptoms of depression, bipolar disorder, neurosis and other diseases, especially for depression.
The Japanese Orthopaedic Association Scores (JOA) and Neck Disability Index (NDI) scores were used to evaluate the severity of patient's symptoms before surgery and 1 year after surgery. JOA mainly evaluates the motor function, sensation and bladder function of the limbs, the total scores are between 0 and 17, the lower the scores, the more obvious the dysfunction. The NDI scores include two parts: neck pain-related symptoms and assessment of the ability of daily living, the total scores rank from 0 to 50, higher scores predict more severe symptoms.
We used the preoperative and postoperative changes of JOA and NDI scores to indicate the patient's improvement, the changes were calculated by JOA as follows: |postoperative JOA−preoperative JOA|, by NDI scores as follows: |postoperative NDI scores−preoperative NDI scores|. The recovery rate (RR) was calculated by JOA as follows: (postoperative JOA−preoperative JOA)/(17−preoperative JOA) × 100% (27), by NDI scores as follows: (postoperative NDI scores−preoperative NDI scores)/(1−preoperative NDI scores) × 100%.
Statistical analysis
Statistical analysis was performed with the Statistical Package for Social Sciences (v.23.0, IBM Statistics, Armonk, NY, United States). All continuous variables were expressed as mean (SD, standard deviation) and compared by analysis of one-way ANOVA test or t test. Categorical variables were expressed as the number of patients with a percentage and compared by χ2 test or Fisher's exact test. In the final analysis, Univariate and multiple linear regression analysis were used to analyze the relationship between BDI and HAMD-24 scores and postoperative outcomes. P < 0.05 was considered statistically significant.
Results
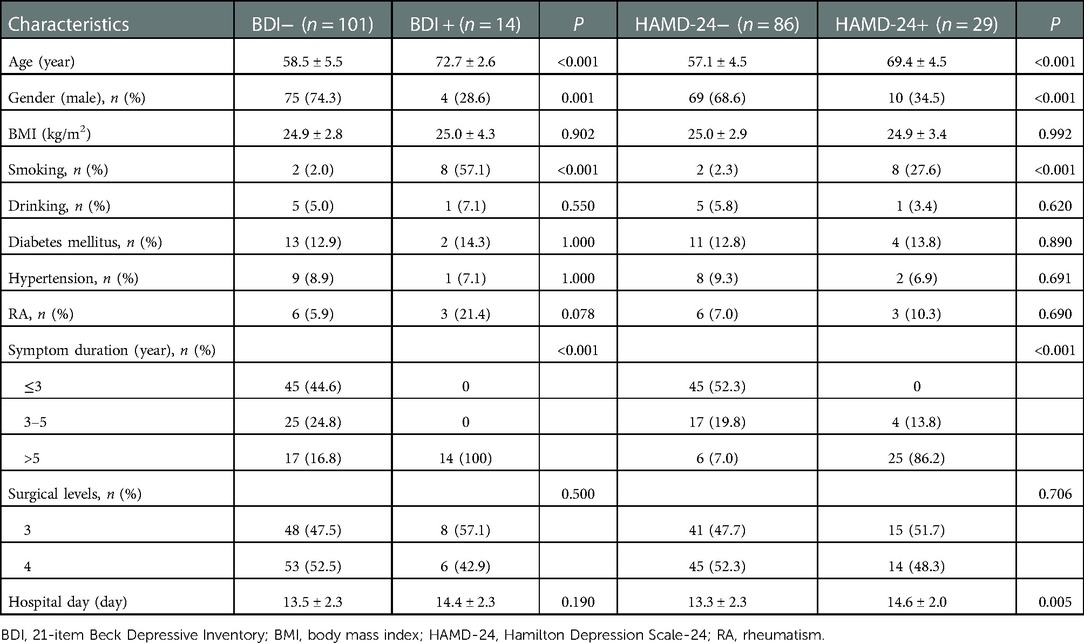
Ultimately, a total of 121 patients underwent laminoplasty were enrolled in this study, but 6 patients were excluded, because 3 patients had surgical site infection and the other 3 had hematoma after surgery. Screened by BDI, the depression group included 14 patients, including 4 males (28.6%), the mean age of patients was 72.7 ± 2.6 years, average BMI was 25.0 ± 4.3, mean hospital stay was 14.4 ± 2.3 days. Meanwhile, 8 smokers (57.1%), 1 drinker (7.1%), 2 with diabetes (14.3%), 1 with hypertension (7.1%), 3 with rheumatism (21.4%), 14 patients with >5 years (100%) of symptoms duration, and 8 with three surgical levels (57.1%), 6 with four surgical levels (42.9%). Screened by HAMD-24, the depression group included 29 people, including 10 males (34.5%), the mean age of patients was 69.4 ± 4.5 years, average BMI was 24.9 ± 3.4, mean hospital stay was 14.6 ± 2.0 days. Meanwhile, 8 smokers (27.6%), 1 drinker (3.4%), 4 with diabetes (13.8%), 2 with hypertension (6.9%), 3 with rheumatism (10.3%), 4 patients with 3–5 years (13.8%), 25 patients with >5 years (86.2%) of symptoms duration, and 15 with three surgical levels (51.7%), 14 with four surgical levels (48.3%). Similarly, patient characteristics in the non-depression group were summarized in the same way. Patients with depression screened by BDI or HAMD undergoing laminoplasty are older in age, higher in smoking proportion and females (P < 0.001), and have a longer duration of symptoms (P < 0.001) (Table 1).
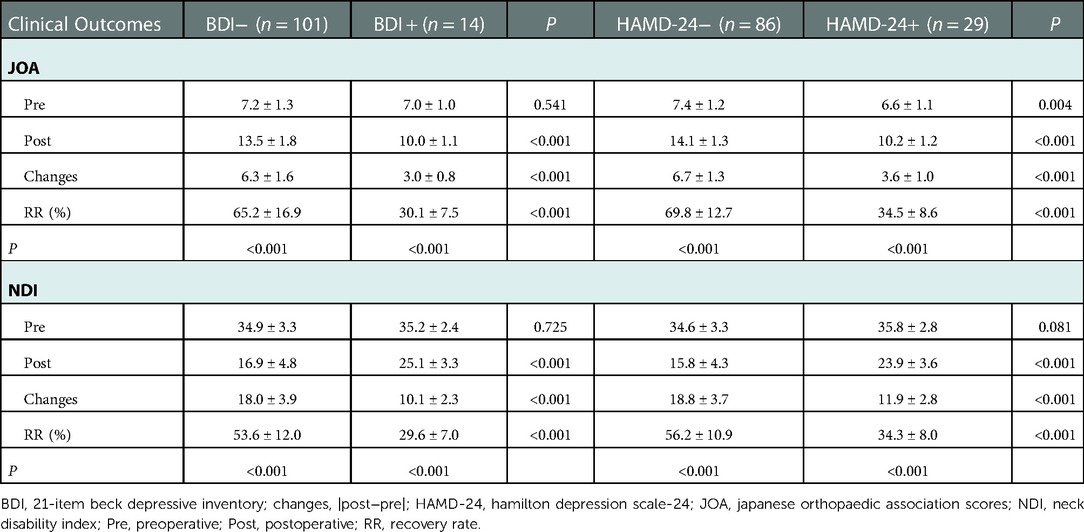
The analysis of postoperative outcomes and improvement showed that there were statistically significance in postoperative JOA, NDI scores and RR between patients with depression and patients without depression in both BDI and HAMD-24 group (P < 0.05). In the BDI group, patients with depression had worse postoperative results, including postoperative JOA (13.5 ± 1.8 vs. 10.0 ± 1.1, P < 0.001), JOA changes (6.3 ± 1.6 vs. 3.0 ± 0.8, P < 0.001), RR (65.2 ± 16.9 vs. 30.1 ± 7.5, P < 0.001), postoperative NDI scores (16.9 ± 4.8 vs. 25.1 ± 3.3, P < 0.001), NDI changes (18.0 ± 3.9 vs. 10.1 ± 2.3, P < 0.001), RR (53.6 ± 12.0 vs. 29.6 ± 7.0, P < 0.001). Similarly, in the HAMD-24 group, patients with depression had worse postoperative results (Table 2).
The results of univariate linear regression analysis showed that the higher the preoperative BDI and HAMD-24 scores, the worse the postoperative clinical outcomes (P < 0.05). After considering confounding factors, multivariate linear regression analysis showed that the BDI scores were recognized as a negative predictor of postoperative JOA (β = 0.171, P = 0.017), JOA changes (β = −0.147, P = 0.020), RR (β = −1.225, P = 0.036), and a negative predictor of postoperative NDI scores (β = 0.472, P = 0.020), NDI changes (β = −0.327, P = 0.010) and RR (β = −0.919, P = 0.027). Besides, HAMD-24 scores were negative predictor of postoperative JOA (β = −0.067, P = 0.030), changes (β = −0.065, P = 0.017) and RR (β = −0.554, P = 0.028) (Table 3).

Table 3. Correlation between preoperative BDI, HAMD-24 and postoperative clinical outcomes and improvement by using regression analysis.
Discussion
Posterior cervical approach is a common surgical method for the treatment of multilevel CSM. Liu et al. (28) indicated that ACDF was recommended when there were no more than three cumulative segments in CSM, but when there are three or more segments involved in the vertebral bodies, laminoplasty should be selected to treat multilevel CSM in order to avoid surgical complications and reoperation related to complications. Some scholars also reported that patients with ACDF and patients with laminoplasty had similar postoperative recovery, but the incidence of reoperation and complications in ACDF group was higher than that in laminoplasty group (29). Similarly, Liu et al. (30) conducted a meta-analysis, contained 11 studies with a total of 712 patients, which showed that patients in the posterior approach group had more postoperative JOA than patients in the anterior approach group. What factors cause the worse effect of posterior cervical surgery?.
Previous studies have shown there are some factors which can affect the curative effect of posterior cervical surgery, such as age (31), gender (32), smoking (33), symptom duration (34) and so on (35). Other studies have confirmed that mental factors affect the results of surgery in heart surgery, brain surgery, transplantation surgery and thoracic surgery (14, 36–40). In spinal surgery, there are some similar studies (41–43). Tuomainen et al. (44) conducted a 10-year prospective study that included a total of 102 patients with lumbar spinal stenosis and found that even patients with mild depressive symptoms had an increased risk of postoperative pain and disability. A retrospective study by Kevin et al. (45) on patients who underwent ACDF found that patients with depressive symptoms postoperatively had a significantly higher Nurick score than patients without depression. At present, there is no study on the relationship between depression and postoperative results of laminoplasty.
Therefore, we conducted this retrospective study where a total of 115 patients were included and followed up for more than 1 year. The result demonstrated that there was a relationship between preoperative depression and postoperative outcomes in patients with multilevel CSM, and patients with depressive symptoms had poorer symptoms improvement after laminoplasty. In addition, BDI and HAMD-24 were used to assess the mental state of patients, which could assess the patient's depressive symptoms more accurately. BDI includes a series of indicators, such as self-evaluation, environment, work, life, future, and so on, to judge depression symptoms, while HAMD evaluates individual depression symptoms through mental, weight, cognitive impairment, block, sleep disturbance, etc. BDI and HAMD cooperate and complement each other, at the same time, BMI can exclude the influence of anxiety disorder included in HAMD on the experimental results.
The baseline data analysis showed that compared with the patients without depression, the patients with depression screened by BDI and HAMD-24 were older in age, higher in female and smoking proportion, and had a longer duration of symptoms. Factors, such as aging of population, socioeconomic status, disability and cognitive impairment, widowhood, might lead to the result that patients with depression have an elder age (19). That Females in depression group are more is related to susceptibility, gender differences, and environmental factors, the conclusion is consistent with other research (46). The reason why there are more smokers in depression group may be related to the fact that smoking behavior and nicotine intake can enhance pleasure in people with lack of pleasure (47, 48). The longer the duration of symptoms, the longer the dysfunction associated with the disease bothers patients, which will lead to the incidence of depression (49, 50). In addition, HAMD-24 had screened more patients with depression than BDI, which might be because HAMD-24 also diagnosed some patients with anxiety symptoms as depression. In this study, the postoperative JOA and NDI scores of all patients were improved compared with those before operation, and the improvement of depressed patients was worse than that of non-depressed patients. Linear regression analysis showed that the higher the preoperative BDI scores, the worse the postoperative outcome, and the higher the preoperative HAMD-24, the worse the postoperative JOA recovery.
The effect of depression on clinical outcomes may be caused by the following factors. Depression is closely related to pain and will affect the prognosis of patients. Studies have shown that one suffering from physical diseases is often accompanied by mental symptoms, and long-term illnesses will increase their psychological burden (51). The main symptoms of multilevel CSM include pain and dysfunction. Long-term pain will seriously affect the patient's psychological mood and the quality of life (52). When the pain reaches moderate to severe, impaired body function and/or is difficult to treat, it has a clear correlation with depressive symptoms (53). In addition, depression can also cause somatization symptoms in patients, including pain, discomfort, neurasthenia, gastrointestinal symptoms, and somatosensory amplification (54, 55). Consequently, when multilevel CSM patients with depression receive a questionnaire after surgery, their pain scores may be relatively higher, leading to worse postoperative results.
Postoperative functional exercise is an important way to determine the prognosis of patients, which is helpful to the recovery of body function and the healing of surgical incision (56). Patients with depression are depressed, lack of confidence to overcome the disease, and resistance to rehabilitation training and exercise, which may lead to worse surgical results. Patients with depression also have different degrees of cognitive impairment, which may lead to a lack of correct and rational understanding of the disease and postoperative treatment, and also lead to worse prognosis (57). In addition, it has been confirmed that individuals with depression have a high level of inflammation marks (58). Depression is related to the changes of neuroendocrine immunity, which will lead to more inflammatory cytokines (59), thus affecting the rehabilitation process.
There are some limitations in this study. First of all, the sample size of the study is relatively small, with only 115 patients included in the study, which may be statistically biased, leading to inaccurate conclusions. Secondly, this is a retrospective study with a few factors included in the analysis. Some factors that have an impact on the clinical outcome may be overlooked, such as the lack of evaluation of the surgical quality, which will also have an important impact on the surgical outcome. Therefore, in order to clarify the relationship between psychological factors and surgical results more clearly, further prospective, multi-center and large-sample studies are needed.
Conclusion
Laminoplasty can alleviate the symptoms of patients with multilevel CSM, but the improvement of symptoms in patients with depression after surgery is relatively worse. In order to improve the curative effect of laminoplasty, we should pay attention to the psychological state monitoring and intervention of patients before they receive laminoplasty.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This research was approved by the ethics committee of the First Affiliated Hospital of Dalian Medical University. This report does not contain any personal information that could lead to the identification of the patient(s) and/or volunteers. This study was performed in accordance with relevant guidelines and regulations and all participants provided written informed consent to participate in the study.
Author contributions
WTZ, Methodology, Formal analysis, Software, Writing - Original draft, Writing - review & editing. TZS, Methodology, Formal analysis, Visualization. SYW, Writing - review & editing, Visualization, Supervision. JZ, Software, Validation, Visualization. MY, Visualization, Project administration, Data curation. ZHL, Conceptualization, Investigation, Writing - review & editing. WTZ, TZS and SYW contributed equally to the manuscript and should be considered co-first authors. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Science and Technology Innovation Foundation of Dalian (2022JJ12SN045), the Natural Science Foundation of Liaoning Province (2022-MS-322) and the open project of Key Laboratory for Micro/Nano Technology and System of Liaoning Province, Dalian University of Technology (20210101). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Acknowledgments
We would like to thank all the participants in the studies. The authors would like to thank YW for advice on the statistical analyses.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ACCF, anterior cervical subtotal corpectomy and fusion; ACDF, anterior cervical discectomy and fusion; BDI, 21-item Beck Depression Inventory; BMI, body mass index; CSM, cervical spondylotic myelopathy; DMI, depression in the medically ill; HAMD-24, hamilton depression scale-24; JOA, japanese orthopaedic association scores; NDI, neck disability index; RA, rheumatism; RR, recovery rate.
References
1. Li Z, Huang J, Zhang Z, Li F, Hou T, Hou S. A comparison of multilevel anterior cervical discectomy and corpectomy in patients with 4-level cervical spondylotic myelopathy: a Minimum 2-year follow-up study: multilevel anterior cervical discectomy. Clin Spine Surg. (2017) 30(5):E540–6. doi: 10.1097/BSD.0000000000000212
2. Mummaneni PV, Kaiser MG, Matz PG, Anderson PA, Groff MW, Heary RF, et al. Cervical surgical techniques for the treatment of cervical spondylotic myelopathy. J Neurosurg Spine. (2009) 11(2):130–41. doi: 10.3171/2009.3.SPINE08728
3. Li Z, Zhao Y, Tang J, Ren D, Guo J, Wang H, et al. A comparison of a new zero-profile, stand-alone fidji cervical cage and anterior cervical plate for single and multilevel ACDF: a minimum 2-year follow-up study. Eur Spine J. (2017) 26(4):1129–39. doi: 10.1007/s00586-016-4739-2
4. de Dios E, Heary RF, Lindhagen L, MacDowall A. Laminectomy alone versus laminectomy with fusion for degenerative cervical myelopathy: a long-term study of a national cohort. Eur Spine J. (2022) 31(2):334–45. doi: 10.1007/s00586-021-07067-w
5. Bakhsheshian J, Mehta VA, Liu JC. Current diagnosis and management of cervical spondylotic myelopathy. Global Spine J. (2017) 7(6):572–86. doi: 10.1177/2192568217699208
6. Li Z, Wang H, Tang J, Ren D, Li L, Hou S, et al. Comparison of three reconstructive techniques in the surgical management of patients with four-level cervical spondylotic myelopathy. Spine (Phila Pa 1976). (2017) 42(10):E575–83. doi: 10.1097/BRS.0000000000001907
7. Li Z, Liu H, Yang M, Zhang W. A biomechanical analysis of four anterior cervical techniques to treating multilevel cervical spondylotic myelopathy: a finite element study. BMC Musculoskelet Disord. (2021) 22(1):278. doi: 10.1186/s12891-021-04150-7
8. Hirabayashi K, Watanabe K, Wakano K, Suzuki N, Satomi K, Ishii Y. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine (Phila Pa 1976). (1983) 8(7):693–9. doi: 10.1097/00007632-198310000-00003
9. Xu D, Zhou C, Tao H, Zhu K, Wang C, Peng C, et al. Relationship between hinge fracture and postoperative axial symptoms after cervical laminoplasty. Br J Neurosurg. (2022):1–6. doi: 10.1080/02688697.2021.1923647
10. Li X, Yu H, Welle K, Gathen M, Zhang L, Xiao J, et al. Comparative effectiveness and safety of open-door laminoplasty, French-door laminoplasty, laminectomy and fusion, and laminectomy alone for multilevel degenerative cervical myelopathy: a Bayesian network analysis. Adv Ther. (2022) 39(1):117–39. doi: 10.1007/s12325-021-01980-8
11. Chen G, Liu X, Chen N, Chen B, Zou X, Wei F, et al. Ten-Year surgical outcomes and prognostic factors for French-door laminoplasty in the treatment of multilevel cervical spondylotic myelopathy. Biomed Res Int. (2020) 2020:3627071. doi: 10.1155/2020/3627071
12. Abudouaini H, Liu H, Wang B, Meng Y, Yang Y, Ding C, et al. Outcome and predictive factors in rapid progressive cervical spondylotic myelopathy: a retrospective case-control study. Clin Neurol Neurosurg. (2020) 198:106226. doi: 10.1016/j.clineuro.2020.106226
13. Wang LF, Zhang YZ, Shen Y, Su YL, Xu JX, Ding WY, et al. Using the T2-weighted magnetic resonance imaging signal intensity ratio and clinical manifestations to assess the prognosis of patients with cervical ossification of the posterior longitudinal ligament. J Neurosurg Spine. (2010) 13(3):319–23. doi: 10.3171/2010.3.SPINE09887
14. Levett DZH, Grimmett C. Psychological factors, prehabilitation and surgical outcomes: evidence and future directions. Anaesthesia. (2019) 74(Suppl 1):36–42. doi: 10.1111/anae.14507
15. Kurosu K, Oe S, Hasegawa T, Shimizu S, Yoshida G, Kobayashi S, et al. Preoperative prognostic nutritional index as a predictive factor for medical complication after cervical posterior decompression surgery: a multicenter study. J Orthop Surg (Hong Kong). (2021) 29(1):23094990211006869. doi: 10.1177/23094990211006869
16. Ren L, Lin H, Xu B, Zhang S, Yang L, Sun S. Depression detection on reddit with an emotion-based attention network: algorithm development and validation. JMIR Med Inform. (2021) 9(7):e28754. doi: 10.2196/28754
17. Malhi GS, Mann JJ. Depression. Lancet. (2018) 392(10161):2299–312. doi: 10.1016/S0140-6736(18)31948-2
18. Zinbarg RE, Williams AL, Mineka S. A current learning theory approach to the etiology and course of anxiety and related disorders. Annu Rev Clin Psychol. (2022) 18:233–58. doi: 10.1146/annurev-clinpsy-072220-021010
19. Alexopoulos GS. Depression in the elderly. Lancet. (2005) 365(9475):1961–70. doi: 10.1016/S0140-6736(05)66665-2
20. Zong Y, Xue Y, Zhao Y, Ding H, He D, Li Z, et al. Depression contributed an unsatisfactory surgery outcome among the posterior decompression of the cervical spondylotic myelopathy patients: a prospective clinical study. Neurol Sci. (2014) 35(9):1373–9. doi: 10.1007/s10072-014-1714-8
21. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. (1961) 4:561–71. doi: 10.1001/archpsyc.1961.01710120031004
22. Schwab JJ, Bialow MR, Clemmons RS, Holzer CE. Hamilton Rating scale for depression with medical in-patients. Br J Psychiatry. (1967) 113(494):83–8. doi: 10.1192/bjp.113.494.83
23. Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. Jama. (1999) 282(18):1737–44. doi: 10.1001/jama.282.18.1737
24. Parker G, Hilton T, Bains J, Hadzi-Pavlovic D. Cognitive-based measures screening for depression in the medically ill: the DMI-10 and the DMI-18. Acta Psychiatr Scand. (2002) 105(6):419–26. doi: 10.1034/j.1600-0447.2002.01248.x
25. Wang YP, Gorenstein C. Assessment of depression in medical patients: a systematic review of the utility of the beck depression inventory-II. Clinics (Sao Paulo). (2013) 68(9):1274–87. doi: 10.6061/clinics/2013(09)15
26. Zhou Z, Ni HJ, Zhao W, Gu GF, Chen J, Zhu YJ, et al. Percutaneous endoscopic lumbar discectomy via transforaminal approach combined with interlaminar approach for L4/5 and L5/S1 two-level disc herniation. Orthop Surg. (2021) 13(3):979–88. doi: 10.1111/os.12862
27. Hirabayashi K, Miyakawa J, Satomi K, Maruyama T, Wakano K. Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine (Phila Pa 1976). (1981) 6(4):354–64. doi: 10.1097/00007632-198107000-00005
28. Liu X, Min S, Zhang H, Zhou Z, Wang H, Jin A. Anterior corpectomy versus posterior laminoplasty for multilevel cervical myelopathy: a systematic review and meta-analysis. Eur Spine J. (2014) 23(2):362–72. doi: 10.1007/s00586-013-3043-7
29. Hirai T, Yoshii T, Sakai K, Inose H, Yamada T, Kato T, et al. Long-term results of a prospective study of anterior decompression with fusion and posterior decompression with laminoplasty for treatment of cervical spondylotic myelopathy. J Orthop Sci. (2018) 23(1):32–8. doi: 10.1016/j.jos.2017.07.012
30. Liu X, Wang H, Zhou Z, Jin A. Anterior decompression and fusion versus posterior laminoplasty for multilevel cervical compressive myelopathy. Orthopedics. (2014) 37(2):e117–122. doi: 10.3928/01477447-20140124-12
31. Maeno T, Okuda S, Yamashita T, Matsumoto T, Yamasaki R, Oda T, et al. Age-related surgical outcomes of laminoplasty for cervical spondylotic myelopathy. Global Spine J. (2015) 5(2):118–23. doi: 10.1055/s-0034-1396759
32. Toci GR, Lambrechts MJ, Karamian BA, Mao J, Heinle J, Bhatt S, et al. Depression increases posterior cervical decompression and fusion revision rates and diminishes neck disability Index improvement. Spine (Phila Pa 1976). (2022) 47(18):1287–94. doi: 10.1097/BRS.0000000000004371
33. Zheng LM, Zhang ZW, Wang W, Li Y, Wen F. Relationship between smoking and postoperative complications of cervical spine surgery: a systematic review and meta-analysis. Sci Rep. (2022) 12(1):9172. doi: 10.1038/s41598-022-13198-x
34. Takeshima Y, Matsuoka R, Nakagawa I, Nishimura F, Nakase H. Surgical outcome of laminoplasty for cervical spondylotic myelopathy in an elderly population - potentiality for effective early surgical intervention: a meta-analysis. Neurol Med Chir (Tokyo). (2017) 57(7):366–73. doi: 10.2176/nmc.ra.2016-0302
35. Doi T, Nakamoto H, Nakajima K, Hirai S, Sato Y, Kato S, et al. Effect of depression and anxiety on health-related quality of life outcomes and patient satisfaction after surgery for cervical compressive myelopathy. J Neurosurg Spine. (2019):1–8. doi: 10.3171/2019.6.SPINE19569. [Epub ahead of print]31518976
36. Ghoneim MM, O'Hara MW. Depression and postoperative complications: an overview. BMC Surg. (2016) 16:5. doi: 10.1186/s12893-016-0120-y
37. Stenman M, Holzmann MJ, Sartipy U. Association between preoperative depression and long-term survival following coronary artery bypass surgery - A systematic review and meta-analysis. Int J Cardiol. (2016) 222:462–6. doi: 10.1016/j.ijcard.2016.07.216
38. El-Jawahri A, Chen YB, Brazauskas R, He N, Lee SJ, Knight JM, et al. Impact of pre-transplant depression on outcomes of allogeneic and autologous hematopoietic stem cell transplantation. Cancer. (2017) 123(10):1828–38. doi: 10.1002/cncr.30546
39. Rumalla K, Lin M, Orloff E, Ding L, Zada G, Mack W, et al. Effect of comorbid depression on surgical outcomes after craniotomy for malignant brain tumors: a nationwide readmission database analysis. World Neurosurg. (2020) 142:e458–73. doi: 10.1016/j.wneu.2020.07.048
40. Kitagawa R, Yasui-Furukori N, Tsushima T, Kaneko S, Fukuda I. Depression increases the length of hospitalization for patients undergoing thoracic surgery: a preliminary study. Psychosomatics. (2011) 52(5):428–32. doi: 10.1016/j.psym.2011.03.010
41. Tuck AN, Scribani MB, Grainger SD, Johns CA, Knight RQ. The 9-item patient health questionnaire (PHQ-9): an aid to assessment of patient-reported functional outcomes after spinal surgery. Spine J. (2018) 18(8):1398–405. doi: 10.1016/j.spinee.2018.01.004
42. Merrill RK, Zebala LP, Peters C, Qureshi SA, McAnany SJ. Impact of depression on patient-reported outcome measures after lumbar spine decompression. Spine (Phila Pa 1976). (2018) 43(6):434–9. doi: 10.1097/BRS.0000000000002329
43. Pakarinen M, Vanhanen S, Sinikallio S, Aalto T, Lehto SM, Airaksinen O, et al. Depressive burden is associated with a poorer surgical outcome among lumbar spinal stenosis patients: a 5-year follow-up study. Spine J. (2014) 14(10):2392–6. doi: 10.1016/j.spinee.2014.01.047
44. Tuomainen I, Pakarinen M, Aalto T, Sinikallio S, Kröger H, Viinamäki H, et al. Depression is associated with the long-term outcome of lumbar spinal stenosis surgery: a 10-year follow-up study. Spine J. (2018) 18(3):458–63. doi: 10.1016/j.spinee.2017.08.228
45. Phan K, Moran D, Kostowski T, Xu R, Goodwin R, Elder B, et al. Relationship between depression and clinical outcome following anterior cervical discectomy and fusion. J Spine Surg. (2017) 3(2):133–40. doi: 10.21037/jss.2017.05.02
46. Kuehner C. Why is depression more common among women than among men? Lancet Psychiatry. (2017) 4(2):146–58. doi: 10.1016/S2215-0366(16)30263-2
47. Mathew AR, Hogarth L, Leventhal AM, Cook JW, Hitsman B. Cigarette smoking and depression comorbidity: systematic review and proposed theoretical model. Addiction. (2017) 112(3):401–12. doi: 10.1111/add.13604
48. Rubin LF, Haaga DAF, Pearson JL, Gunthert KC. Depression as a moderator of the prospective relationship between mood and smoking. Health Psychol. (2020) 39(2):99–106. doi: 10.1037/hea0000816
49. Chen Z, Luo R, Yang Y, Xiang Z. The prevalence of depression in degenerative spine disease patients: a systematic review and meta-analysis. Eur Spine J. (2021) 30(12):3417–27. doi: 10.1007/s00586-021-06977-z
50. Sinikallio S, Aalto T, Koivumaa-Honkanen H, Airaksinen O, Herno A, Kröger H, et al. Life dissatisfaction is associated with a poorer surgery outcome and depression among lumbar spinal stenosis patients: a 2-year prospective study. Eur Spine J. (2009) 18(8):1187–93. doi: 10.1007/s00586-009-0955-3
51. Rees L. The physical constitution and mental illness. Eugen Rev. (1947) 39(2):50–5. PMID: 20260951
52. Pereira MG, Carvalho C, Costa ECV, Leite Â, Almeida V. Quality of life in chronic pain patients: illness- and wellness-focused coping as moderators. Psych J. (2021) 10(2):283–94. doi: 10.1002/pchj.410
53. Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med. (2003) 163(20):2433–45. doi: 10.1001/archinte.163.20.2433
54. Duddu V, Isaac MK, Chaturvedi SK. Somatization, somatosensory amplification, attribution styles and illness behaviour: a review. Int Rev Psychiatry. (2006) 18(1):25–33. doi: 10.1080/09540260500466790
55. Lipowski ZJ. Somatization and depression. Psychosomatics. (1990) 31(1):13–21. doi: 10.1016/S0033-3182(90)72212-8
56. Ozkara GO, Ozgen M, Ozkara E, Armagan O, Arslantas A, Atasoy MA. Effectiveness of physical therapy and rehabilitation programs starting immediately after lumbar disc surgery. Turk Neurosurg. (2015) 25(3):372–9. doi: 10.5137/1019-5149.JTN.8440-13.0
57. Culpepper L, Lam RW, McIntyre RS. Cognitive impairment in patients with depression: awareness, assessment, and management. J Clin Psychiatry. (2017) 78(9):1383–94. doi: 10.4088/JCP.tk16043ah5c
58. Kohler O, Krogh J, Mors O, Benros ME. Inflammation in depression and the potential for anti-inflammatory treatment. Curr Neuropharmacol. (2016) 14(7):732–42. doi: 10.2174/1570159X14666151208113700
Keywords: cervical spondylotic myelopathy (CSM), laminoplasty, depression, clinical outcomes, 21-item beck depression inventory (BDI), Hamilton depression scale-24 (HAMD-24)
Citation: Zhang W, Sun T, Wang S, Zhang J, Yang M and Li Z (2023) Influence of preoperative depression on clinical outcomes after cervical laminoplasty: A retrospective study. Front. Surg. 9:1098043. doi: 10.3389/fsurg.2022.1098043
Received: 14 November 2022; Accepted: 14 December 2022;
Published: 9 January 2023.
Edited by:
Fang Fang Yu, College of Public Health, Zhengzhou University, China© 2023 Zhang, Sun, Wang, Zhang, Yang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhonghai Li bGl6aG9uZ2hhaXNwaW5lQDEyNi5jb20=
†These authors have contributed equally to this work and share first authorship
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Wentao Zhang1,2,†
Wentao Zhang1,2,† Tianze Sun
Tianze Sun Jing Zhang
Jing Zhang Ming Yang
Ming Yang Zhonghai Li
Zhonghai Li