- 1Department of Oral and Maxillofacial Surgery, Nanjing Stomatological Hospital, Medical School of Nanjing University, Nanjing, China
- 2Department of Oral Anesthesiology, Nanjing Stomatological Hospital, Medical School of Nanjing University, Nanjing, China
Purpose: The study aims to compare the velopharyngeal morphology of hard and soft cleft palate (HSCP) patients after Furlow and Sommerlad palatoplasty.
Patients and methods: A total of 51 patients (20 cases in Furlow palatoplasty group, 16 cases in Sommerlad palatoplasty group and 15 normal children in the control group) were included in our study. Velopharyngeal function and speech outcomes of patients with HSCP who had either Furlow palatoplasty or Sommerlad palatoplasty for cleft palate repair were evaluated by perceptual speech assessment (PSA), lateral cephalometric radiographs and nasopharyngoscopy. To assess velopharyngeal morphology of patients treated with two techqiques, we analyzed measurements such as velar length, pharyngeal depth, and the Adequate ratio (the ratio of velar length to pharyngeal depth). Furthermore, skeletal landmarks including cranial base, cervical vertebrae, posterior nasal spine which were defined as the pharyngeal triangle were measured. Finally, the position of the point U relative to the pharyngeal triangle were compared.
Results: Velopharyngeal closure (VPC) rate in Furlow palatoplasty group accounted for 90%, while that in Sommerlad palatoplasty group was 81.3%. PSA of the former group was significantly better than that of the latter group (P < 0.05). Velar length, pharyngeal depth and the Adequate ratio (1.37 ± 0.14 vs. 1.41 ± 0.15) were comparable between the Furlow group and control group (P > 0.05), while Sommerlad group had a shorter velar length, deeper pharyngeal depth and a smaller Adequate ratio (1.20 ± 0.18) compared to the above two groups (P < 0.05). Furhermore, the point U of Sommerlad group in the pharyngeal triangle was higher than that of the other two groups.
Conclusions: In the treatment modality of patients with HSCP, both Furlow palatoplasty and Sommerlad palatoplasty seem to be effective. Furlow palatoplasty appears to have velopharyngeal morphology similar to normal control group., while Sommerlad group shows a shorter velar length, deeper pharyngeal depth and a smaller Adequate ratio
Introduction
Cleft palate is the most common congenital developmental deformity of the maxillofacial region, the incidence of it lies on top of congenital birth defect diseases (1–3). It exerts a serious socio-economic and psychosocial burden on patients and their families (4–6). Currently, surgical intervention has still emerged as the first treatment choice. Although various techniques have been described for cleft palate repair, however, there is no consensus on the ideal palatal repair technique applicable to all cleft palate types (7–10). The primary goal of cleft palate repair is the achievement of optimal speech outcomes (11, 12). To accomplish this goal, anatomical separation between the oral and nasal cavities and restoration of the muscular sling in the soft palate is pivotal (13). Furlow palatoplasty proposed by Furlow in 1986, and Sommerlad palatoplasty described by Sommerlad in 2002 were currently two popular methods to achieve VPC and yield intelligible speech by means of anatomical reconstruction of the levator palatine muscle (14, 15). Whereas the way restoring abnormally attached muscles was different. The former was by means of dissection and reposition of the levator veli palatini, while the latter was achieved with the help of the double-opposing Z-plasty. Previously, several studies had evaluated the clinical outcomes of these two surgical procedures (16–20). Khosla et al. reported Furlow Z-plasty yielded excellent speech results for primary cleft palate repair, and the rate of VPC reached 84% (16). According to Wang et al., 80% patients with Sommerlad palatoplasty had no evidence of velopharyngeal insufficiency (18). In addition, Li et al. compared the incidence of postoperative fistula formation of the above two techniques and found that the fistula rate of Furlow palatoplasty is lower than that of Sommerlad palatoplasty (19). However, few research have been conducted to compare the velopharyngeal morphology between Furlow and Sommerlad techniques. If any, they were assessed only using subjective evaluation methods (18). Thus, the current study aims to compare velopharyngeal morphology and speech outcomes using subjective and objective parameters after cleft palate repair with Furlow or Sommerlad palatoplasty, to provide clinical evidence for a better choice of surgical methods to reconstruct a functional velopharyngeal unit and restore optimal speech in patients with HSCP.
Materials and methods
Subjects
Medical records of patients with HSCP who underwent primary cleft palate repair in Nanjing Stomatological Hospital, Medical School of Nanjing University between 2012 and 2018 were reviewed retrospectively. All patients enrolled in the study met the following inclusion criteria: patients with HSCP; non-syndromic patients; and primary cleft palate repair using Furlow or Sommerlad palatoplasty. Patients were excluded for syndromic diseases, and for a history of delayed language development and dysacusia.
This study was approved by the Ethics Committee, Nanjing Stomatological Hospital, Medical School of Nanjing University.
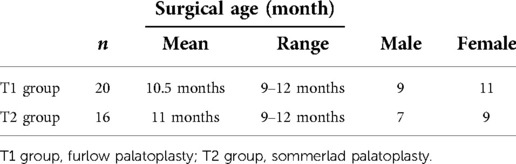
Patients with HSCP underwent surgical repair by Furlow or Sommerlad palatoplasty. Their ages performing surgical procedures ranged from 9 months to 12 months. The mean age at follow-up was similar between groups. Patients were randomly assigned to Furlow palatoplasty group (n = 20, 9 males and 11females) and Sommerlad palatoplasty group (n = 16, 7 males and 9 females). Surgical procedures were performed by two senior surgeons, respectively (14, 15). Fifteen healthy children (good articulation, no hearing handicap, no cleft lip or cleft palate, no congenital maxillofacial developmental malformations, no orthodontic treatment history) were selected as the control group. Details were provided in Table 1.
Perceptual speech assessment
Speech evaluation was evaluated by two experienced speech pathologists using a speech articulation test table (21). Patients were asked to read a standard list of 63 phrases that cover all phonemes and most common phonetic combinations in Mandarin Chinese, and 20 short sentences containing voiced and unvoiced pressure consonants, no-pressure consonants, and a mixture of nasal consonants. The next part of the test was a casual conversation between the participants and the speech pathologist, in which speech intelligibility, hypernasality and nasal emission were measured. These parameters were evaluated following the scoring guidelines and definitions of the CAPS-A protocol (22). Intelligibility and hypernasality were evaluated using a five-point scale, whereas for the evaluation of nasal emission a three-point scale was used. Interrater and intrarater reliabilities were investigated using weighted kappa statistics to assess observer variability. Each speech language pathologist rated speech after listening to 20 recorded speech samples and the ratings were compared to determine agreement between the two raters. The ratings were made twice with an interval of one week by each rater and two ratings by the same rater were compared.
Nasoendoscopy
Nasoendoscopy was performed for patients diagnosed with hypernasality or nasal emission that were cooperative, usually over the age of 4 years. Nasoendoscopy was used to observe the motility of the velum and posterior pharyngeal wall and lateral pharyngeal wall of patients with VPI. The results were diagnosed as VPC and VPI.
Lateral cephalometric assessments
Set points (Figure 1): ANS, anterior nasal spine; PNS, posterior nasal spine; PPW, posterior pharyngeal wall; N, nasion; S, center of the sella turcica; PCB, pterygoid cranial base; AA, atlas; U, uvula, tip of the uvula when at rest.
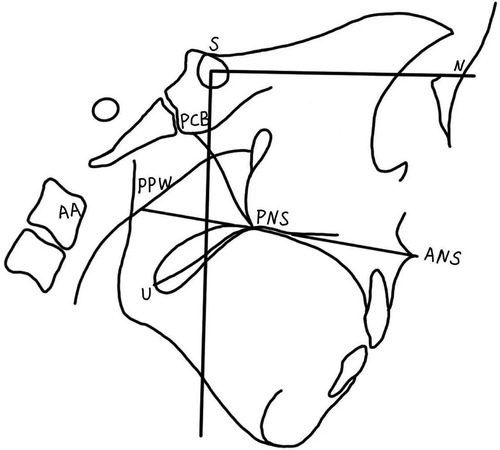
Figure 1. Cephalometric landmarks and velopharyngeal measures. ANS, anterior nasal spine; PNS, posterior nasal spine; PPW, posterior pharyngeal wall; N, nasion; S, center of the sella turcica; PCB, pterygoid cranial base; AA, atlas; U, uvula, tip of the uvula when at rest.
Measurement methods: To eliminate the interference of age and sex among the 3 groups, all craniopharyngeal dimensions were standardized according to the anterior cranial base length (S–N) with a given value of 100 (S–N revision). Measurements derived from tracing of lateral cephalograms by drawing the sella nasion (S–N) plane as the x-axis and projecting a perpendicular line to this plane through the point S as the y-axis. The length of the velar PNS-U, the depth of the nasopharynx PNS-PPW and the length of the hard palate ANS-PNX (Figure 1) were measured, and the adequate ratio (velar length to pharyngeal depth ratio) was calculated. For the three groups, ANS, PNS, PCB, AA, U, PPW were marked in the coordinates according to their (x, y) values. To facilitate the comparison of velopharyngeal morphology among the 3 groups, the triangle connecting PNS, PCB, and AA was defined as the pharyngeal triangle (Figure 2). Each measurement was performed twice by the first author, and the mean value was recorded.
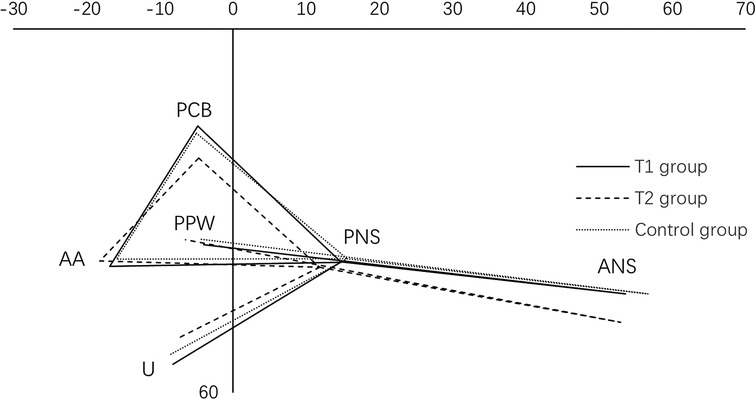
Figure 2. Velopharyngeal morphology of three groups. ANS, anterior nasal spine; PNS, posterior nasal spine; PPW, posterior pharyngeal wall; N, nasion; S, center of the sella turcica; PCB, pterygoid cranial base; AA, atlas; U, uvula, tip of the uvula when at rest.
Statistical analysis
The Wilcoxon rank sum test was used to compare the speech outcomes. The results of cephalometric measurements of the three groups were subscribed to one-way ANOVA using IBM SPSS (version 26.0). Differences with P < 0.05 were considered statistically significant.
Results
Speech outcomes
The kappa values for interrater reliability were 0.67, and for intrarater reliability were 0.72 and 0.68, indicating substantial agreement. The results of PSA were shown in Table 3. The speech intelligibility in Furlow group was significantly better than that in Sommerlad palatoplasty (P = 0.023). Furlow palatoplasty's hypernasality improved better than Sommerlad palatoplasty (P = 0.009). Postoperative nasal emissions differed significantly between the two groups (P = 0.016) (Table 2).
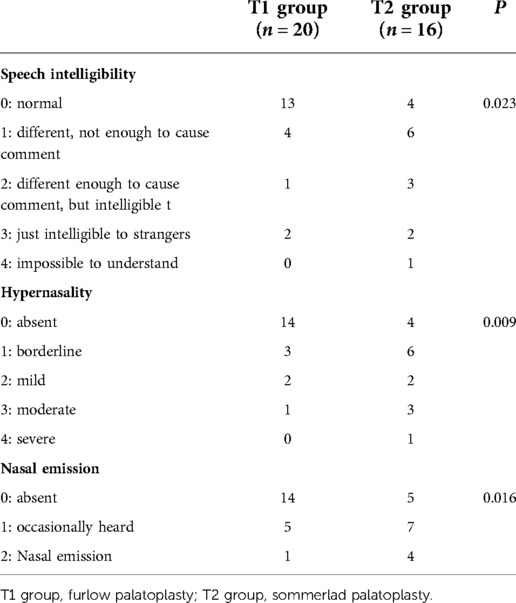
Table 2. Comparative analysis of speech intelligibility, hypernasality and nasal emission in furlow and sommerlad palatoplasty groups.
Nasoendoscopy
3 patients of T1 group and 4 patients of T2 group were recommended to perform nasoendoscopy. There were 2(20) and 3(16) patients who were diagnosed with having VPI, respectively. Eventually, the rate of VPC in T1 group (90%) was higher than that in T2 group (81.3%).
Lateral cephalogram evaluation
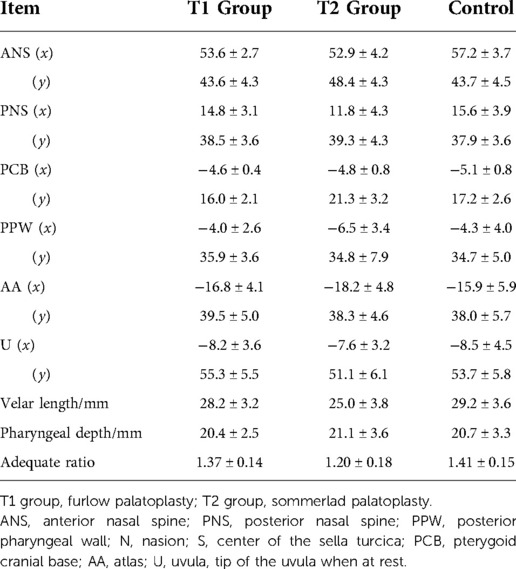
The interclass correlation coefficient results for the test-retest reliability ranged between 0.72 and 0.83 (P < 0.05), suggesting dependable reliability and reproducibility of the adopted measuring strategy. The results of cephalometric measurements for the velopharyngeal structure of the three groups were presented in Table 3. There was no significant difference in the coordinates of points PNS, PCB, and AA on either axis among the 3 groups (P > 0.05). The velar length and Adequate ratio of T1 group was similar to that of the normal group (P > 0.05). The velopharyngeal structure was also similar to that of the control group. The velopharyngeal depths of the three groups were similar (P > 0.05). Velar length and adequate ratio were significantly smaller in T2 group than in the other two groups (P < 0.05). Adequate ratio averaged more than 1.3 in T1 group and control group. The point U of T2 group in the pharyngeal triangle was above that of the other two groups. The coordinate of point ANS on the x-axis in the T1 and T2 group was inferior to that in the control group (P < 0.05).
Discussion
The main objective of cleft palate repair is to reconstruct proper velopharyngeal function for normal speech intelligibility (19), which requires restoration of an anatomically well-integrated dynamic and functional soft palate. Furlow and Sommerlad methods are two well-established methods to optimize velopharyngeal function by restoring the velar muscular sling (14, 15). Numerous studies applied these two techniques to cleft repair and evaluated the postoperative outcomes respectively. However, limited studies performed a definitive comparison of velopharyngeal morphology between them. Herein, the comparisons were made between the two techniques in several methods, revealing that better speech outcome was produced in Furlow palatoplasty as opposed to Sommerlad palatoplasty.
VPC is the premise to yield adequate speech intelligibility. It was reported that 5% to 30% of patients have unsatisfactory speech outcomes and require secondary treatment because of velopharyngeal insufficiency (VPI) after primary palatoplasty (23–34), which may be related to several risk factors, including short velar length, insufficient velopharyngeal motility and deep palatopharyngeal cavity (26). Consistent with previous studies, our data suggested that the VPC rate was 90% in Furlow palatoplasty group vs. 81.3% in Sommerlad palatoplasty group. Furthermore, poorer speech intelligibility, higher hypernasality and nasal emissions were displayed in our study. This difference between these two methods is possibly due to the surgical characteristics that exert influence on the outcome of the operation. Both the Sommerlad and Furlow techniques repositioned the displaced levator veli palatini, contributing to develop a functional velum. Sommerlad palatoplasty focused more on anatomical reconstruction of the abnormal levater veli palatine and enhancement of muscular function, while the extension of the soft palate length is limited, which influences the outcome of palatopharynx closure. Nevertheless, Furlow palatoplasty not only restored the velar muscular sling to proper orientation but also elongated the velar length reducing the risk of longitudinal scar contracture. Consequently, the Furlow repair has a stronger ability to extend the soft palate length than sommerlad palatoplasty (18). After 289 patients with cleft palate repaired by Furlow palatoplasty, Chorney et al. (27) found only 5% of the patients needed secondary surgery as a result of VPI. And Wang et al. reported the length of soft palate increased by 13.23%, 10.10% after Furlow and Sommerlad palatoplasty, respectively (18). In line with these results, lateral cephalogram evaluation revealed a significantly increased soft palate length and higher adequate ratio after Furlow palatoplasty compared with Sommerlad palatoplasty, while there were no significantly differences in velopharyngeal depth between them.
Vlopharyngeal function assessment in previous studies depended largely on perceptual examination (8, 28, 29), which existed with the defect of significant heterogeneity and prevented comparison of results from different centers. Several methods have been developed to assess and describe velopharyngeal function and speech outcome, including electromyogram and nasopharyngeal endoscopy, but none of the existing methods can assess all indexes independently (30–34). To ensure a more reliable and accurate evaluation of velopharyngeal function and speech results in cleft patients, various evaluation methods were applied simultaneously in our study. Apart from perceptual assessment, 2-dimensional cephalometric studies provide a static evaluation of the velopharynx, while nasopharyngeal endoscopy can record and immediately replay velopharyngeal closure. Nasoendoscopy played a critical role in determining VPI, especially marginal VPI, which perceptual speech evaluation was in doubt. Therefore, jointly applying these methods can provide compelling data that can be made through comparison and analysis between different centers.
Of course, this present study exists certain limitations that should be acknowledged.
A notable shortcoming of our research is the insufficient sample size. Further data collection is required. Besides the surgical technique, for the lack of standardization of variables such as cleft width and hard palate repair technique, further analyses based on the above variables will be conducted in future research. The present study revealed that Sommerlad technique yielded worse velopharyngeal function and speech outcomes compared to Furlow technique. For HSCP patients, relative to Sommerlad palatoplasty, Furlow palatoplasty may be a more suitable surgical option. Of note, the opposing Z-plasty sacrificed velar width to gain length, which is not applicable to all types of clefts, particularly wide clefts due to excessive tension.
Conclusion
Furlow technique was proven to be superior compared to Sommerlad palatoplasty in terms of velopharyngeal function and morphology following primary cleft palate repair, which showed better speech intelligibility, higher VPC rate, longer velar length, shorter pharyngeal depth and a bigger Adequate ratio. Based on the above results, the Furlow palatoplasty should be preferred for patients with HSCP.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by This study was approved by the Ethics Committee, Nanjing Stomatological Hospital, Medical School of Nanjing University. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
YL, YCD conceived and designed the research studies. XFF, WLL, JCN and XXC performed data collection and analysis; YL, YCD critically revised the manuscript. XFF, WLL and JCN wrote the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Dixon MJ, Marazita ML, Beaty TH, Murray JC. Cleft lip and palate: understanding genetic and environmental influences. Nat Rev Genet. (2011) 12:167–78. doi: 10.1038/nrg2933
2. JC M AJ. Orofacial clefting recent insights into a complex trait. Curr Opin Genet Dev. (2005) 15:270–8. doi: 10.1016/j.gde.2005.03.003
3. Eppley BL, van Aalst JA, Robey A, Havlik RJ, Sadove AM. The spectrum of orofacial clefting. Plast Reconstr Surg. (2005) 115:101e–114. doi: 10.1097/01.prs.0000164494.45986.91
4. Cheng X, Bo Z, Yin H, Yang K, Li J, Shi B. Age and preoperative velar closure ratio are significantly associated with surgical outcome of furlow double-opposing Z-plasty in palatal Re-repair. J Oral Maxillofac Surg. (2020) 78:431–9. doi: 10.1016/j.joms.2019.09.023
5. Wei Y, Zhong T, Yin X, Shi B, Zheng Q, Li J. Dynamic nasolabial growth after primary surgery for patients with bilateral cleft lip: a five-year follow-up study. J Oral Maxillofac Surg. (2019) 77:2125.e2121–2110. doi: 10.1016/j.joms.2019.05.013
6. Xu X, Cao C, Zheng Q, Shi B. The influence of four different treatment protocols on maxillofacial growth in patients with unilateral complete cleft lip, palate, and alveolus. Plast Reconstr Surg. (2019) 144:180–6. doi: 10.1097/prs.0000000000005711
7. Li F, Wang HT, Chen YY, Wu WL, Liu JY, Hao JS. Cleft relapse and oronasal fistula after furlow palatoplasty in infants with cleft palate: incidence and risk factors. Int J Oral Maxillofac Surg. (2017) 46:275–80. doi: 10.1016/j.ijom.2016.09.019
8. Williams WN, Seagle MB, Pegoraro-Krook MI, Souza TV, Garla L, Silva ML Prospective clinical trial comparing outcome measures between furlow and von langenbeck palatoplasties for UCLP. Ann Plast Surg. (2011) 66:154–63. doi: 10.1097/SAP.0b013e3181d60763
9. Sakran KA, Wu M, Alkebsi K, Mashrah MA, Al-Rokhami RK, Wang Y. The sommerlad-furlow modified palatoplasty technique: postoperative complications and implicating factors. Laryngoscope. (2022). doi: 10.1002/lary.30385. [Epub ahead of print]
10. Sakran KA, Yin J, Yang R, Elayah SA, Alkebsi K, Zhang S. Early cleft palate repair by a modified technique without relaxing incisions. Cleft Palate Craniofac J. (2022):10556656221135288. doi: 10.1177/10556656221135288. [Epub ahead of print]36300250
11. Calis M, Ekin O, Kayikci ME, lcen M, Suslu N, Ozgur F. Does contribution of extended vomer flap to palatoplasty affects speech results. J Craniofac Surg. (2014) 25:1980–4. doi: 10.1097/SCS.0000000000001030
12. Prathanee B, Pumnum T, Seepuaham C, Jaiyong P. Five-year speech and language outcomes in children with cleft lip-palate. J Craniomaxillofac Surg. (2016) 44:1553–60. doi: 10.1016/j.jcms.2016.08.004
13. Devani P, Watts R, Markus AF. Speech outcome in children with cleft cleft palate: aerophonoscope assessment of nasal emission. J Craniomaxillofac Surg. (1999) 27:180–6. doi: 10.1016/S1010-5182(99)80048-1
14. Sommerlad BC. A technique for cleft palate repair. Plast Reconstr Surg. (2003) 112:1542–8. doi: 10.1097/01.PRS.0000085599.84458.D2
15. Furlow LT. Cleft palate repair by double opposing Z-plasty. Plast Reconstr Surg. (1986) 78:724–38. doi: 10.1097/00006534-198678060-00002
16. Khosla RK, Mabry K, Castiglione CL. Clinical outcomes of the furlow Z-plasty for primary cleft palate repair. Cleft Palate Craniofac J. (2008) 45:501–10. doi: 10.1597/07-063.1
17. Kara M, Calis M, Kara I, Kayikci ME, Gunaydin RO, Ozgur F. Comparison of speech outcomes using type 2b intravelar veloplasty or furlow double-opposing Z plasty for soft palate repair of patients with unilateral cleft lip and palate. J Craniomaxillofac Surg. (2021) 49:215–22. doi: 10.1016/j.jcms.2021.01.003
18. Wang K, Wang Q, He W, Wang F, Chen S, Zhang N. The effect of Zigzag palatoplasty on the repair of cleft palate and its comparative study with sommerlad palatoplasty and the double opposing Z palatoplasty. J Craniofac Surg. (2020) 31:e717–20. doi: 10.1097/SCS.0000000000006673
19. Li Y, Wu M, Yang C, Tsauo C, Li C, Liu R. Evaluation of fistula rates in three cleft palate techniques without relaxing incisions. J Craniomaxillofac Surg. (2021) 49:456–61. doi: 10.1016/j.jcms.2021.01.022
20. Perkins JA, Lewis CW, Gruss JS, Eblen LE, Sie KC. Furlow palatoplasty for management of velopharyngeal insufficiency: a prospective study of 148 consecutive patients. Plast Reconstr Surg. (2005) 116:72–80; discussion 81–74.doi: 10.1097/01.prs.0000169694.29082.69
21. Qiu Y, Zheng Q, Shi B, Li Y, Wang Y, Yin H. Influential factors affecting the postoperative velopharyngeal function among aged cleft palate patients. Hua Xi Kou Qiang Yi Xue Za Zhi. (2014) 32:54–7. doi: 10.7518/hxkq.2014.01.013
22. John A, Sell D, Sweeney T, Harding-Bell A, Williams A. The cleft audit protocol for speech-augmented: a validated and reliable measure for auditing cleft speech. Cleft Palate Craniofac J. (2006) 43:272–88. doi: 10.1597/04-141.1
23. Nam SM. Surgical treatment of velopharyngeal insufficiency. Arch Craniofac Surg. (2018) 19:163–7. doi: 10.7181/acfs.2018.02082
24. Collins J, Cheung K, Farrokhyar F, Strumas N. Pharyngeal flap versus sphincter pharyngoplasty for the treatment of velopharyngeal insufficiency: a meta-analysis. J Plast Reconstr Aesthet Surg. (2012) 65:864–8. doi: 10.1016/j.bjps.2012.01.020
25. Liu BY, Chen XX, Cao J, Lu Y. Analysis of velopharyngeal function and speech outcomes of sommerlad palatoplasty combined with sphincter pharyngoplasty in surgical repair of older patients with cleft palateexperience from a major craniofacial surgery centre in eastern China. Br J Oral Maxillofac Surg. (2020) 58:819–23. doi: 10.1016/j.bjoms.2020.04.026
26. Nguyen DC, Patel KB, Skolnick GB, Skladman R, Grames LM, Stahl MB. Progressive tightening of the levator veli palatini muscle improves velopharyngeal dysfunction in early outcomes of primary palatoplasty. Plast Reconstr Surg. (2015) 136:131–41. doi: 10.1097/PRS.0000000000001323
27. Chorney SR, Commesso E, Tatum S. Incidence of secondary surgery after modified furlow palatoplasty: a 20-year single-surgeon case series. Otolaryngol Head Neck Surg. (2017) 157:861–6. doi: 10.1177/0194599817703948
28. Dong Y, Dong F, Zhang X, Hao F, Shi P, Ren G. An effect comparison between furlow double opposing Z-plasty and two-flap palatoplasty on velopharyngeal closure. Int J Oral Maxillofac Surg. (2012) 41:604–11. doi: 10.1016/j.ijom.2012.01.010
29. Reddy RR, Gosla Reddy S, Vaidhyanathan A, Bergé SJ, Kuijpers-Jagtman AM. Maxillofacial growth and speech outcome after one-stage or two-stage palatoplasty in unilateral cleft lip and palate. A systematic review. J Craniomaxillofac Surg. (2017) 45:995–1003. doi: 10.1016/j.jcms.2017.03.006
30. Yin H, Ma L, Shi B, Guo C, Zhao S, Li Y. A study on the application of the perceptual assessment in the diagnosis of the velopharyngeal function. Hua Xi Kou Qiang Yi Xue Za Zhi. (2012) 30:197–200. doi: 10.3969/j.issn.1000-1182.2012.02.021
31. Perry JL, Sutton BP, Kuehn DP, Gamage JK. Using MRI for assessing velopharyngeal structures and function. Cleft Palate Craniofac J. (2014) 51:476–85. doi: 10.1597/12-083
32. Kuehn DP, Moon JB. Velopharyngeal closure force and levator veli palatini activation levels in varying phonetic contexts. J Speech Lang Hear Res. (1998) 41:51–62. doi: 10.1044/jslhr.4101.51
33. Huang H, Chen N, Yin H, Skirko JR, Guo C, Ha P, et al. Validation of the Chinese velopharyngeal insufficiency effects on life outcomes instrument. Laryngoscope. (2019) 129:E395–401. doi: 10.1002/lary.27792
Keywords: cleft palate, velopharyngeal function, speech outcome, furlow, sommerlad
Citation: Fan X, Liu W, Nie J, Chen X, Dong Y and Lu Y (2023) Comparison of velopharyngeal morphology of two palatoplasty techniques in patients with hard and soft cleft palate. Front. Surg. 9:1080955. doi: 10.3389/fsurg.2022.1080955
Received: 26 October 2022; Accepted: 21 November 2022;
Published: 6 January 2023.
Edited by:
Hanyao Huang, Sichuan University, ChinaReviewed by:
Wen-lin Xiao, The Affiliated Hospital of Qingdao University, ChinaTingting Lan, Nankai University, China
© 2023 Fan, Liu, Nie, Chen, Dong and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yong Lu Y2xlZnRfc3VyZ2VyeUBzaW5hLmNvbQ== Yingchun Dong ZG9uZ3lpbmdjaHVuQG5qdS5lZHUuY24=
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Pediatric Surgery, a section of the journal Frontiers in Surgery
 Xiaofen Fan
Xiaofen Fan Weilong Liu1,†
Weilong Liu1,† Yong Lu
Yong Lu