- Department of Blood Purification Center, Shengzhou People's Hospital (the First Affiliated Hospital of Zhejiang University Shengzhou Branch), Shengzhou, China
Objective: It is currently unclear if the anastomosis technique impacts the patency of upper arm arteriovenous fistula (AVF) in hemodialysis patients. This review compared outcomes of end-to-side and side-to-side anastomosis for AVF fistula in hemodialysis patients.
Methods: PubMed, CENTRAL, Web of Science, and Embase were searched for all types of studies published between 1st January 2000 to 3rd September 2022. Patency rates at 6, 12 months, maturation time, and complications were compared between ETS and STS groups.
Results: Sixteen studies including six randomized controlled trials (RCTs) were included. Meta-analysis showed no difference in patency rates between ETS and STS group at 6 months (OR: 1.15 95% CI: 0.72, 1.83 I2 = 52% p = 0.56) but better patency with STS at 12 months (OR: 0.63 95% CI: 0.41, 0.95 I2 = 21% p = 0.03). The difference was non-significant in a subgroup analysis of RCTs and non-RCTs. In the absence of distal vein ligation in the STS group, the ETS group had significantly better patency at 6 months but with distal vein ligation, STS had higher patency at 12 months. Meta-analysis demonstrated no difference in maturation time between the two groups (MD: 0.10 95% CI: 0.29, 0.49 I2 = 89% p = 0.61). Only a descriptive analysis of complications could be carried out with no major difference.
Conclusion: Our review demonstrates that the STS anastomosis technique with distal vein ligation may result in significantly better patency rates as compared to the standard ETS technique. Data for complication rates are scarce and varied but without any significant differences between the two techniques.
Introduction
Chronic kidney disease is a major healthcare problem affecting most parts of the world. Estimates suggest that around 13% of the global population suffers from chronic kidney disease while around 4.9–7.1 million individuals are with end-stage renal disease (ESRD) that require renal replacement therapy (1). Hemodialysis remains the most prevalent dialysis modality throughout the world despite the stress on utilization of peritoneal dialysis (2). In the USA, hemodialysis is the renal replacement modality in >60% of patients with ESRD (3). Despite the long-term use of hemodialysis in ESRD patients, vascular access remains difficult with high rates of morbidity and mortality. Access-related complications like primary failure, patency issues, and other complications have led to increased hospitalization costs even in developed countries (4).
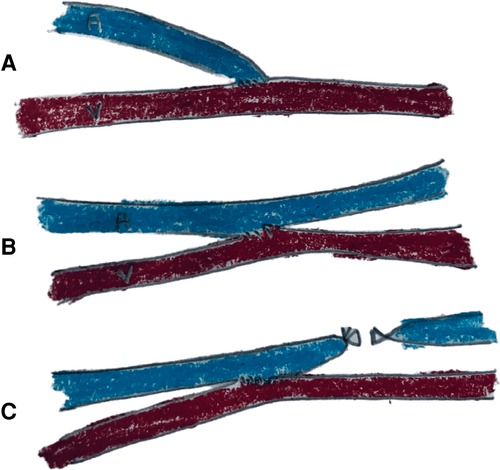
Arteriovenous fistula (AVF) has been commonly used to provide access for hemodialysis because of lower complication rates and higher survival as compared to other modalities (3). Guidelines recommend that the AVF be created at least 3–6 months prior to the initiation of hemodialysis (5). To achieve high success rates with AVF, it is important to ensure adequate preoperative assessment, meticulous patient selection, and good surgical technique. The arteriovenous connection can be provided by two techniques: End-to-side anastomosis (ETS) and side-to-side anastomosis (STS) (Figure 1). The advantages of the ETS method is that it achieves high fistula flow and is associated with reduced risk of venous hypertension. On the other hand, STS is technically easier with the highest fistula flow. Back in 1984, Wedgwood et al. (6) demonstrated that the ETS technique is the method of choice for AVF since their study showed equivalent patency rates with the two methods but higher risk of hyperemaia with STS. However, due to a lack of further evidence, there has been no consensus on the choice of anastomosis technique with only the European Society for Vascular Surgery (ESVS) guidelines recommending the ETS technique (7). With the study of Wedgwood et al. more than three decades old, there have been numerous publications (8–11) in the recent past comparing the two techniques and even suggesting that the STS technique may be better than ETS (12). Since vascular access is the primary lifeline of hemodialysis, it is essential that the selected surgical technique has a positive effect on hemodynamic changes corresponding to access formation to support maturation and patency while concurrently reducing the risk of complications. In 2018, Bashar et al. (12) compared outcomes of the ETS vs. STS technique for AVF but with only seven studies in the review. In order to incorporate recent and missed literature, we hereby performed an updated review comparing the outcomes of the ETS vs. STS technique for AVF to present the best possible evidence to clinicians.
Material and methods
The PROSPERO registration (No CRD42022355620) of the review was initiated before beginning the study. The standard guidelines of the PRISMA statement were taken into account during the conduct of the review (13).
Literature search
The search strategy involved two independent reviewers examining the databases of PubMed, CENTRAL, Web of Science, and Embase electronically. The search was conducted without any language restrictions. Studies published between 1st January 2000 to 3rd September 2022 were eligible. To identify relevant publications, we used combinations of the following keywords: “anastomosis”; “arteriovenous fistula”; “AVF”; “fistula”; “hemodialysis”; “end-to-side”; and “side-to-side”. A detailed description of the search is shown in Supplementary Table S1. After obtaining the search results of every database, they were combined for screening by the two reviewers. Once deduplication was complete, the articles were sorted by their titles and abstracts and only those that were inclined towards the review topic were included for further examination. Full texts articles were obtained and they were read by both reviewers against the eligibility criteria. All discrepancies between the reviewers were solved with discussion. We also examined previous reviews on the topic to look for additional studies.
Eligibility criteria
The PICOS inclusion criteria were:
Population- Adult patients undergoing upper limb AVF surgery for hemodialysis
Intervention- ETS technique of anastomosis
Comparison- STS technique of anastomosis
Outcomes- Patency rates or maturation time or complications
Study type- both randomized controlled trials (RCTs) and observation studies
To restrict our study to current and relevant evidence, we omitted studies before the year 2000. We excluded single-arm studies and studies with overlapping or duplicate data. For studies with duplicate data, the study reporting the maximum outcomes and with the maximum sample size was to be included.
Data and risk of bias
Two reviewers were independently involved in data collection. Details of authors, study location, study type, total sample, age, gender, diabetics, hypertensives, surgical site, and vein size were collected. In case distal vein ligation was carried out in the STS technique, it was recorded in the master table. The primary outcome of the review was patency rates (at 6 and 12 months). Secondary outcomes were maturation time and complications. If a meta-analysis was not possible a descriptive analysis was conducted. The definition of patency was as per the included study.
For observation studies, bias risk was judged using the Newcastle-Ottawa scale (NOS) (14). Every study was examined for: the selection of sample, comparability, and outcomes. We used the Cochrane Collaboration risk assessment tool for risk of bias analysis of RCTs (15). Studies were rated for risk of bias in randomization, allocation, blinding protocol, incomplete outcome reporting, selective reporting, and other biases.
Statistical analysis
“Review Manager” [RevMan, version 5.3; Nordic Cochrane Centre (Cochrane Collaboration), Copenhagen, Denmark; 2014] was the software used. Patency rates and complication rates were compared using the DerSimonian and Laird random-effects model. Data was combined to generate odds ratio (OR) and 95% confidence intervals (CI). Maturation time was compared to obtain Mean Difference (MD). The I2 statistic was used to examine heterogeneity. Funnel plots could not be used for publication bias as there were <10 studies in each meta-analysis. A sensitivity analysis was conducted to judge the impact of each study on the meta-analysis results. Additionally, a subgroup analysis was conducted based on the study type, use of distal vein ligation in the STS technique, and location of fistula (radiocephalic or mixed). p values <0.05 were considered statistically significant.
Results
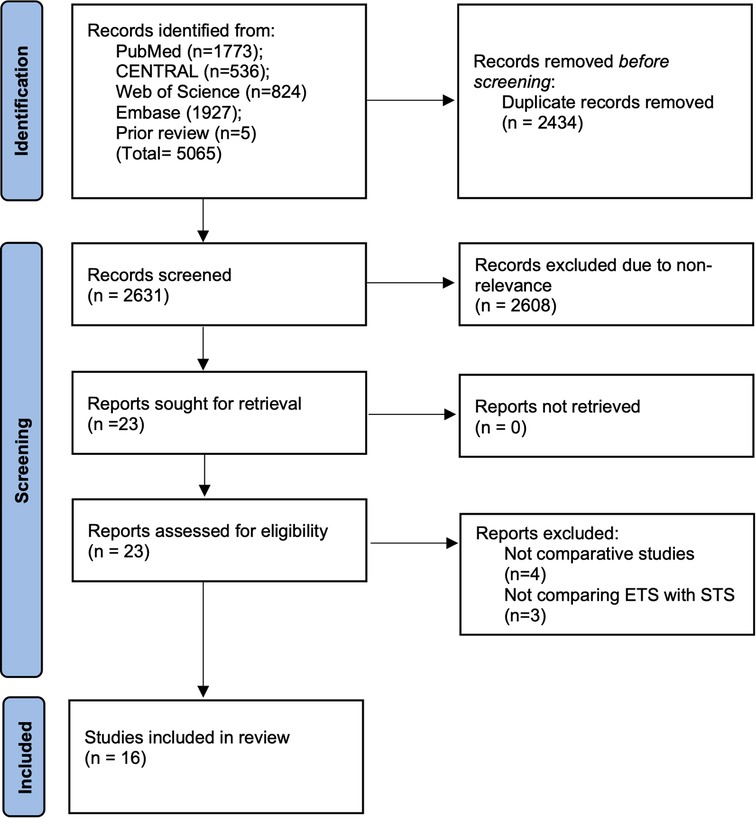
2,631 unique studies were retrieved after the literature search (Figure 2). These included 5 Chinese studies (16–20) retrieved from the previous review. All studies were thoroughly screened to identify 23 articles related to the review topic. Seven studies were excluded and 16 studies were analyzed in our systematic review and meta-analysis (8–12, 16–26).
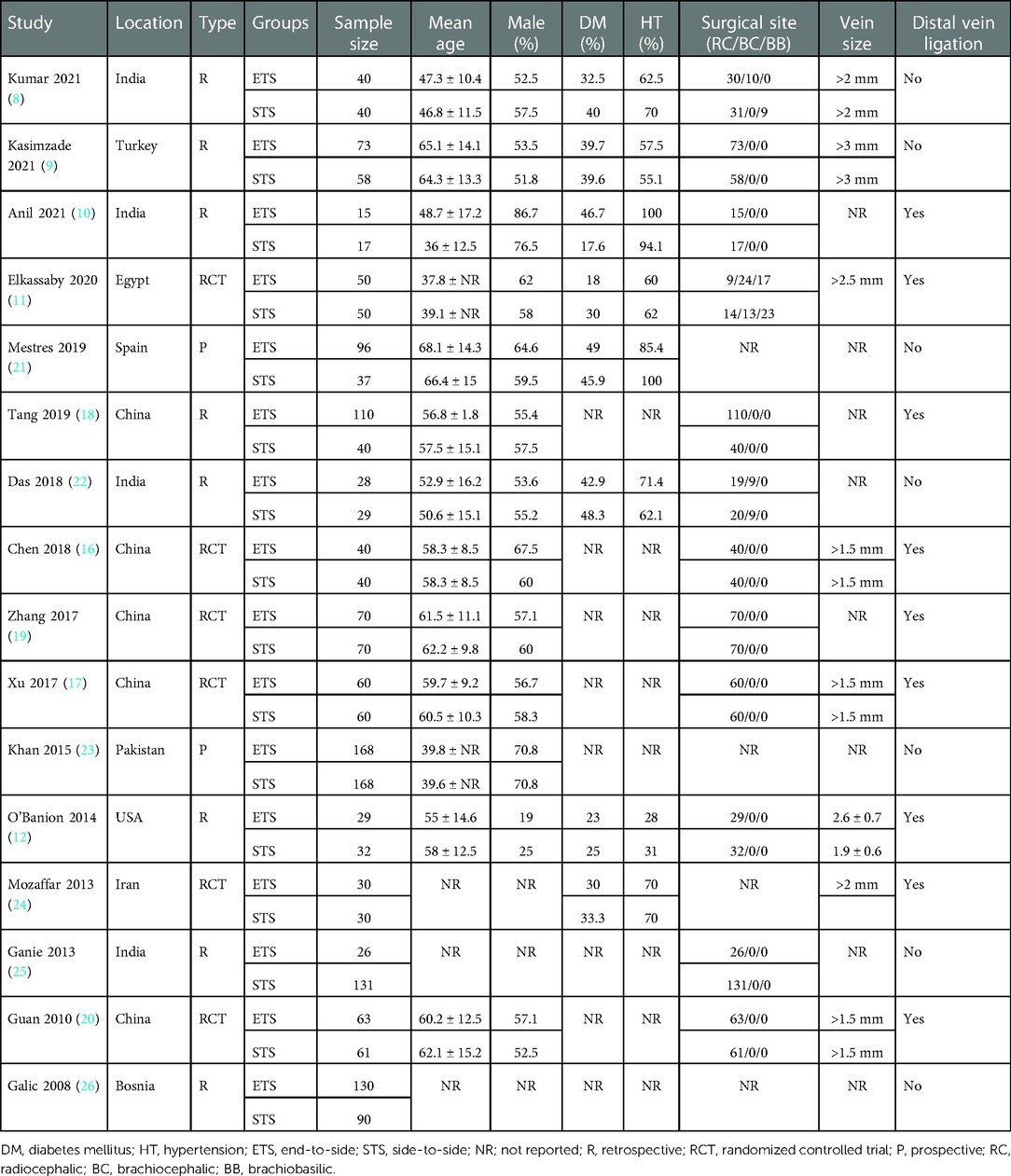
There were six RCTs, two prospective, and eight retrospective observational studies (Table 1). A total sample size of the 16 studies was 1,981 patients. The studies were published between 2008 and 2021. In nine studies, only radiocephalic AVF was compared while three studies included a mix of radiocephalic, brachiocephalic, and brachiobasilic AVFs in the two groups while four studies failed to report the exact site of AVF in their studies. The minimum vein size varied from 1.5 to 3 mm in the studies. Nine studies reported the use of distal vein ligation after the STS technique. Most of the studies did not define the reported outcomes. Data on definitions is presented in Supplementary Table S2.
Patency rates
Nine studies reported patency rates after 6 months. Meta-analysis showed that there was no difference in patency rates between ETS and STS groups at 6 months (OR: 1.15 95% CI: 0.72, 1.83 I2 = 52% p = 0.56) (Figure 3). The results did not change on the exclusion of any study. On subgroup analysis based on types of studies revealed that the difference was non-significant for both RCTs (OR: 0.77 95% CI: 0.43, 1.39 I2 = 0% p = 0.38) and non-RCTs (OR: 1.43 95% CI: 0.77, 2.63 I2 = 63% p = 0.25). On subgroup analysis based on distal vein ligation in the STS group, when no distal vein ligation was carried out in the STS group, the ETS group had significantly better patency at 6 months (OR: 1.87 95% CI: 1.27, 2.75 I2 = 0% p = 0.02). Based on fistula location, it was noted that STS group had better patency in studies on radiocephalic fistula only while ETS had better patency in mixed subgroup (Table 2).
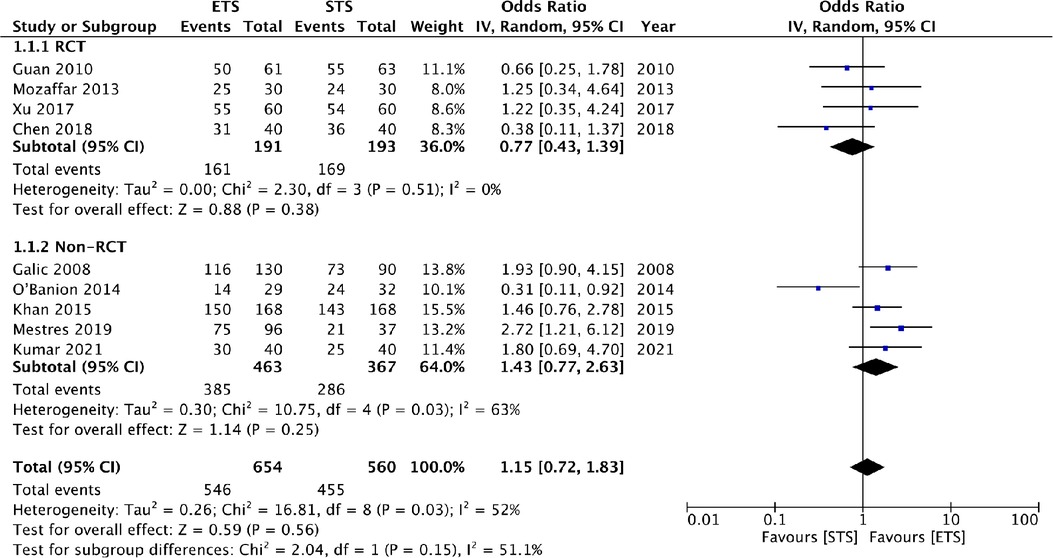
Figure 3. Meta-analysis of patency rates at 6 months between ETS and STS groups with subgroup analysis based on type of study.
Eight studies reported patency rates at 12 months. Meta-analysis showed that STS has significantly better patency at 12 months then ETS group (OR: 0.63 95% CI: 0.41, 0.95 I2 = 21% p = 0.03) (Figure 4). Results were unchanged on sensitivity analysis. For subgroup analysis based on study type, the results were non-significant for both RCTs (OR: 0.72 95% CI: 0.47, 1.10 I2 = 0% p = 0.13) and non-RCTs (OR: 0.45 95% CI: 0.14, 1.40 I2 = 62% p = 0.17) (Figure 4), but with a tendency of better patency with STS. On subgroup analysis based on distal vein ligation in the STS group, it was noted that STS had higher patency at 12 months as compared to ETS when the distal vein was ligated. On the other hand, no difference was noted in both groups when the distal vein was not ligated. Based on fistula location, it was noted that STS group had better patency in studies on radiocephalic fistula only (Table 2).
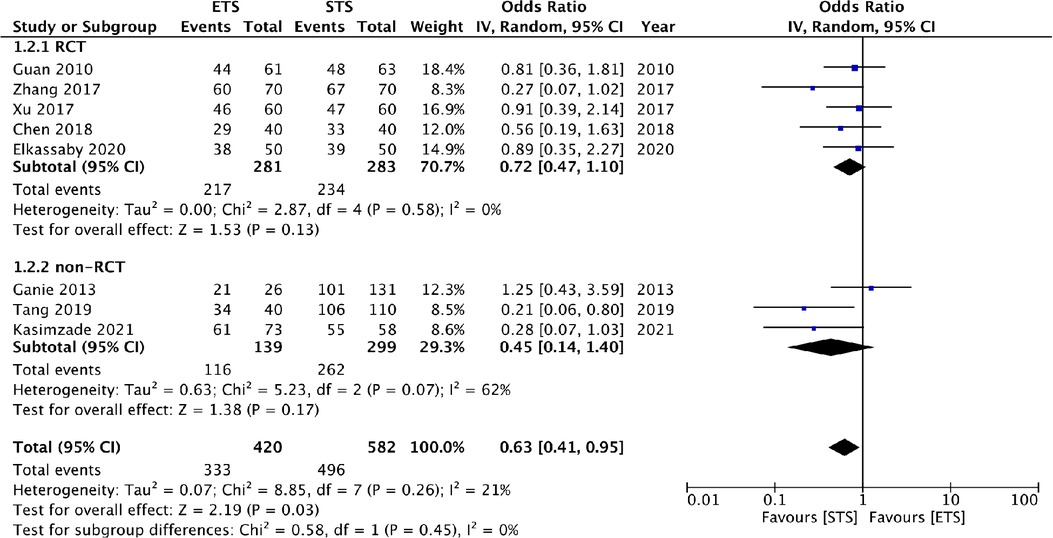
Figure 4. Meta-analysis of patency rates at 12 months between ETS and STS groups with subgroup analysis based on type of study.
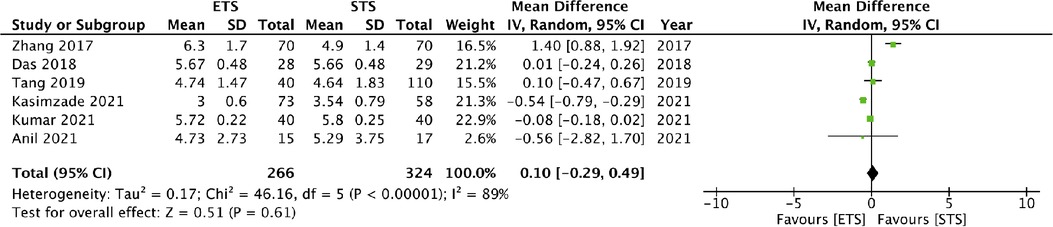
Maturation time
Six studies reported data on maturation time. Meta-analysis demonstrated no difference between the two groups (MD: 0.10 95% CI: 0.29, 0.49 I2 = 89% p = 0.61) (Figure 5). The results did not change on sensitivity analysis. There was only one RCT in the meta-analysis hence a subgroup analysis based on study type was not conducted. On subgroup analysis based on distal vein ligation in the STS group, it was noted that maturation times did not differ with or without distal vein ligation. There was no difference in maturation time based on fistula location (Table 2).
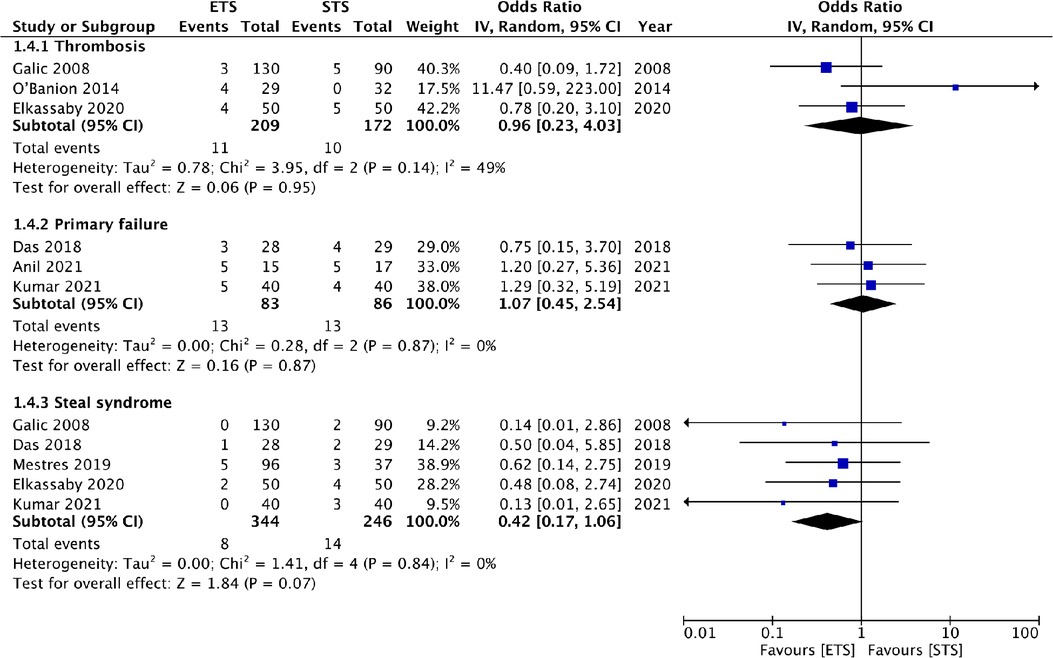
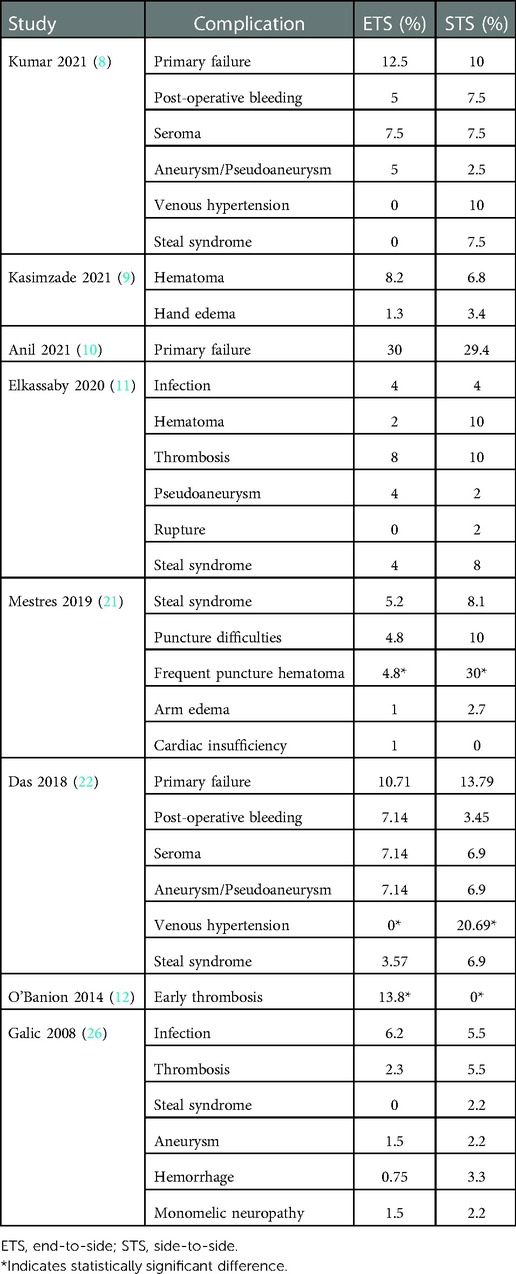
Complications
Meta-analysis showed no difference in the risk of thrombosis (OR: 0.96 95% CI: 0.23, 4.03 I2 = 49% p = 0.95), primary failure (OR: 1.07 95% CI: 0.45, 2.54 I2 = 0% p = 0.87) and steal syndrome (OR: 0.42 95% CI: 0.17, 1.06 I2 = 0% p = 0.07) between ETS and STS groups (Figure 6). There was a large variation between the studies for the remaining complications. Hence, a quantitative analysis was not conducted, and instead a descriptive analysis was carried out. Details of all complications reported by the studies in the two groups are presented in Table 3. Statistically, significant differences are marked with an asterisk.
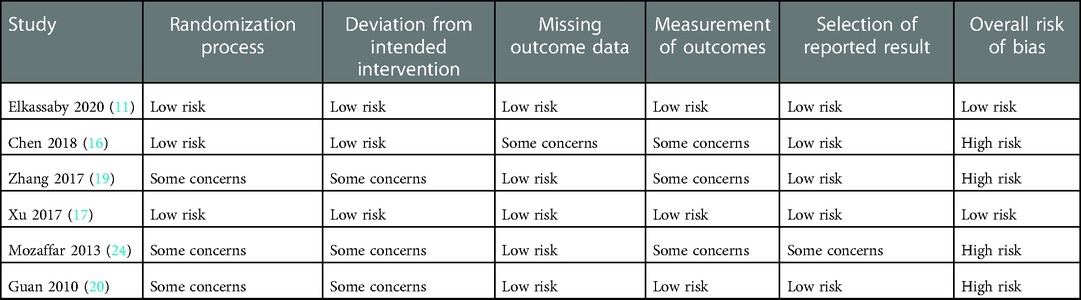
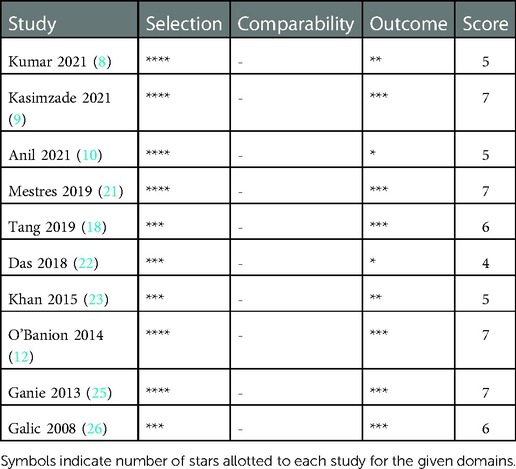
Risk of bias
The risk of bias analysis of RCTs is presented in Table 4. Only two trials had a low risk of bias. The remaining had a high risk of bias. For non-RCTs, the NOS score was in the range of 5–7 (Table 5).
Discussion
Successful application of hemodialysis in ESRD patients is directly dependent on a well-functioning AVF which provides sufficient blood flow with minimal complications. Due to limited vascular resources in the upper limb, the radiocephalic fistula is one of the commonest modalities of vascular access in such patients. First described in 1966 by Brescia and Cimino (27), radiocephalic AVF is a distal anastomosis that has fewer vascular complications. It also promotes the development of proximal veins which can be utilized for future hemodialysis accesses. Indeed, in most of the studies included in the review, radiocephalic AVF was the most common access technique. One of the most critical factors influencing the success rates of AVF is the surgical technique. it is paramount that high-quality evidence is generated to guide surgeons in selecting or disregarding a particular technique. In this review, we aimed to collate recent data on the effect of two anastomosis techniques on outcomes of AVF.
ETS anastomosis is one of the commonly used methods for AVF creation owing to its high fistula flow and reduced risk of venous hypertension of the hand. On the other hand, the STS method is the easier method with the highest fistula flow (28). Nevertheless, STS has a high risk of venous hypertension, AVF-induced ischemia, and greater complexity with vein approximation and mobilization (21). An old study by Wedgwood et al. (6) with 71 patients had shown that ETS and STS techniques had a 9-month patency rate of 79.2% and 78.6% respectively. But, 7 patients in the STS group developed hyperemia which required revision surgery. No such complication was noted in the ETS group. This prompted the authors to recommend ETS as the technique of choice for AVF anastomosis. Indeed, post this study there has been a dearth of evidence that can establish the efficacy of one technique over the other.
In this context, the results of our meta-analysis assume clinical significance as it is one of the largest meta-analyses to compare the outcomes of ETS vs. STS for AVF outcomes. In the analysis of 16 studies published in the past two decades, we noted no difference in the maturation time and 6-month patency rates of ETS and STS techniques. However, in the analysis of 12-month outcomes, we noted better patency with the STS technique as compared to the ETS method. These results are in contrast to the RCT of Wedgwood et al. (6) which has been long used to guide the anastomosis technique in AVF. Furthermore, our results are also in direct contrast with the recent meta-analysis of Bashar et al. (12), which too did not find any difference in patency rates with either ETS or STS at 3, 6, 12, and 24 months. Important differences between the previous review (12) and the current are the exclusion of pre-2000 studies, which we believe present significantly old evidence, and the addition of 12 new studies to present significantly updated evidence. Also, unlike the previous review, a subgroup analysis based on study type was conducted to separate high-quality evidence from those of retrospective studies. In the subgroup analysis too we found a tendency of better patency with STS technique at 12 months as compared to ETS but without statistical significance which could be due to the limited power of each subgroup. The results of the review are further strengthened by the absence of any change of direction of the effect size on sensitivity analysis.
Important to note is that the STS technique can be modified with ligation of the distal end of the vein to reduce the incidence of venous hypertension. The nomenclature is still STS in most studies but it has also been named functional ETS by others (21). Single arm studies have reported good outcomes with the STS technique accompanied with distal vein ligation. Hong et al. (29) in a study of 112 patients reported a patency rate of 93% after 1 year with very few complications. Similarly, Ahsan et al. (30) have reported patency rates of 96.1% without any incidence of venous hypertension. In this review, 9/16 studies reported distal vein ligation with the STS technique. When the studies were divided based on distal vein ligation, it was found that at 6 months ETS had better patency rates when no distal vein ligation was carried out while at 12 months STS had better patency when accompanied with distal vein ligation. There was no difference in patency rates between the two techniques at 12 months when no distal vein ligation was done. Thus, it can be concluded that the better patency noted with STS at 12 months in the combined meta-analysis of all studies was influenced by distal vein ligation. These results are similar to another recent meta-analysis of Weigang et al. (21) which too noted better patency rates with STS and distal vein ligation but with just seven studies in the review.
The better patency rates with STS and distal vein ligation could be due to two reasons (21). Firstly, when using this technique repeated turnover of the vessels is avoided as the artery and vein are relatively parallel and stationary. This limits arteriovenous angulation, poor vessel alignment, vessel distortion as well as rotation. Secondly, vein damage is also minimized as the operator need not prune the vessel much as in the case of ETS. Furthermore, it has been suggested that in case of thrombus formation, the surgeon can easily open the distal vein ligation to explore and retrieve the thrombus.
Not all studies in the review were exclusively on radiocephalic AVF and a small percentage of studies included other sites as well. To assess the effect of fistula location another subgroup analysis was conducted. It was noted that patency rates at 6 months were better with STS in radiocephalic group and ETS in the mixed group. Such difference could be due to the difference in technique used in the two subgroups. In the radiocephalic group, all studies used distal vein ligation which resulted in better outcomes with STS while in the mixed group most studies used ETS. Similarly, better patency at 12 months was also noted in radiocephalic group which could be attributable to distal vein ligation.
One limitation of our review was the inability to conduct a meta-analysis of all complication rates and only three complications namely, thrombosis, primary failure, and steal syndrome could be quantitatively analysed. While our review demonstrated no differences in the incidence of thrombosis, primary failure, and steal syndrome between the two techniques, data was too scarce to draw strong conclusions. On descriptive analysis, most studies failed to demonstrate major differences in complication rates between the two techniques. Only the study of Das et al. (22) found significantly higher rates of venous hypertension with the STS technique (without distal vein ligation) as compared to the ETS method. Given the limited data, it was not possible to analyze if STS with distal vein ligation and ETS techniques resulted in similar rates of venous hypertension. Further studies with a larger sample size may be able to provide further data on complication rates with the two techniques.
Other limitations of our review include, firstly, the limited number of studies in each meta-analysis. Despite including 16 studies, outcome data was not coherent which reduced the number of studies in each analysis. We were also unable to analyze patency rates beyond 1 year due to limited data. Also, patency as primary/secondary patency rates was not clearly defined in most studies and therefore the same is not clear from our results as well. Secondly, many of the included studies were non-RCTs which can be biased due to confounding. Research has shown that several factors can influence outcomes of AVF. Amongst them include patients factors like age and gender, diabetes, hypotension, artery diameter, atherosclerosis, arterial flow, vein diameter, venous expandability, smoking, obesity, early hemodialysis, anastomosis type, vascular clip use, antiplatelet therapy, use of systemic heparin, first hemodialysis timing, cannulation technique, surgical experience, and follow-up. These factors could have skewed the results of non-RCTs in the review. Lastly, the quality of included studies was not high. There were only two high-quality RCTs while many observational studies scored low on NOS.
Conclusion
Our review demonstrates that the STS anastomosis technique with distal vein ligation may result in significantly better patency rates as compared to the standard ETS technique. Data for complication rates are scarce and varied but without any significant differences between the two techniques. Based on the results, it may be recommended that the STS technique with distal vein ligation be preferred over the ETS method while creating upper limb AVFs. Nevertheless, the current evidence is fraught with low-quality studies and needs to be supplemented with future high-quality RCTs to generate better-quality evidence.
Author contributions
Both authors took part in substantial contributions to the study. YZ was the main contributor to the work. HW and YZ participated in the collection and analysis of clinical data. YZ involved in writing—original draft. HW involved in review and editing. Both authors had full access to all the data in the study and had final responsibility for the decision to submit for publication. Both authors read and approved the final manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.1079291/full#supplementary-material.
References
1. Lv JC, Zhang LX. Prevalence and disease burden of chronic kidney disease. Adv Exp Med Biol. (2019) 1165:3–15. doi: 10.1007/978-981-13-8871-2_1
2. Sasaki Y, Ogawa T, Kanayama Y, Tokui K, Morita T, Yasuda K, et al. Methods we currently use for home hemodialysis management. Contrib Nephrol. (2018) 196:237–42. doi: 10.1159/000485728
3. Lawson JH, Niklason LE, Roy-Chaudhury P. Challenges and novel therapies for vascular access in haemodialysis. Nat Rev Nephrol. (2020) 16:586. doi: 10.1038/S41581-020-0333-2
4. Masud A, Costanzo EJ, Zuckerman R, Asif A. The complications of vascular access in hemodialysis. Semin Thromb Hemost. (2018) 44:57–9. doi: 10.1055/S-0037-1606180
5. Rocco M, Daugirdas JT, Depner TA, Inrig J, Mehrotra R, Rocco M V, et al. KDOQI clinical practice guideline for hemodialysis adequacy: 2015 update. Am J Kidney Dis. (2015) 66:884–930. doi: 10.1053/J.AJKD.2015.07.015
6. Wedgwood KR, Wiggins PA, Guillou PJ. A prospective study of end-to-side vs. side-to-side arteriovenous fistulas for haemodialysis. Br J Surg. (1984) 71:640–2. doi: 10.1002/BJS.1800710831
7. Schmidli J, Widmer MK, Basile C, de Donato G, Gallieni M, Gibbons CP, et al. Editor’s choice - vascular access: 2018 clinical practice guidelines of the European society for vascular surgery (ESVS). Eur J Vasc Endovasc Surg. (2018) 55:757–818. doi: 10.1016/J.EJVS.2018.02.001
8. Kumar N, Patel S. Comparative study of end to side versus side to side arteriovenous fistula: a tertiary care center experience. Int J Med Biomed Stud. (2021) 5:226–232. doi: 10.32553/ijmbs.v5i8.2052
9. Kasimzade F, Ada F. Comparison of one-year patency rates of end-to-side and side-to-side anastomosis technique in proximal forearm region radial-cephalic fistulas. Vascular. (2021) 29:784–9. doi: 10.1177/1708538120977023
10. Anil R, Avinash P, Niranjan K, Nagraj N. Comparison between the techniques of radiocephalic arteriovenous fistulas for haemodialysis: a retrospective analytical study. J Clin Diagnostic Res. (2021) 15:OC26–9. doi: 10.7860/jcdr/2021/46567.14456
11. ElKassaby M, Elsayed N, Mosaad A, Soliman M. End-to-side versus side-to-side anastomosis with distal vein ligation for arteriovenous fistula creation. Vascular. (2021) 29:790–6. doi: 10.1177/1708538120976993
12. O’Banion LA, Van Buren D, Davis JW. Radiocephalic fistulas for hemodialysis: a comparison of techniques. Am Surg. (2015) 81:341–4. doi: 10.1177/000313481508100421
13. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. (2021) 88:105906. doi: 10.1016/j.ijsu.2021.105906
14. Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (Accessed October 30, 2020).
15. Higgins J, Altman D, Sterne J. Cochrane statistical methods group and the cochrane bias methods group. Chapter 8: assessing risk of bias in included studies. In: Cochrane handbook for systemic reviews of interventions (the cochrane collaboration). Available at: https://handbook-5-1.cochrane.org/chapter_8/8_assessing_risk_of_bias_in_included_studies.htm (Accessed on 01 Oct 2022).
16. Chen J, Feng X. The application of improved end-to- side anastomosis and traditional end-to-side anastomosis in arteriovenous fistula. Clin J Chinese Med. (2018) 10:38–41.
17. Xu H, Deng B, Wang X. The difrerenees between functional end-to-side anastomosis and traditional end-to-side anastomosis in the establishment of arteriovenous fistula surgery. Int Med Heal Guid News. (2017) 23:1200–2.
18. Tang W, Gong L, Lu J. The clinical application of functional end-to-side anastomosis in the primary arterio- venous fistula. Chinese J Integr Tradit West Nephrol. (2019) 20:730–31.
19. Zhang C. Application of functional end-to-side anasto- mosis for arteriovenous fistula angioplasty used in hemodialysis. Chinese J Integr Tradit West Nephrol. (2017) 18:808–9.
20. Guan S, Bao W, Duan Y. Functional and traditional end-to-side anastomosis for arteriovenous fistula plasty in hemo- dialysis patients:a randomized controlled study. Acad J Second Mil Med Univ. (2010) 31:1065–7. doi: 10.3724/SP.J.1008.2010.01065
21. Mestres G, Gonzalo B, Mateos E, Yugueros X, Martínez-Rico C, Marcos L, et al. Comparison of side-to-end vs. side-to-side proximal arteriovenous fistula anastomosis in chronic renal failure patients. Vascular. (2019) 27:628–35. doi: 10.1177/1708538119847392
22. Das S. Comparison of side to side vs end to side arteriovenous fistula in upper limb for hemodialysis. J Med Sci Clin Res. (2018) 6:10–15. doi: 10.18535/jmscr/v6i11.02
23. Khan MW, Khan MM, Qadir I, Ch ZA, Liaquat H. Comparative study of efficacy of end-to-side with side-to-side arteriovenous fistula in patients on hemodialysis. Pakistan J Med Heal Sci. (2015) 9:235–8.
24. Mozaffar M, Fallah M, Lotfollahzadeh S, Sobhiyeh MR, Gholizadeh B, Jabbehdari S, et al. Comparison of efficacy of side to side versus end to side arteriovenous fistulae formation in chronic renal failure as a permanent hemodialysis access. Nephrourol Mon. (2013) 5:827–30. doi: 10.5812/numonthly.10248
25. Ganie FA, Lone H, Dar AM, Lone GN, Wani ML. Native arterio-venous fistula is the vascular access of choice for hemodialysis in end stage renal disease. Int Cardiovasc Res J. (2013) 7:67–70.24757624
26. Galić G, Kvesić A, Tomić M, Rebac Z, Brekalo Z, Martinović V, et al. The advantages of end-to-side arteriovenous anastomosis over the other two types of arteriovenous anastomosis in dialysis patients. Coll Antropol. (2008) 32:109–14.
27. Cimino JE. Historical perspective on more than 60 years of hemodialysis access. Semin Vasc Surg. (2007) 20:136–40. doi: 10.1053/J.SEMVASCSURG.2007.07.010
28. Weigang T, Wei X, Lifeng G, Jingkui L, Yani L, Huaqin J, et al. A meta-analysis of traditional and functional end-to-side anastomosis in radiocephalic fistula for dialysis access. Int Urol Nephrol. (2021) 53:1373–82. doi: 10.1007/S11255-020-02691-9
29. Hong SY, Yoon YC, Cho KH, Lee YH, Han IY, Park KT, et al. Clinical analysis of radiocephalic fistula using side-to-side anastomosis with distal cephalic vein ligation. Korean J Thorac Cardiovasc Surg. (2013) 46:439–43. doi: 10.5090/KJTCS.2013.46.6.439
Keywords: hemodialysis, vascular access, fistula, surgery, patency
Citation: Zhou Y and Wu H (2023) Comparison of end-to-side versus side-to-side anastomosis in upper limb arteriovenous fistula in hemodialysis patients: A systematic review and meta-analysis. Front. Surg. 9:1079291. doi: 10.3389/fsurg.2022.1079291
Received: 25 October 2022; Accepted: 9 December 2022;
Published: 6 January 2023.
Edited by:
Nikolaos Kontopodis, University Hospital of Heraklion, GreeceReviewed by:
George Galyfos, National and Kapodistrian University of Athens, GreeceBaoyu Zhao, Shanxi Provincial People's Hospital, China
© 2023 Zhou and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongyan Wu d2h5NjI5MTQ3NjdAMTI2LmNvbQ==
Specialty Section: This article was submitted to Vascular Surgery, a section of the journal Frontiers in Surgery
 Yu Zhou
Yu Zhou Hongyan Wu
Hongyan Wu