- 1Department of Plastic Surgery and Burn, Peking University First Hospital, Beijing, China
- 2Department of Anti-Infection, Institute of Clinical Pharmacology, Peking University First Hospital, Beijing, China
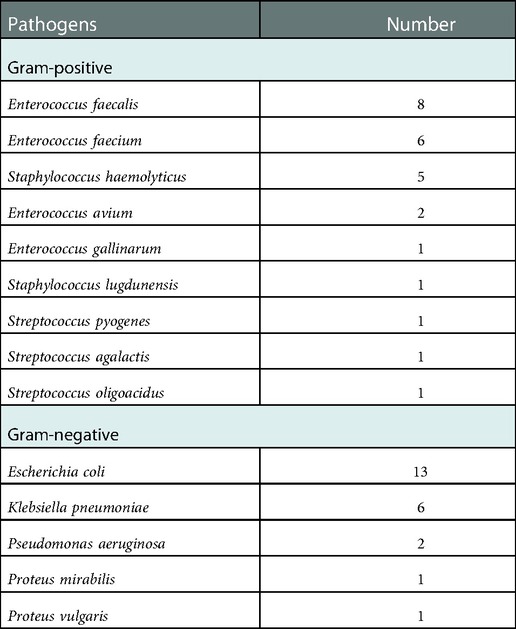
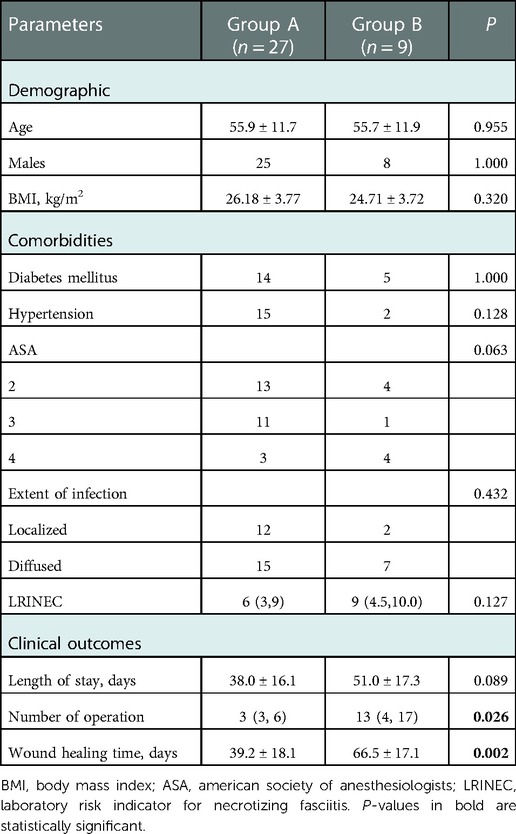
Fournier gangrene (FG) is a life-threatening disease affecting the soft tissues of the genital, perineal, and perianal regions. This retrospective study aimed to summarize the characteristics of FG and evaluate the effects of negative-pressure wound therapy (NPWT). We analyzed clinical data of 36 patients with FG admitted to our department. Thirty-four cases had perianal and external genital infections, and the other two had secondary infection of the urinary fistula after trauma and retroperitoneal abscess, respectively. Monomicrobial, polymicrobial, culture-negative, and fungal infections were identified in 16, 17, 2, and 1 cases, respectively. Escherichia coli, Enterococcus faecalis, Enterococcus faecium, Klebsiella pneumoniae, and Staphylococcus haemolyticus were the most common pathogens. The mortality rate was 8%. Twenty-seven and nine patients were treated with NPWT (group A) and conventional dressing (group B), respectively. The length of stay was 38.0 ± 16.1 and 51.0 ± 17.3 days, number of operations were 3 (3,6) and 13 (4,17), and wound healing times were 39.2 ± 18.1 and 66.5 ± 17.1 days in groups A and B, respectively. Taken together, clinicians should always consider the possibility of perianal or external genital infections progressing to FG in the daily work, especially for patients with diabetes mellitus. Enterobacteriaceae, Enterococcus, and Staphylococcus haemolyticus are the most common causative pathogens, and NPWT is an effective adjuvant therapy for wound management with fewer operations and a shorter wound healing time.
1. Introduction
Fournier's gangrene (FG) is a specific form of necrotizing fasciitis that involves the soft tissues of the genital, perineal, and perianal regions. It is an uncommon disease that can affect people of any age and rapidly progress to a life-threatening stage. The incidence is reported to be 1.6 cases per 100,000 men per year and remains steady after the age of 50 at 3.3 cases per 100,000 men (1). Early diagnosis and emergency intervention are mandatory owing to the rapid rate of fascial necrosis. However, non-specific symptoms at the early stage and lack of awareness among clinicians may delay diagnosis, hence, leading to a miss of the best time for intervention. As the infection progresses, typical symptoms may present, such as blistering, purulent discharge, crepitation, or necrosis, accompanied by systemic inflammatory response syndrome, sepsis, shock, or multiple organ dysfunction syndrome (MODS), leading to death. The infection can spread to distal regions, such as the abdominal wall, ischiorectal fossa, hip, and thigh through the fascial plane. Currently, the mortality remains at 20%–30% (2, 3). Negative-pressure wound therapy (NPWT) is an effective wound management technique that is widely used for almost all types of wounds. This study aimed to summarize the characteristics of FG and evaluate the effects of NPWT.
2. Materials and methods
This retrospective case-control study enrolled patients with FG treated at our department between May 2010 and June 2022. Data were obtained from medical records. The diagnosis was based on clinical findings (necrosis of the skin and/or fascia, gray discolored fascia, “dishwater fluid,” lack of bleeding, and tissue resistance of the fascial layer). The extent of infection that limited itself to the genital, perineal, or perianal regions was considered as “localized;” otherwise it was considered as “diffused”. Patients were divided into two groups based on wound management: group A comprised patients treated with NPWT and group B comprised patients treated with conventional dressing. This study was approved by the Institutional Human Investigations Committee.
2.1. Treatment approaches
2.1.1. Anti-infection treatment
Broad-spectrum anti-infection treatment comprising carbapenem and vancomycin was empirically administered upon diagnosis of FG and subsequently modified based on the culture results. The duration of anti-infection treatment required comprehensive consideration of systemic signs and symptoms, local signs of infection, and laboratory test results.
2.1.2. Surgical treatment
Emergency surgical debridement was performed within 24 h after admission. An incision was made in the area of sclerosis, erythema, ulceration, or necrosis. The necrotic tissue was removed, drainage was ensured, and thorough dissection along the fascial plane was performed to explore the extent of the infection until viable tissue was identified. Samples for culture were routinely obtained. Digital rectal examination was routinely performed to confirm the presence of anal fistula. Colostomy was performed for patients with anal fistulas or severe perianal involvement. Suprapubic cystostomy was performed for patients with urethral fistulas.
After the initial debridement, conventional dressing or NPWT was used for postoperative wound management based on patients' choice. Dressings were changed when the wound became wet for the conventional method or every 5–7 days when NPWT was applied. Negative pressure was applied in continuous mode with the suction level of −125 mmHg. A series of debridement procedures were performed if residual necrotic tissue was present. The wound reconstruction method depended on the location and extent of the defect (Figure 1).
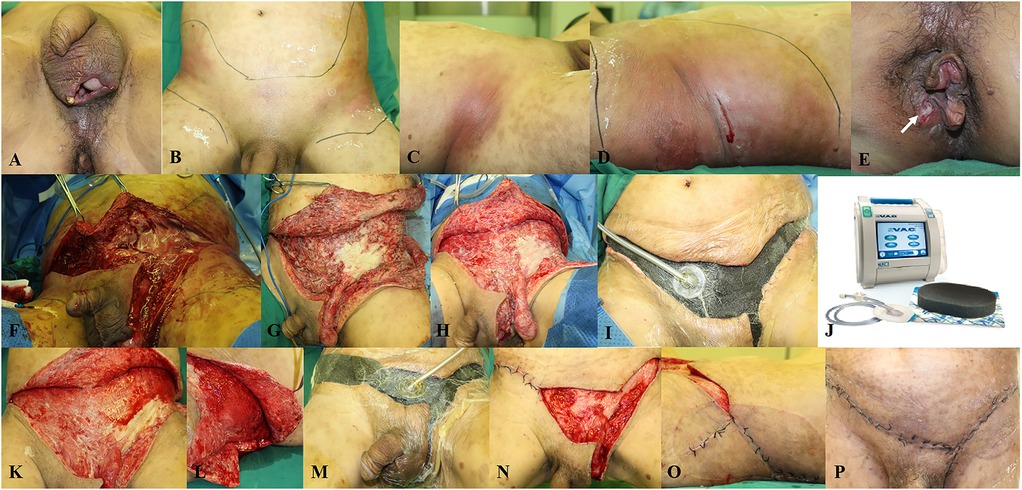
Figure 1. A representative case of a 50-year-old patient diagnosed with fournier gangrene and transferred to our department. (A–D) Despite incision and drainage of the scrotum before admission, the infection spread to the lower and lateral abdominal wall. (E) The etiology is the perianal abscess (white arrow). (F) Emergency surgical debridement is performed. (G) Appearance after debridement. (H) Appearance before the second debridement. (I) NPWT is applied during the third debridement. (J) The V.A.C. system used in our department. (K,L) Appearance before the fourth debridement. (M) Part of the wound is closed and NPWT is continued after the fourth debridement. (N,O) Appearance before the fifth debridement; the rest of the wound is closed. (P) Appearance before discharge.
2.1.3. Supportive treatment
Nutritional support, glucose control, fluid and electrolyte balance, blood product transfusion, and comorbidity control were also important treatments for FG. Patients with hemodynamic instability, septic shock, or MODS were transferred to the intensive care unit.
2.2. Data collection
Medical record data including demographic data, initial symptoms, physical examination findings, vital signs, treatment before admission, comorbidities, laboratory tests, microbiological results, American Society of Anesthesiologists score, number of operations, extent of infection, wound coverage, length of stay, and wound healing time were collected. Laboratory risk indicators for necrotizing fasciitis (LRINEC) (4) were also calculated.
2.3. Statistical analysis
Statistical analyses were performed using SPSS software version 22. Continuous parametric variables are shown as means with standard deviations (SDs) and continuous nonparametric variables, as medians with interquartile ranges (IQRs). All continuous variables were subjected to the Kolmogorov–Smirnov test. Normally distributed variables were analyzed using an independent-sample t-test. Otherwise, the variables were compared using the Mann–Whitney U test. Categorical variables were analyzed using the Pearson's χ2 test (Fisher's exact test, as appropriate). P < 0.05 was considered to be statistically significant.
3. Results
Thirty-six patients were enrolled in the study. Patient characteristics and diseases are shown in Table 1. Diabetes mellitus (DM) was the most common comorbidity (53%). Twenty-eight patients were transferred to our department from other hospitals, 12 of whom had undergone incision and drainage. The predominant etiologies were perianal (64%) and external genital (31%) infections. The infection had spread to the distal part beyond the genital, perineal, or perianal regions in 24 cases, including the lower or lateral abdominal wall, inguinal region, thigh, ischiorectal fossa, and hip.
Pathogens were identified in 34 (95%) patients. The details of the 49 bacterial strains cultured were listed in Table 2. Enterobacteriaceae, Enterococcus, and Staphylococcus haemolyticus were the most common causative pathogens. The resistance rate of gram-negative bacilli to third-generation cephalosporins was 35%. Vancomycin-resistant gram-positive bacteria were not found, but all S. haemolyticus isolates were methicillin resistant.
Colostomy and suprapubic cystostomy was performed in 10 and 2 patients, respectively. The mortality rate was 8%. Delayed primary closure, secondary intention, or split-thickness skin grafts (STSG) were applied for wound reconstruction.
3.1. Comparison between the two groups
Twenty-seven and nine patients received NPWT (group A) and conventional dressing treatment (group B), respectively. There were no significant differences in the baseline clinical characteristics between the two groups (Table 2). However, the number of operations in group A was significantly lower than that in group B, and the wound healing time in group A was significantly shorter than that in group B (Table 3).
4. Discussion
FG is a fulminant and life-threatening disease that requires timely and standardized intervention. The initial symptoms vary; therefore, FG is easily misdiagnosed as cellulitis or erysipelas. Once typical symptoms appear, the infection is usually severe or has already spread to the distal regions. Pathogens play an important role in the development of FG (5). We enrolled a relatively large number of patients with FG, summarized their characteristics, provided the spectrum of pathogens, shared treatment experiences, and evaluated the effects of NPWT.
DM is one of the main predisposing factors, apart from immunosuppression, malignancy, and chronic steroid use (5). Local intravenous drug injection can also be the predisposing factor in rare cases (6). Concordant with previous studies, 53% of patients in the present study had DM. A meta-analysis showed that mortality due to FG is associated with DM (7). In the present study, the prevalence of DM in patients who died (67%) was higher than that in patients who survived (52%); however, the relatively small number of patients who died precludes statistical conclusions from being drawn. Perianal and external genital infections were the predominant etiologies, and the infection had spread to the distal parts in most cases (67%). This finding was consistent with the anatomical features and pathogenesis of FG. Perianal sources of infection can spread to the perineal fascia through perianal space, and fascial systems of the penis, scrotum, perineum, and abdominal wall are all connected. Therefore, perianal abscess may involve the Colles fascia, and the infection may spread to the penis and scrotum via Buck's and Dartos fascia, or to the anterior abdominal wall via Scarpa's fascia, or vice versa. Therefore, to avoid misdiagnosis or delayed diagnosis, clinicians should always consider the possibility of perianal or external genital infections progressing to FG in the daily work, especially for patients with DM. Patients are recommended to routinely undergo LRINEC scoring, closely observe the wound, and maintain timely communication.
An early diagnosis of FG is challenging, but the principles of treatment are clear and include aggressive debridement, anti-infection treatment, and supportive treatment (5, 7). Furthermore, the principles of anti-infection treatment depend on empirical broad-spectrum antibiotic coverage before pathogen identification. Therefore, it is imperative to understand the characteristics of these pathogens. Some studies suggested polymicrobial infection as the predominant type (5, 8, 9), but another study identified predominant incidence of monomicrobial gram-negative organisms in southwestern China (10). Nevertheless, Escherichia coli is the most frequently isolated microorganism (2, 9, 10). The generally accepted and recommended empirical antibiotic therapy includes aminoglycosides, metronidazole or clindamycin, and third-generation cephalosporin (5, 9). In the present study, the incidence of monomicrobial infections was approximately equal to that of polymicrobial infections. Escherichia coli and Klebsiella pneumoniae were the most common gram-negative, causative pathogens, whereas Enterococcus faecalis, Enterococcus faecium, and Staphylococcus haemolyticus were the most common gram-positive, causative pathogens. These findings are consistent with the predominant etiology of FG. The proportion of resistant bacteria was high; the resistance rate of gram-negative bacilli to third-generation cephalosporins was 35%, and all cases with Staphylococcus haemolyticus were methicillin resistant. Therefore, considering the drug resistance and severity of FG, carbapenem and vancomycin were used as empirical antibiotic therapies at our department. We believe that empirical antibiotic therapy in different regions should be consistent with the characteristics of the pathogens. Furthermore, although fungal infections have rarely been reported in the literature, fungal smears should be indicated to clarify the possibilities of fungal infections.
As a series of debridement procedures are normally required, an appropriate method for wound management should be applied. For conventional dressing treatment, frequent dressing changes, difficulty in timely and adequate control of exudate, and limited mobility are disadvantages. However, NPWT can create a controlled and closed negative-pressure environment. By continuously removing the wound exudate, reducing the wound area, increasing blood perfusion, and stimulating angiogenesis, it can effectively promote wound healing (11). Owing to these advantages, NPWT has been widely used to treat various types of wounds. In the present study, NPWT significantly reduced the number of operations and shortened wound healing time than conventional dressing treatment. Moreover, NPWT can effectively fix grafted skin on the surface of irregular wounds, such as the penis or scrotum. Patients can carry the device while moving in the ward, ensuring increased compliance to the treatment. However, NPWT cannot replace surgical debridement as a wound management technique as inappropriate use can aggravate infection. Colostomy is recommended for patients with anal fistulas or severe perianal involvement, making NPWT feasible. Hyperbaric oxygen therapy (HBOT) is also an effective adjuvant therapy for FG, and NPWT combined with HBOT shows advanced wound healing with a high efficiency rate (12). However, the main reason hampering the use of HBOT is the poor availability of the devices.
The present study has some limitations. First, as this was a single-center retrospective study, the applicability of the findings may be limited. However, the cohort size was relatively larger than that of other single-center studies. Thus, for the possible differences in the pathogenic spectrum, we also proposed relevant principles. Second, as several patients were transferred from other hospitals, some initial laboratory parameters were unavailable and previous treatment may have caused changes in the laboratory test results. However, owing to the low incidence of FG and difference in medical capacity, this phenomenon cannot be avoided.
5. Conclusion
Clinicians should always consider the possibility of perianal or external genital infections progressing to FG in the daily work, especially for patients with DM. Enterobacteriaceae, Enterococcus, and Staphylococcus haemolyticus were the most common causative agents. NPWT is an effective adjuvant therapy for wound management, with fewer operations and shorter wound healing times.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Institutional Human Investigations Committee of Peking university first hospital. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
RH, BW and XQ: contributed to conception and design of the study. RH: organized the database. RH and KX: performed the statistical analysis. RH: wrote the first draft of the manuscript. RH and XL: wrote sections of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Youth Clinical Research Project of the Peking University First Hospital (grant no. 2017CR13).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sorensen MD, Krieger JN. Fournier’s gangrene: epidemiology and outcomes in the general US population. Urol Int. (2016) 97:249–59. doi: 10.1159/000445695
2. Pehlivanlı F, Aydin O. Factors affecting mortality in Fournier gangrene: a single center experience. Surg Infect. (2019) 20:78–82. doi: 10.1089/sur.2018.208
3. Morais H, Neves J, Maciel Ribeiro H, Ferreira M, Guimarães N, Azenha N, et al. Case series of Fournier’s gangrene: affected body surface area-the underestimated prognostic factor. Ann Med Surg. (2017) 16:19–22. doi: 10.1016/j.amsu.2017.02.043
4. Wong CH, Khin LW, Heng KS, Tan KC, Low CO. The LRINEC (Laboratory Risk Indicator for Necrotizing fasciitis) score: a tool for distinguishing necrotizing fasciitis from other soft tissue infections. Crit Care Med. (2004) 32:1535–41. doi: 10.1097/01.CCM.0000129486.35458.7D
5. Chennamsetty A, Khourdaji I, Burks F, Killinger KA. Contemporary diagnosis and management of Fournier’s gangrene. Ther Adv Urol. (2015) 7:203–15. doi: 10.1177/1756287215584740
6. Zingaro MD, Boni A, Vermandois JAR, Paladini A, Lepri E, Ursi P, et al. Fournier’s gangrene and intravenous drug abuse: an unusual case report and review of the literature. Open Med. (2019) 14:694–710. doi: 10.1515/med-2019-0114
7. El-Qushayri AE, Khalaf KM, Dahy A, Mahmoud AR, Benmelouka AY, Ghozy S, et al. Fournier’s gangrene mortality: a 17-year systematic review and meta-analysis. Int J Infect Dis. (2020) 92:218–25. doi: 10.1016/j.ijid.2019.12.030
8. Ozkan OF, Koksal N, Altinli E, Celik A, Uzun MA, Cıkman O, et al. Fournier’s gangrene current approaches. Int Wound J. (2016) 13:713–6. doi: 10.1111/iwj.12357
9. Yilmazlar T, Gulcu B, Isik O, Ozturk E. Microbiological aspects of Fournier’s gangrene. Int J Surg. (2017) 40:135–8. doi: 10.1016/j.ijsu.2017.02.067
10. He X, Xiang X, Zou Y, Liu B, Liu L, Bi Y, et al. Distinctions between Fournier’s gangrene and lower extremity necrotising fasciitis: microbiology and factors affecting mortality. Int J Infect Dis. (2022) 122:222–9. doi: 10.1016/j.ijid.2022.05.040
11. Apelqvist J, Willy C, Fagerdahl AM, Fraccalvieri M, Malmsjö M, Piaggesi A, et al. [EWMA document]. EWMA document: negative pressure wound therapy. J Wound Care. (2017) 26(Suppl 3):S1–154. doi: 10.12968/jowc.2017.26.Sup3.S1
Keywords: Fournier gangrene, negative-pressure wound therapy, necrotizing fasciitis, microbiology, treatment
Citation: He R, Li X, Xie K, Wen B and Qi X (2023) Characteristics of Fournier gangrene and evaluation of the effects of negative-pressure wound therapy. Front. Surg. 9:1075968. doi: 10.3389/fsurg.2022.1075968
Received: 21 October 2022; Accepted: 6 December 2022;
Published: 6 January 2023.
Edited by:
Ettore Mearini, University of Perugia, ItalyReviewed by:
Gianluca Gaudio, University of Perugia, ItalyVincenzo Vindigni, University of Padua, Italy
© 2023 He, Li, Xie, Wen and Qi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xin Qi 04983@pkufh.com
Specialty Section: This article was submitted to Reconstructive and Plastic Surgery, a section of the journal Frontiers in Surgery
 Rui He
Rui He Xiangyan Li2
Xiangyan Li2 Xin Qi
Xin Qi