- 1Department of Thoracic Surgery, Peking Union Medical College Hospital, Chinese Academy of Medical Science and Peking Union Medical College, Beijing, China
- 2Chinese Academy of Medical Science and Peking Union Medical College, Beijing, China
Background: The left lung has two lobes and one fissure, while the right lung has three lobes and two fissures. Accessory fissures are usually found in imaging examinations and autopsies; however, finding an actual accessory lobe is rare.
Case presentation: In a lung nodule resection surgery, a 68-year-old male patient was found with three lobes and two fissures in his left lung. The lung nodule was misdiagnosed as being located in the lower lobe because the accessory fissure was misregarded as the oblique fissure. The lung nodule was found in the upper lobe, and this anatomical variation changed the surgical plan. The pathology of the lung nodule was granulomatous inflammation with caseous necrosis with the positive antacid stain. The patient was eventually diagnosed with tuberculosis.
Literature review: Cases involving the lung accessory fissure and lung accessory lobe variants were reviewed. In 10 autopsy and dissection studies, the incidence of accessory fissure in the left lung was 13.5% (79/587, ranging from 2.7% to 50.0%), and in the right lung, it was 7.3% (42/575, ranging from 3.1% to 30.4%). The incidence of accessory lobes in the left lung was 2.0% (11/547, ranging from 0.0% to 7.4%), and in the right lung was 2.6% (14/539, ranging from 0.0% to 17.4%). The incidence of accessory fissures in bilateral lungs identified by chest x-ray or computed tomography ranged from 7.3% to 32.0%. Three surgical case reports inferred accessory lobes, including a left upper lobectomy, left lung transplantation, and an open thoracotomy.
Conclusion: This is the first clinical case report that shows that lung accessory lobe caused the mislocation of a lung nodule. Therefore, radiologists and surgeons should be aware of the possibility of an accessory lobe in the lung.
Introduction
The lungs are essential organs of respiration and are situated in the thoracic cavity on either side of the mediastinum. They are divided by fissures into lobes, facilitating movements of lobes toward one another. Usually, the left lung is divided by an oblique fissure into two lobes, namely the upper and lower lobes. The right lung is divided by oblique and horizontal fissures into the upper, middle, and lower lobes.
The spectacular advances in thoracic surgery in significant part date from the successful lobectomies performed during the early 1930s and from Graham's successful pneumonectomy for carcinoma of the lung in 1933 (1). If the surgeon's efforts were confined to the resection of a lobe or a whole lung, the importance of segmental anatomy was not fully appreciated. However, many factors still caused the misdiagnosis in segmental anatomy confirmation before surgery. The lung anatomical variations were one of the most frequently occurring causes of misdiagnosis.
Awareness of anatomical variations of lobes of the lung is essential because radiologists may misinterpret them on a chest x-ray (CXR) or a computed tomography (CT) scan. To our knowledge, there has been no report on the misdiagnosis before the lobectomy due to the anatomical variations. We herein report a 68-year-old male who was misdiagnosed with a pulmonary nodule located in the left dorsal segment (S6) before surgery. He was found to have a complete fissure splitting the upper lobe into two lobes, and the nodule was actually located in the apicoposterior segment (S1 + 2) as an accessory lobe.
Case presentation
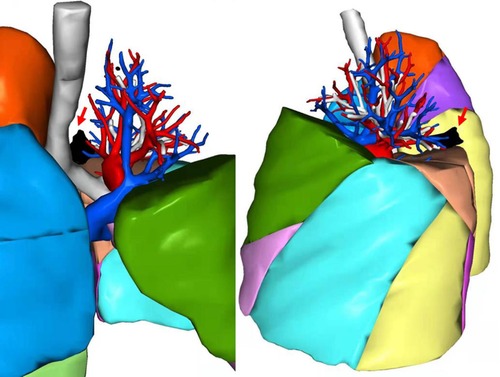
A 68-year-old male was discovered to have a pulmonary nodule in a CT scan for 4 years with no apparent symptoms. The latest CT scan (10/2021) indicated a blade-like hyperdense shadow (2.4 cm × 2.0 cm) in the lower-left lung (Figure 1), which had a higher density than before (06/2019). The positron emission tomography/CT (PET/CT) showed that the standard uptake value (SUV) max of the nodule was 8.1 and had high suggestive of malignancy. Both CT and PET/CT reported that the nodule was located in the left dorsal segment (S6) (Figure 1). Considering the possibility of high suggestive malignancy, it was planned for this patient to receive a video-assisted thoracic surgery (VATS) lobectomy of the left lower lobe.
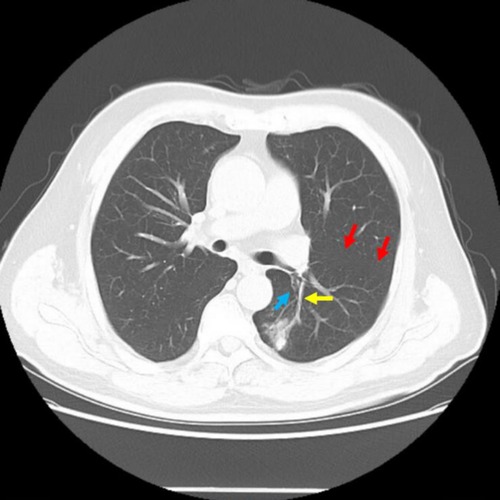
Figure 1. CT imaging of the patient before the surgery. The red arrow refers to the oblique fissure, the yellow arrow refers to the S6 artery, and the blue arrow refers to the S6 bronchus, regarded by radiologists and surgeons.
During intraoperative exploration, the patient was found to have a complete fissure splitting the upper lobe into two lobes (Figure 2). The accessory fissure completely splits the apicoposterior segment (S1 + 2) from the upper lobe. Therefore, there were three lobes in the left lung, including the S1 + 2 as an accessory lobe, the rest of the upper lobe, and the lower lobe. In addition, the target nodule was actually in the S1 + 2, not the S6 considered before surgery.
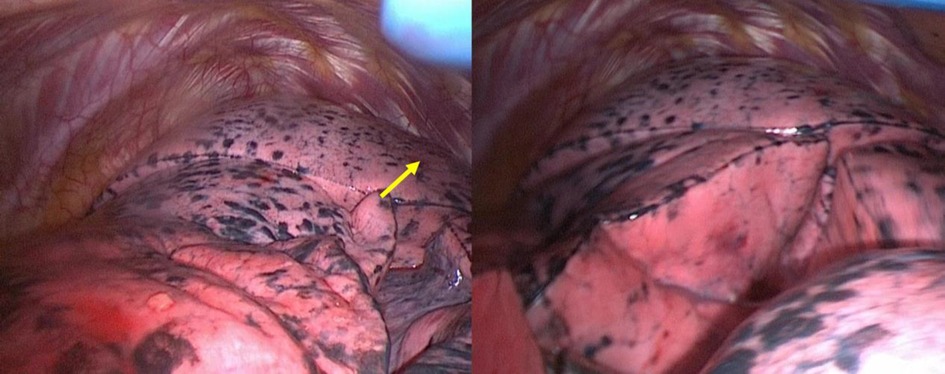
Figure 2. The three lobes of left lung photographed in the VATS. The yellow arrow refers to the lung nodule which cannot be found in the surface.
The surgery was changed to a segmentectomy of the S1 + 2. After the surgery, the patient recovered well and was discharged from the hospital after three days. The pathology of the lung nodule was granulomatous inflammation with caseous necrosis, with the positive antacid stain. The patient was eventually diagnosed with tuberculosis.
This misdiagnosis of location could be avoided, as the additional fissure, the real bronchus, and vessels of S1 + 2 and S6 were not tricky to identify in preoperative CT (Figure 3). Figure 4 shows a three-dimensional (3D) reconstruction of the lungs. The nodule was located in the S + 2, adjacent to the S6. A1 + 2a and A1 + 2b come from the posterior ascending artery, while A1 + 2c comes from the first trunk of the pulmonary artery.
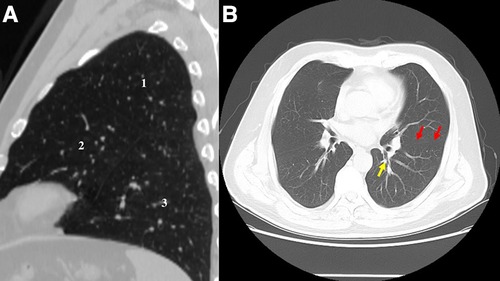
Figure 3. (A) CT image before the surgery shows the three lobes of the left lung: 1, accessory lobe (S1 + 2); 2, the rest upper lobe; 3, lower lobe. (B) CT image before the surgery. The red arrow refers to true oblique fissure. The yellow arrow refers to the true S6 bronchus.
Literature review and discussion
Fissural anomalies include the presence of accessory fissures that develop to subdivide lobes or segments of the lung. The commonly described accessory fissures (also called supernumerary fissures) are the azygos fissure, superior accessory fissure, inferior accessory fissure, and left and right minor fissures (2–6). The most common accessory fissure described by anatomical studies (7–10) is the left minor fissure, which was first described by Boyden (11). Inferior accessory fissure (12) and left minor fissure (2) were the first and second most common accessory fissures detected by CT.
Grade classification of lung fissures, including accessory fissure proposed, by Craig and Walker (13) in 1997:
• Grade 1, complete fissure with entirely separate lobes.
• Grade 2, complete visceral cleft with parenchymal fusion at the base of the fissure.
• Grade 3, visceral cleft is evident for part of the fissure.
• Grade 4, complete fusion of the lobes with no evident fissural line.
Only when the accessory fissure is at Grade 1, which means a complete fissure with entirely separate lobes, does the accessory fissure demarcate the accessory lobe.
Accessory fissures are commonly identified incidentally during autopsy, dissection, and imaging examinations performed on the chest, including CXR and CT. Their presence may be of clinical importance both surgically and radiologically (14). Accessory fissures can be mistakenly confused with areas of linear atelectasis, pleural scars, pleural effusion, or walls of bullae (15, 16). The presence of a superior accessory fissure of the lower lobe correlates with characteristic patterns of atelectasis and pleural fluid collection on conventional radiographs (17). In the presence of extra lobes, the CT scan showed a significant increase in the size of the mediastinum around the trachea (6). Familiarization with accessory fissures is essential because they may be mistaken for a disease condition.
Previous studies showed a wide variation in accessory fissures and lobes occurrence (2, 15, 18). Therefore, it is necessary to review case reports of accessory fissures and lobes in both lungs in the process of autopsy, imaging examination, and surgery. The incidences of accessory fissure and accessory lobe in autopsy or dissection were reviewed in Table 1, in imaging examination as Table 2, and in lung resection surgery as Table 3.

Table 1. The literature reporting lung with accessory fissures and three lobes in autopsy and dissection.
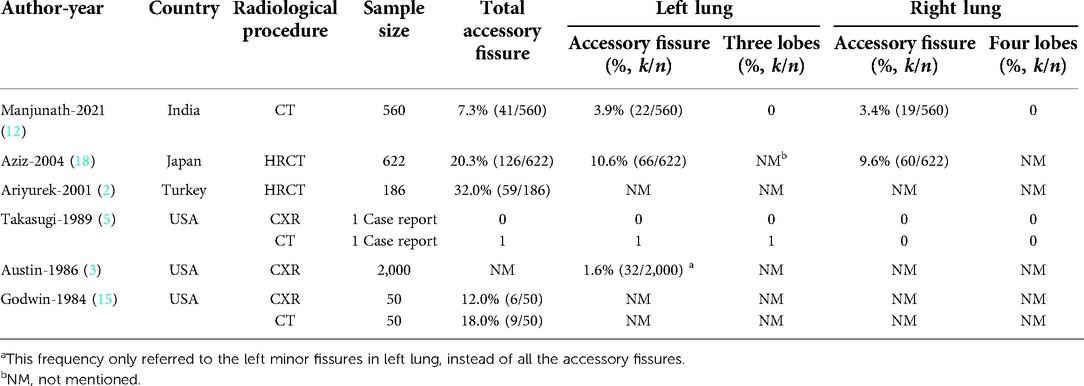
Table 2. The literature reporting lung with accessory fissures and three lobes in radiological procedure including CXR and (HR)CT.
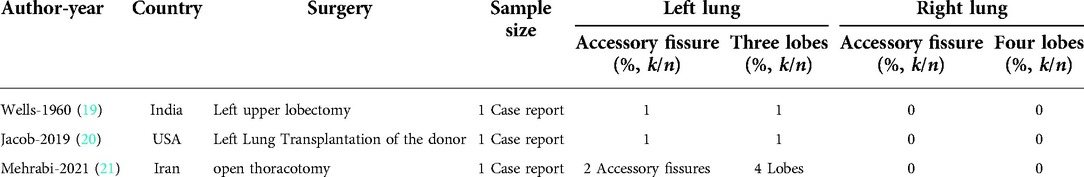
Table 3. The literature reporting lung with accessory fissures and three lobes in lung resection surgery case report.
In ten autopsy and dissection studies from five countries (Table 1), the incidence of accessory fissure in the left lung was 13.5% (79/587, ranging from 2.7% to 50.0%), and in the right lung, it was 7.3% (42/575, ranging from 3.1% to 30.4%). The incidence of accessory lobes in the left lung was 2.0% (11/547, ranging from 0.0% to 7.4%), and in the right lung, it was 2.6% (14/539, ranging from 0.0% to 17.4%). According to the result of the case review, the variation that there were three lobes in the left lung was rare, and the incidence was about 2.0% in the previous studies.
In five radiological studies (Table 2), the incidence of accessory fissures in bilateral lungs found by CXR or CT ranged from 7.3% to 32.0%. There were 20.3% (126/622) (18) to 32.0% (59/186) (2) patients detected with accessory fissures in high-resolution CT (HRCT). 7.3% (41/560) of the patients were detected with an accessory fissure by CT (12). Therefore, the screening effect of CT for accessory fissures might be lower than that of HRCT in the previous study. The effect of CXR to detect accessory fissures might also be worse than CT or HRCT (5, 15).
The accessory lobes discovered in surgeries were reported in three case reports, including a left upper lobectomy (19) in 1960, a left lung transplantation (20) in 2019, and an open thoracotomy (21) in 2021. In history, when the doctors reported meeting the true tri-lobes in the left lung for the first time all around the world (19), the first thought that came to their mind was whether this patient had a “situ inversus.” Nevertheless, when the stomach and heart were in their normal position, as seen in the plain film of the chest, they confirmed that the patient had tri-lobes in the left lung. Moreover, in a left lung transplantation case report (20), the left lung from the donor was recognized with tri-lobes until the surgery team received the lung. In another open thoracotomy case report, the surgeon team (21) reported a bilateral primary spontaneous pneumothorax case that underwent talc slurry and bleomycin pleurodesis at the right and left sides retrospectively, complicated with left-sided recurrent spontaneous pneumothorax. The patient underwent open thoracotomy and was accidentally found to have four lobes and three fissures in the left lung. The knowledge of variant fissures is fundamental, especially in the pre-operative planning of lung surgery.
How and why accessory fissures occurs in the lung is not known. The fissures of the lungs are embryologically separating the bronchopulmonary segments, which later on persist in the interlobar planes of the fully developed lung. All the variations noted in lobulation and fissures in both lungs might result from altered pulmonary development. In humans and other species, including dogs, cats, bovines, horses, et al., the accessory lobes were reported in the previous studies (21). Generally, they are considered to be incidental findings that are not associated with lung symptoms.
Conclusion
To our knowledge, this is the first report of a mislocated lung nodule because of a left lung with three lobes. The presence of this accessory fissure and accessory lobe changed the surgical plan. We reviewed the literature inferring accessory fissures in autopsy, dissection, imaging examination, and surgery. The incidence of three lobes in the left lung was about 2.0%. The radiologists and surgeons should be aware of the accessory lobe possibility.
Author contributions
HL evaluated the patient clinically, operated on the patient (the main surgeon), and read and revised the manuscript. YX evaluated the patient clinically, helped to operate the patient (co-surgeon), prepared the first draft, and revised the manuscript. YQ, DM evaluated the patient clinically andhelped to operate the patient (co-surgeon). XL wrote the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by National High Level Hospital Clinical Research Funding (2022-PUMCH-B-012).
Acknowledgments
We all express our gratitude to the patient, who kindly gave consent for this case to be presented in this paper.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
CXR, chest x-ray; CT, computed tomography; S6, left dorsal segment; S1 + 2, apicoposterior segment; PET/CT, positron emission tomography/CT; SUV, standard uptake value; VATS, video-assisted thoracic surgery; 3D, three-dimensional; HRCT, high-resolution CT.
References
2. Ariyürek OM, Gülsün M, Demirkazik FB. Accessory fissures of the lung: evaluation by high-resolution computed tomography. Eur Radiol. (2001) 11(12):2449–53. doi: 10.1007/s003300100852
3. Austin JH. The left minor fissure. Radiology. (1986) 161(2):433–6. doi: 10.1148/radiology.161.2.3763915
4. Mata J, Cáceres J, Alegret X, Coscojuela P, De Marcos JA. Imaging of the azygos lobe: normal anatomy and variations. AJR Am J Roentgenol. (1991) 156(5):931–7. doi: 10.2214/ajr.156.5.2017954
5. Takasugi JE, Godwin JD. Left azygos lobe. Radiology. (1989) 171(1):133–4. doi: 10.1148/radiology.171.1.2928516
6. Speckman JM, Gamsu G, Webb WR. Alterations in CT mediastinal anatomy produced by an azygos lobe. AJR Am J Roentgenol. (1981) 137(1):47–50. doi: 10.2214/ajr.137.1.47
7. Kc S, Shrestha P, Shah AK, Jha AK. Variations in human pulmonary fissures and lobes: a study conducted in Nepalese cadavers. Anat Cell Biol. (2018) 51(2):85–92. doi: 10.5115/acb.2018.51.2.85
8. Nene AR. Lung lobes and fissures: a morphological study. Anatomy. (2011) 5:30–8. doi: 10.2399/ana.10.005
9. Quadros LS. Variations in the lobes and fissures of lungs – a study in south Indian lung specimens. Eur J Anat. (2014) 18(1):16–20. doi: 10.1177/2050313X19834155
10. Magadum A. Fissures and lobes of lung – an anatomical study and its clinical significance. Int J Cur Res Rev. (2015) 7(3):08–12.
11. Boyden EA. Cleft left upper lobes and the split anterior bronchus. Surgery. (1949) 26(2):167–80.18136869
12. Manjunath M, Sharma MV, Janso K, John PK, Anupama N, Harsha DS. Study on anatomical variations in fissures of lung by CT scan. Indian J Radiol Imaging. (2021) 31(4):797–804. doi: 10.1055/s-0041-1741045
13. Craig SR, Walker WS. A proposed anatomical classification of the pulmonary fissures. J R Coll Surg Edinb. (1997) 42(4):233–4.9276555
14. Aldur MM, Denk CC, Celik HH, Tasçioglu AB. An accessory fissure in the lower lobe of the right lung. Morphologie. (1997) 81(252):5–7.9737903
15. Godwin JD, Tarver RD. Accessory fissures of the lung. AJR Am J Roentgenol. (1985) 144(1):39–47. doi: 10.2214/ajr.144.1.39
16. Meenakshi S, Manjunath KY, Balasubramanyam V. Morphological variations of the lung fissures and lobes. Indian J Chest Dis Allied Sci. (2004) 46(3):179–82.15553206
17. Davis SD, Yu LS, Hentel KD. Obliquely oriented superior accessory fissure of the lower lobe of the lung: CT evaluation of the Normal appearance and effect on the distribution of parenchymal and pleural opacities. Radiology. (2000) 216(1):97–106. doi: 10.1148/radiology.216.1.r00jl4797
18. Aziz A, Ashizawa K, Nagaoki K, Hayashi K. High resolution CT anatomy of the pulmonary fissures. J Thorac Imaging. (2004) 19(3):186–91. doi: 10.1097/01.rti.0000131590.74658.24
19. Wells JA. A left eparterial bronchus and a tri-lobed left lung: a case report. Dis Chest. (1960) 37:129–31. doi: 10.1378/chest.37.1.129
20. Jacob S, Makey IA, El-Sayed Ahmed MM, Mallea JM, Erasmus DB, Belli EV. Transplantation of a three-lobed donor left lung: a case report. SAGE Open Med Case Rep. (2019) 7:1–3, 2050313X19834155.
21. Mehrabi S, Tanideh N, Hosseinpour R, Irajie C, Yavari Barhaghtalabi MJ. A left lung with four lobes: a new discovery during the thoracotomy for recurrent primary spontaneous pneumothorax. J Cardiothorac Surg. (2021) 16(1):276. doi: 10.1186/s13019-021-01651-3
22. Channabasanagouda HM. Types of pulmonary fissures and its surgical implications: A cadaveric study. Indian J Clin Anat Physiol. (2020) 7(1):72-6. doi: 10.18231/j.ijcap.2020.016
23. Unver Dogan N, Uysal II, Demirci S, Dogan KH, Kolcu G. Major anatomic variations of pulmonary fissures and lobes on postmortem examination. Acta Clin Croat. (2015) 54(2):201-7.26415317
24. George BM, Nayak SB, Marpalli S. Morphological variations of the lungs: a study conducted on Indian cadavers. Anat Cell Biol. (2014) 47(4):253-8. doi: 10.5115/acb.2014.47.4.253
25. Esomonu UG, Taura MG, Modibbo MH, Egwu AO. Variation in the lobar pattern of the right and left lungs: a case report. Australas Med J. (2013) 6(10):511-4. doi: 10.4066/AMJ.2013.1856
26. Murlimanju BV, Prabhu LV, Shilpa K, Pai MM, Kumar CG, Rai A, et al.. Pulmonary fissures and lobes: a cadaveric study with emphasis on surgical and radiological implications. Clin Ter. (2012) 163(1):9-13.22362226
Keywords: lung cancer surgery, diagnosis, lung cancer, CT scan, computed tomography, chest, anatomy
Citation: Lyu X, Xu Y, Qin Y, Ma D and Liu H (2023) A pulmonary nodule mislocated in “dorsal” segment due to tri-lobed left lung. Front. Surg. 9:1069543. doi: 10.3389/fsurg.2022.1069543
Received: 14 October 2022; Accepted: 25 October 2022;
Published: 6 January 2023.
Edited by:
Eugenio Pompeo, University of Rome Tor Vergata, ItalyReviewed by:
Luca Frasca, Campus Bio-Medico University, ItalyH. Volkan Kara, Istanbul University-Cerrahpasa, Turkey
© 2023 Lyu, Xu, Qin, Ma and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongsheng Liu aG9uZ3NoZW5nbGl1MTZAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
Specialty Section: This article was submitted to Thoracic Surgery, a section of the journal Frontiers in Surgery
 Xiaohong Lyu
Xiaohong Lyu Yuan Xu1,†
Yuan Xu1,†