- 1Orthopedics and Traumatology, The First Affiliated Hospital of Zhejiang Chinese Medical University(Zhejiang Provincial Hospital of Chinese Medicine), Hangzhou, China
- 2Shi's Center of Orthopedics and Traumatology, Shuguang Hospital Affiliated to Shanghai University of Traditional Chinese Medicine, Shanghai, China
- 3The First School of Clinical Medicine, Zhejiang Chinese Medical University, Hangzhou, China
Background: Total knee arthroplasty (TKA) is recommended for haemophilic patients with end-stage arthritis. TKA combined with a one-stage extraarticular osteotomy is uncommon in the treatment of haemophilic arthritis (HA) with severe extra-articular deformities (EADs) and a history of inhibitors under the guidance of a patient-specific cutting guide (PSI).
Case presentation: We reported a 20-year-old male patient with severe haemophilia, limited knee functionality, a 30° sagittal deformity on the femoral side and a history of inhibitors. We adopted the Van Creveld protocol to decrease the inhibitors. TKA and extra-articular osteotomy (EAO) were performed simultaneously and sequentially under the guidance of PSI. An appropriate central alignment of the lower limb was restored by using cement prostheses with antibiotics and femur shaft locking compression plates. The last follow-up showed that the knee function was good, the VAS score was 0, the WOMAC score was 18 and the ROM was 0°–95°.
Conclision: Regular haematology management can reduce the perioperative bleeding risk in haemophilic patients treated with inhibitors. PSI plays an important role in guiding the TKA and EAO of end-stage HA patients with severe EAD.
Introduction
More than 80% of bleeding in haemophilia patients occurs in the musculoskeletal system (1). Repeated spontaneous bleeding leads to irreversible damage to the joints, which eventually progresses to haemophilic arthropathy (HA). As HA progresses, pain, loss of joint movement, and progressive deformities will become apparent, which seriously affect the quality of life of haemophilia patients. Due to their coagulation dysfunction and the high cost of coagulation factors, some patients receive nonsurgical treatment after fractures, which may lead to the occurrence of an extra-articular deformity (EAD).
EAD can change the distribution of the mechanical load on the knee joint and accelerate the occurrence of arthritis (2). Total knee arthroplasty (TKA) is challenging due to the influences of the abnormal stress, anatomical structures, and soft tissue conditions for HA with severe EAD. Surgical options include a TKA combined with extra-articular osteotomy (EAO) or an intra-articular compensatory osteotomy (3). Most scholars (4–6) believe that a TKA combined with an EAO should be considered when the angle of coronal or sagittal deformity on the femoral side is greater than 20 to avoid an excessive intra-articular osteotomy, a poor mechanical axis (MA) and joint instability. Patient-specific cutting guides (PSIs) provide a new solution for HA with severe EADs during TKA (6).
We report a case of a patient with severe haemophilia, sagittal deformity (30°) on the femoral side and a history of inhibitor usage.
Case presentation
A 20-year-old male presented with pain and limited motion in the right knee for 15 years. The patient presented to our clinic with HA, restricted flexion and extension of the right knee and a sagittal deformity of the right femur 8 months prior to the surgery. He was diagnosed with severe haemophilia A (coagulation factor VIII was 1.52%) and haemophilic arthritis of right knee. At the age of 13, the patient was fixed with plaster for a fracture of the femoral shaft, which resulted in a malunion.
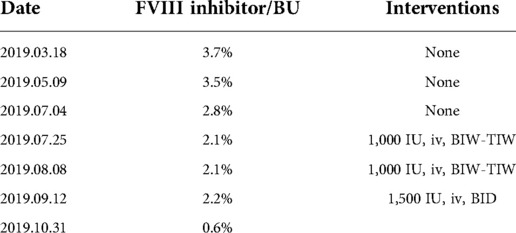
Because he was positive for inhibitors, the patient was re-examined regularly by the Haematology Clinic after discharge. The patient did not take any interventions during the first 4 months while being positive for inhibitors. During this period, the patient suffered from knee joint bleeding and recovered after ice compression and lying in bed. In the 5th month after the discovery of the inhibitors, the patient received irregular injections of factor VIII intravenously (1,000 IU, BIW or TIW, Kovaltry, Bayer), which did not follow the haematologist's recommendation. After 66 days of injections, he was still positive for inhibitors. Since then, the patient started to receive regular injections of factor VIII (1,500 IU, BID) intravenously. Forty-nine days after the first injection, he became negative for inhibitors (Table 1). The patient came to the hospital again 3 days prior to the surgery.
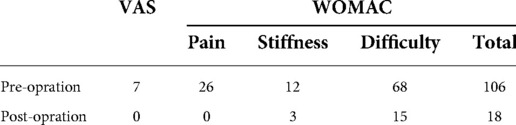
Preoperative examinations showed the patient had pain in his right knee. His right foot could not touch the ground. The range of joint motion (ROM) was 20°–90°, the visual analogue scale (VAS) was 7 and the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) was 106 (Figure 1, Table 2). Other systemic examinations were normal. X-ray and CT showed that the patient's right knee joint space was narrow, with a right femoral flexion deformity (30°, sagittal, anterior) (Figure 2).

Figure 1. (A,B) Preoperative appearance of the right lower limb which shows that the right foot cannot touch the ground; (C,D) preoperative range of joint motion (20°–90°); (E–G) postoperative appearance of the right lower limb and the right foot touching the ground; (H,I) postoperative range of joint motion (0°–95°).
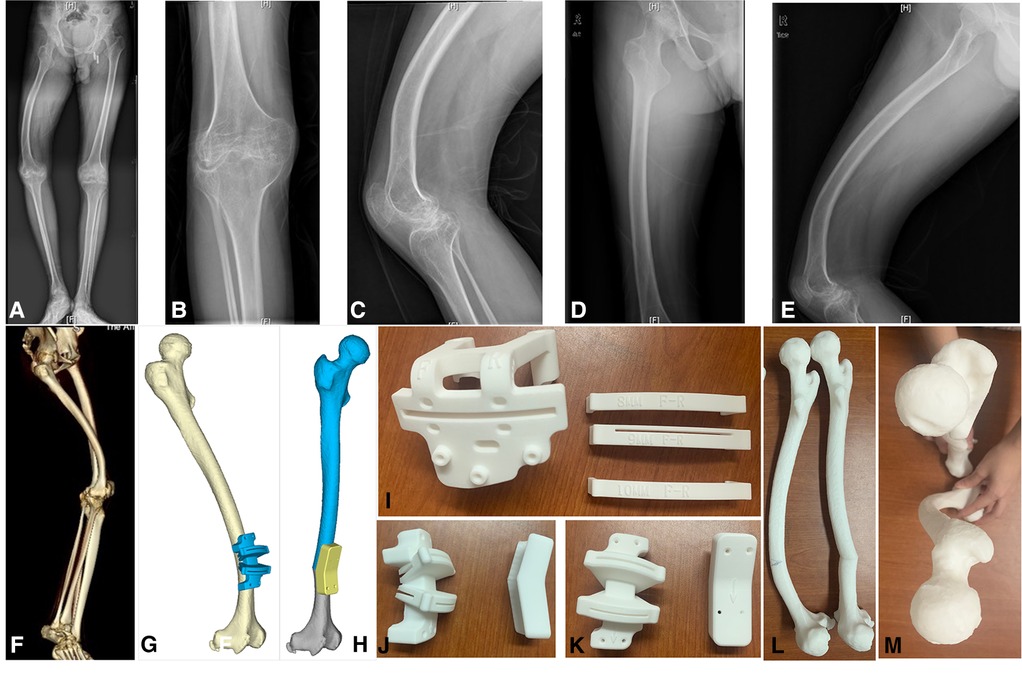
Figure 2. (A) Full-length x-rays of both lower limbs (weight-bearing); (B–E) anteroposterior and lateral x-rays of the knee joints and femur. The sagittal deformity angle of the femur was 30° (anterior); (F) full-length computer tomography film of right lower limb; (G,H) computer model of distal femoral osteotomy; (I) distal femur osteotomy guide plate in TKA; (J, K) osteotomy and reduction guide plate for extra-articular deformities; (L,M) models of femur in lateral and overhead positions after the osteotomy.
Treatment
Considering the cost, risk and degree of deformity, we decided to carry out a TKA combined with a one-stage EAO under the guidance of PSI to correct the deformity and restore joint function. 3D modelling of the full-length CT of the lower limbs was completed by Arigin 3D STS Design Software (Figure 2). Considering of the possible internal fixation failure and implant failure during TKA, we plan to conduct TKA first, and then perform extra-articular osteotomy. The advantage of this scheme is that the extra-articular osteotomy can adjust the MA again after TKA.
The surgery was performed in the supine position. A tourniquet (40 kPa) was used during the operation. The incision site was at the mid-level knee with a medial patellar approach. According to the bony landmarks of the distal femur, the distal femoral osteotomy was completed by PSI. Neutral tibial resection without PSI was performed for the proximal tibia. External rotation resection (3°) and “4 in 1” guide resection were performed at the 90° position of knee flexion. The patella was not resurfaced, but osteophyte cleaning and denervation were achieved. A cement implant containing vancomycin was placed (PS implant, Stryker Scorpio NRG Knee System).
The incision was extended approximately 15 cm along the proximal femur. Exposure of the deformed segment and bony landmark of the distal femur was made along the lateral femoral muscle space. The PSI was placed in the correct position. A closed osteotomy (30°) was performed on the front of the femur, and the posterior hinge was cut off. A femoral reduction plate was used to fit the osteotomy ends of the femur, which were fixed temporarily by Kirschner wires. After removing the femoral reduction guide plate, a femur shaft locking compression plate (Wego) was placed on the lateral side of the femur. The tourniquet was loosened, and the bleeding was stopped at the visible bleeding points. Layer by layer, the incision was sutured. The joint cavity was injected with 50 ml of normal saline containing 0.8 g of tranexamic acid after the congestion of the joint cavity was removed. The knee joint was bandaged with cotton pads and elastic bandages. After returning to the ward, the knee was immediately iced for 5 days (Figure 3).
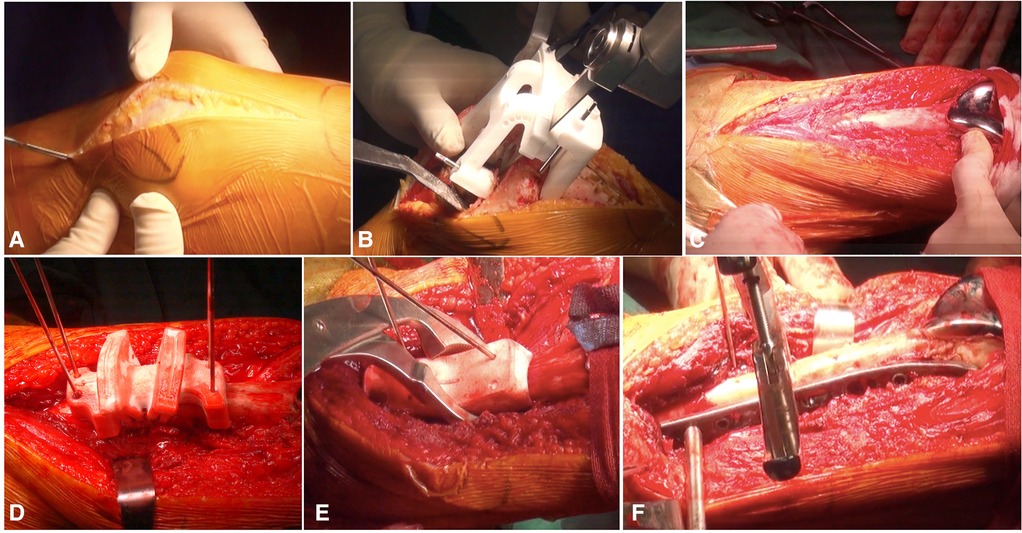
Figure 3. (A) Total knee arthroplasty approach; (B) the distal femoral osteotomy was guided by PSI; (C) the incision was lengthened; (D) the femoral shaft osteotomy by patient-specific cutting guide; (E) femoral shaft closed reduction was guided by femoral reduction guide plate; (F) fixation of osteotomy site.
We followed our haematological management protocol, which involves 80%–100% correction of Factor VIII before surgery, with the same dose repeated after 8 h. Daily correction of 80%–100% was provided twice a day for 2 days. Then, the patient was evaluated on the third day by the haematologist, and the dose was modified to a 40%–80% correction daily for 5 days. From the 8th day, supplementation with at least 30% correction was performed before each manipulation and rehabilitation training. We performed inhibitor tests before surgery, 3 days after surgery, 1 week after surgery, and before discharge because of the positive history for inhibitors.
Outcome and follow-up
For this patient, we developed an individualized rehabilitation plan. On the first day after the operation, the rehabilitation physician and physical therapist began to intervene, guiding the patient to perform active foot extensions and leg raising exercises under the protection of a brace. From the 3rd day after surgery, active knee flexion and extension exercises and partial weight-bearing were allowed. A continuous passive motion machine was used under the guidance of a rehabilitation specialist. The patient could completely bear weight beginning in postoperative week 12. Within 30 min after the rehabilitation exercise, an ice compress was applied to the surgical site to reduce bleeding and pain. The last follow-up showed that the knee function was good, the VAS was 0, the WOMAC was 18 (Table 2) and the ROM was 0°–95° (28 months) (Figures 1, 4).
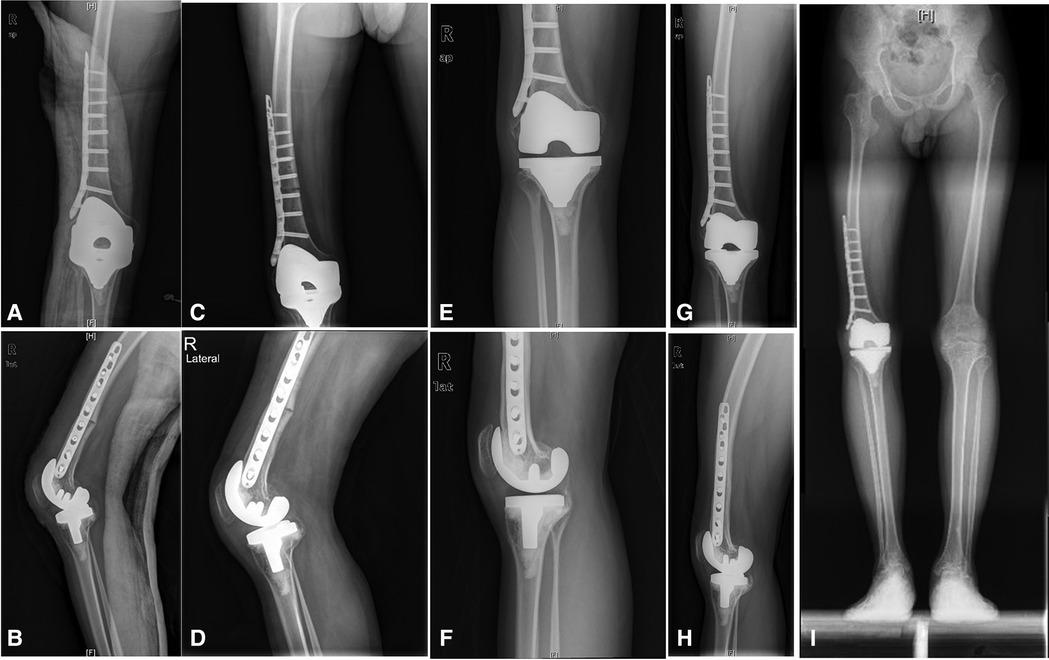
Figure 4. (A,B) Postoperative knee and femur x-rays at 3 days; (C,D) postoperative x-rays at 7 months; (E–H) postoperative x-rays at 23 months; (I) full-length x-rays of both lower limbs in weight-bearing positions at 23 months after surgery.
Discussion and review of literatures
We reported a haemophilia patient with inhibitors and end-stage HA who underwent a TKA and osteotomy for severe femoral side deformities with the aid of PSI synchronously.
Haemophilia patients develop end-stage arthritis at a younger age than ordinary arthritis patients. When nonsurgical treatment does not provide satisfactory pain relief and functional improvements, WFH recommends surgical intervention (1). TKA in haemophilic patients is challenging because of the special features of haemophilic patients compared to primary KOA, such as tendencies for bleeding, abnormal bone structures, osteopenia, and a poor soft tissue condition (7).
Patients with FVIII/FIX inhibitors face a higher risk of bleeding during treatment and higher treatment-related costs (8, 9). Despite good results among haemophilia patients with inhibitors (10–12) surgical intervention for haemophilia patients with inhibitors, especially those with high response inhibitors, is limited to emergency treatment of life- or limb-threatening clinical conditions (13). There are different strategies for performing surgical procedures in inhibitor patients (1). The eradication of antibodies through immune tolerance induction (ITI) is still the preferred management strategy for treating inhibitor patients, such as the Bonn scheme, the Van Creveld scheme and the Malmö scheme (14). However, some patients are unresponsive to ITI (15). The inhibitor concentration in this patient was <5.0 BU, which is a low-responding inhibitor. In some patients with low-response inhibitors, the inhibitor would disappear by itself within 6 months (14, 16). It has been proven to be useful for us to control bleeding by eliminating persistent inhibitors by the Van Creveld scheme, which strengthens the perioperative management of coagulation factors and the detection of inhibitors.
EAD was the main surgical challenge for this patient. EAD is mostly secondary to fracture malunion, metabolic bone disease and congenital malformations, accounting for 12% of TKAs (17). The incidence of nonsurgical treatment after fractures in haemophilia patients is higher than that in nonhemophilia patients, which may increase the risk of an EAD. The TKA of knee with EAD can be completed by intra-articular osteotomy, primary or secondary extra-articular osteotomy. Intra-articular osteotomy has the advantages of short operation time, less trauma, quick recovery and fewer complications, but it is limited by the angle of deformity. Although extra-articular osteotomy is not limited by the angle of deformity, there are risks of poor or nonunion of the osteotomy site, increased operation time and cost, delayed rehabilitation and increased infection. For HA patients with severe EAD, simultaneous EAO and TKA can reduce costs and accelerate the return to normal life (6). However, a prolonged operation time and increased tissue damage will increase the risk of bleeding and infection (18, 19). Simultaneous osteotomy and TKA could increase the infection rate, although there are no studies that address this question. We routinely use vancomycin-loaded cement to prevent infection. In addition, we take measures such as supplementation with factor VIII, the use of tourniquets, maintain adequate haemostasis, use tranexamic acid retention perfusion (20), and use compression bandaging and local ice to prevent perioperative blood loss during TKA.
PSI is of great significance for TKA with severe EAD because the osteotomy guide cannot be accurately positioned. Regardless of single-plane or multiplane deformities, PSI can plan the angle and direction of the osteotomy using computer guidance to reduce errors caused by visual observation and operator experience. Lv et al. (6) used PSI to complete 9 cases of TKA with EAD on the femoral side. The follow-up results showed that PSI could effectively restore the lower limb line of force, simplify the operation process, and shorten the operation time.
After orthopaedic surgery, patients should undergo rehabilitation as early as possible, including haemophilia patients. The rehabilitation plan should be jointly decided by a team of haematology specialists, rehabilitation specialists, physical therapists and orthopaedic specialists. Postoperative rehabilitation can help with functional recovery. Inappropriate rehabilitation programs and coagulation factor concentrations will increase the risk of bleeding, which will seriously affect the postoperative joint function and rehabilitation progress (8, 21). In our opinion, the minimum concentration of the coagulation factor should be maintained above 30% during rehabilitation, even if the patient has been discharged from the hospital.
Inhibitor management, surgical planning of HA with severe EAD, individualized rehabilitation and perioperative bleeding risk management were difficulties in the treatment of this haemophilic patient. We consulted haematology experts to complete the cleaning of inhibitors and guide perioperative management of the coagulation factors. With the help of PSI, the TKA and EAO were completed at the same time. PSI can reduce intraoperative bleeding and infection by reducing the difficulty of intraoperative localization and the operation time. Under the guidance of rehabilitation experts and physiotherapists, individualized rehabilitation plans can reduce the risk of bleeding and fracture and obtain good joint function. Since this article is a single case report, the postoperative efficacy and safety of this approach need to be confirmed by a study using a larger sample size.
Conclusion
Regular haematology management can reduce the perioperative bleeding risk in haemophilic patients treated with inhibitors. With PSI, haemophilic patients who have severe EAD can complete TKA and EAO at the same time, thereby obtaining good postoperative joint function.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of the First Affiliated Hospital of Zhejiang Chinese Medical University(2021-KL-007-02). The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
P-JT, XL and S-JL conceived and coordinated the study and wrote the paper. Z-MW, H-KJ, and RW carried out the data collection and analysis and revised the paper. XL, P-JT and S-JL prepared and implemented the operation. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Srivastava A, Santagostino E, Dougall A, Kitchen S, Sutherland M, Pipe SW, et al. Wfh guidelines for the management of hemophilia, 3rd edition. Haemophilia. (2020) 26(Suppl 6):1–158. doi: 10.1111/hae.14046
2. Deschamps G, Khiami F, Catonné Y, Chol C, Bussière C, Massin P. Total knee arthroplasty for osteoarthritis secondary to extra-articular malunions. Orthop Traumatol Surg Res. (2010) 96(8):849–55. doi: 10.1016/j.otsr.2010.06.010
3. Catonné Y, Sariali E, Khiami F, Rouvillain JL, Wajsfisz A, Pascal-Moussellard H. Same-Stage total knee arthroplasty and osteotomy for osteoarthritis with extra-articular deformity. Part I: tibial osteotomy, prospective study of 26 cases. Orthop Traumatol Surg Res. (2019) 105(6):1047–54. doi: 10.1016/j.otsr.2019.04.010
4. Loures FB, Correia W, Reis JH, Pires EARS, de Paula Mozela A, de Souza EB, et al. Outcomes after knee arthroplasty in extra-articular deformity. Int Orthop. (2019) 43(9):2065–70. doi: 10.1007/s00264-018-4147-9
5. Wolff AM, Hungerford DS, Pepe CL. The effect of extraarticular Varus and Valgus deformity on total knee arthroplasty. Clin Orthop Relat Res. (1991) 271:35–51. doi: 10.1097/00003086-199110000-00007
6. Lü SJ, Tong PJ, Huang JF, Liu X, Zhang SX, Wang J, et al. Clinical effect of one-stage total knee arthroplasty for knee osteoarthritis with femoral extra-articular deformity. Zhonghua Yi Xue Za Zhi. (2020) 100(31):2429–34. doi: 10.3760/cma.j.cn112137-20200110-00073
7. China TJSBotCOAHTCCN. Guideline for perioperative management in hemophilic arthropathy patients undergoing hip and/or knee arthroplasty in China. Chinese Journal Bone and Joint Surgery. (2022) 15(7):481–90. doi: 10.3969/j.issn.2095-9958.2022.07.01.
8. Solimeno LP, Escobar MA, Krassova S, Seremetis S. Major and Minor classifications for surgery in people with hemophilia: a literature review. Clin Appl Thromb Hemost. (2018) 24(4):549–59. doi: 10.1177/1076029617715117
9. Renchi Y. Chinese Guidelines on the treatment of hemophilia (version 2020). Zhonghua Xue Ye Xue Za Zhi. (2020) 41(4):265–71. doi: 10.3760/cma.j.issn.0253-2727.2020.04.001
10. Rodriguez-Merchan EC, Rocino A. Literature review of surgery management in inhibitor patients. Haemophilia. (2004) 10(Suppl 2):22–9. doi: 10.1111/j.1365-2516.2004.00937.x
11. Goudemand J, Tagariello G, Lopaciuk F. Cases of surgery in high-responder haemophilia patients. Haemophilia. (2004) 10(Suppl 2):46–9. doi: 10.1111/j.1365-2516.2004.00940.x
12. Jenkins PJ, Ekrol I, Lawson GM. Total knee replacement in patients with haemophilia: the Scottish experience. Scott Med J. (2013) 58(4):223–7. doi: 10.1177/0036933013507870
13. Ilg A, Stahlschmidt K, Zotz RB, Krauspe R, Scharf RE, Gerhardt A. Interdisciplinary management of total knee replacement in a haemophilia patient with high-titre inhibitor and severe arthropathy complicated by an aneurysmatic bone cyst. Haemophilia. (2009) 15(1):377–9. doi: 10.1111/j.1365-2516.2008.01861.x
14. Thrombosis and Hemostasis Group CSoH, Chinese Medical Association, Hemophilia Treatment Center Collaborative Network of China. Chinese Guidelines on the diagnosis and treatment of coagulation factor VIII/IX inhibitors (version 2018). Zhonghua Xue Ye Xue Za Zhi. (2018) 39(10):793–9. doi: 10.3760/cma.j.issn.0253-2727.2018.10.001
15. Ljung R, Auerswald G, Benson G, Dolan G, Duffy A, Hermans C, et al. Inhibitors in haemophilia a and B: management of bleeds, inhibitor eradication and strategies for difficult-to-treat patients. Eur J Haematol. (2019) 102(2):111–22. doi: 10.1111/ejh.13193
16. Carulli C, Innocenti M, Linari S, Morfini M, Castaman G, Innocenti M. Joint replacement for the management of haemophilic arthropathy in patients with inhibitors: a long-term experience at a single haemophilia centre. Haemophilia. (2021) 27(1):e93–e101. doi: 10.1111/hae.14169
17. Bala A, Penrose CT, Seyler TM, Mather RC 3rd, Wellman SS, Bolognesi MP. Outcomes after total knee arthroplasty for post-traumatic arthritis. Knee. (2015) 22(6):630–9. doi: 10.1016/j.knee.2015.10.004
18. Rodríguez-Merchán EC. Total knee arthroplasty in hemophilic arthropathy. Am J Orthop (Belle Mead NJ). (2015) 44(12):E503–7. PMID: 26665252
19. Silva M, Luck JV Jr. Long-Term results of primary total knee replacement in patients with hemophilia. J Bone Joint Surg Am. (2005) 87(1):85–91. doi: 10.2106/jbjs.C.01609
20. Wang R, Wang Z, Gu Y, Zhang J, Wang P, Tong P, et al. Total knee arthroplasty in patients with haemophilic arthropathy is effective and safe according to the outcomes at a mid-term follow-up. J Orthop Traumatol. (2022) 23(1):31. doi: 10.1186/s10195-022-00648-5
Keywords: haemophilic arthritis, extra-articular deformity, PSI, total knee arthroplasty, case report
Citation: Lv S, Wang Z, Wang R, Jin H, Tong P and Liu X (2023) Total knee arthroplasty and femoral osteotomy with a patient-specific cutting guide to treat haemophilic arthritis with severe extra-articular deformity: A case report and review of literatures. Front. Surg. 9:1067306. doi: 10.3389/fsurg.2022.1067306
Received: 11 October 2022; Accepted: 7 November 2022;
Published: 6 January 2023.
Edited by:
Longpo Zheng, Tongji University, ChinaReviewed by:
Yu Xiuchun, 960th Hospital of the PLA, ChinaPei Yang, The Second Affiliated Hospital of Xi'an Jiaotong University, China
© 2023 Lv, Wang, Wang, Jin, Tong and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xun Liu MzUxNjUzMTYxQHFxLmNvbQ==
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Shuai-Jie Lv
Shuai-Jie Lv Zheng-Ming Wang
Zheng-Ming Wang Rui Wang
Rui Wang Heng-Kai Jin
Heng-Kai Jin Pei-Jian Tong1
Pei-Jian Tong1