- 1Department of Spine Surgery, The Third Hospital of Hebei Medical University, Shijiazhuang, China
- 2Department of Orthopedic Surgery, Hebei General Hospital, Shijiazhuang, China
- 3School of Chemical Engineering, The University of Queensland, QLD, Brisbane, Australia
Purpose: The purpose of this study is to investigate the clinical effect of posterior lumbar fusion surgery on patients who suffer from lumbar disc herniation concurrent with peroneal nerve paralysis.
Methods: The patients suffering from peroneal nerve paralysis and undergoing posterior lumbar fusion surgery between January 2012 and December 2019 were retrospectively reviewed. The data of the identified patients were then collected and processed. All patients were followed up post-operatively after discharge from the hospital. The data was analyzed in terms of Oswestry disability index (ODI), visual analogue scale (VAS) score, and relative lower-limb muscle strength.
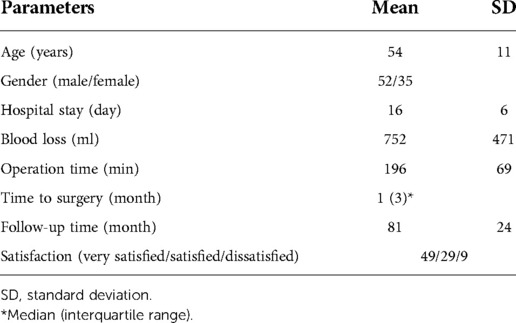
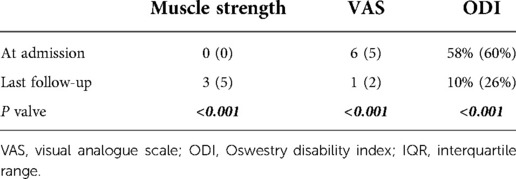
Results: A total of 87 patients (52 males and 35 females) aged 54 ± 11 years met the inclusion criteria for this study. These patients stayed in hospital for 16 ± 6 days and were followed up for 81 ± 24 months. Data analysis showed that muscle strength of the tibialis anterior and extensor digitorum significantly recovered at the last follow-up with a grade of 3 (median), compared to grade 0 at admission (p < 0.001). Furthermore, the median VAS score decreased to 1 at the last follow-up from 6 at admission (p < 0.001), and the ODI greatly improved with 10% (median) at the last follow-up, while it was 58% at admission (p < 0.001). The ODI improvement rate was 60% on average at the last follow-up. Multivariate regression analysis regarding the ODI and muscle strength improvement rates showed that advanced age was a risk factor for postoperative recovery.
Conclusions: Most of the patients suffering from lumbar disc herniation concurrent with peroneal nerve paralysis can improve after undergoing posterior lumbar fusion surgery, but few can reach full recovery. Advanced age might be a risk factor that affects the prognosis of these patients after surgery.
Introduction
In clinical scenarios, lumbar disc herniation (LDH) has a high incidence, most cases being caused by intervertebral disc degeneration (IVDD) (1–3). LDH can lead to lower back pain (LBP), radicular pain and numbness of lower limbs, and even peroneal nerve paralysis (4–7). The clinical symptoms caused by peroneal nerve paralysis include foot and toe (hallux) drop, which results from weakness of ankle (tibialis anterior) and toe dorsiflexion (extensor digitorum) (8). Foot drop has been reported to have an incidence of 0.6%–7.7% in lumbar IVDD diseases, most of which are LDH cases (9).
For these LDH patients with peroneal nerve paralysis, lumbar surgeries are usually performed to remove the herniated nucleus pulposus (the disc), decompress the nerve root and enlarge spinal canal. Nowadays, posterior lumbar surgery, with or without interbody fusion, is widely used to treat LDH, particularly for those cases concurrent with peroneal nerve paralysis (10). However, some previous studies indicated that patients after lumbar surgery might experience prolonged LBP which significantly lowers their quality of life (11–14). Although there have been some studies on LDH-induced peroneal nerve paralysis so far, it is still difficult to make definitive conclusions based on these studies considering the variety of surgical procedures used (4).
Thus, the purpose of this study is to investigate the clinical effect of posterior lumbar fusion surgery on patients who suffered from LDH concurrent with peroneal nerve paralysis.
Patients and methods
Ethics
This retrospective study has been approved by Medical Ethics Council of the Third Hospital of Hebei Medical University (approval no. K2022-127-1). All informed consent was obtained from the patients (or their lawful guardians).
Patients
The patients who were diagnosed with LDH and peroneal nerve paralysis between January 2012 and December 2019 were retrospectively reviewed. All participants in this study underwent posterior lumbar fusion surgery (Figure 1) as previously reported (15). The data of the identified patients were then collected and processed. All patients were followed up after discharge from the hospital.

Figure 1. A representative case of posterior fusion surgery. (A,B) Preoperative x-ray radiographs; (C,D) preoperative CT scans of L4-5 and L5-S1, respectively; (E) preoperative MRI scan (sagittal plane); (F,G) preoperative MRI scans of L4-5 and L5-S1, respectively (axial plane); (H,I) postoperative x-ray radiographs. The arrows indicate the herniation of intervertebral disc.
Assessment
The data collected in this study included baseline data and functional parameters. Baseline data consisted of age, gender, hospital stay, blood loss, operation time, follow-up time, and patient satisfaction. Functional parameters included Oswestry disability index (ODI), visual analogue scale (VAS) score, and lower-limb muscle strength. The lower-limb muscle strength was scored and analyzed by assessing muscle strength of the tibialis anterior and extensor digitorum, using the muscle scale established by the Medical Research Council (16). Foot drop and toe drop are defined as muscle strength below or equal to grade 3 (out of 5) (17). Additionally, the patients' satisfaction was collected and graded to three levels; dissatisfied, satisfied, and very satisfied.
ODI improvement rate was calculated using the equation (18, 19):
Muscle strength improvement rate was calculated using the equation:
To identify the risk factors that affect postoperative recovery, multivariate regression analyses were performed in terms of the ODI improvement rate and muscle strength improvement rate, respectively.
Statistics
SPSS for Windows 18.0 (SPSS Inc, US) was used for statistical analysis in this study. The data of ODI, VAS score and muscle strength is presented as median and interquartile range (IQR). The other data is presented as mean ± standard deviation (SD). Mann–Whitney U tests were used to analyze ODI, VAS score and muscle strength between pre-operation and post-operation. In addition, multivariate regression analyses (Enter method)were performed to identify the risk factors that would affect postoperative recovery in terms of the ODI improvement rate and muscle strength improvement rate, respectively. p values less than 0.05 were regarded as significant.
Results
Baseline data
After screening and review of the patients who had undergone lumbar fusion surgeries between January 2012 and December 2019, a total of 87 patients were identified and included in this study. As shown in Table 1, there are 52 males and 35 females. The age of these participants was 54 ± 11 years. The hospital stay was 16 ± 6 days, and blood loss was 752 ml on average. Operation time was 196 min on average, and the follow-up time for these patients was 81 ± 24 months. Median time to surgery was 1 month. Among all participants, most were very satisfied or satisfied about their treatment effects (78 in 87) and only 9 patients were dissatisfied.
Interbody fusions
As shown in Figure 2A, all participants underwent posterior lumbar interbody fusion surgeries. Among all 87 patients, 28 underwent L4-5 fusions, 24 underwent L4-S1 fusions, 14 underwent L3-5 fusions, and 21 underwent other segments’ fusions. As shown in Figure 2B, there were a total of 139 interbody fusions performed across all 87 patients. The majority of these fusions were L4-5 fusions and L5-S1 fusions, while the fusions of L3-4 and L2-3 were less common.
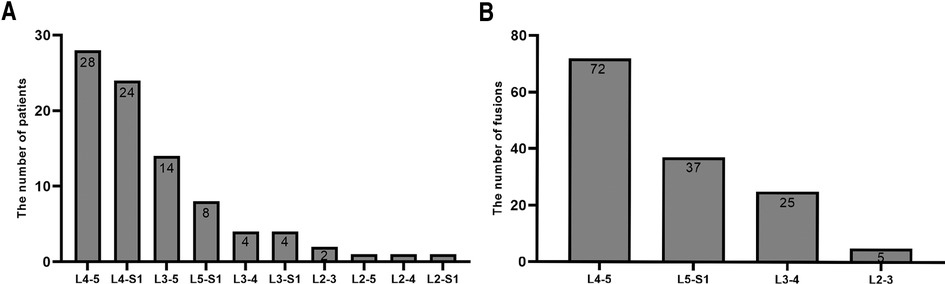
Figure 2. Lumbar fusions performed to the patients. (A) The number of patients in terms of fusions; (B) the number of lumbar fusions in terms of every fused segment.
Muscle strength and improvement rate
As shown in Figure 3, 66 of 87 patients were at grade 0 muscle strength of the tibialis anterior and extensor digitorum at admission, and 40 of the 87 patients improved to grades 4 or 5 at the last follow-up. Among 87 patients, 56 (64.4%)improved their muscle strength. As shown in Table 2, overall, the median preoperative muscle strength of the tibialis anterior and extensor digitorum was grade 0 at admission and grade 3 at the last post-operative follow-up. Compared to the preoperative gradings, the patients' muscle strength significantly recovered after surgery (p < 0.001). Muscle strength improvement rate was 50% on average at the last follow-up.
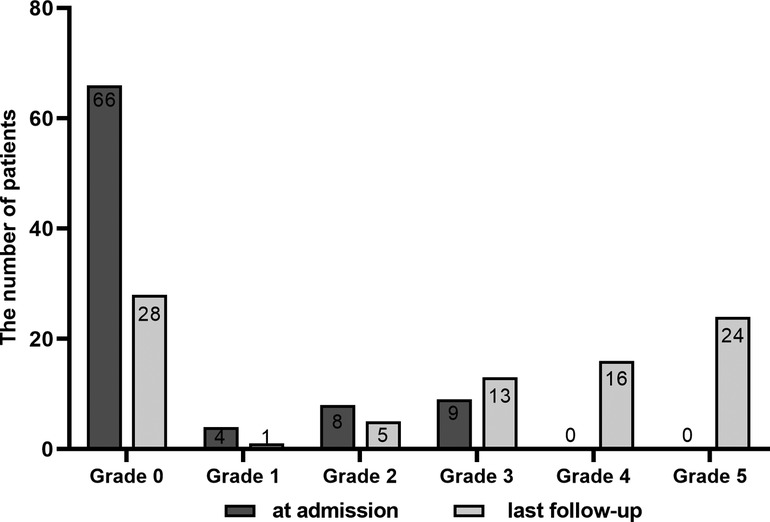
Figure 3. Comparison of muscle strength between pre-surgery (at admission) and last follow-up after surgery.
VAS score
As shown in Table 2, the median VAS score of the patients was 6 at admission. By contrast, the median VAS score decreased to 1 at the last post-operative follow-up. Statistical analysis showed that the patients' post-operative VAS score significantly decreased compared with pre-operation (p < 0.001).
ODI and ODI improvement rate
As shown in Table 2, the patients' median ODI was 58% at admission, and decreased to 10% at the last post-operative follow-up (p < 0.001). The ODI improvement rate was 60% on average at the last follow-up.
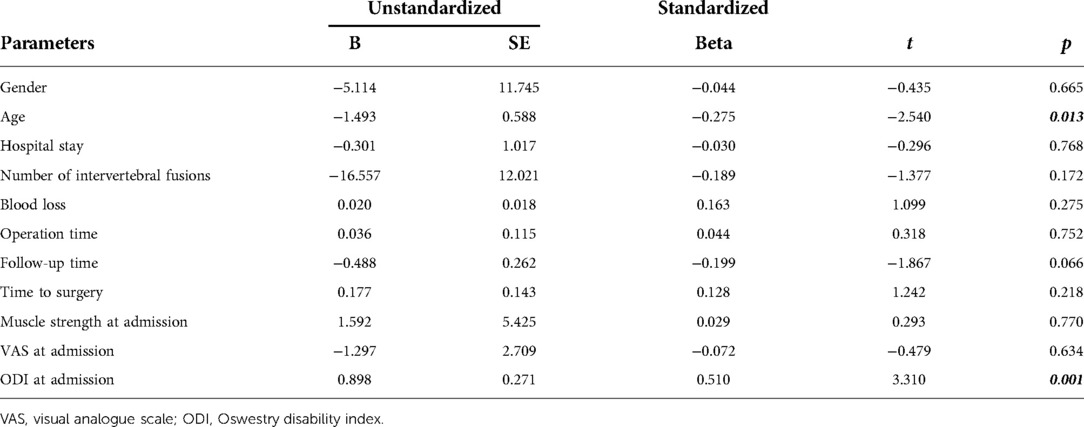
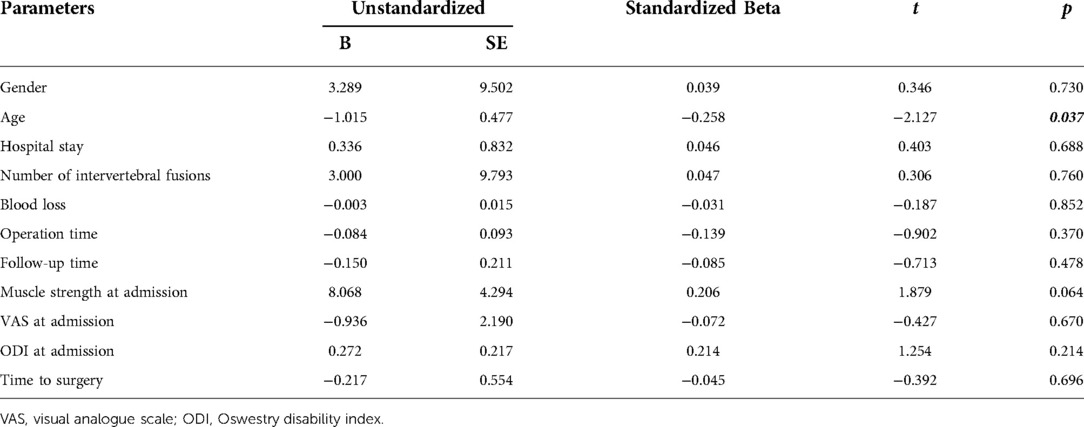
Multivariate regression analysis
In this study, multivariate regression analysis was performed to identify risk factors that may influence the recovery of the patients after surgery. In the regression analyses, ODI improvement rate and muscle strength improvement rate were used as the dependent variables, respectively. It showed that advanced age was a risk factor that might affect the final ODI improvement rate and muscle strength improvement rate (both p < 0.05), as shown in Tables 3, 4.
Discussion
Clinically, pathological changes in neural structures that influence the dorsiflexion of ankle would cause peroneal nerve paralysis, such as nerve compression, trauma, infection, tumor, and external oppression (5). LDH is one of the common diseases that lead to peroneal nerve paralysis (7, 8). Clinical symptoms caused by peroneal nerve paralysis usually include foot and toe (hallux) drop, resulting from weakness of the ankle (tibialis anterior) and toe (extensor digitorum) dorsiflexion. As previously reported, L4-5 disc herniation is the most common LDH that causes peroneal nerve paralysis, and L5-S1 disc herniation contributes 25% of cases with peroneal nerve paralysis (4, 5). In clinical settings, these LDH patients need to undergo lumbar spine surgeries regardless of interbody fusions. In the current study, we retrospectively collected 87 patients who underwent posterior lumbar fusion surgeries to treat LDH with peroneal nerve paralysis. The purpose of this study is to investigate the clinical effect of posterior lumbar fusion surgery on patients who suffered from LDH concurrent with peroneal nerve paralysis.
After being reviewed and identified, a total of 87 participants are finally enrolled in our study. Compared with pre-surgery, the functional parameters have significantly improved after surgery in terms of VAS score, lower-limb muscle strength, and ODI score. Moreover, most patients are very satisfied or satisfied about their treatment effects after fusion surgery. Our findings are in line with some existing reports indicating postoperative pain relief and functional recovery after the patients underwent lumbar surgeries to remove protruded disc and decompress nerve roots (4, 5, 9).
In our study, 56 out of 87 patients had improvements of muscle strength. Overall, the median muscle strength of the tibialis anterior and extensor digitorum improved to a grade of 3 at the last follow-up from grade 0 at admission. Among all 87 patients, there are 40 (46%) patients with muscle strength of grades 4 or 5 at last follow-up. Liu et al. (17) reported 135 patients who suffered from lumbar degenerative diseases with foot drop, and all these patients underwent posterior lumbar interbody fusion surgery with pedicle screw instrumentation. Their study shows 83.7% cases improved in muscle strength; however, only 15.6% patients improved to grades ≧4. By contrast, our study has shown a higher improvement rate (46%, grades ≧4) in muscle strength for the patients who had undergone lumbar fusion surgeries because of LDH and peroneal nerve paralysis. In addition, a multivariate regression analysis of our study shows that advanced age is a risk factor that may affect the final recovery of postoperative patients. This finding is consistent with Liu et al. (17) who reported that younger patients more often have a better surgical outcome.
To date, some studies have proposed a few risk factors and prognosis factors that influence post-operative recovery, but there is no consensus in this aspect. Shorter duration of peroneal nerve paralysis (17, 20), better pre-operative muscle strength (17, 20–22), shorter time to surgery (22), and younger age (17, 23) have been reported to indicate better recovery outcomes for patients who undergo lumbar surgeries due to lumbar spine diseases with peroneal nerve paralysis. However, it has been reported that there are no significant associations between postoperative recovery and the factors including age, diagnosis (LDH or spinal stenosis), duration of symptoms, and preoperative muscle strength (24).
Previous studies (25–27) have indicated that lower-limb exercise can effectively facilitate post-operative pain relief and promote functional recovery of patients undergoing spinal surgery. However, it still remains controversial regarding whether postoperative lower-limb exercise can really accelerate postoperative recovery. Some studies reported that postoperative lower-limb exercise can increase pain relief, functional improvement and patient satisfaction (25–30), while some others did not show positive effects of postoperative lower-limb exercise on final recovery (31–33).
There are some limitations restricting the data interpretation of this study. To start with, this is a single-center retrospective study, and as such the participants lack extensive representation which may affect the accuracy of the data. In addition, the patient sample size is not large, as only 87 participants were included in this study. The results and conclusions would be more robust if the patient sample size was larger. Hence, a larger and therefore more comprehensive study is needed to address all the issues above. The preferred study design would be multi-center, prospective, blinded and randomly controlled, with a larger sample size.
Conclusions
Most of patients suffering from lumbar disc herniation concurrent with peroneal nerve paralysis can improve after undergoing posterior lumbar fusion surgery, but few can reach full recovery. Advanced age might be a risk factor that affects the prognosis of these patients after surgery.
Data availability statement
The raw data supporting the conclusions of this article is available from the corresponding authors upon request.
Ethics statement
The studies involving human participants were reviewed and approved by Medical Ethics Council of the Third Hospital of Hebei Medical University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
WD and SY designed and supervised this study. SG, ZL, HW and ZG collected data. ZL and ZG followed up patients. SG, XL and SY performed statistical analysis and data interpretation. XL and SY made tables and figures. SG drafted the manuscript. SY and SR edited the manuscript. SY finalized the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wang H, Li Z, Huo Y, Tian T, Yang D, Ma L, et al. 17β-Estradiol Alleviates intervertebral disc degeneration by inhibiting NF-κB signal pathway. Life Sci. (2021) 284:119874. doi: 10.1016/j.lfs.2021.119874
2. Yang S, Zhang F, Ma J, Ding W. Intervertebral disc ageing and degeneration: the antiapoptotic effect of oestrogen. Ageing Res Rev. (2020) 57:100978. doi: 10.1016/j.arr.2019.100978
3. Huo Y, Yang D, Ma L, Wang H, Ding W, Yang S. Oblique lumbar interbody fusion with stand-alone cages for the treatment of degenerative lumbar spondylolisthesis: a retrospective study with 1-year follow-up. Pain Res Manag. (2020) 2020:9016219. doi: 10.1155/2020/9016219
4. Telfeian AE, Oyelese A, Fridley J, Doberstein C, Gokaslan ZL. Prognosis for recovery of foot drop after transforaminal endoscopic decompression of far lateral lumbar 5-sacral 1 herniated disc: case series. Pain Physician. (2019) 22:E97–97E103. doi: 10.36076/ppj/2019.22.E97
5. Wang YP, Zhang W, Zhang J, Sun YP, An JL, Ding WY. Analysis of the clinical effects of transforaminal endoscopic discectomy on lumbar disk herniation combined with common peroneal nerve paralysis: a 2-year follow-up retrospective study on 32 patients. J Pain Res. (2017) 10:105–12. doi: 10.2147/JPR.S120463
6. Emamhadi M, Naseri A, Aghaei I, Ashrafi M, Emamhadi R, Andalib S. Soleus nerve transfer to deep peroneal nerve for treatment of foot drop. J Clin Neurosci. (2020) 78:159–63. doi: 10.1016/j.jocn.2020.04.086
7. Hiramatsu K, Yonetani Y, Kinugasa K, Nakamura N, Yamamoto K, Yoshikawa H, et al. Deep peroneal nerve palsy with isolated lateral compartment syndrome secondary to peroneus longus tear: a report of two cases and a review of the literature. J Orthop Traumatol. (2016) 17:181–5. doi: 10.1007/s10195-015-0373-8
8. Marciniak C. Fibular (peroneal) neuropathy: electrodiagnostic features and clinical correlates. Phys Med Rehabil Clin N Am. (2013) 24:121–37. doi: 10.1016/j.pmr.2012.08.016
9. Nakashima H, Ishikawa Y, Kanemura T, Kato F, Satake K, Ito K, et al. Neurological function following early versus delayed decompression surgery for drop foot caused by lumbar degenerative diseases. J Clin Neurosci. (2020) 72:39–42. doi: 10.1016/j.jocn.2020.01.039
10. van Erp R, Jelsma J, Huijnen I, Lundberg M, Willems PC, Smeets R. Spinal Surgeons’ opinions on Pre- and postoperative rehabilitation in patients undergoing lumbar spinal fusion surgery: a survey-based study in The Netherlands and Sweden. Spine. (2018) 43:713–9. doi: 10.1097/BRS.0000000000002406
11. Jansson KA, Németh G, Granath F, Jönsson B, Blomqvist P. Health-related quality of life (EQ-5D) before and one year after surgery for lumbar spinal stenosis. J Bone Joint Surg Br. (2009) 91:210–6. doi: 10.1302/0301-620X.91B2.21119
12. Jansson KA, Németh G, Granath F, Jönsson B, Blomqvist P. Health-related quality of life in patients before and after surgery for a herniated lumbar disc. J Bone Joint Surg Br. (2005) 87:959–64. doi: 10.1302/0301-620X.87B7.16240
13. Mannion AF, Denzler R, Dvorak J, Grob D. Five-year outcome of surgical decompression of the lumbar spine without fusion. Eur Spine J. (2010) 19:1883–91. doi: 10.1007/s00586-010-1535-2
14. Martin BI, Mirza SK, Comstock BA, Gray DT, Kreuter W, Deyo RA. Reoperation rates following lumbar spine surgery and the influence of spinal fusion procedures. Spine. (2007) 32:382–7. doi: 10.1097/01.brs.0000254104.55716.46
15. Kong LD, Zhang YZ, Wang F, Kong FL, Ding WY, Shen Y. Radiographic restoration of sagittal spinopelvic alignment after posterior lumbar interbody fusion in degenerative spondylolisthesis. Clin Spine Surg. (2016) 29:E87–92. doi: 10.1097/BSD.0000000000000104
16. Compston A. Aids to the investigation of peripheral nerve injuries. Medical research council: nerve injuries research committee. His majesty's stationery office: 1942; pp. 48 (iii) and 74 figures and 7 diagrams; with aids to the examination of the peripheral nervous system. By michael O'Brien for the guarantors of brain. Saunders elsevier: 2010; pp. [8] 64 and 94 figures. Brain. (2010) 133:2838–44. doi: 10.1093/brain/awq270
17. Liu K, Zhu W, Shi J, Jia L, Shi G, Wang Y, et al. Foot drop caused by lumbar degenerative disease: clinical features, prognostic factors of surgical outcome and clinical stage. PLoS One. (2013) 8:e80375. doi: 10.1371/journal.pone.0080375
18. Chen Y, Yang H, Zhang L, Wang Y, Zou J. Analyzing the influence of modic changes on patients with lower back pain undergoing conservative treatment. Pain Res Manag. (2019) 2019:8185316. doi: 10.1155/2019/8185316
19. Du JP, Fan Y, Liu JJ, Zhang JN, Huang YS, Zhang J, et al. The analysis of MSTMOVCF (multi-segment thoracolumbar mild osteoporotic fractures surgery or conservative treatment) based on ASTLOF (the assessment system of thoracolumbar osteoporotic fracture). Sci Rep. (2018) 8:8185. doi: 10.1038/s41598-018-26562-7
20. Aono H, Iwasaki M, Ohwada T, Okuda S, Hosono N, Fuji T, et al. Surgical outcome of drop foot caused by degenerative lumbar diseases. Spine. (2007) 32:E262–6. doi: 10.1097/01.brs.0000259922.82413.72
21. Iizuka Y, Iizuka H, Tsutsumi S, Nakagawa Y, Nakajima T, Sorimachi Y, et al. Foot drop due to lumbar degenerative conditions: mechanism and prognostic factors in herniated nucleus pulposus and lumbar spinal stenosis. J Neurosurg Spine. (2009) 10:260–4. doi: 10.3171/2008.12.SPINE08500
22. Macki M, Syeda S, Kerezoudis P, Gokaslan ZL, Bydon A, Bydon M. Preoperative motor strength and time to surgery are the most important predictors of improvement in foot drop due to degenerative lumbar disease. J Neurol Sci. (2016) 361:133–6. doi: 10.1016/j.jns.2015.12.035
23. Ghahreman A, Ferch RD, Rao P, Chandran N, Shadbolt B. Recovery of ankle dorsiflexion weakness following lumbar decompressive surgery. J Clin Neurosci. (2009) 16:1024–7. doi: 10.1016/j.jocn.2008.10.017
24. Girardi FP, Cammisa FP Jr, Huang RC, Parvataneni HK, Tsairis P. Improvement of preoperative foot drop after lumbar surgery. J Spinal Disord Tech. (2002) 15:490–4. doi: 10.1097/00024720-200212000-00010
25. Wang H, Huo Y, Zhao Y, Zhang B, Yang D, Yang S, et al. Clinical rehabilitation effect of postoperative lower-limb training on the patients undergoing OLIF surgery: a retrospective study. Pain Res Manag. (2020) 2020:1065202. doi: 10.1155/2020/1065202
26. Liu SK, Song YL, Ding WY, Yang DL, Ma L, Yang SD. The effect of systematic lower-limb rehabilitation training in elderly patients undergoing lumbar fusion surgery: a retrospective study. Oncotarget. (2017) 8:112720–6. doi: 10.18632/oncotarget.22746
27. Yang SD, Ning SH, Zhang LH, Zhang YZ, Ding WY, Yang DL. The effect of lower limb rehabilitation gymnastics on postoperative rehabilitation in elderly patients with femoral shaft fracture: a retrospective case-control study. Medicine. (2016) 95:e4548. doi: 10.1097/MD.0000000000004548
28. Ostelo RW, Costa LO, Maher CG, de Vet HC, van Tulder MW. Rehabilitation after lumbar disc surgery: an update cochrane review. Spine. (2009) 34:1839–48. doi: 10.1097/BRS.0b013e3181abbfdf
29. Nielsen PR, Jørgensen LD, Dahl B, Pedersen T, Tønnesen H. Prehabilitation and early rehabilitation after spinal surgery: randomized clinical trial. Clin Rehabil. (2010) 24:137–48. doi: 10.1177/0269215509347432
30. Canbulat N, Sasani M, Ataker Y, Oktenoglu T, Berker N, Ercelen O, et al. A rehabilitation protocol for patients with lumbar degenerative disk disease treated with lumbar total disk replacement. Arch Phys Med Rehabil. (2011) 92:670–6. doi: 10.1016/j.apmr.2010.10.037
31. Aalto TJ, Leinonen V, Herno A, Alen M, Kröger H, Turunen V, et al. Postoperative rehabilitation does not improve functional outcome in lumbar spinal stenosis: a prospective study with 2-year postoperative follow-up. Eur Spine J. (2011) 20:1331–40. doi: 10.1007/s00586-011-1781-y
32. McGregor AH, Doré CJ, Morris TP, Morris S, Jamrozik K. ISSLS Prize winner: function after spinal treatment, exercise, and rehabilitation (FASTER): a factorial randomized trial to determine whether the functional outcome of spinal surgery can be improved. Spine. (2011) 36:1711–20. doi: 10.1097/BRS.0b013e318214e3e6
33. Ilves O, Häkkinen A, Dekker J, Pekkanen L, Piitulainen K, Järvenpää S, et al. Quality of life and disability: can they be improved by active postoperative rehabilitation after spinal fusion surgery in patients with spondylolisthesis? A randomised controlled trial with 12-month follow-up. Eur Spine J. (2017) 26:777–84. doi: 10.1007/s00586-016-4789-5
Keywords: lumbar disc herniation, peroneal nerve paralysis, lumbar fusion, lower back pain, risk factor, foot drop
Citation: Gao S, Li Z, Li X, Rudd S, Wang H, Gao Z, Ding W and Yang S (2023) The treatment effect of posterior lumbar fusion surgery on patients suffering from lumbar disc herniation concurrent with peroneal nerve paralysis. Front. Surg. 9:1063528. doi: 10.3389/fsurg.2022.1063528
Received: 7 October 2022; Accepted: 25 November 2022;
Published: 6 January 2023.
Edited by:
Xiaolong Chen, University of New South Wales, AustraliaReviewed by:
Hongfei Xiang, The Affiliated Hospital of Qingdao University, ChinaShouqian Dai, Soochow University, China
Kaiqiang Sun, Department of Orthopedic Surgery, Changzheng Hospital, China
© 2023 Gao, Li, Li, Rudd, Wang, Gao, Ding and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wenyuan Ding d2VueXVhbmRpbmdAaGVibXUuZWR1LmNu Sidong Yang c2lkb25neWFuZ0BoZWJtdS5lZHUuY24=
†These authors have contributed equally to this work and share first authorship
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Shangju Gao1,2,†
Shangju Gao1,2,† Zhaohui Li
Zhaohui Li Xiangyu Li
Xiangyu Li Ze Gao
Ze Gao Wenyuan Ding
Wenyuan Ding Sidong Yang
Sidong Yang