
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Surg., 06 January 2023
Sec. Vascular Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.1063224
This article is part of the Research TopicChronic Carotid Artery Occlusion: Surgical Techniques, Screening modalities, Evaluation Scale, Prescription, and BeyondView all 8 articles
The right aortic arch (RAA) is a rare congenital vascular variant disease. We reported a case of subclavian steal syndrome associated with RAA. The primary clinical symptoms were vertigo and ischemic symptoms of the left upper extremity. We diagnosed the condition using aortic computed tomography angiography and digital subtraction angiography. The patient underwent carotid-subclavian bypass surgery.
A 60-year-old female patient was admitted to the hospital after she reported experiencing frequent nausea and dizziness for more than 1 year. Vertigo did not reveal a significant relationship with the body position and spontaneously resolved after a while. For a year, the appeal symptoms had recurred. She presented with a 3-year history of hypertension and coronary heart disease. The patient's mother and three sisters had a history of identical undiagnosed vertigo. Upon admission, physical examination revealed that the blood pressures of the left upper limb and the right upper limb were 113/67 mmHg and 157/85 mmHg, respectively, and the systolic pressure difference between the two upper limbs was 44 mmHg. Although the right brachial and radial arteries were normal, the pulse rates of the left brachial and radial arteries were low. The left hand and forearm had slightly lower skin temperature than the right hand and forearm. The sensory muscle strength of both forearms was normal. The right aortic arch and aberrant great branch of the aortic arch were detected by thoracic aortic computed-tomography angiography (CTA) (Figure 1A). The left subclavian artery was not visible. as revealed by the aortic arc digital subtraction angiography (DSA) (Figure 1B). The left vertebral artery (LVA) supplied the left subclavian artery (LSA) (Figure 1C).
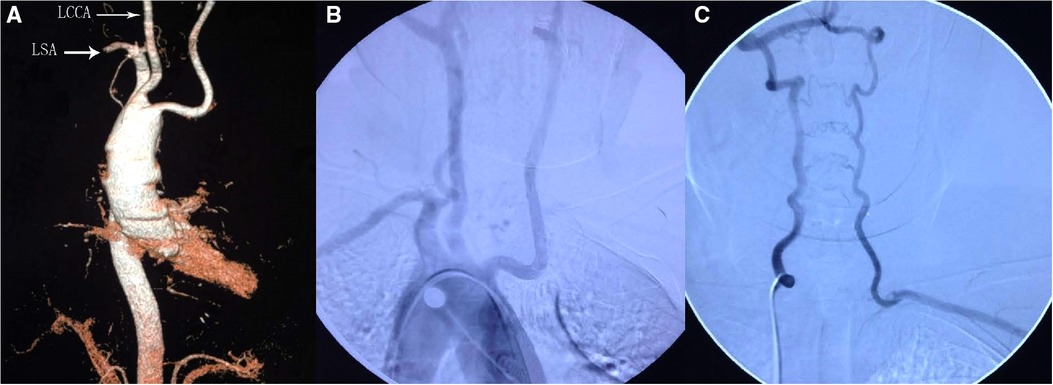
Figure 1. Preoperative CTA of the aorta showed a right-sided aortic arch with an abnormal great branch (A). Aortic DSA showed that the left subclavian artery was not visible (B). Left subclavian artery supplied by the left vertebral artery (C). LSA, left subclavian artery; LCCA, left common carotid artery.
The patient underwent a left common carotid artery-subclavian bypass surgery (Figure 2). The patient's vertigo improved following surgery. The throb of the left brachial artery and radial artery was intensified. The skin temperature of the left hand and forearm was elevated; however, there was no significant difference observed in the blood pressure of the two upper limbs. A postoperative review of cervical vascular CTA (Figure 3) revealed effective bypass vessel angiography. Our patient had no symptoms associated with subclavian steal syndrome at 3-month and 6-month follow-up.
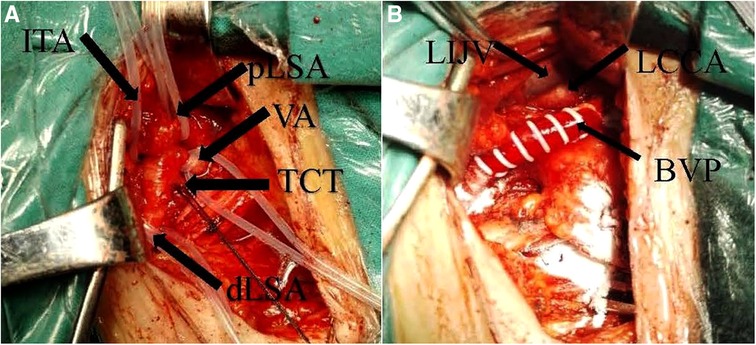
Figure 2. Intraoperative dissociation of the left subclavian artery and its branches, proximal narrowing of the lumen of the left subclavian artery is seen (A). Common carotid artery—left subclavian graft (B). PLSA, proximal left subclavian artery; DLSA, distal left subclavian artery; VA, vertebral artery; ITA, internal thoracic artery; TCT, thyroid trunk; BVP, artificial vessel; LCCA, left common carotid artery; LIJV, left internal jugular vein.
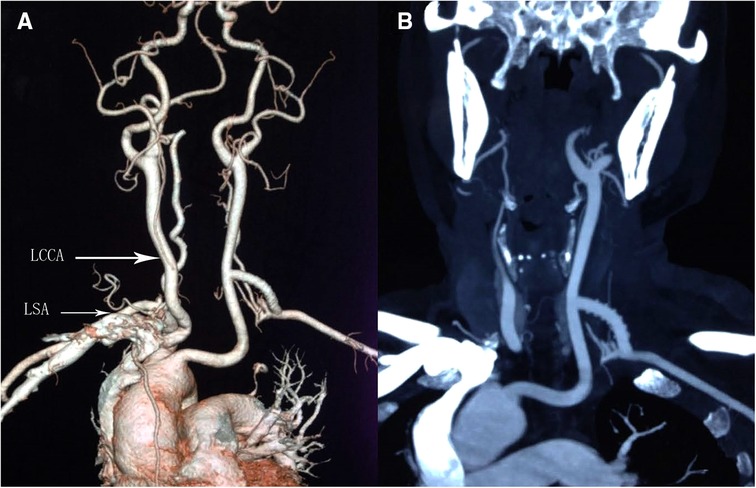
Figure 3. Postoperative CTA showed that good angiography of bypass vessels (A,B). LSA, left subclavian artery; LCCA, left common carotid artery.
With a global prevalence of 0.1%, RAA is a rare vascular malformation that can either be a mirror image of normal branches or a combination of various abnormalities (1, 2). Cases of subclavian steal syndrome associated with RAA are quite rare. One report showed symptoms of left arm ischemia and vertebrobasilar insufficiency years after left subclavian artery ligation (3). There are reports of a man with Peutz-Jeghers syndrome who had his first episode of vertigo at the age of 29 due to subclavian steal syndrome (4).
The ductus arteriosus is usually on the left side. However, the ductus arteriosus may also be present on the right side, possibly with bilateral arterial development associated with aortic arch malformations (3). The patient included in our study belonged to the third category. The separation of the left subclavian artery from the right aortic arch may be related to 22q11 deletion in embryological development (5, 6).
Contorni was the first to define subclavian steal syndrome, a condition in which blood flow is reversed in branches of the subclavian artery (7). The criteria for the diagnosis of subclavian steal syndrome are as follows: (1) Occlusion or marked stenosis of the subclavian or innominate arteries; (2) retrograde vertebral arterial flow; (3) patency of both the vertebral and basilar arteries (8). Our case met these criteria. Owing to the inadequate blood supply to the brain arteries, some patients with subclavian steal syndrome may experience symptoms of temporary ischemia (9). The symptoms of this disease include vertigo, dizziness, headache, diplopia, and a wide spectrum of symptoms involving the brain stem (1). It is caused by posterior circulation (brainstem vestibular system) ischemia, and vertigo generally lasts for several minutes and subsides on its own and thus can be distinguished from pseudovertigo, which is caused by hypertension (10). To accurately diagnose the subclavian syndrome, it is imperative to ascertain the blood pressure (BP) differences between retrograde blood flow in the arm and vertebral arteries (11, 12). More than 95% of patients have been documented in the literature to have overtly visible clinical symptoms, including dizziness, vomiting, headache, and syncope. The external carotid artery, the thyrocervical artery, the external carotid artery-occipital artery, the muscular branches of the vertebral artery systems, and a crossover flow between the internal mammary arteries are all collateral pathways for blood to enter the subclavian artery; however, the main anastomotic network is the vertebrobasilar system (10).
The primary imaging tests used to diagnose this disease were transthoracic echocardiography (TTE), magnetic resonance imaging (MRI), and angiography. Eighty-four percent of the cases were suspected based on the initial TTE; however, in many cases, echocardiography often indicated a suspicion albeit did not confirm the diagnosis. To determine the details of vascular connections, further imaging is generally required. In 38% of the cases, cardiac catheterization was used, allowing for hemodynamic assessment. A cardiac CT scan is preferred if the airway needs to be evaluated (13). Moreover, compared to other modalities, a cardiac CT scan can detect a smaller or stenotic patent ductus arteriosus (14). MRI provides the advantage of assessing blood flow through vessels with small diameters and into the heart chambers (15).
The patient underwent left common carotid artery-subclavian bypass surgery, which reduced the stress on the vertebral artery by diverting blood flow from the left common carotid artery to the subclavian artery. The patient's vertigo improved following surgery. The throb of the left brachial artery and radial artery was enhanced. The bypass surgery treatment proved to be an effective method of surgery for the patient.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
JC performed the data analyses and wrote the manuscript. XW contributed to the conception of the study; CX contributed to the manuscript preparation; All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Mamopoulos AT, Luther B. Congenital subclavian steal syndrome with multiple cerebellar infarctions caused by an atypical circumflex retroesophageal right aortic arch with atretic aberrant left subclavian artery. J Vasc Surg. (2014) 60:776–9. doi: 10.1016/j.jvs.2013.06.086
2. Alhuzaimi AN, Aldawsari KA, AlAhmadi M. Isolated left subclavian artery with right aortic arch: case report and literature review of 50 cases. Gen Thorac Cardiovasc Surg. (2021) 69:885–9. doi: 10.1007/s11748-020-01564-3
3. Abe M, Isobe T, Atsumi N. Right aortic arch with isolation of the left subclavian artery and bilateral patent ductus arterioses. Pediatr Cardiol. (2000) 21:497–9. doi: 10.1007/s002460010121
4. Hokari M, Kuroda S, Furukawa K, Houkin K, Iwasaki Y. Subclavian steal syndrome associated with the right aortic arch in a patient with Peutz-Jeghers syndrome: case report. No Shinkei Geka. (2003) 31:281–6. PMID: 12684982
5. Madan N, Schneider DJ, Jacobs ML. Right aortic arch, isolated left subclavian artery and ductus arteriosus with normal intracardiac anatomy: rare manifestation of chromosome 22q11 deletion. Pediatr Cardiol. (2006) 27:781–3. doi: 10.1007/s00246-006-6009-2
6. Lee Y, Hong SW. Abnormal origin of the left subclavian artery from the left pulmonary artery in a patient with double outlet right ventricle. Korean J Thorac Cardiovasc Surg. (2014) 47:32–4. doi: 10.5090/kjtcs.2014.47.1.32
7. Contorni L. The vertebro-vertebral collateral circulation in obliteration of the subclavian artery at its origin. Minerva Chir. (1960) 15:268–71. PMID: 13811644
8. Hastreiter AR, D'Cruz IA, Cantez T, Namin EP, Licata R. Right-sided aorta. I. Occurrence of right aortic arch in various types of congenital heart disease. II. Right aortic arch, right descending aorta, and associated anomalies. Br Heart J. (1966) 28:722–39. doi: 10.1136/hrt.28.6.722
9. Fields WS, Lemak NA. Joint study of extracranial arterial occlusion. VII. Subclavian steal–a review of 168 cases. JAMA. (1972) 222:1139–43. doi: 10.1001/jama.1972.03210090019004
10. Komatsubara I, Kondo J, Akiyama M, Takeuchi H, Nogami K, Usui S, et al. Subclavian steal syndrome: a case report and review of advances in diagnostic and treatment approaches. Cardiovasc Revasc Med. (2016) 17:54–8. doi: 10.1016/j.carrev.2015.11.001
11. Tan TY, Schminke U, Lien LM, Tegeler CH. Subclavian steal syndrome: can the blood pressure difference between arms predict the severity of steal? J Neuroimaging. (2002) 12:131–5. doi: 10.1111/j.1552-6569.2002.tb00109.x
12. von Reutern GM, Pourcelot L. Cardiac cycle-dependent alternating flow in vertebral arteries with subclavian artery stenoses. Stroke. (1978) 9:229–36. doi: 10.1161/01.STR.9.3.229
13. Yubbu P, Latiff HA, Adam Abbaker AM. Right aortic arch with isolation of the left subclavian artery: a rare association with airway obstruction. Cardiol Young. (2017) 27:613–6. doi: 10.1017/S1047951116001840
14. Jesudian V, Ravikumar R, Kumar RS. Isolation of the left subclavian artery-origin from the left pulmonary artery by way of ductus arteriosus: multidetector row computed tomographic angiographic imaging. Pediatr Cardiol. (2009) 30:549–50. doi: 10.1007/s00246-009-9392-7
Keywords: right aortic arch, subclavian steal syndrome, bypass surgery treatment, case, report
Citation: Cai J, Xie C and Wang X (2023) Subclavian steal syndrome associated with right aortic arch: A case report. Front. Surg. 9:1063224. doi: 10.3389/fsurg.2022.1063224
Received: 6 October 2022; Accepted: 21 November 2022;
Published: 6 January 2023.
Edited by:
Jieqing Wan, Shanghai Jiao Tong University, ChinaReviewed by:
Anshuman Darbari, All India Institute of Medical Sciences, India© 2023 Cai, Xie and Wang, This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xianwei Wang Email eHd3YW5neHl5eUAxNjMuY29t
Specialty Section: This article was submitted to Vascular Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.