
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 06 January 2023
Sec. Surgical Oncology
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.1055338
This article is part of the Research Topic Digital Revolution in Oncology: How Digital Tools Transform the Evaluation and Management of Cancer Patients View all 24 articles
 Hongzhen Zhang1,†
Hongzhen Zhang1,† Dingfei Ren2,†
Dingfei Ren2,† Danqing Cheng3
Danqing Cheng3 Wenping Wang3
Wenping Wang3 Yongtian Li4
Yongtian Li4 Yisong Wang4
Yisong Wang4 Dekun Lu5
Dekun Lu5 Feng Zhao5*
Feng Zhao5*
Background: An increasing number of lung cancer patients are opting for lobectomy for oncological treatment. However, due to the unique organismal condition of elderly patients, their short-term postoperative mortality is significantly higher than that of non-elderly patients. Therefore, there is a need to develop a personalised predictive tool to assess the risk of postoperative mortality in elderly patients.
Methods: Information on the diagnosis and survival of 35,411 older patients with confirmed lobectomy NSCLC from 2009 to 2019 was screened from the SEER database. The surgical group was divided into a high-risk mortality population group (≤90 days) and a non-high-risk mortality population group using a 90-day criterion. Survival curves were plotted using the Kaplan-Meier method to compare the differences in overall survival (OS) and lung cancer-specific survival (LCSS) between the two groups. The data set was split into modelling and validation groups in a ratio of 7.5:2.5, and model risk predictors of postoperative death in elderly patients with NSCLC were screened using univariate and multifactorial logistic regression. Columnar plots were constructed for model visualisation, and the area under the subject operating characteristic curve (AUC), DCA decision curve and clinical impact curve were used to assess model predictiveness and clinical utility.
Results: Multi-factor logistic regression results showed that sex, age, race, histology and grade were independent predictors of the risk of postoperative death in elderly patients with NSCLC. The above factors were imported into R software to construct a line graph model for predicting the risk of postoperative death in elderly patients with NSCLC. The AUCs of the modelling and validation groups were 0.711 and 0.713 respectively, indicating that the model performed well in terms of predictive performance. The DCA decision curve and clinical impact curve showed that the model had a high net clinical benefit and was of clinical application.
Conclusion: The construction and validation of a predictive model for death within 90 days of lobectomy in elderly patients with lung cancer will help the clinic to identify high-risk groups and give timely intervention or adjust treatment decisions.
Lung cancer is one of the most common malignancies in the world, killing nearly 2 million people each year, mainly in the older age group of 65 years and above (1, 2). Non-small cell lung cancer (NSCLC) accounts for approximately 85% of lung cancers. With the accelerated ageing of the population and widespread screening by low-dose CT, the number of confirmed cases of NSCLC in the elderly has increased significantly (3, 4), posing a serious threat to human health and life.
Surgical resection is the treatment of choice for early-stage lung cancer, but there are many factors that affect post-operative survival due to the high mortality rate, multiple comorbidities and complex post-operative non-cancer related conditions that characterise the elderly lung cancer population (5–7). In 2021, Jiao et al. (8) constructed a prediction model combining radiological features and mortality risk parameters with a c-index as high as 0.734, which helped clinical identification of patients with early-stage NSCLC and was not an effective predictor of survival in NSCLC patients after surgery. A recent study (9) combined clinical and genomic features to construct a columnar graph model for risk stratification of early-stage NSCLC to assess the prognostic value of postoperative prognosis in NSCLC patients. These recent studies have used diverse approaches to construct postoperative predictive models for NSCLC, giving the models greater clinical predictive value, but these models are generally applicable to postoperative NSCLC patients without specific age differentiation.
Few current studies have investigated predictive models for monitoring risk factors for death and survival at 90 days after lobectomy in elderly (age ≥75 years) NSCLC. Based on the (SEER) database, this study retrospectively analysed the consultation and survival information of elderly patients with confirmed lobectomy NSCLC from 2009 to 2019 to develop a clinical line chart for predicting mortality after lobectomy in elderly NSCLC patients to facilitate clinical assessment of postoperative survival and development of individualised treatment strategies for elderly NSCLC patients.
The data used in this study were all obtained from the National Cancer Institute's SEER database (SEER.cancer.gov) registry, a publicly available cancer database covering approximately 34.6% of the US population. Data from older patients with confirmed NSCLC from (2009 to 2019) were downloaded using SEER*Stat version 8.3.6 for analysis of the study. Screening inclusion criteria: (1) age ≥75 years; (2) meeting diagnostic criteria for NSCLC, confirmed clinically and pathologically; (3) Patients who underwent lobectomy for NSCLC; (4) Those with complete clinical data, including age, race, gender, tumour histological grade, molecular typing, postoperative survival time, and survival outcome. Exclusion criteria: (1) age <75 years; (2) previous history of lung tumors and other malignancies; (3) patients with non-NSCLC lobectomy; (4) those with incomplete clinical information. A total of 35,411 patients were eventually included as study subjects.
In this study, patients aged >75 years in the NSCLC surgery group were classified as non-high-risk for survival >90 days after surgery, and those with survival ≤90 days were classified as high-risk for death. To eliminate the influence of confounding factors on the study results, the 1:1 propensity score matching (PSM) was used to eliminate differences in baseline information between the two groups of data, and survival curves were plotted using the Kaplane-Meier method and log-rank tests were used to compare the differences in survival curves between the groups.
All enrolled CSCLC patients were further randomly split into a modelling and validation group in a ratio of 7.5:2.5. For the modelling group, univariate and multifactorial logistic regression were used to screen independent risk predictors for elderly patients undergoing lobectomy for NSCLC as the construct variables for the line graph model.
Screened independent risk predictors for elderly patients undergoing lobectomy for NSCLC were incorporated into the prediction model, and the risk factors were presented visually using R software version 3.6.3 (http://www.r-project.org/). The predictive efficacy and clinical utility of the line graph prediction model was evaluated by analysing the receiver operating characteristic curve (ROC curve) and Decision Curve Analysis (DCA).
All statistical analyses were performed using EmpowerStats (version 2.2) and R software (version 4.0.5). Count data were expressed as relative numbers and comparisons were made using the χ2 test; measurement data conforming to a normal distribution were expressed as (`x ± s) and measurement data not conforming to a normal distribution were expressed as M (P25, P75); one-way and multi-way logistic regression analyses were used to screen risk factors in CSCLC patients, and P < 0.05 was considered a statistically significant difference.
A total of 35,411 elderly patients with NSCLC aged ≥75 years in the SEER database were included in this study. To eliminate the influence of confounding factors on this study, we used a 1:1 propensity score matching (PSM) method for analysis. 21,658 patients in the NSCLC surgical group and 13,753 patients in the NSCLC non-surgical group before PSM were analyzed in both groups in terms of Age, Gender Marrital ststus, Race, Tuomor Position, Lung lobectomy, Histologic Type, Grade, AJCC-T, AJCC-N, AJCC-M were statistically significant (P < 0.05); after PSM, 9,058 patients in the NSCLC surgery group were compared with 9,058 patients in the NSCLC non-surgical group were successfully matched, with statistically significant differences in all variables except for the four confounding variables Gender, Involved lung lobes, AJCC-T, and AJCC-M, which were not statistically significant between groups (P > 0.05) (Table 1).
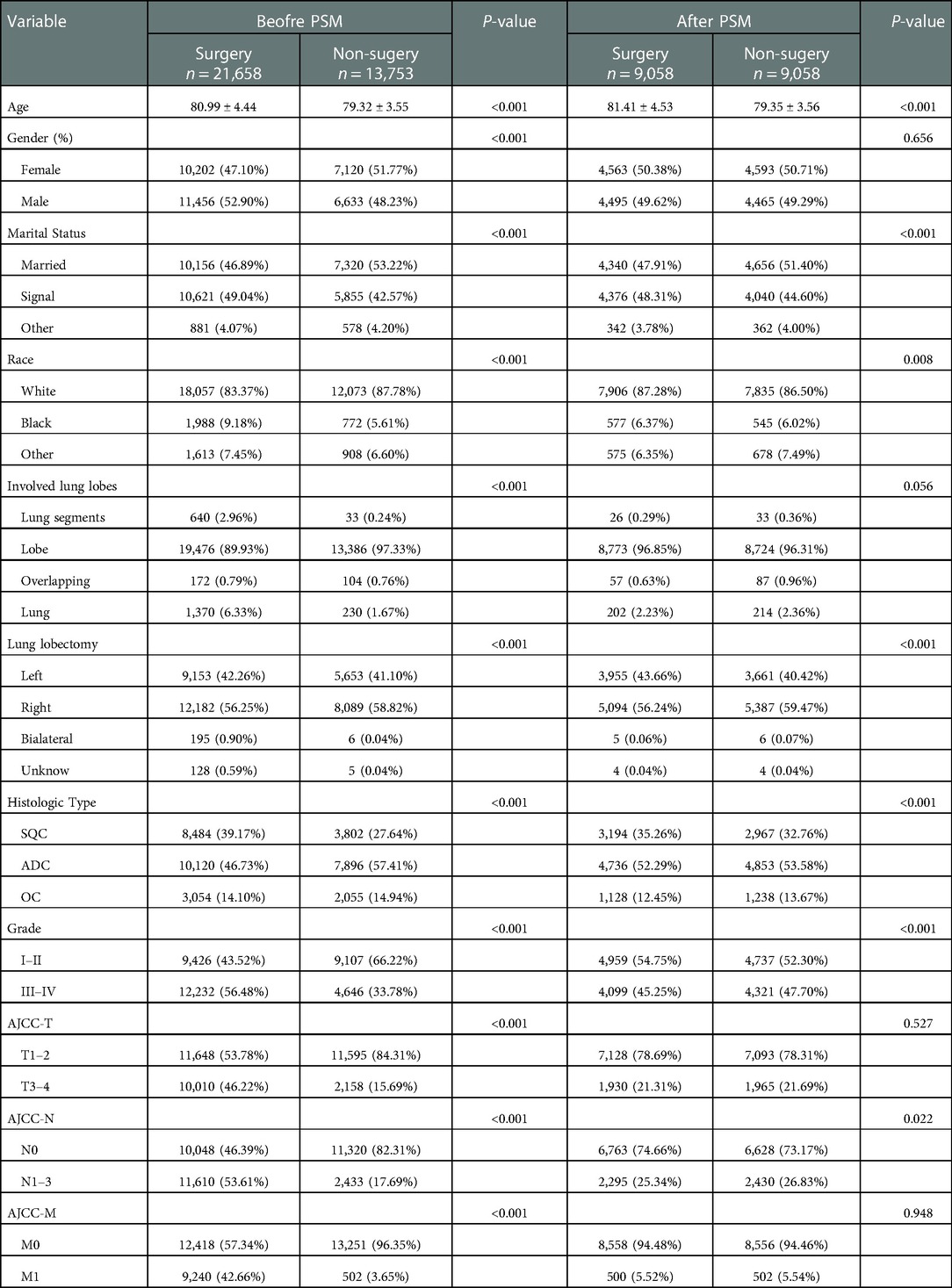
Table 1. Patient information based on their baseline features before and after 1:1 PSM in surgery and non surgery groups.
Kaplan-Meier plots visualise the differences in survival time after lobectomy in older patients with NSCLC. Overall, before and after propensity score matching (PSM), OS was shorter in the NSCLC high-risk mortality group than in the NSCLC non-high-risk group (P < 0.001). When comparing survival data between the two groups, survival rates were higher in the NSCLC non-high-risk group than in the NSCLC high-risk death group before and after matching, with survival rates of 73%, 43% and 18% at 25, 50 and 75 months in the NSCLC non-high-risk group and 25%, 8% and 2% at 25, 50 and 75 months in the NSCLC high-risk death group, respectively. Post-matching survival rates at 25, 50 and 75 months were 68%, 22% and 4% for the NSCLC non-high-risk group and 41%, 16% and 5% for the NSCLC high-risk mortality group, respectively. As shown in Figure 1.
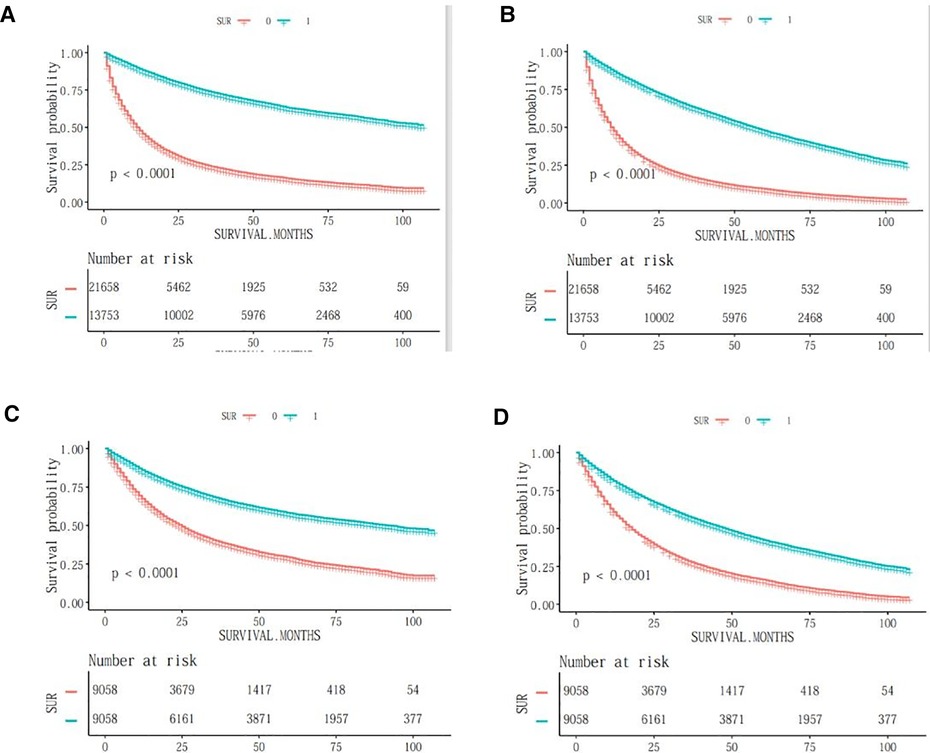
Figure 1. OS survival curves before and after PSM in elderly patients with NSCLC. (A) css-tumour-specific mortality before PSM; (B) os-tumour overall survival before PSM; (C) css-tumour-specific mortality after PSM; (D) os-tumour overall survival after PSM.
In the modeled group, the results of the one-way logistic regression analysis showed that the risk factors affecting the survival of elderly patients with confirmed lobectomy NSCLC were Sex, Age, Race, Histologic Type, and Grade (T, N, M), and the differences were all statistically significant at P < 0.05. These five risk factors were included again in the further multifactorial logistic regression analysis, and the results proved that these five risk factors were independent risk factors for survival in elderly patients with confirmed lobectomy NSCLC (Table 2).
Based on the results of multi-factor logistic regression analysis, the survival of elderly patients diagnosed with lobectomy NSCLC was visualized and analyzed by including 5 factors affecting survival prognosis, sex, age, race, histology and grade, and a Nomogram prediction model was constructed based on the above 5 risk factors, as shown in Figure 2.
The Nomogram prediction model was validated by applying ROC curves, and the results showed that the area under the ROC curve for the modelling group prediction model was 0.711 AUC, and the area under the ROC curve for the validation group prediction model was 0.713 AUC, indicating that the Nomogram model has good prediction accuracy; as shown in Figures 3A,B. DCA decision curves and clinical impact curves are method to assess the value of the prediction model for clinical application. When the threshold probability of the DCA decision curve was shown to be between 1% and 90%, it indicated that the column line graph prediction model developed in this study had a high net clinical benefit, as shown in Figure 4.
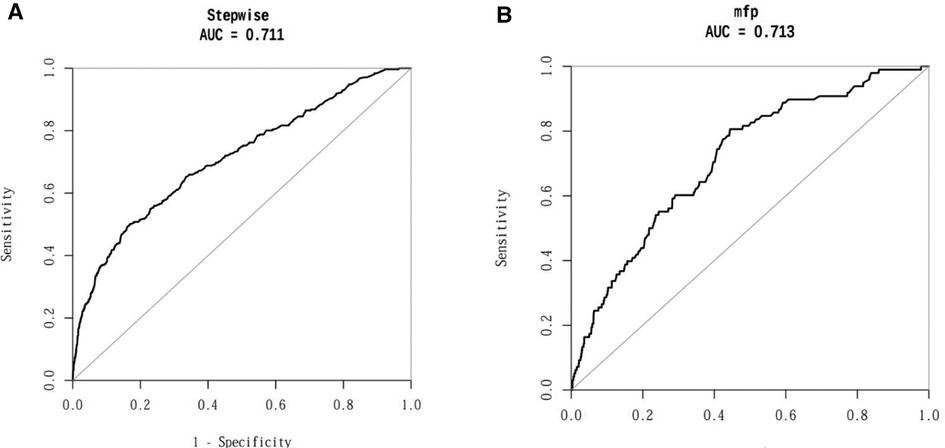
Figure 3. ROC curves of the prediction model for the column line graph of elderly patients with NSCLC. (A) AUC of the modelling group; (B) AUC of the validation group.
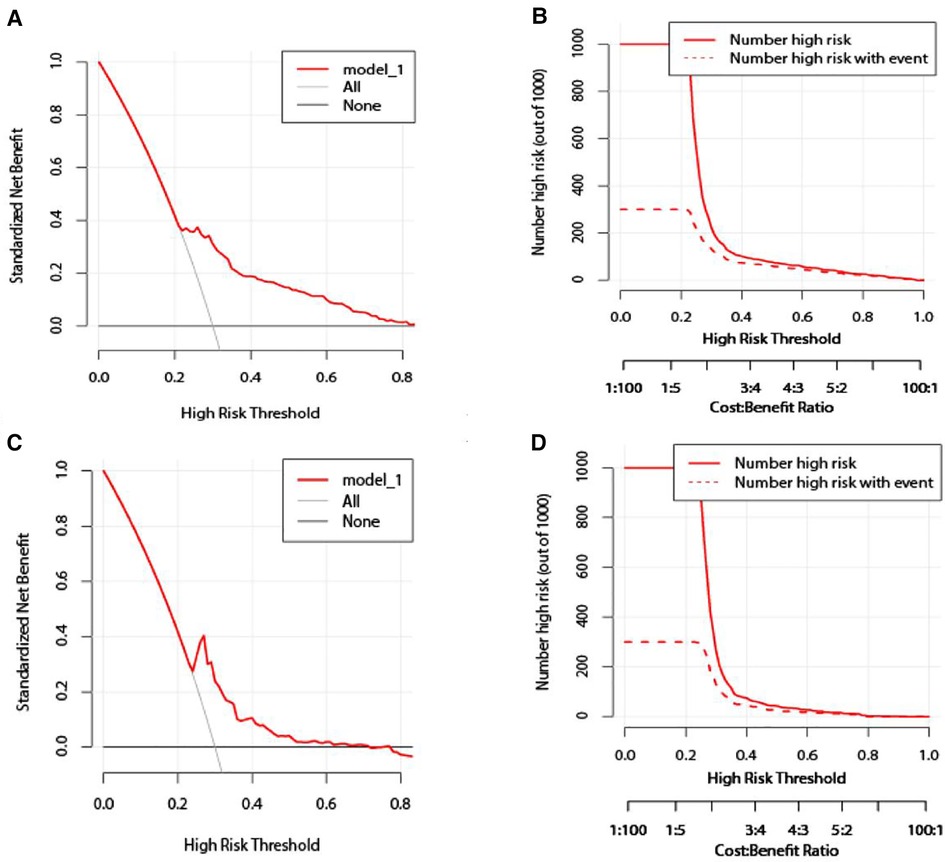
Figure 4. Validation of the column line graph prediction model. (A,C) Modeling group/validation group DCA decision curve; (B,D) modeling group/validation group clinical impact curve.
Non-small cell lung cancer (NSCLC), is the leading cause of cancer deaths worldwide (10–12). Surgery is currently the main treatment for non-small cell lung cancer (NSCLC), with anatomical lobectomy being the main surgical treatment modality for NSCLC (13–15). With the development of lung cancer epidemiology and an ageing population, elderly patients with non-small cell lung cancer (NSCLC) have become an important patient group in lung cancer surgery. In this study, we analyzed the risk factors for postoperative mortality and the incidence of postoperative mortality in a special population of elderly patients undergoing lobectomy for NSCLC, and developed a practical prediction model to predict survival after lobectomy in elderly patients with NSCLC. The results of the study showed that the model has good predictive performance and has good clinical utility, providing guidance and decision making for the clinical survival of elderly patients undergoing lobectomy for NSCLC.
A prediction model (16) for NSCLC after radiotherapy has been proposed and predicts patient survival at 6 months, 1 year, 2 years and 3 years, but the model is only predictive of survival for patients treated with radiation for NSCLC. In the latest study on columnar graph prediction models for NSCLC, Chen (17) constructed a columnar graph model to predict prognosis of lymph node metastasis in NSCLC patients by four factors: age, SIRI, PNI and CEA. Zhang et al. (18) developed a line graph model to predict the development of advanced non-small cell lung cancer by combining clinical and molecular features. Xiaoping (19) developed a personalised line graph model based on CT-based sarcopenic to predict survival of patients with non-small cell lung cancer after receiving chemotherapy, which has some similarities to the present study. This study explored postoperative prognosis and survival model construction in NSCLC patients, but its study population was broad, none of which had predictive model construction regarding survival within 90 days after lobectomy in older (age ≥75 years) NSCLC patients.
As people continue to age, changes in the physiology and pathology of the elderly patient's organism are influenced by a number of factors, particularly physiological changes in the cardiovascular and respiratory systems (20, 21). This is mainly reflected in the reduced catecholamine response to stress, significantly reduced cardiac output, reduced lung tissue compliance, reduced expiratory effort and reduced pulmonary ventilation-perfusion capacity in elderly patients (22–24). In elderly patients with a long history of smoking, their vulnerability to hypoxaemia and hypercapnia presents a significant challenge for the surgical management of elderly patients with NSCLC (25–27). At the same time, the fact that patients older than 75 years of age often have many other underlying conditions (e.g., diabetes, hypertension, chronic bronchitis and emphysema) increases the risk of surgery and seriously affects the post-operative recovery of elderly patients.
We found that age, race, gender, degree of differentiation, histological type, and grade (T, N stage) were independent factors for OS in studies related to lung cancer, and these factors were consistent with findings on risk factors for non-small cell lung cancer (28–30). However, many previous studies have not clarified the multi-prognostic analysis of survival at 90 days postoperatively in elderly patients undergoing lobectomy for NSCLC (31–33). In this study, as many variables related to postoperative survival information for elderly patients undergoing lobectomy for NSCLC as possible will be included in the clinical prediction model to improve its accuracy. In this study, age and tumour infiltration grade were found to have a considerable impact on the survival of NSCLC patients. Guo et al. (34) showed that plasma-related pulmonary artery embolism levels in NSCLC patients increased significantly with increasing age, and that the prognostic hypercoagulable status of NSCLC patients was related to patients’ age, tumour infiltration grade and metastasis, and their postoperative treatment needed to take these factors into account. In addition, gender and ethnicity are important prognostic factors for patients with NSCLC, and gender is a strong prognostic factor when assessing the survival of patients with non-small cell lung cancer (35–37). Prognostic studies related to NSCLC (38–42) have also shown that the histologic subtype of NSCLC is associated with the risk of postoperative death in NSCLC patients, and that the overall postoperative survival OS of patients with different non-small cell lung cancer (NSCLC) histologic subtypes varies. Therefore, we identified Sex, Age, Race, Histologic Type, and Grade (T, N, M) as variables used in the column line graph, and the column line graph model constructed by these variables is of great importance in predicting the survival rate of elderly patients after lobectomy for NSCLC and guiding their treatment.
In this study, we constructed a survival prediction line graph model for elderly patients after lobectomy for NSCLC, which was based on a large database population to predict OS in patients undergoing lobectomy for NSCLC. in the model testing and validation, we found that the area under the ROC curve AUC of the model was 0.711 and 0.713 in the testing and validation groups, respectively, which were both much greater than 0.5, indicating that the model was predictive of survival of elderly patients after lobectomy for NSCLC is predictive efficacy and the model has good predictive performance. The clinical utility of the model was assessed by DCA decision curves and clinical impact curves, and the results of the validation group showed that the column line graph prediction model developed in our study has a high net clinical benefit and can be used as a tool for clinical decision making. Physicians and patients can use the column line graph model prediction scoring system to understand the individualised survival expectations of elderly patients after lobectomy for NSCLC, and based on the results of the column line graph prediction, effective interventions can be made to improve the survival of elderly patients after lobectomy for NSCLC with low survival rates.
This study was enrolled in the National Cancer Institute's SEER database, and although the sample size was large, there were some limitations. (1) This study is a retrospective study with a low level of evidence compared to prospective cohort studies. (2) In order to eliminate the influence of confounding factors on the study results, the data were processed using propensity score matching (PSM), but there was still an unavoidable selective bias in the two data sets. (3) This study is a single-centre study, with both the test and validation sets from the same database, and lacks external datasets to validate the prediction model of this study. Our next research direction is to conduct a multicentre, large sample size prospective study of elderly patients after lobectomy for NSCLC. (4) The SEER database does not provide more information on elderly patients undergoing lobectomy for NSCLC, such as cause of death, surgical approach, and postoperative adjuvant treatment options, which may also be important factors influencing the information on postoperative survival of elderly patients with NSCLC. Despite some limitations, the Nomogram was constructed based on a large population and provides a practical and effective clinical tool for predicting survival in elderly patients undergoing lobectomy for NSCLC.
In this study, sex, age, race, histology and grade were important factors influencing postoperative survival in elderly patients after lobectomy for NSCLC. For elderly patients after lobectomy for NSCLC, timely and effective postoperative survival assessment and enhanced clinical supervision are beneficial to improve the survival rate of elderly patients after lobectomy for NSCLC.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
This is a retrospective clinical study with a dataset from the SEER public database in the USA, conducted in accordance with the ethical standards of the World Medical Association Declaration of Helsinki.
FZ and HZ contributed to the writing of the manuscript, DC and WW design of the study and statistical analysis. DR and DC contributed to data retrieval and manuscript review. WW, YL and DL contributed to data collection and data collation. All authors contributed to the article and approved the submitted version.
The authors carried out all the work in this study with the support of the Organization Department of the Huainan Municipal Committee of Anhui Province and the Huainan Science and Technology Bureau. This study was funded by the Key Research Project of Anhui Provincial Education Department (No. KJ2019A0094), the Key Research Project of Anhui Provincial Education Department (No. KJ2019A0095), and the Research Project Plan of Bengbu Medical College (No. BYKY2019318ZD).
This work was supported by the Huainan City Occupational Disease Control Institute, Anhui Province, China; the School of Medicine of Anhui University of Technology; and the First People's Hospital affiliated to Anhui University of Technology (Huainan First People's Hospital).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2018) 68:394–424. doi: 10.3322/caac.21492
2. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. (2022) 72:7–33. doi: 10.3322/caac.21708
3. Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, Fagerstrom RM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. (2011) 365:395–409. doi: 10.1056/NEJMoa1102873
4. Kwan TY, Chowdhury EH. Clinical outcomes of chemotherapeutic molecules as single and multiple agents in advanced non-small-cell lung carcinoma (NSCLC) patients. Medicina. (2021) 57(11), 1252. doi: 10.3390/medicina57111252
5. Blanco R, Maestu I, de la Torre MG, Cassinello A, Nuñez I. A review of the management of elderly patients with non-small-cell lung cancer. Ann Oncol. (2015) 26:451–63. doi: 10.1093/annonc/mdu268
6. Rocco G, Weder W. Lung surgery in the elderly today. Lung Cancer. (2013) 80:115–9. doi: 10.1016/j.lungcan.2013.01.004
7. Zhang B, Liu R, Ren D, Li X, Wang Y, Huo H, et al. Comparison of lobectomy and sublobar resection for stage IA elderly NSCLC patients (≥70 years): a population-based propensity score matching's study. Front Oncol. (2021) 11:610638. doi: 10.3389/fonc.2021.610638
8. Jiao Z, Li H, Xiao Y, Aggarwal C, Galperin-Aizenberg M, Pryma D, et al. Integration of risk survival measures estimated from pre- and posttreatment computed tomography scans improves stratification of patients with early-stage non-small cell lung cancer treated with stereotactic body radiation therapy. Int J Radiat Oncol Biol Phys. (2021) 109:1647–56. doi: 10.1016/j.ijrobp.2020.12.014
9. Hu C, Shu L, Chen C, Fan S, Liang Q, Zheng H, et al. A prediction model integrated genomic alterations and immune signatures of tumor immune microenvironment for early recurrence of stage I NSCLC after curative resection. Transl Lung Cancer Res. (2022) 11:24–42. doi: 10.21037/tlcr-21-751
10. Miller KD, Nogueira L, Mariotto AB, Rowland JH, Yabroff KR, Alfano CM, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. (2019) 69:363–85. doi: 10.3322/caac.21565
11. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. (2019) 69:7–34. doi: 10.3322/caac.21551
12. Xia L, Wang Z, Wu X, Zeng T, Luo W, Hu X, et al. Multiplatform discovery and regulatory function analysis of structural variations in non-small cell lung carcinoma. Cell Rep. (2021) 36:109660. doi: 10.1016/j.celrep.2021.109660
13. Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung cancer study group. Ann Thorac Surg. (1995) 60:615–22; discussion 622–3. doi: 10.1016/0003-4975(95)00537-u
14. Veluswamy RR, Ezer N, Mhango G, Goodman E, Bonomi M, Neugut AI, et al. Limited resection versus lobectomy for older patients with early-stage lung cancer: impact of histology. J Clin Oncol. (2015) 33:3447–53. doi: 10.1200/JCO.2014.60.6624
15. Song C, Lu Z, Li D, Pan S, Li N, Geng Q. Survival after wedge resection versus lobectomy for stage IA second primary NSCLC with previous lung cancer-directed surgery. Front Oncol. (2022) 12:890033. doi: 10.3389/fonc.2022.890033
16. Duijm M, Oomen-de Hoop E, van Voort van der Zyp N, van de Vaart P, Tekatli H, Hoogeman M, et al. The development and external validation of an overall survival nomogram in medically inoperable centrally located early-stage non-small cell lung carcinoma. Radiother Oncol. (2021) 156:223–30. doi: 10.1016/j.radonc.2020.12.038
17. Chen M, Yang Y, He C, Chen L, Cheng J. Nomogram based on prognostic nutrition index and chest CT imaging signs predicts lymph node metastasis in NSCLC patients. J Xray Sci Technol. (2022) 30:599–612. doi: 10.3233/XST-211080
18. Zhang Y, Zeng L, Zhang X, Li Y, Liu L, Xu Q, et al. Clinical and molecular feature-based nomogram model for predicting benefit from bevacizumab combined with first-generation EGFR-tyrosine kinase inhibitor (TKI) in EGFR-mutant advanced NSCLC. BMC Med. (2021) 19:245. doi: 10.1186/s12916-021-02118-x
19. Yi X, Chen Q, Yang J, Jiang D, Zhu L, Liu H, et al. CT-based sarcopenic nomogram for predicting progressive disease in advanced non-small-cell lung cancer. Front Oncol. (2021) 11:643941. doi: 10.3389/fonc.2021.643941
20. Zhang X, Lin G, Li J. Comparative effectiveness of lobectomy, segmentectomy, and wedge resection for pathological stage I non-small cell lung cancer in elderly patients: a population-based study. Front Surg. (2021) 8:652770. doi: 10.3389/fsurg.2021.652770
21. Adachi T, Tsunekawa Y, Tanimura D. Association among mild cognitive impairment, social frailty, and clinical events in elderly patients with cardiovascular disease. Heart Lung. (2022) 55:82–8. doi: 10.1016/j.hrtlng.2022.04.011
22. Gök G, Kılıç S, Sinan ÜY, Turkoglu E, Kemal H, Zoghi M. Epidemiology and clinical characteristics of hospitalized elderly patients for heart failure with reduced, mid-range and preserved ejection fraction. Heart Lung. (2020) 49:495–500. doi: 10.1016/j.hrtlng.2020.03.023
23. Shi X, Shen Y, Yang J, Du W, Yang J. The relationship of the geriatric nutritional risk index to mortality and length of stay in elderly patients with acute respiratory failure: a retrospective cohort study. Heart Lung. (2021) 50:898–905. doi: 10.1016/j.hrtlng.2021.07.012
24. Lee H, Kim HK, Kang D, Kong S, Lee JK, Lee G, et al. Prognostic value of 6-min walk test to predict postoperative cardiopulmonary complications in patients with non-small cell lung cancer. Chest. (2020) 157:1665–73. doi: 10.1016/j.chest.2019.12.039
25. Fu D, Wu C, Li X, Chen J. Elevated preoperative heart rate associated with increased risk of cardiopulmonary complications after resection for lung cancer. BMC Anesthesiol. (2018) 18:94. doi: 10.1186/s12871-018-0558-9
26. Yang H, Yun Y, Mao Y. Clinical analysis of the impact of sublobectomy on pulmonary function. Medicine. (2017) 96:e8662. doi: 10.1097/MD.0000000000008662
27. Arrieta O, Campos-Parra AD, Zuloaga C, Avilés A, Sánchez-Reyes R, Manríquez ME, et al. Clinical and pathological characteristics, outcome and mutational profiles regarding non-small-cell lung cancer related to wood-smoke exposure. J Thorac Oncol. (2012) 7:1228–34. doi: 10.1097/JTO.0b013e3182582a93
28. Zeng Y, Mayne N, Yang CJ, D'Amico TA, Ng C, Liu CC, et al. A nomogram for predicting cancer-specific survival of TNM 8th edition stage I non-small-cell lung cancer. Ann Surg Oncol. (2019) 26:2053–62. doi: 10.1245/s10434-019-07318-7
29. Liang W, Zhang L, Jiang G, Wang Q, Liu L, Liu D, et al. Development and validation of a nomogram for predicting survival in patients with resected non-small-cell lung cancer. J Clin Oncol. (2015) 33:861–9. doi: 10.1200/JCO.2014.56.6661
30. Agarwal M, Brahmanday G, Chmielewski GW, Welsh RJ, Ravikrishnan KP. Age, tumor size, type of surgery, and gender predict survival in early stage (stage I and II) non-small cell lung cancer after surgical resection. Lung Cancer. (2010) 68:398–402. doi: 10.1016/j.lungcan.2009.08.008
31. Douillard JY, Rosell R, De Lena M, Carpagnano F, Ramlau R, Gonzáles-Larriba JL, et al. Adjuvant vinorelbine plus cisplatin versus observation in patients with completely resected stage IB-IIIA non-small-cell lung cancer (adjuvant navelbine international trialist association [ANITA]): a randomised controlled trial. Lancet Oncol. (2006) 7:719–27. doi: 10.1016/S1470-2045(06)70804-X
32. Arriagada R, Dunant A, Pignon JP, Bergman B, Chabowski M, Grunenwald D, et al. Long-term results of the international adjuvant lung cancer trial evaluating adjuvant cisplatin-based chemotherapy in resected lung cancer. J Clin Oncol. (2010) 28:35–42. doi: 10.1200/JCO.2009.23.2272
33. Shang S, Wang R, Wang F, Wu M, Chen D, Yu J. Treatment patterns for patients with unresected stage III NSCLC: analysis of the surveillance, epidemiology, and End results (SEER) database. Front Oncol. (2022) 12:874022. doi: 10.3389/fonc.2022.874022
34. Guo J, Gao Y, Gong Z, Dong P, Mao Y, Li F, et al. Plasma D-dimer level correlates with age, metastasis, recurrence, tumor-node-metastasis classification (TNM), and treatment of non-small-cell lung cancer (NSCLC) patients. Biomed Res Int. (2021) 2021:9623571. doi: 10.1155/2021/9623571
35. Upadhyay VA, Shah KA, Makwana DP, Raval AP, Shah FD, Rawal RM. Putative stemness markers octamer-binding transcription factor 4, sex-determining region Y-box 2, and NANOG in non-small cell lung carcinoma: a clinicopathological association. J Cancer Res Ther. (2020) 16:804–10. doi: 10.4103/jcrt.JCRT_213_18
36. Gardner LD, Loffredo PhD CA, Langenberg P, George D, Deepak J, Harris CC, et al. Associations between history of chronic lung disease and non-small cell lung carcinoma in Maryland: variations by sex and race. Ann Epidemiol. (2018) 28:543–8. doi: 10.1016/j.annepidem.2018.04.012
37. Barquín M, Calvo V, García-García F, Nuñez B, Sánchez-Herrero E, Serna-Blasco R, et al. Sex is a strong prognostic factor in stage IV non-small-cell lung cancer patients and should be considered in survival rate estimation. Cancer Epidemiol. (2020) 67:101737. doi: 10.1016/j.canep.2020.101737
38. Jia B, Zheng Q, Wang J, Sun H, Zhao J, Wu M, et al. A nomogram model to predict death rate among non-small cell lung cancer (NSCLC) patients with surgery in surveillance, epidemiology, and end results (SEER) database. BMC Cancer. (2020) 20:666. doi: 10.1186/s12885-020-07147-y
39. Pastuszak-Lewandoska D, Domańska-Senderowska D, Antczak A, Kordiak J, Górski P, Czarnecka KH, et al. The expression levels of IL-4/IL-13/STAT6 signaling pathway genes and SOCS3 could help to differentiate the histopathological subtypes of non-small cell lung carcinoma. Mol Diagn Ther. (2018) 22:621–9. doi: 10.1007/s40291-018-0355-7
40. Nagasaka M, Pansare RS, Abdulfatah E, Guan H, Tranchida P, Gadgeel SM. Histologic transformation in NSCLC with PD-1 therapy. J Thorac Oncol. (2017) 12:e133–134. doi: 10.1016/j.jtho.2017.04.026
41. Patel MI, Cheng I, Gomez SL. US lung cancer trends by histologic type. Cancer. (2015) 121:1150–2. doi: 10.1002/cncr.29180
Keywords: SEER, NSCLC, lobectomy, propensity matching, columnar maps
Citation: Zhang H, Ren D, Cheng D, Wang W, Li Y, Wang Y, Lu D and Zhao F (2023) Construction of a mortality risk prediction model for elderly people at risk of lobectomy for NSCLC. Front. Surg. 9:1055338. doi: 10.3389/fsurg.2022.1055338
Received: 27 September 2022; Accepted: 13 December 2022;
Published: 6 January 2023.
Edited by:
Mengling Feng, National University of Singapore, SingaporeReviewed by:
Duilio Divisi, University of L'Aquila, Italy© 2023 Zhang, Ren, Cheng, Wang, Li, Wang, Lu and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Feng Zhao ZG9jdG9yemhhb2ZlbmdAMTYzLmNvbQ==
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Surgical Oncology, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.