- Department of Orthopaedics, Yuhuan People’s Hospital, Taizhou, China
Background and aims: Both casts and braces can be used for post-operational immobilization of ankle fractures. This meta-analysis aimed to assess the complications and functional effects of the two types of immobilization.
Material and methods: PubMed, Embase, Cochrane, and CNKI was searched for randomized controlled trials (published between Jan 1, 1950, and March 2022). Relative risk (RR) or standard mean difference (SMD) with a 95% confidence interval (CI) was used to present the outcomes. The pooled data were assessed by using the fixed-effects model or random-effects model.
Results: A total of 5 randomized controlled studies involving 930 subjects were included according to our inclusion criteria. On the ankle score at 6w,12w and 52w, there was no statistically significant difference between the two groups. In terms of 6w, the brace group showed better ankle dorsiflexion (MD = 6.78, 95% CI 0.56–13.00, p = 0.03) and plantar flexion (MD = 6.58, 95% CI 1.60–11.55, p = 0.01) than the cast group. The wound complications (RR = 3.49, 95% CI 1.32 to 9.24, p = 0.01) and total complications (RR = 3.54, 95% CI 1.92 to 6.50, p < 0.0001) in the brace group were three times more than that in the cast group. There was no statistically significant difference between the two groups in the non-wound complications. There was no statistically significant difference between the two groups in the time of going back to work, swelling of the ankle, and atrophy of the calf muscle.
Conclusion: The short-term and long-term functional outcomes after postoperative treatment of adult ankle fractures with braces are similar to those with casts. The usage of braces may cause three times more wound complications than that of casts.
Introduction
As one of the most commonly seen fractures among humans, ankle fractures have an incidence ranging from 42.2 to 179/per 100,000 person-years (1–5), especially high in adolescent men and middle-aged and old women (1, 3, 4). The high incidence of ankle fractures may be associated with an aging population, increasing obesity rates, and widespread participation in physical activities (6). It greatly impacts society and individuals, increasing the medical and economic burden on society and individuals (7–9). Moreover, limb pain and reduced mobility caused by ankle fractures widely affect patients’ daily social activities, family life, and mental health (10).
Generally, cast immobilization is required for several weeks after an ankle fracture because the cast can provide maximum support for the fracture, promoting the healing of the fracture and decreasing the possibility of delayed union or nonunion of the fracture. However, prolonged ankle immobilization can bring a series of adverse effects, including muscle atrophy, stiffness of joint, joint pain, thrombosis in deep vein, and even some long-term impacts, such as abnormal gait and calf muscle weakness (11, 12). Detachable ankle joint braces, which have emerged in recent years, can avoid adverse consequences caused by the long-term immobilization of ankle joints and promote the early rehabilitation of patients. These braces can be worn freely, allowing patients to perform early rehabilitation activities, however, they may cause some adverse effects, such as wound infection, and dehiscence (11, 13, 14). Both methods are currently widely used in clinical practice. Nevertheless, which one is better for patients with ankle fractures remains debatable and inconclusive.
Therefore, this article aims to analyze the functional prognosis and complications of plaster casts and removable braces.
Material and methods
Our research was reported strictly according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses guidelines (15).
Literature research and study selection
Pubmed, Cochrane, Embase, and CNKI electronic databases were retrieved to identify eligible publications describing the role of braces and casts in the post-operational immobilization published before March 2022. For Pubmed, the following The retrieval strategy used for Pubmed was shown in Appendix.
Inclusion and exclusion criteria
Inclusion criteria: Comparative studies and RCTs comparing the clinical effects of casts versus braces for the treatment of adult ankle fractures (age ≥ 14 years) were eligible, and the outcomes included ankle scores (including Olerud and Molander ankle score, Mazur ankle score), complications (including wound complications and other complications), time of returning to work, motion range, swelling in the ankle, atrophy of the calf muscle. At the same time, eligible studies should provide sufficient data, including standard deviation and mean, for further extraction and pooling, and the number of participants grouped by different treatments for dichotomous and continuous outcomes. Exclusion criteria: retrospective studies; meeting abstracts; case reports; participants which are not adult ankle fractures; studies which cannot get available data.
Study selection
Two researchers (JXi, ZZ) screened the abstracts and titles of all the selected studies in an independent way. The full text was downloaded if they failed to make a decision based on the abstract of a study. If there was any dissent, final decision was made through discussion and consensus with another reviewer (BL). The reasons why certain studies were excluded or ineligible were demonstrated.
Quality assessment
The quality of the included studies were assessed by 2 researchers (QL, JXu) independently, during which the risk of bias assessment tool provided by the Cochrane collaboration in RevMan software was used. The quality assessment involved the following items: (1) selection bias: the generation of sequence and allocation concealment; (2) performance bias: blinding; (3) detection bias: incomplete data on the outcomes, (4) reporting bias: selective reporting of outcomes; and (5) other issues. There are three types of judgment: “Yes” (low risk of bias), “No” (high risk of bias), and “Unclear” (unclear or unknown risk of bias). Any dissent was resolved by consultation from a third reviewer (BL) for a final consensus.
Data extraction
According to the Cochrane guidelines, a data collection spreadsheet was developed before data extraction, including publication information, type of study, patient number, age, follow-up time, outcome measures, and complications. Relevant data were extracted from all included studies by two researchers (BL, CY).
Statistical analysis
The Cochrane Review Manager software, version 5.4.1, was employed in data analysis. The 95% confidence intervals and risk ratios were reported in the present research. p ≤ 0.05 demonstrated that there was a statistically significant difference. The pooled data was assessed by using the fixed-effects or random-effects model. The chi-square test was applied to explore the heterogeneity, with the statistical significance of p < 0.100. The index of I2 was used to quantify the heterogeneity, I2 <50% indicates low heterogeneity and we should choose fixed-effects model. I2 >50% indicates low heterogeneity and we should choose random-effects model.
Results
Descriptions of the included studies
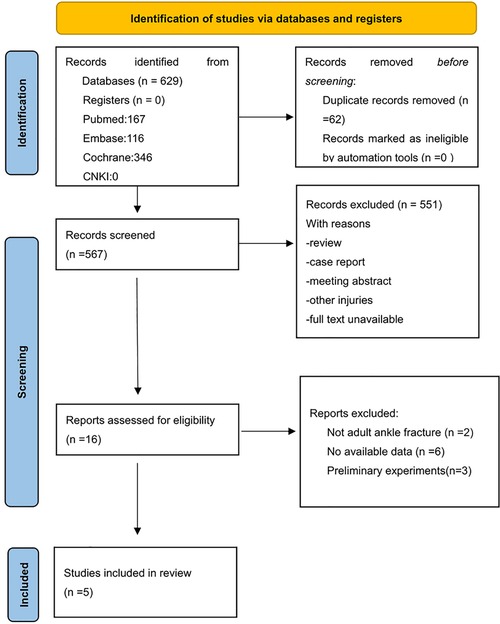
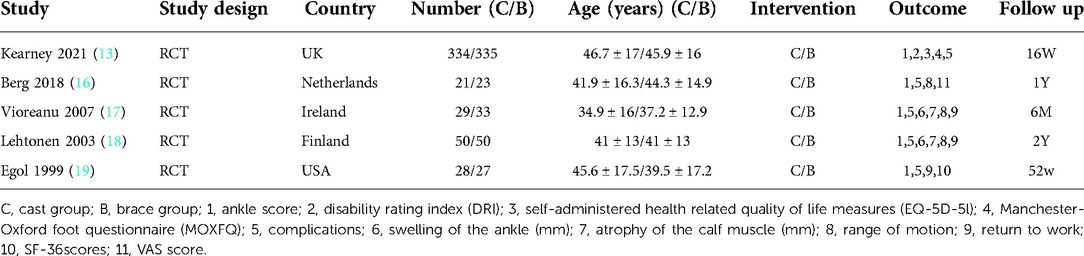
The PRISMA Flow Diagram was used to present the process of study selection (Figure 1). A total of 484 studies were searched from the aforementioned electronic databases, and 5 randomized control trials were eligible. All of the five eligible studies (13, 16–19) compared the two immobilization methods (casts and braces) for ankle fractures. These studies involved 930 patients, with 462 and 468 cases in the cast and brace group, respectively. Among the 5 eligible studies, 2 studies (18, 19) assessed the ankle score at 6w; three (17–19) rated the ankle score at 12w; two (18, 19) evaluated the ankle score at 52w; and two studies (17, 18) examined the time of returning to work, swelling of the ankle, and atrophy of the calf muscle. All of them provided data on complication rate and further details were shown in Table 1.
Bias assessment
Assessment of bias was performed for each of the five eligible RCTs, three of which (13, 16, 18) adopted adequate approach to obtain random sequence. For another two studies, one of them (17) used even or odd day of the date of birth, which revealed that selection bias was at high risk while the other one (19) only used “randomly,” which revealed that the risk of selection bias was unclear. Because the interventions in the five included studies were immobilization methods, it is challenging to apply blinding for research subjects and the staffs. The blinding of study participants and staffs was at high risk in the 5 studies, and the risk of selective reporting and other biases was unclear (Figures 2, 3).
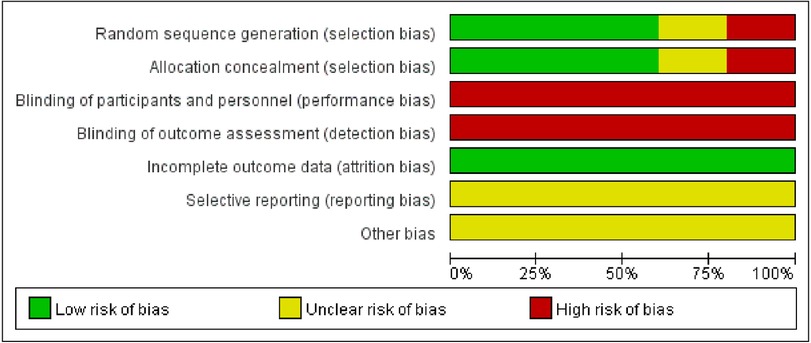
Figure 2. Map for the risk of bias: review the author's decision on the risk of bias items, expressed as a percentage of all the included articles.
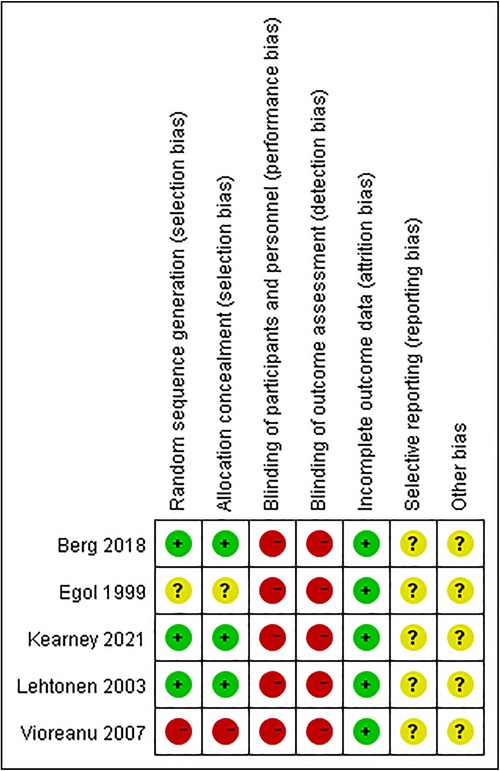
Figure 3. Summary of the risk of bias: review authors’ decision on the risk of bias item one by one for every included article.
Ankle score
Olerud Molander ankle score and Mazur score were used to assessing the ankle function. Two studies assessed the ankle scores at 6 and 52w; three studies assessed the ankle score at 12w. The random-effects model for the meta-analysis on the ankle score at 6w and 12w, and fixed-effects model for the meta-analysis on the ankle scores at 52w. The meta-analyses presented that there was no statistically significant difference on the ankle score at 6w (mean difference 1.39, 95% CI −4.55 to 7.33, I² = 72%, p = 0.06; figure 4), 12w (mean difference 5.56, 95% CI −1.71 to 12.84, I²= 83%, p = 0.13; Supplementary Figure S1) and 52w (mean difference 0.45, 95% CI −2.24 to 3.15, I² = 47%, p = 0.74; Supplementary Figure S2) between the brace and cast groups.
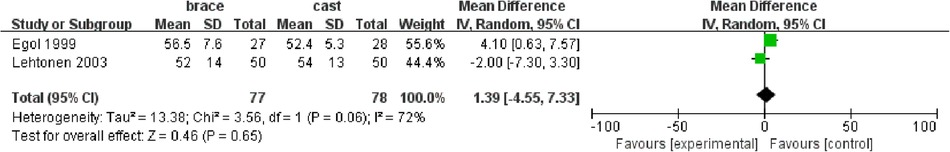
Figure 4. Forest plot of comparing cast versus brace groups for the 6w ankle score. CI, confidence interval.
Complications
All included studies mentioned complications, two reporting no complications and the other three reporting complications, including wound complications and non-wound complications (such as deep vein thrombosis, chronic dysesthesias, chronic allodynia, and loss of internal fixation). However one study only reported wound complications (13). There was no markedly significant difference in non-wound complications (risk ratio 0.84, 95% CI 0.10 to 7.10, I² = 51%, p = 0.15; Supplementary Figure S4) between the two groups. However, the incidence of total complications (risk ratio 3.54, 95% CI 1.92 to 6.50, I² = 32%, p < 0.0001; Supplementary Figure S3) and wound complications (risk ratio 3.49, 95% CI 1.32 to 9.24, I² = 57%, p = 0.01; figure 5) in the brace group were higher compared with the cast group.

Figure 5. Forest plot of the comparison of cast versus brace groups for the wound complication. CI, confidence interval; M-H, Mantel-Haenszel test.
Other outcomes
Two studies reported time of returning to work, swelling and motion range of the ankle, and atrophy of the calf muscle. The random-effects model was only used in the meta-analysis on swelling of the ankle. Between the cast and brace groups, there was no statistically significant difference in the time of returning to work (mean difference −12.61, 95% CI −41.90 to 16.69, I2 = 95%, p = 0.40; Supplementary Figure S5), swelling of the ankle (mean difference −0.28, 95% CI −3.33 to 2.77, I2 = 0%, p = 0.86; Supplementary Figure S6), atrophy of the calf muscle (mean difference −9.59, 95% CI −39.81 to 20.63, I2 = 98%, p = 0.53; Supplementary Figure S7). However, the brace group showed better ankle dorsiflexion (mean difference 6.78, 95% CI 0.56–13.00, I2 = 97%, p = 0.03; Figure 6) and plantar flexion (mean difference 6.58, 95% CI 1.60–11.55, I2 = 64%, p = 0.01; Figure 7) than the cast group in 6w.
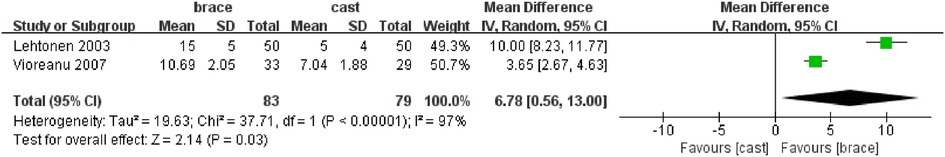
Figure 6. Forest plot of the comparison of cast versus brace groups for the ankle dorsiflexion in 6w. CI, confidence interval.
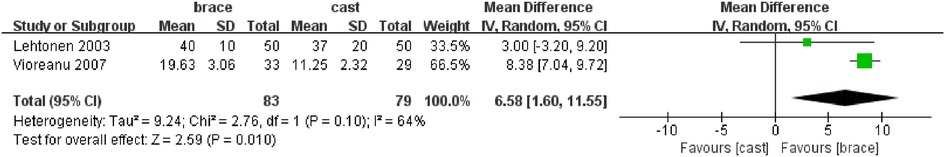
Figure 7. Forest plot of comparing cast versus brace groups for the ankle plantar flexion in 6w. CI, confidence interval.
Discussion
This meta-analysis revealed that the short-term and long-term functional outcomes after postoperative treatment of ankle fractures with braces are similar to those with casts. Although the ankle range of motion in the brace group is better compared with the cast group at the short term (6w). However, the total complications and wound complications in the brace group are three times more than that in the cast group. The non-wound complications were similar between the brace and cast groups. The time of returning to work, swelling of the ankle, and atrophy of the calf muscle show no remarkable difference between brace and cast groups.
Casts and braces have an obvious difference in biomechanical characteristics. One study (20) compared the capability of braces and casts in immobilizing the hindfoot and ankle. As tested, the results showed that casts showed better immobilizing effects in all directions compared with braces. However, casts are irremovable, which may constrain the ankle joint's early mobilization and hinder patients from observing and cleaning their limbs. Conversely, braces are removable and have properly fixed strength. Whether the braces would bring better clinical outcomes remains controversial.
Of the five eligible clinical trials comparing the two immobilization types, three trials (13, 16, 18) concluded that the function after treating ankle fracture using a cast is similar to using a functional brace. Some trails (17, 19) showed that the function was better at short-term follow-up. Our meta-analysis shows that the outcomes of ankle fracture adults using braces are similar to those with casts. Our results are different to previous reviews (14, 21).
Early ankle mobilization has been shown to restore the motion range of the joints, attenuate muscle atrophy (12), and prevent the progression of osteoporosis (22). This provides a theoretical basis for using a functional brace. A systematic review (21) concludes that motion at an early phase contributed to early return to work and improved motion range at 12w in comparison with using cast for immobilization. As mentioned, our study showed that the range of motion in the brace group was markedly improved compared with the cast group. However, this advantage can't transfer to more minor swelling of the ankle, milder atrophy of the calf muscle, or shorter time of returning to work. This difference may be attribute to few studies and higher heterogeneity in our meta-analysis.
Treating ankle fracture patients with a brace may improve the outcomes for a short time, but the complications should not be ignored. Two reviews (14, 21) conclude that using a brace has an elevated risk of infection in wounds compared with a cast. Our meta-analysis shows the total complications and wound complications in patients using braces are three times higher than those using casts. This outcome may be due to the early mobilization affecting the wounds or few soft tissues enveloping the ankle. This meta-analysis was the first to compare the brace and the cast for adult ankle fractures. There are still several limitations to this study. First, few trials are included in the present study. Of only five eligible studies, three studies have relatively small sample sizes. Second, the braces in these trials are different, which may influence the outcomes. Moreover, the technology of orthopedic internal fixation differs from each other, which may influence the stability of the ankle fracture after operation. One study (20) reported that the braces’ fixed strength depends on their conformity to foot shape and the properties of the material. Third, the follow-up time varies in each trial, from 16 weeks to 2 years. It might be possible that the longer the follow-up is, the more adverse events would occur, especially non-wound complications. At last, heterogeneity is statistically significant in the meta-analysis of some outcomes, such as time of returning to work as well as swelling and motion range of ankle. On the other hand, these studies didn't mention the costs or the comfort of the two types, which may influence patients’ final choice.
In conclusion, the functional outcomes after postoperative treatment of adult ankle fractures with braces may be similar to those with casts, no matter in the short-term or long-term. However, using a brace may cause three times wound complications more than a cast. Additional large randomized controlled trials are desired to validate our conclusions.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
All authors contributed to the study conception and design. BL: conceptualization, methodology, software, writing—original draft, data curation, visualization were performed. JXi, ZZ and QL: investigation, writing—original draft, writing—reviewing and editing were performed. JXu and CY: methodology, software, writing—original draft were performed. BL: conceptualization, supervision, project administration were performed. All authors contributed to the article and approved the submitted version.
Acknowledgments
We would like to thank the researchers and study participants for their contributions.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.1055008/full#supplementary-material.
References
1. Scheer RC, Newman JM, Zhou JJ, Oommen AJ, Naziri Q, Shah NV, et al. Ankle fracture epidemiology in the United States: patient-related trends and mechanisms of injury. J Foot Ankle Surg. (2020) 59(3):479–83. doi: 10.1053/j.jfas.2019.09.016
2. Juto H, Nilsson H, Morberg P. Epidemiology of adult ankle fractures: 1756 cases identified in norrbotten county during 2009–2013 and classified according to Ao/Ota. BMC Musculoskelet Disord. (2018) 19(1):441. doi: 10.1186/s12891-018-2326-x
3. Elsoe R, Ostgaard SE, Larsen P. Population-based epidemiology of 9767 ankle fractures. Foot Ankle Surg. (2018) 24(1):34–9. doi: 10.1016/j.fas.2016.11.002
4. Thur CK, Edgren G, Jansson KA, Wretenberg P. Epidemiology of adult ankle fractures in Sweden between 1987 and 2004: a population-based study of 91,410 Swedish inpatients. Acta Orthop. (2012) 83(3):276–81. doi: 10.3109/17453674.2012.672091
5. Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. (2006) 37(8):691–7. doi: 10.1016/j.injury.2006.04.130
6. King CM, Hamilton GA, Cobb M, Carpenter D, Ford LA. Association between ankle fractures and obesity. J Foot Ankle Surg. (2012) 51(5):543–7. doi: 10.1053/j.jfas.2012.05.016
7. Noback PC, Freibott CE, Dougherty T, Swart EF, Rosenwasser MP, Vosseller JT. Estimates of direct and indirect costs of ankle fractures: a prospective analysis. J Bone Joint Surg Am. (2020) 102(24):2166–73. doi: 10.2106/JBJS.20.00539
8. Stull JD, Bhat SB, Kane JM, Raikin SM. Economic burden of inpatient admission of ankle fractures. Foot Ankle Int. (2017) 38(9):997–1004. doi: 10.1177/1071100717709576
9. Murray AM, McDonald SE, Archbold P, Crealey GE. Cost description of inpatient treatment for ankle fracture. Injury. (2011) 42(11):1226–9. doi: 10.1016/j.injury.2010.08.023
10. McKeown R, Kearney RS, Liew ZH, Ellard DR. Patient experiences of an ankle fracture and the most important factors in their recovery: a qualitative interview study. BMJ Open. (2020) 10(2):e033539. doi: 10.1136/bmjopen-2019-033539
11. Lin CW, Donkers NA, Refshauge KM, Beckenkamp PR, Khera K, Moseley AM. Rehabilitation for ankle fractures in adults. Cochrane Database Syst Rev. (2012) 11:Cd005595. doi: 10.1002/14651858.CD005595.pub3
12. Tropp H, Norlin R. Ankle performance after ankle fracture: a randomized study of early mobilization. Foot Ankle Int. (1995) 16(2):79–83. doi: 10.1177/107110079501600205
13. Kearney R, McKeown R, Parsons H, Haque A, Parsons N, Nwankwo H, et al. Use of cast immobilisation versus removable brace in adults with an ankle fracture: multicentre randomised controlled trial. Br Med J (Clin Res Ed). (2021) 374:n1506. doi: 10.1136/bmj.n1506
14. Drakos MC, Murphy CI. Bracing versus casting in ankle fractures. Phys Sportsmed. (2014) 42(4):60–70. doi: 10.3810/psm.2014.11.2092
15. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The prisma 2020 statement: an updated guideline for reporting systematic reviews. Br Med J (Clin Res Ed). (2021) 372:n71. doi: 10.1136/bmj.n71
16. van den Berg C, Haak T, Weil NL, Hoogendoorn JM. Functional bracing treatment for stable type B ankle fractures. Injury. (2018) 49(8):1607–11. doi: 10.1016/j.injury.2018.06.009
17. Vioreanu M, Dudeney S, Hurson B, Kelly E, O'Rourke K, Quinlan W. Early mobilization in a removable cast compared with immobilization in a cast after operative treatment of ankle fractures: a prospective randomized study. Foot Ankle Int. (2007) 28(1):13–9. doi: 10.3113/fai.2007.0003
18. Lehtonen H, Järvinen TL, Honkonen S, Nyman M, Vihtonen K, Järvinen M. Use of a cast compared with a functional ankle brace after operative treatment of an ankle fracture. A prospective, randomized study. J Bone Joint Surg Am. (2003) 85(2):205–11. doi: 10.2106/00004623-200302000-00004
19. Egol KA, Dolan R, Koval KJ. Functional outcome of surgery for fractures of the ankle. A prospective, randomised comparison of management in a cast or a functional brace. J Bone Joint Surg Br. (2000) 82(2):246–9. doi: 10.1302/0301-620X.82B2.10039
20. Raikin SM, Parks BG, Noll KH, Schon LC. Biomechanical evaluation of the ability of casts and braces to immobilize the ankle and hindfoot. Foot Ankle Int. (2001) 22(3):214–9. doi: 10.1177/107110070102200308
21. Thomas G, Whalley H, Modi C. Early mobilization of operatively fixed ankle fractures: a systematic review. Foot Ankle Int. (2009) 30(7):666–74. doi: 10.3113/FAI.2009.0666
Keywords: cast, brace, ankle fractures, post operational, immobilization
Citation: Li B, Xie J, Zhang Z, Liu Q, Xu J and Yang C (2023) Braces versus casts for post-operational immobilization of ankle fractures: A meta-analysis. Front. Surg. 9:1055008. doi: 10.3389/fsurg.2022.1055008
Received: 27 September 2022; Accepted: 25 November 2022;
Published: 25 January 2023.
Edited by:
Enbo Wang, ShengJing Hospital of China Medical University, ChinaReviewed by:
Wei Wang, ShengJing Hospital of China Medical University, ChinaBo Han, Capital Medical University, China
Tianyu Han, Shenyang Northern Hospital, China
© 2023 Li, Xie, Zhang, Liu, Xu and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bin Li MTI4MjQzMTIyMkBxcS5jb20=
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Bin Li
Bin Li Jianying Xie
Jianying Xie