- 1Department of Orthopedic Surgery, The Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, China
- 2Orthopedics Research Institute, Zhejiang University, Hangzhou, China
- 3Key Laboratory of Motor System Disease Research and Precision Therapy of Zhejiang Province, Hangzhou, China
- 4Clinical Research Center of Motor System Disease of Zhejiang Province, Hangzhou, China
Study Design: Retrospective.
Objectives: To investigate the efficacy of cervical single open-door laminoplasty with and without local lateral mass screw fixation and fusion as treatments for cervical spinal cord injuries accompanied by multisegmental spinal canal stenosis.
Setting: The Second Affiliated Hospital, School of Medicine, Zhejiang University.
Methods: Of all enrolled patients, 42 formed a stable group who underwent cervical single open-door laminoplasty alone and 14 formed an unstable group who underwent the procedure combined with lateral mass screw fixation and fusion. Neurological function was evaluated before surgery, at discharge, and at final follow-up using the American Spinal Cord Injury Association (ASIA) impairment scale and the Japanese Orthopedic Association (JOA) score.
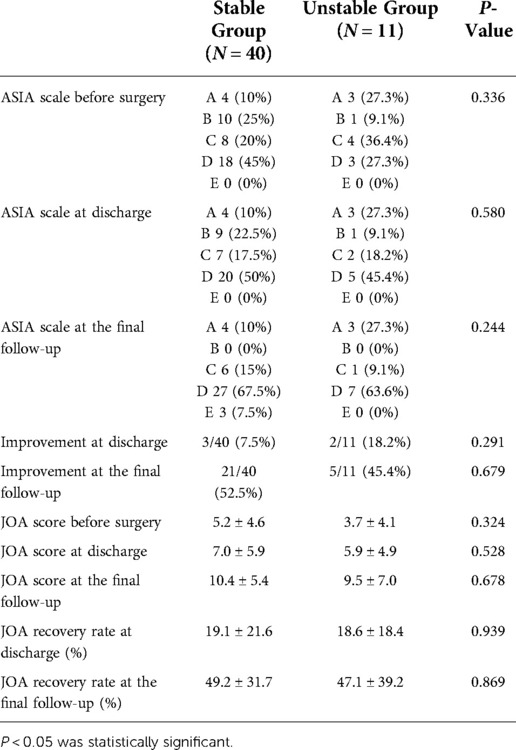
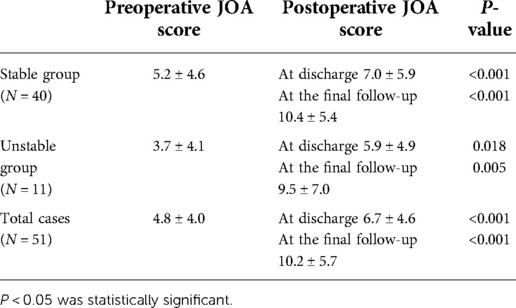
Results: ASIA scores reflected improved neurological function in 52.5% of the stable group (15 with grade-D and 4 with grade-A injuries did not improve) and 45.5% of the unstable group (3 with grade-D and 3 with grade-A injuries did not improve). Postoperative JOA scores reflected 19.1% ± 21.6% improvement in the stable group and 18.6% ± 18.4% improvement in the unstable group (P > 0.05). Final follow-up JOA scores reflected 49.2% ± 31.7% improvement in the stable group and 47.1% ± 39.2% improvement in the unstable group (P > 0.05).
Conclusions: Laminoplasty combined with local fusion aided the treatment of unstable cervical spinal cord injuries and spinal stenosis. Such stenosis is the main pathological factor causing multiple spinal cord compressions in patients with cervical spinal cord injuries.
Introduction
Many high-energy injuries are osseous in nature; however, many low-energy spinal cord injuries in patients with pre-existing cervical stenosis are not associated with any fracture or other cause of instability. The treatment of central cord syndrome without associated instability remains controversial. Classically, nonsurgical treatment was considered to yield results similar to those of surgery (1). This position has recently been questioned; given the lack of instability, some authors have advocated non-fusion surgeries such as posterior laminoplasty (2–4). Fehlings et al. found that early surgical intervention improved neurological recovery in patients with cervical spinal cord injuries (5–7). However, the optimal surgical treatment, especially for patients with pre-existing stenosis and central cord syndrome, remains unclear. This study was a retrospective analysis of data from patients with cervical spinal cord injuries accompanied by multisegmental spinal canal stenosis treated via cervical single open-door laminoplasty. Additional intervertebral disc injuries, anterior longitudinal ligament injuries, and vertebral body avulsion fractures, when present, were stabilized via local lateral mass screw fixation and fusion in addition to laminoplasty. The improvements in neurological symptoms afforded by these treatments, the effects of surgical timing, and the risk factors for local instability were also investigated.
Materials and methods
Subjects
Between December 2014 and August 2017, 56 patients underwent surgery to treat traumatic cervical spinal cord injuries accompanied by multisegmental cervical spinal canal stenosis. The stenosis and cord injury were examined by magnetic resonance imaging (MRI). All patients evidenced greatly increased T2 signal changes in the spinal cord and cervical spinal canal stenosis [cervical sagittal diameter < 13 mm on MR images (8)] at three or more levels. Some stenoses were developmental [cross-sectional distance from the posterior edge of the vertebral body to the spinous process root < 13 mm on computed tomography (CT) images (9–11)]; other stenoses were attributable to the ossification of the posterior longitudinal ligament (OPLL), multilevel intervertebral disc herniation, and ligamenta flava folds. All patients were followed for at least 6 months. The exclusion criteria were vertebral compression, burst or facet fracture, cervical subluxation or dislocation, history of cervical spine surgery, upper cervical vertebral injury, and cervical kyphotic deformity. Patients who died or were lost to follow-up were excluded. We measured improvements using the American Spinal Cord Injury Association (ASIA) impairment scale and the Japanese Orthopedic Association (JOA) score.
Surgical procedure
According to MRI and CT findings, the patients were divided into stable and unstable groups. Stability and instability were defined as the absence and presence, respectively, of intervertebral disc or anterior longitudinal ligament rupture or teardrop-like fracture at the anterior edge of the vertebral body. Simple cervical single open-door laminoplasty was indicated for the stable group. The open-door side was that of the most severe symptom. When symptoms on both sides were similar, we chose the side on which stenosis was more obvious on imaging. On the open-door side, fixation was performed using small titanium-alloy plates (ARCH Laminoplasty System, Synthes GmbH, Switzerland) to support the lamina and prevent postoperative “door closing.” Single open-door laminoplasty with local lateral mass screw fixation was indicated for the unstable group. Single open-door laminoplasty was used to treat the stenotic segment, and laminoplasty plus fixation with lateral mass screws was used to treat the local unstable segments. The lateral mass screws were placed on the hinge side and/or the open-door side. The facet joints of fusion segments were decorticated using a high-speed drill. Next, bone fragments from the autogenous spinous process were implanted in the facet joints. Methylprednisolone (80 mg QD) was prescribed for the first 2 postoperative days and was then reduced to 40 mg QD for the next 2 days to prevent spinal cord edema. Cefuroxime was prescribed at 2 g BID for 2 days postoperatively to prevent infection of the incision. The drainage tube was removed 48 h after surgery, or within 8 h when the drainage volume was <50 ml. After tube removal, the patients were encouraged to leave the bed and walk. The patients were told to protect their necks with a cervical collar for 2 weeks after surgery, and then to commence exercises that rehabilitated neck muscle function. Imaging data from a typical case are provided in Figure 1.
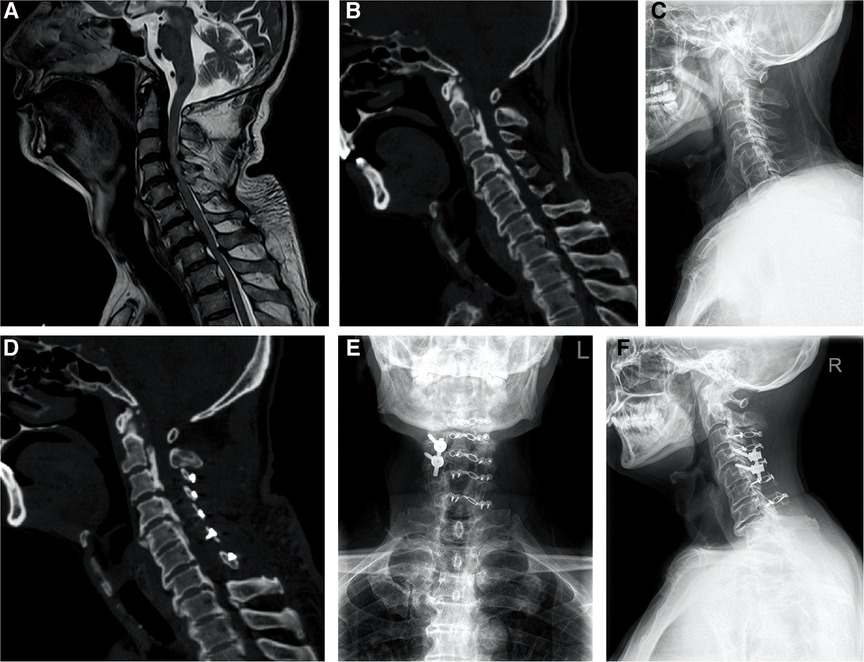
Figure 1. Imaging data of a typical case. A 66-year-old male patient with limb numbness caused by falling from height received single open-door laminoplasty and lateral mass screw fixation and fusion. (A) Preoperative MRI showed the rupture of C4/5 intervertebral disc and anterior longitudinal ligament, and the cervical spinal cord signal of C3–C6 increased on T2-weighted image. (B) Preoperative CT scan confirmed ossification of posterior longitudinal ligament and cervical spinal canal stenosis. (C) Preoperative radiograph. (D) Postoperative CT scan showed that the cervical spinal canal was enlarged and the effect of the operation was clear. (E,F). The anteroposterior and lateral radiographs 1 year after surgery suggested that the fixations were in good condition.
Assessments
We recorded patient sex and age, cause of injury, time from injury to operation, duration of operation, amount of intraoperative blood loss, pathological type of cervical spinal stenosis, numbers and distributions of high-signal segments in the cervical spinal cord, and unstable segment pathological type and distribution. Patients' neurological status was evaluated before surgery, at discharge, and at the final follow-up using the ASIA impairment scale, and was classified as grades A–E based on symptom severity. Improvement was defined as at least one increment of improvement in the ASIA score at the final follow-up assessment. Neurological function was also evaluated using the JOA score before surgery, at discharge, and at the final follow-up. The JOA recovery rates at discharge and final follow-up were calculated using the Hirabayashi method as: [(postoperative JOA score—preoperative JOA score)/(17—preoperative JOA score)] × 100%.
Statistical analysis
All statistical analyses were performed using SPSS software (ver. 12.0 for Windows; SPSS Inc., Chicago, IL, USA). We present means ± standard deviations. The unpaired independent-samples t test, Mann–Whitney U test, and chi-squared test were used, as appropriate, for group comparisons. P values < 0.05 were considered to be statistically significant.
Results
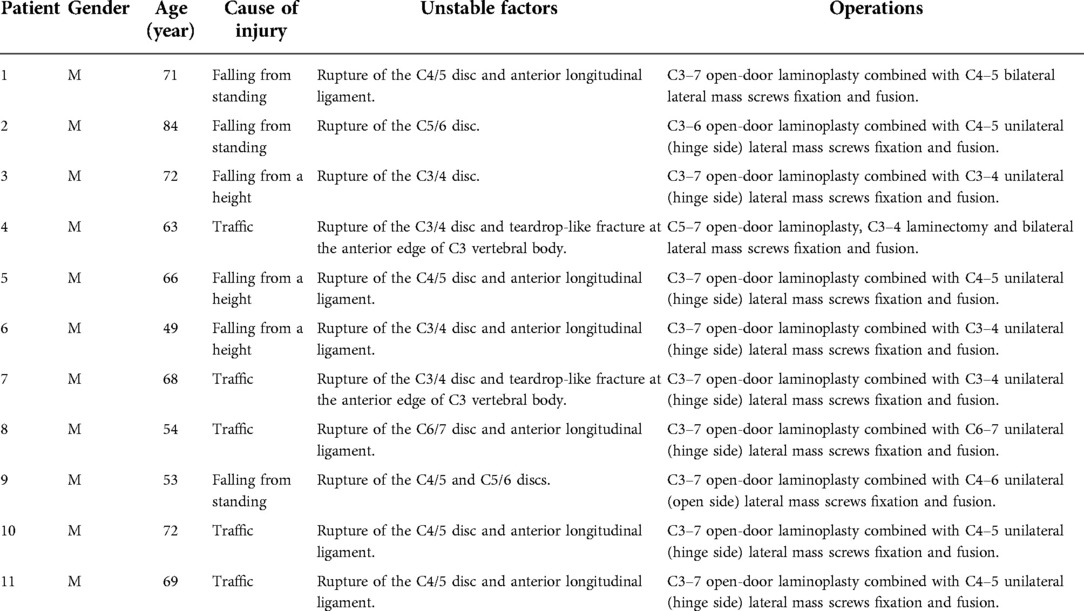
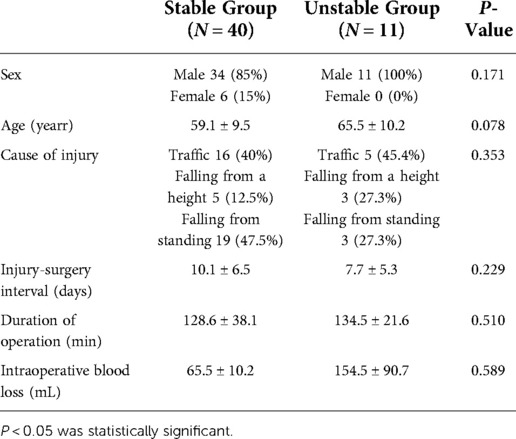
The stable group comprised 42 patients (36 males and 6 females), including 1 patient who died and another who was lost to follow-up. The mean age was 59.1 ± 9.5 (range, 34–75) years, and the average time from injury to surgery was 10.1 ± 6.5 (range, 3–32) days. All patients in the stable group underwent cervical single open-door laminoplasty. Thirty-two patients required surgery from C3 to C7, eight patients required C3–C6 laminoplasty, and two patients required C4–C7 laminoplasty. The mean operation time was 128.6 ± 38.1 min and the average intraoperative blood loss was 136.3 ± 120.9 ml. The unstable group consisted of 14 patients (all male), including 3 who died during follow-up; thus, data from only 11 patients are provided in Table 1. The average age was 65.5 ± 10.2 (range, 49–84) years. The average time from injury to surgery was 7.7 ± 5.3 (range, 3–22) days. The operative details, including segments treated, are provided in Table 2. The average operative time was 134.5 ± 21.6 min and the average blood loss was 154.5 ± 90.7 ml. Patient age, the interval from injury to surgery, the operative time, and the amount of intraoperative blood loss did not differ between groups (all P > 0.05). Pre- and postoperative radiographic data from a typical case (from the unstable group) are provided in Figure 1.
High-energy injuries (falls from heights and car accidents) accounted for 52.5% of injuries in the stable group and 72.7% of injuries in the unstable group (P = 0.230). In the stable group, 64.3% of cervical canal stenoses were developmental; 9.5% of these cases were combined with OPLL. OPLL alone was observed in 21.4% of cases and simple multilevel disc herniation was observed in 14.3% of cases in this group. In the unstable group, all cervical spinal canal stenoses were developmental, and 35.7% of them were combined with OPLL (P = 0.03). Intervertebral disc injuries and vertebral body avulsion fractures were located principally in the regions of stress concentration in patients with multisegmental OPLL or intervertebral joint stiffness; the proportion of such patients in the unstable group was 57.1%.
Neurological function improvements are shown in Tables 3, 4. ASIA scores reflected improvement at the final follow-up assessment in 52.5% of patients in the stable group (15 patients with grade-D and 4 patients with grade-A function did not improve). Six of seven grade-D central spinal cord syndrome cases in this group remained grade D at the end of follow-up, accounting for 40.0% of unimproved cases. In the unstable group, 45.5% of patients improved (three patients each with grade-D and grade-A function did not). Postoperative JOA scores reflected 19.1% ± 21.6% improvement in the stable group and 18.6% ± 18.4% improvement in the unstable group (P > 0.05). JOA scores from the final follow-up assessments reflected 49.2% ± 31.7% improvement in the stable group and 47.1% ± 39.2% improvement in the unstable group. Improvements reflected by JOA scores obtained at discharge and final follow-up did not differ between groups. JOA scores improved in patients with grade-B–D neurological function according to the ASIA impairment scale.
Discussion
We found that 73.2% of patients with cervical spinal cord injuries but no significant fracture or dislocation had developmental spinal canal stenosis (anteroposterior spinal canal diameter < 13 mm). The relationship between such stenosis and cervical spinal cord injury has been of concern to researchers. In asymptomatic populations, the incidences of cervical spinal cord compression and signal change are related closely to developmental spinal canal stenosis (9). Morishita et al. (11) showed that the kinematic properties of the cervical spine in patients with such stenosis (diameter < 13 mm) explain secondary pathological changes. This type of stenosis is a risk factor for cervical spondylosis (12, 13), and it is associated with a higher incidence of cervical spinal cord injury after mild trauma because it reduces the functional reserve space for the spinal cord. Aarabi et al. (14) reported a cervical spinal canal stenosis rate of 37.4% in a sample of 211 patients with central spinal cord injury syndrome. Aebli (15) found that Pavlov ratios < 0.7 and anteroposterior spinal canal diameter < 8 mm were risk factors for cervical spinal cord injury after mild trauma.
The use of surgery to treat cervical spinal cord injuries with no significant fracture or dislocation remains controversial. Similar outcomes of nonoperative and operative treatments have been reported (1, 16). However, other studies have shown that spinal canal decompression yields better results for patients with stable cervical spinal cord injuries and spinal canal stenosis (3, 4). In a retrospective study, Gu et al. (2) found more improvement, according to JOA and SF-36 scores, among patients with cervical spinal cord injuries and OPLL who underwent laminoplasty (n = 31) than among those who underwent nonoperative treatment (n = 29 cases). The degree of improvement in the JOA score at the final follow-up was about 50%. The JOA scores of all patients with grade-B–D function improved, whereas those of patients with grade-A function did not; no patient evidenced neurological deterioration after surgery. A prospective study on this topic would be difficult to conduct because the conditions and pathogenic factors of patients with spinal cord injuries are complex. Further research is needed.
The optimal timing of surgery remains controversial. Fehlings et al. (17) found no significant difference in neurological function improvement between early (≤24 h after injury) and late (>24 h after injury) surgery groups. Another study showed that operation within 8 h after injury was better than operation 8–24 h after injury (6). Early surgery is usually defined as that performed within 24 or 72 h. In China, however, primary hospitals lack experienced surgeons and the required surgical equipment, and patients are referred to regional medical centers. Most patients included in this study were referred from local primary hospitals, and some had other serious injuries, such as traumatic brain injuries and chest trauma. Thus, the performance of all emergency operations within 8 or 24 h is difficult. In a retrospective sample of 595 patients from 6 hospitals in China, 212 patients underwent early (<72 h after injury) surgery and 383 patients underwent late (≥72 h after injury) surgery (5). ICU stays were longer but hospital stays were shorter in the early surgery group than in the late surgery group, and the rates of complications (pneumonia, wound infection, and sepsis) did not differ between groups. More importantly, neurological improvements did not differ significantly between groups, but the neurological deterioration and mortality rates were higher in the early surgery group than in the late surgery group. The authors concluded that the performance of surgery >72 h after injury was safer. We also found that surgeries performed at this interval were effective; we noted no postoperative neurological deterioration in these cases. When resources are available and the patient's condition permits, emergency surgery (performed within 8 h of injury) may aid functional recovery in patients with severely impaired neurological function (ASIA grade A). Some authors have recommended emergency surgery for patients exhibiting locking of the bilateral cervical facets with incomplete paralysis or worsening neurological function (6).
A semi-hybrid surgical technique involving laminoplasty and internal screw fixation has been used to treat degenerative cervical diseases, including cervical spondylosis with kyphosis (18, 19) and cervical spondylosis (or OPLL) combined with the presence of unstable segments (20, 21). However, few reports on the use of this technique to treat traumatic cervical spinal cord injuries have been published (22–24). The technique not only reduces the need for operation via the anterior approach, but avoids the posterior scar formation and risk of C5 nerve root palsy associated with laminectomy and internal fixation (22, 25). One report describes the treatment of cervical spinal cord injuries in six patients in Korea via single open-door laminoplasty combined with internal fixation with unilateral lateral mass screws; the clinical results were good (22). As kyphosis was present, the authors used long-segment lateral mass screw fixation (i.e., with an average of five screws) to correct the cervical deformities. Some surgeons have combined laminoplasty with pedicle screw fixation to treat cervical spinal canal stenosis accompanied by unstable fractures (23, 24). We found that cervical single open-door laminoplasty combined with short-segment lateral mass screw fixation enabled adequate stabilization of local segment instabilities caused by intervertebral disc damage or avulsion fracture, and that the neurological improvement rate did not differ significantly between the stable and unstable groups. We found that many unstable segments were located in regions of stress concentration, such as areas of discontinuous ossification in patients with multisegmental OPLL or intervertebral joint stiffness. Thus, areas of stress concentration constitute a risk factor for local instability after mild trauma.
The limitations of this study include the small sample and slight variation in hybrid techniques employed, specifically the side and number of lateral mass screw implantations, according to surgeons’ preferences. More long-term or multicenter data are required. In addition, this study was retrospective and lacked a control group. The evidence does not yet reveal whether the type of operation or the injury-to-operation interval (> or <72 h) affects the neurological outcomes.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by Human Research Ethics Committee of the Second Affiliated Hospital of Zhejiang University School of Medicine. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
HX: was responsible for writing the manuscript, extracting data, interpreting results and provided feedback on the report. These authors (ZY,HX) contributed equally to this work and should be considered co-first authors. All authors contributed to the article and approved the submitted version.
Acknowledgments
Great acknowledgement is made to Zhang Hua who gave me considerable help by means of suggestion, comments and criticism.
Funding
This work is in financially supported by the National Natural Science Foundation of China (NSFC) [grant number 81672246].
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ASIA, American spinal cord injury association; JOA, Japanese orthopedic association; MRI, magnetic resonance imaging; OPLL, ossification of posterior longitudinal ligament.
References
1. Mazaki T, Ito Y, Sugimoto Y, Koshimune K, Tanaka M, Ozaki T. Does laminoplasty really improve neurological status in patients with cervical spinal cord injury without bone and disc injury? A prospective study about neurological recovery and early complications. Arch Orthop Trauma Surg. (2013) 133(10):1401–5. doi: 10.1007/s00402-013-1810-x
2. Gu Y, Chen L, Dong RB, Feng Y, Yang HL, Tang TS. Laminoplasty versus conservative treatment for acute cervical spinal cord injury caused by ossification of the posterior longitudinal ligament after minor trauma. Spine J. (2014) 14(2):344–52. doi: 10.1016/j.spinee.2013.06.083
3. Lee HJ, Kim HS, Nam KH, Han IH, Cho WH, Choi BK. Neurologic outcome of laminoplasty for acute traumatic spinal cord injury without instability. Korean J Spine. (2013) 10(3):133–7. doi: 10.14245/kjs.2013.10.3.133
4. Ghasemi AA, Behfar B. Outcome of laminoplasty in cervical spinal cord injury with stable spine. Asian J Neurosurg. (2016) 11(3):282–6. doi: 10.4103/1793-5482.175638
5. Liu Y, Shi CG, Wang XW, Chen HJ, Wang C, Cao P, et al. Timing of surgical decompression for traumatic cervical spinal cord injury. Int Orthop. (2015) 39(12):2457–63. doi: 10.1007/s00264-014-2652-z
6. Fehlings MG, Perrin RG. The role and timing of early decompression for cervical spinal cord injury: update with a review of recent clinical evidence. Injury. (2005) 36(Suppl 2):B13–26. doi: 10.1016/j.injury.2005.06.011
7. Jug M, Kejžar N, Vesel M, Al Mawed S, Dobravec M. Neurological recovery after traumatic cervical spinal cord injury is superior if surgical decompression and instrumented fusion are performed within 8 hours versus 8 to 24 hours after injury: a single center experience. J Neurotrauma. (2015) 32(18):1385–92. doi: 10.1089/neu.2014.3767
8. Inoue H, Ohmori K, Takatsu T, Teramoto T, Ishida Y, Suzuki K. Morphological analysis of the cervical spinal canal, dural tube and spinal cord in normal individuals using CT. Neuroradiology. (1996) 38(2):148–51. doi: 10.1007/BF00604802
9. Nakashima H, Yukawa Y, Suda K, Yamagata M, Ueta T, Kato F. Narrow cervical canal in 1211 asymptomatic healthy subjects: the relationship with spinal cord compression on MRI. Eur Spine J. (2016) 25(7):2149–54. doi: 10.1007/s00586-016-4608-z
10. Bajwa NS, Toy JO, Young EY, Ahn NU. Establishment of parameters for congenital stenosis of the cervical spine: an anatomic descriptive analysis of 1066 cadaveric specimens. Eur Spine J. (2012) 21(12):2467–74. doi: 10.1007/s00586-012-2437-2
11. Bajwa NS, Toy JO, Young EY, Ahn NU. The relationship between the cervical spinal canal diameter and the pathological changes in the cervical spine. Eur Spine J. (2009) 18(6):877–83. doi: 10.1007/s00586-009-0968-y
12. Edwards WC, LaRocca H. The developmental segmental sagittal diameter of the cervical spinal canal in patients with cervical spondylosis. Spine. (1983) 8(1):20–7. doi: 10.1097/00007632-198301000-00003
13. Hayashi H, Okada K, Hamada M, Tada K, Ueno R. Etiologic factors of myelopathy. A radiographic evaluation of the aging changes in the cervical spine. Clin Orthop Relat Res. (1987) (214):200–9. 10.1007/BF004568773791744
14. Aarabi B, Alexander M, Mirvis SE, Shanmuganathan K, Chesler D, Maulucci C, et al. Predictors of outcome in acute traumatic central cord syndrome due to spinal stenosis. J Neurosurg Spine. (2011) 14(1):122–30. doi: 10.3171/2010.9.SPINE09922
15. Aebli N, Wicki AG, Rüegg TB, Petrou N, Eisenlohr H, Krebs J. The torg-pavlov ratio for the prediction of acute spinal cord injury after a minor trauma to the cervical spine. Spine J. (2013) 13(6):605–12. doi: 10.1016/j.spinee.2012.10.039
16. Kawano O, Ueta T, Shiba K, Iwamoto Y. Outcome of decompression surgery for cervical spinal cord injury without bone and disc injury in patients with spinal cord compression: a multicenter prospective study. Spinal Cord. (2010) 48(7):548–53. doi: 10.1038/sc.2009.179
17. Fehlings MG, Vaccaro A, Wilson JR, Singh AW, Cadotte D, Harrop JS, et al. Early versus delayed decompression for traumatic cervical spinal cord injury: results of the surgical timing in acute spinal cord injury study (STASCIS). PLoS One. (2012) 7(2):e32037. doi: 10.1371/journal.pone.0032037
18. Yeh KT, Lee RP, Chen IH, Yu TC, Liu KL, Peng CH, et al. Laminoplasty instead of laminectomy as a decompression method in posterior instrumented fusion for degenerative cervical kyphosis with stenosis. J Orthop Surg Res. (2015) 10:138. doi: 10.1186/s13018-015-0280-y
19. Miyamoto H, Maeno K, Uno K, Kakutani K, Nishida K, Sumi M. Outcomes of surgical intervention for cervical spondylotic myelopathy accompanying local kyphosis (comparison between laminoplasty alone and posterior reconstruction surgery using the screw-rod system). Eur Spine J. (2014) 23(2):341–6. doi: 10.1007/s00586-013-2923-1
20. Uehara M, Takahashi J, Ogihara N, Hirabayashi H, Hashidate H, Mukaiyama K, et al. Cervical pedicle screw fixation combined with laminoplasty for cervical spondylotic myelopathy with instability. Asian Spine J. (2012) 6(4):241–8. doi: 10.4184/asj.2012.6.4.241
21. Chen Y, Wang X, Chen D, Miao J, Liao X, Yu F. Posterior hybrid technique for ossification of the posterior longitudinal ligament associated with segmental instability in the cervical spine. J Spinal Disord Tech. (2014) 27(4):240–4. doi: 10.1097/BSD.0b013e31825c6e2f
22. Son S, Lee SG, Park CW, Kim WK. Combined open door laminoplasty with unilateral screw fixation for unstable multi-level cervical stenosis: a preliminary report. J Korean Neurosurg Soc. (2013) 53(2):83–8. doi: 10.3340/jkns.2013.53.2.83
23. Zhang L, Sun Y, Jiang Y, Wang Y. Posterior cervical pedicle screw-rod/plate instrumentation combined with unilateral open-door laminoplasty for the treatment of acute cervical spinal cord compression injury: report of five cases. Turk Neurosurg. (2018) 28(1):152–7. 10.5137/1019-5149.JTN.15052-15.127593761
24. Xu ZW, Lun DX. Surgical management of multilevel cervical spinal stenosis and spinal cord injury complicated by cervical spine fracture. J Orthop Surg Res. (2014) 9:77. doi: 10.1186/s13018-014-0077-4
Keywords: laminoplasty, lateral mass screw fixation, spinal cord injury, cervical spinal canal stenosis, neurological function
Citation: Yu Z, Xie H, Ouyang Z and Zhang H (2023) Cervical single open-door laminoplasty with or without local lateral mass screw fixation and fusion to treat cervical spinal cord injuries accompanied by segmental spinal canal stenosis. Front. Surg. 9:1050308. doi: 10.3389/fsurg.2022.1050308
Received: 21 September 2022; Accepted: 28 November 2022;
Published: 4 January 2023.
Edited by:
Fuxin Wei, Sun Yat-sen University, ChinaReviewed by:
Guangzhou Li, The Affiliated Hospital of Southwest Medical University, ChinaMingzhu Zhang, Capital Medical University, China
© 2023 Yu, Xie, Ouyang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hua Zhang emhhbmdodWEwNjhAemp1LmVkdS5jbg==
†Present Address Hua ZhangDepartment of Orthopedic Surgery, The Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, China; Orthopedics Research Institute, Zhejiang University, Hangzhou, China; Key Laboratory of Motor System Disease Research and Precision Therapy of Zhejiang Province, Hangzhou, China; Clinical Research Center of Motor System Disease of Zhejiang Province, Hangzhou, China
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Zihao Yu
Zihao Yu Hongwei Xie1,2,3,4
Hongwei Xie1,2,3,4