- 1Department of Thoracic Surgery, The Affiliated Yantai Yuhuangding Hospital of Qingdao University, Yantai, China
- 2The Second Medical College, Binzhou Medical University, Yantai, China
- 3Department of Pharmacy, The Affiliated Yantai Yuhuangding Hospital of Qingdao University, Yantai, China
Introduction: Surgeons have widely regarded sternotomy (ST) as the standard surgical method for thymectomy. Minimally invasive methods for thymectomy, including video-assisted and robot-assisted thoracoscopic surgery (RATS), have been explored. There are some studies have researched and compared the outcomes of patients after robotic and sternotomy procedure.
Methods: We searched the databases of Pubmed, the Cochrane Library, Embase and selected the studies on the efficacy and safety of RATS or ST for thymectomy. Meta-analysis was performed for operation time, operation blood loss, postoperative drainage time, operative complications and hospitalization time.
Results: A total of 16 cohort studies with 1,089 patients were included. Compared to ST, RATS is an appropriate alternative for thymectomy which reduced operation blood loss [standardized mean difference (SMD) = −1.82, 95% confidence interval (95% CI): (−2.64, −0.99), p = 0.000], postoperative drainage time [SMD = −2.47, 95% Cl: (−3.45, −1.48), p = 0.000], operative complications [odds ratio (OR) = 0.31, 95% Cl: (0.18, 0.51), p = 0.000] and hospitalization time [SMD = −1.62, 95% Cl: (−2.16, −1.07), p = 0.000].
Conclusions: This meta-analysis based on cohort studies shows that RATS has more advantages over ST. Therefore, RATS is a more advanced and suitable surgical method for thymectomy.
Introduction
Thymus is an important immune and endocrine organ in human body. Thymoma is an unusual thymic tumor. Its annual incidence rate in the population is about 0.15/100,000 (1). Surgical intervention is the only effective method for its treatment. In the past, median sternotomy was regarded as the first surgical approach for all types of thymomas, which ensured the safety of tumor resection. Sternotomy has been widely considered and applied to the standard surgical method of thymectomy. Because sternotomy is an invasive operation, the operation involves the incision of long bone, which may lead to complications such as intraoperative bleeding, postoperative pain and infection (2). Surgeons have explored many minimally invasive surgery approaches, including video-assisted and robot-assisted thoracoscopic surgery. In minimally invasive surgery, video-assisted thoracoscopic surgery (VATS) is the most popular and commonly used approach. Thoracoscopic surgery is considered to be the first choice for thymectomy because it can reduce intraoperative bleeding, postoperative pain and the incidence of postoperative complications (3–5). However, video-assisted thoracoscopy has some limitations. Thymectomy sometimes requires fine anatomy or complex surgery in the narrow upper mediastinum, which is technically challenging.
As an advanced minimally invasive surgery platform, robot-assisted surgery overcomes the limitations of traditional thoracoscopic surgery. The introduction and development of the da Vinci Robotic System has brought many obvious conveniences to surgeons, such as providing clear three-dimensional images, greater freedom of movement of surgical instruments in limited space, and reducing hand-related tremors. The da Vinci Robotic System also can help surgeons achieve more accurate anatomy, resulting in better clinical and tumor results, especially when thymectomy is performed in a narrow space (6). At present, it is not clear whether robot-assisted minimally invasive surgery can bring more benefits to doctors and patients. Many researchers have explored robotic treatment of thymic diseases, and some comparative studies on the surgical effects of robotic and sternotomy surgery have been published. The original purpose of this meta-analysis is to confirm the feasibility and safety advantages of robot-assisted thymectomy compared with sternotomy.
Methods
Search strategies
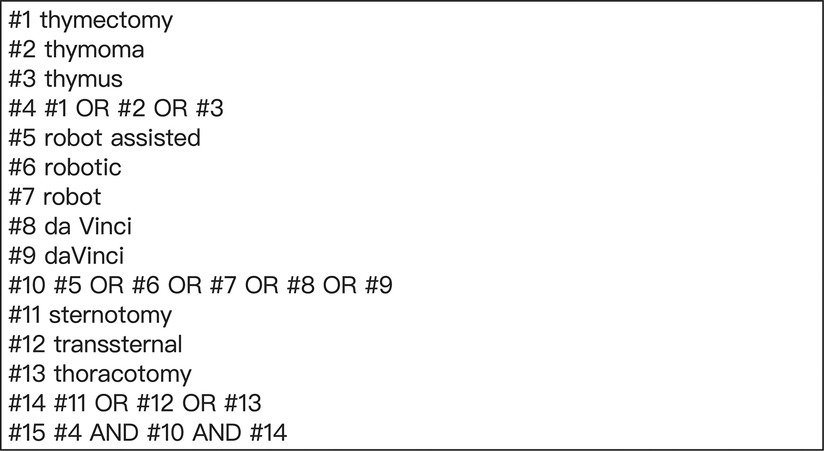
We searched and identified relevant studies from the databases of Pubmed, the Cochrane Library, Embase (from the establishment time of database to August 2022). The search terms that related to thymectomy, sternotomy and robot assisted are as follows: “thymectomy”, “thymoma”, “thymus”, “sternotomy”, “transsternal”, “thoracotomy”, “robot assisted”, “robotic”, “robot”, “da Vinci” and “daVinci”. Figure 1 shows the search strategy. In addition, if we find other studies closely related to robot-assisted thoracoscopic thymectomy in other literatures, we will further search and evaluate them.
Inclusion and exclusion criteria of studies
Inclusion criteria
(1) The English language journal study; (2) the study described robot-assisted surgery and sternotomy for thymectomy; (3) the study provided original data.
Exclusion criteria
(1) Article was not in English; (2) review, conference abstracts, or case report; (3) unable to extract data.
Identification of literature
Three independent researchers reviewed titles or abstracts of the studies. The studies that meet the inclusion criteria were searched for full-text evaluation. The trials selected for detailed analysis were analyzed by three researchers, and disagreements were resolved by the fourth researcher.
Collection of study indicators
The data that we collected included: (1) publication date and country of literature; (2) the number of subjects of each research; (3) the mean age of patients; (4) outcomes include: operation time, operation blood loss, postoperative drainage time, operative complications and hospitalization time.
Quality assessment of included studies
We assessed the quality of all included studies from the perspectives of selection, comparability and exposure by the Newcastle–Ottawa Scale (NOS). The star system was used to score all studies, with a maximum of 9 stars. The specific evaluation criteria are that 8–9 stars represent high quality and 6–7 stars represent reasonable.
Statistical methods and analysis
We used Stata/SE 17.0 software to estimate statistical significance. The odds ratio (OR) was used to assess binary variables and the standardized mean difference (SMD) was used to assess continuous variables. The identification of heterogeneity of studies was calculated by the I2 statistics. When the heterogeneity test result is significant (I2 > 50% or p < 0.05), a random-effect model was used to evaluate. Otherwise, a fixed-effect model was used. At the same time, publication bias was assessed by Egger's test and Begg's test.
Results
Study selection process
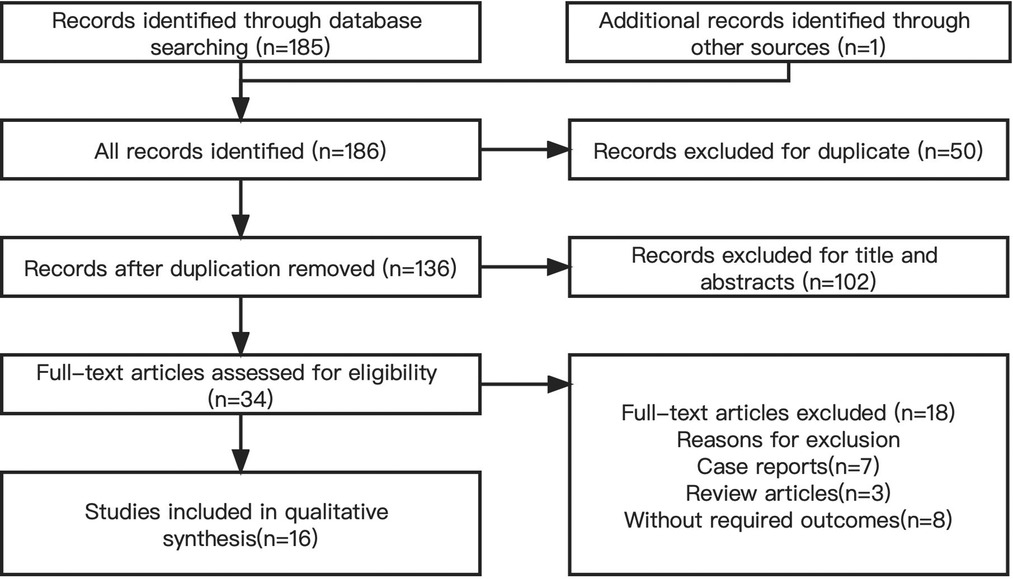
We identified 186 studies, of which 16 (2, 6–20) were included in our analysis. All studies involved a total of 1,089 patients. Figure 2 shows the study selection process.
Characteristics and quality of study
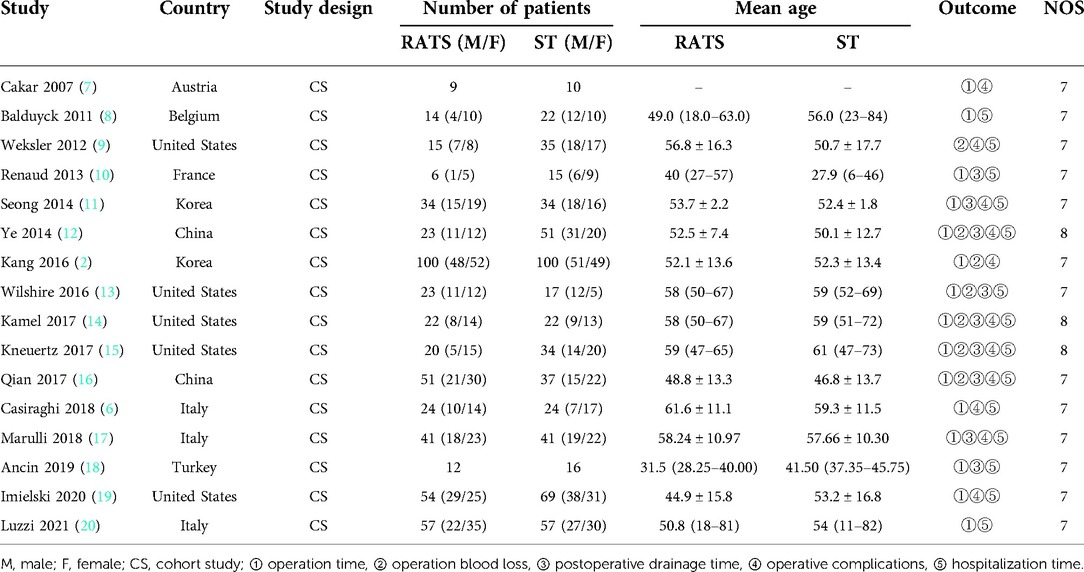
Table 1 shows the characteristics and quality of the studies.
Analysis results
Operation time
Fifteen studies reported operation time. According to the heterogeneity test results, it can be concluded that statistical heterogeneity was significant between the fifteen studies (p = 0.000, I2 = 92.3%), we used random-effect model for calculation. The data revealed that significant difference did not exist between the RATS and the ST [SMD = 0.24, 95% CI: (−0.25, 0.74), p = 0.328] (Figure 3).
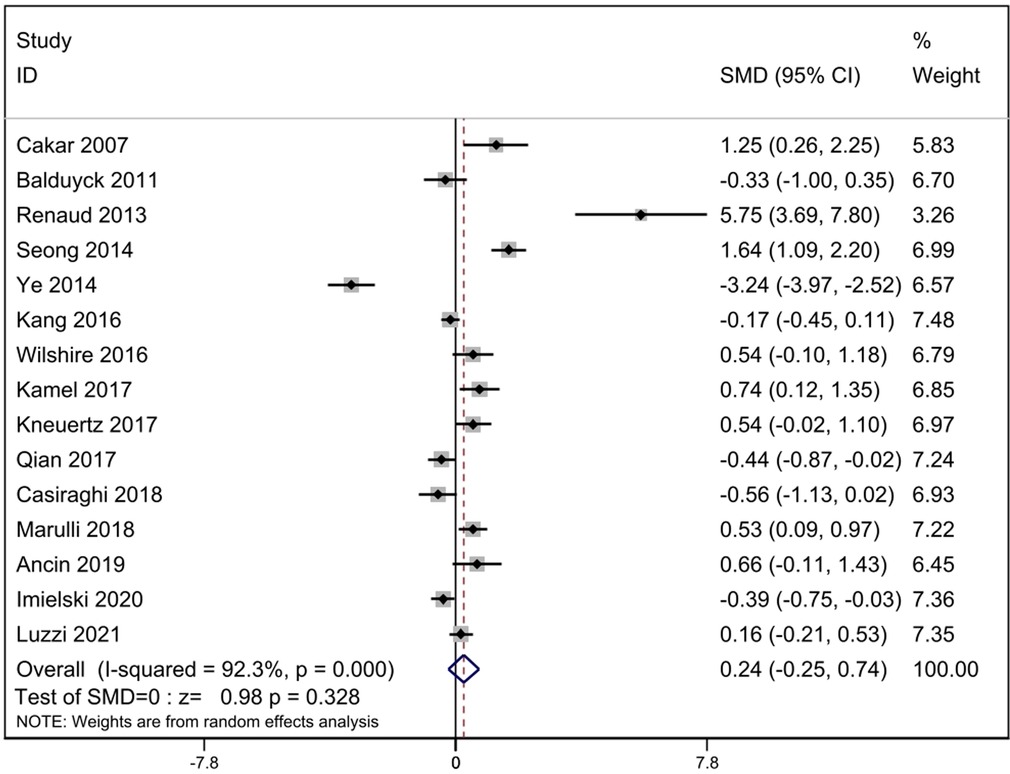
Figure 3. Comparison of operation time between RATS and ST. SMD, standardized mean difference; CI, confidence interval; RATS, robot-assisted thoracoscopic surgery; ST, sternotomy.
Operation blood loss
Operation blood loss was compared in seven studies. According to the heterogeneity test, it can be concluded that statistical heterogeneity was significant between the seven studies (p = 0.000, I2 = 93.4%), we calculated by random-effect model. The result revealed that operation blood loss was less in the RATS group [SMD = −1.82, 95% Cl: (−2.64, −0.99), p = 0.000] (Figure 4).
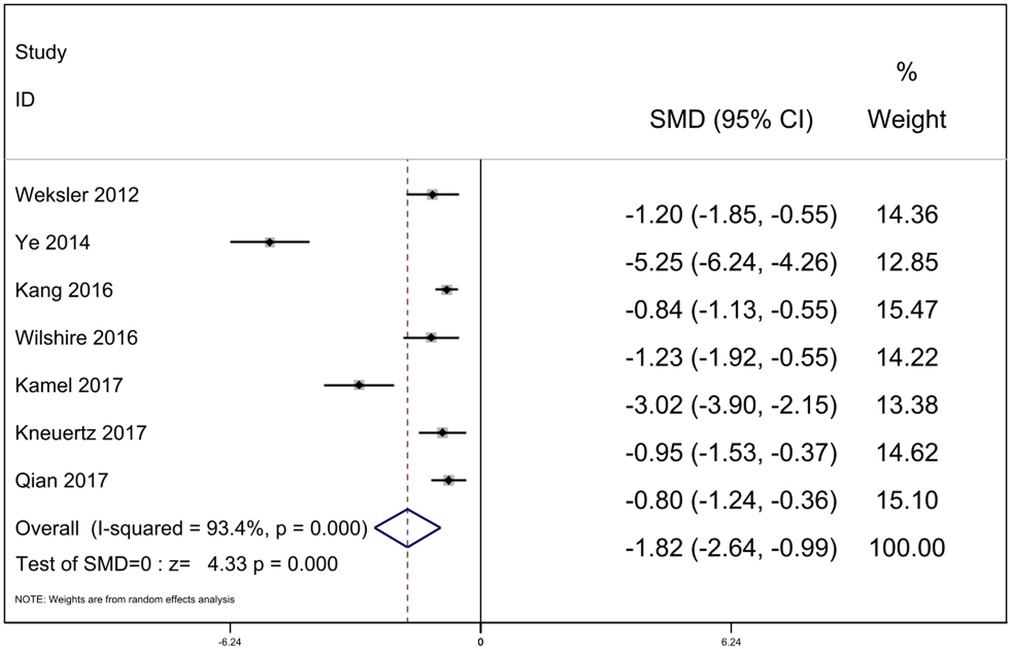
Figure 4. Comparison of operation blood loss between RATS and ST. SMD, standardized mean difference; CI, confidence interval; RATS, robot-assisted thoracoscopic surgery; ST, sternotomy.
Postoperative drainage time
Nine studies reported complete data of postoperative drainage time. The statistical heterogeneity was significant in the nine studies. We uesd the random-effect model for calculation (p = 0.000, I2 = 94.2%). The result indicated that postoperative drainage time were less in the RATS group [SMD = −2.47, 95% Cl: (−3.45, −1.48), p = 0.000] (Figure 5).
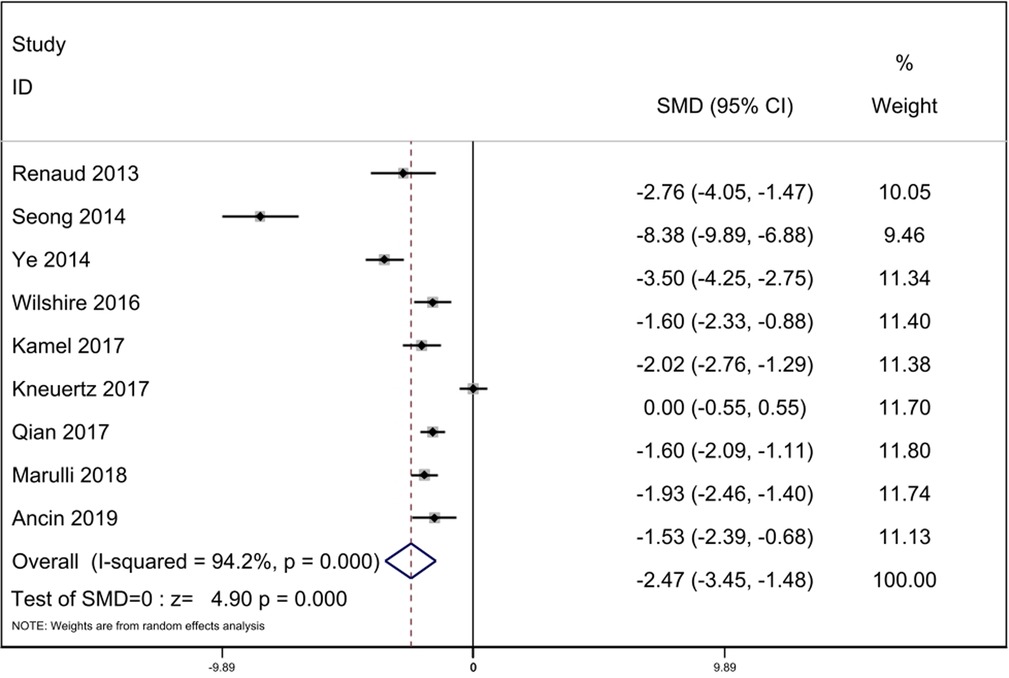
Figure 5. Comparison of postoperative drainage time between RATS and ST. SMD, standardized mean difference; CI, confidence interval; RATS, robot-assisted thoracoscopic surgery; ST, sternotomy.
Operative complications
According to the heterogeneity test results, it can be concluded that statistical heterogeneity was not significant between the eleven studies (p = 0.307, I2 = 14.4%), we adopted fixed-effect model for calculation. The data revealed that operative complications was less in RATS group. [OR = 0.31, 95% Cl: (0.18, 0.51), p = 0.000] (Figure 6).
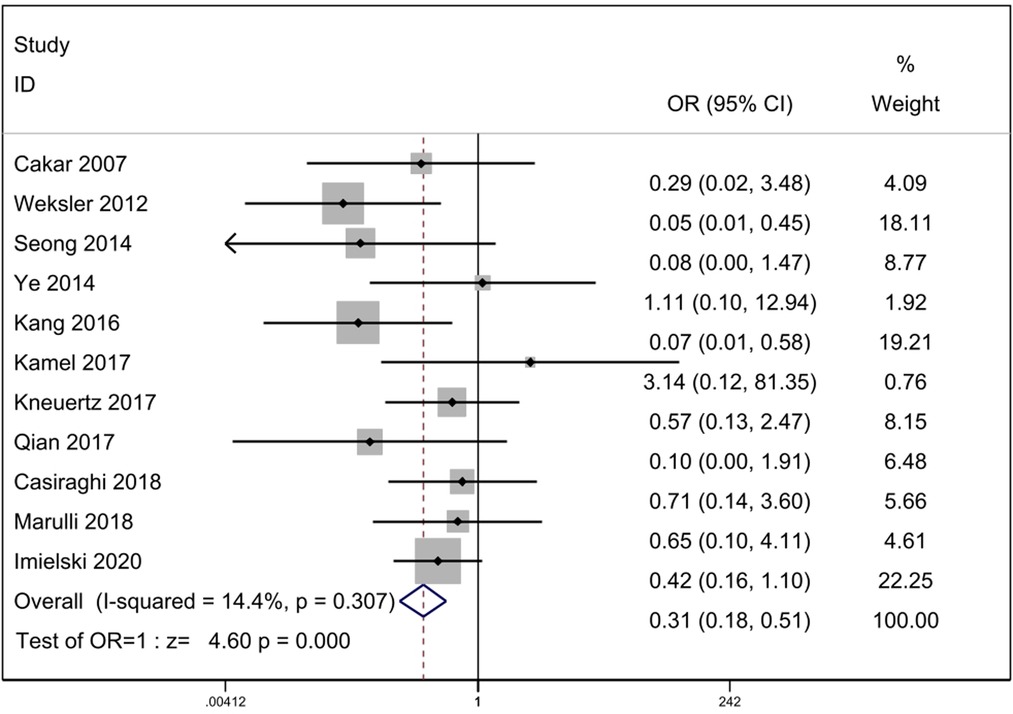
Figure 6. Comparison of operative complications between RATS and ST. OR, odds ratio; CI, confidence interval; RATS, robot-assisted thoracoscopic surgery; ST, sternotomy.
Hospitalization time
Fourteen studies with complete data compared hospitalization time. Statistical heterogeneity was significant (p = 0.000, I2 = 91.3%). We used the random-effect model for calculation. The result indicated that hospitalization time was less in the RATS group [SMD = −1.62, 95% Cl: (−2.16, −1.07), p = 0.000]. There were twelve studies reported total hospitalization time and two studies reported postoperative hospitalization time. We performed subgroup analysis and found that total hospitalization time was less in the RATS group [SMD = −1.37, 95% Cl: (−1.85, −0.88), p = 0.000], but postoperative hospitalization time was similar in two groups [SMD = −3.07, 95% Cl: (−7.36, 1.21), p = 0.160] (Figure 7).
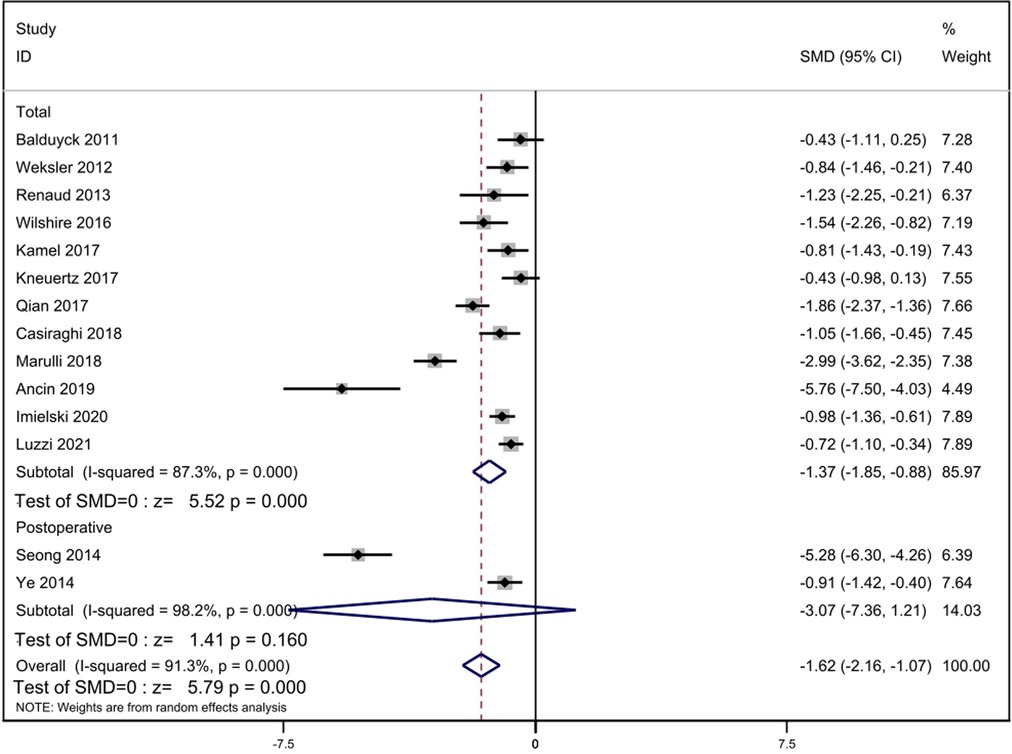
Figure 7. Comparison of hospitalization time between RATS and ST. SMD, standardized mean difference; CI, confidence interval; RATS, robot-assisted thoracoscopic surgery; ST, sternotomy.
Assessment of publication bias
The Begg's test (z = 1.29, Pr > |z| = 0.198) and the Egger's test (t = 1.15, p > |t| = 0.273) revealed that publication bias did not exist in these included studies, and the results of this meta analysis are stable (Figure 8).

Figure 8. Assessment of publication bias. Begg's test and Egger's test did not imply a publication bias.
Discussion
The best surgical method of thymectomy has always been a controversial issue. So far, sternotomy has been regarded as the first choice for thymectomy, especially for thymoma. Surgeons can expose the entire mediastinum in this way to get the best surgical field of vision. In the era of rapid development of artificial intelligence, the introduction of robotic surgery system has brought a valuable choice to doctors. The daVinci robot has all the advantages of minimally invasive surgery. It provides a clearer, three-dimensional 3D field of vision than video-assisted thoracoscopy, reduces the impact of surgeons' hand tremors, and makes the movement of instruments more accurate (21, 23). Many original studies have explored robot-assisted thymectomy for the treatment of thymic diseases, some scholars have studied the surgical results of patients after robotic surgery and sternotomy. Therefore, a meta-analysis was performed to confirm the advantages of robot-assisted thoracoscopic surgery for thymectomy.
From our meta-analysis, it can be concluded that compared with ST, RATS thymectomy has obvious advantages, including less operative blood loss, less drainage time, less postoperative complications and less hospitalization time. The comparison of operation time was not significant.
Our meta-analysis revealed that the significant difference did not exist in operation time between RATS and ST. For surgeons, robotic-assisted surgery has a learning curve, so the operation time may be affected by the surgeons' technology. With the improvement of the surgeons' surgical technology, the operation time will be reduced (11, 24). The comparison results of operation time had significant heterogeneity (I2 = 92.3%). Based on the sensitivity analysis, we conducted that the studies of Ye (12), Renaud (10) and Seong (11) caused the heterogeneity. After reviewing the full texts carefully, there was no significant difference between these three studies and the other fifteen studies. We eliminated the three studies, the heterogeneity decreased slightly (I2 = 73.6%). We speculate that although the general surgical procedures are roughly the same, there are great differences in surgical skills among different institutions, resulting in temporal heterogeneity. Of course, it is also possible that the definition of operation time is different in different studies. some studies define the startup of the robot system as the start time, some count the operation time according to the anesthesia time, and some choose the skin-to-skin time. These may help us to understand the heterogeneity of this result.
From the results of our meta-analysis, operation blood loss of RATS group was less compared with ST group (p = 0.000). We speculate that during the operation, the robot can provide surgeons with clearer three-dimensional images, and its flexible operating arm can avoid hand tremors, help doctors more effectively separate the complex anatomical structures of the chest and accurately expose the thymus, and help surgeons perform accurate operations (25). We observed significant heterogeneity of intraoperative blood loss (I2 = 93.4%), and our sensitivity analysis showed that the study of Ye (12) was most likely to lead to heterogeneity. After excluding the study, the heterogeneity decreased (I2 = 78.5%).
With regard to the postoperative drainage time, the result of heterogeneity test is significant (I2 = 94.2%). The sensitivity analysis was performed and suggested that the heterogeneity was caused by three studies by Seong (11), Ye (12) and Kneuertz (15). We eliminated the studies, the heterogeneity disappeared (I2 = 0%). After reviewing the full texts carefully, We found no significant difference between these three studies and the other six studies. Therefore, we speculated that there are differences in the indicators of removing drainage tube in different institutions, which may explain the heterogeneity of postoperative drainage time. Our analysis suggested that the postoperative drainage time of RATS was less compared with ST (p = 0.000).
Operative complications are related to the recovery of patients. Our meta analysis indicated that for thymectomy, robotic surgery had a lower incidence of operative complications than sternotomy. This result is due to the fact that robotic surgery provides a clear field of vision and precise manipulation, which can reduce tissue damage and reduce complications including postoperative pain and infection.
As for hospitalization time, the analysis suggested that hospitalization time of patients in RATS group was shorter. The result is observably attributed to the minimally invasive characteristics of robot-assisted surgery, which can avoid tissue injury, reduce intraoperative blood loss, shorten the time of pleural drainage days and accelerate the postoperative recovery of patients. The heterogeneity of hospitalization time was significant (I2 = 91.3%). Through the sensitivity analysis, we can conclude that the heterogeneity was mainly caused by the studies of Seong (11), Marulli (17) and Ancin (18). Heterogeneity decreased after the elimination of the two studies (I2 = 56.2%).
Shen et al. (26) and Wu et al. (27) compared the effects of RATS and VATS thymectomy by meta-analysis. They all came to a similar conclusion: RATS has more advantages over VATS, including reducing operation blood loss, postoperative drainage time, postoperative drainage volume, hospitalization time, and postoperative complications. It can be concluded that compared with ST and VATS, RATS is a more suitable surgical method for thymectomy.
The operation field of traditional video-assisted thoracoscopy is two-dimensional, and the field is not clear enough. The robot surgery operating system adds a new dimension, and its camera system can achieve a 10-fold magnification of the surgical field of vision, which helps surgeons to observe complex and small structures in more detail. The flexibility of the robot system is significantly higher than that of traditional surgical instruments, and its surgical arm can flexibly perform complex three-dimensional operations, overcoming some technical and methodological limitations. During thymectomy, the clear, flexible and stable characteristics of the robot system can ensure the structural integrity of blood vessels and nerves which are often damaged (28, 29).
What we need to admit is that our meta-analysis has some limitations. First of all, the studies we searched and included are cohort studies. There is no randomized controlled trial concerning the clinical difference between RATS and ST in databases at present. We will focus on randomized controlled trials in the future so that we can update this meta-analysis.
Conclusion
According to this meta-analysis of cohort studies, it can be concluded that RATS has more advantages over ST, including reducing operation blood loss, postoperative drainage time, incidence of operative complications and hospitalization time. Therefore, robot-assisted thoracoscopic surgery is a more appropriate surgical option for thymectomy.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author contributions
Conception: WW and C-qW. Collection of data: C-qW, JW, F-yL. Data analysis and interpretation: C-qW, JW, F-yL. Manuscript writing and revising: C-qW, F-yL, WW. Final approval of manuscript: C-qW, JW, F-yL, WW. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Engels EA, Pfeiffer RM. Malignant thymoma in the United States: demographic patterns in incidence and associations with subsequent malignancies. Int J Cancer. (2003) 105(4):546–51. doi: 10.1002/ijc.11099
2. Kang CH, Hwang Y, Lee HJ, Park IK, Kim YT. Robotic thymectomy in anterior mediastinal mass: propensity score matching study with transsternal thymectomy. Ann Thorac Surg. (2016) 102(3):895–901. doi: 10.1016/j.athoracsur.2016.03.084
3. Liu TJ, Lin MW, Hsieh MS, Kao MW, Chen KC, Chang CC, et al. Video-assisted thoracoscopic surgical thymectomy to treat early thymoma: a comparison with the conventional transsternal approach. Ann Surg Oncol. (2014) 21(1):322–8. doi: 10.1245/s10434-013-3228-7
4. Chao YK, Liu YH, Hsieh MJ, Wu YC, Chen TP, Lu MS, et al. Long-term outcomes after thoracoscopic resection of stage I and II thymoma: a propensity-matched study. Ann Surg Oncol. (2015) 22(4):1371–6. doi: 10.1245/s10434-014-4068-9
5. Xie A, Tjahjono R, Phan K, Yan TD. Video-assisted thoracoscopic surgery versus open thymectomy for thymoma: a systematic review. Ann Cardiothorac Surg. (2015) 4(6):495–508. doi: 10.3978/j.issn.2225-319X.2015.08.01
6. Casiraghi M, Galetta D, Borri A, Tessitore A, Romano R, Brambilla D, et al. Robotic-assisted thymectomy for early-stage thymoma: a propensity-score matched analysis. J Robot Surg. (2018) 12(4):719–24. doi: 10.1007/s11701-018-0816-3
7. Cakar F, Werner P, Augustin F, Schmid T, Wolf-Magele A, Sieb M, et al. A comparison of outcomes after robotic open extended thymectomy for myasthenia gravis. Eur J Cardiothorac Surg. (2007) 31(3):501–5. doi: 10.1016/j.ejcts.2006.12.016
8. Balduyck B, Hendriks JM, Lauwers P, Mercelis R, Ten Broecke P, Van Schil P. Quality of life after anterior mediastinal mass resection: a prospective study comparing open with robotic-assisted thoracoscopic resection. Eur J Cardiothorac Surg. (2011) 39(4):543–8. doi: 10.1016/j.ejcts.2010.08.009
9. Weksler B, Tavares J, Newhook TE, Greenleaf CE, Diehl JT. Robot-assisted thymectomy is superior to transsternal thymectomy. Surg Endosc. (2012) 26(1):261–6. doi: 10.1007/s00464-011-1879-7
10. Renaud S, Santelmo N, Renaud M, Fleury MC, De Seze J, Tranchant C, et al. Robotic-assisted thymectomy with Da Vinci II versus sternotomy in the surgical treatment of non-thymomatous myasthenia gravis: early results. Rev Neurol. (2013) 169(1):30–6. doi: 10.1016/j.neurol.2012.02.013
11. Seong YW, Kang CH, Choi JW, Kim HS, Jeon JH, Park IK, et al. Early clinical outcomes of robot-assisted surgery for anterior mediastinal mass: its superiority over a conventional sternotomy approach evaluated by propensity score matching. Eur J Cardiothorac Surg. (2014) 45(3):e68–73. doi: 10.1093/ejcts/ezt557
12. Ye B, Li W, Ge XX, Feng J, Ji CY, Cheng M, et al. Surgical treatment of early-stage thymomas: robot-assisted thoracoscopic surgery versus transsternal thymectomy. Surg Endosc. (2014) 28(1):122–6. doi: 10.1007/s00464-013-3137-7
13. Wilshire CL, Vallières E, Shultz D, Aye RW, Farivar AS, Louie BE. Robotic resection of 3 cm and larger thymomas is associated with low perioperative morbidity and mortality. Innovations. (2016) 11(5):321–6. doi: 10.1097/IMI.0000000000000295
14. Kamel MK, Rahouma M, Stiles BM, Nasar A, Altorki NK, Port JL. Robotic thymectomy: learning curve and associated perioperative outcomes. J Laparoendosc Adv Surg Tech A. (2017) 27(7):685–90. doi: 10.1089/lap.2016.0553
15. Kneuertz PJ, Kamel MK, Stiles BM, Lee BE, Rahouma M, Nasar A, et al. Robotic thymectomy is feasible for large thymomas: a propensity-matched comparison. Ann Thorac Surg. (2017) 104(5):1673–8. doi: 10.1016/j.athoracsur.2017.05.074
16. Qian L, Chen X, Huang J, Lin H, Mao F, Zhao X, et al. A comparison of three approaches for the treatment of early-stage thymomas: robot-assisted thoracic surgery, video-assisted thoracic surgery, and median sternotomy. J Thorac Dis. (2017) 9(7):1997–2005. doi: 10.21037/jtd.2017.06.09
17. Marulli G, Comacchio GM, Schiavon M, Rebusso A, Mammana M, Zampieri D, et al. Comparing robotic and trans-sternal thymectomy for early-stage thymoma: a propensity score-matching study. Eur J Cardiothorac Surg. (2018) 54(3):579–84. doi: 10.1093/ejcts/ezy075
18. Kamel MK, Rahouma M, Stiles BM, Nasar A, Altorki NK, Port JL Comparison of early postoperative results of robotic and transsternal thymectomies. Turk Thorac J. (2019) 20(1):40. doi: 10.5152/TurkThoracJ.2019.40
19. Imielski B, Kurihara C, Manerikar A, Chaudhary S, Kosterski S, Odell D, et al. Comparative effectiveness and cost-efficiency of surgical approaches for thymectomy. Surgery. (2020) 168(4):737–42. doi: 10.1016/j.surg.2020.04.037
20. Luzzi L, Corzani R, Ghisalberti M, Meniconi F, De Leonibus L, Molinaro F, et al. Robotic surgery vs. open surgery for thymectomy, a retrospective case-match study. J Robot Surg. (2021) 15(3):375–9. doi: 10.1007/s11701-020-01109-z
21. Kaba E, Cosgun T, Ayalp K, Toker A. Robotic thymectomy for myasthenia gravis. Ann Cardiothorac Surg. (2019) 8(2):288–91. doi: 10.21037/acs.2019.02.02
22. Herron DM, Marohn M. SAGES-MIRA robotic surgery consensus group. A consensus document on robotic surgery. Surg Endosc. (2008) 22(2):313–25. doi: 10.1007/s00464-007-9727-5
23. Kent M, Wang T, Whyte R, Curran T, Flores R, Gangadharan S. Open, video-assisted thoracic surgery, and robotic lobectomy: review of a national database. Ann Thorac Surg. (2014) 97(1):236–44. doi: 10.1016/j.athoracsur.2013.07.117
24. Melfi F, Fanucchi O, Davini F, Viti A, Lucchi M, Ambrogi MC, et al. Ten-year experience of mediastinal robotic surgery in a single referral centre. Eur J Cardiothorac Surg. (2012) 41(4):847–51. doi: 10.1093/ejcts/ezr112
25. Kang CH, Na KJ, Song JW, Bae SY, Park S, Park IK, et al. The robotic thymectomy via the subxiphoid approach: technique and early outcomes. Eur J Cardiothorac Surg. (2020) 58(Suppl_1):i39–43. doi: 10.1093/ejcts/ezaa006
26. Shen C, Li J, Li J, Che G. Robot-assisted thoracic surgery versus video-assisted thoracic surgery for treatment of patients with thymoma: a systematic review and meta-analysis. Thorac Cancer. (2022) 13(2):151–61. doi: 10.1111/1759-7714.14234
27. Wu WJ, Zhang FY, Xiao Q, Li XK. Does robotic-assisted thymectomy have advantages over video-assisted thymectomy in short-term outcomes? A systematic view and meta-analysis. Interact Cardiovasc Thorac Surg. (2021) 33(3):385–94. doi: 10.1093/icvts/ivab109
28. Raza B, Dhamija A, Abbas G, Toker A. Robotic thymectomy for myasthenia gravis surgical techniques and outcomes. J Thorac Dis. (2021) 13(10):6187–94. doi: 10.21037/jtd-2019-rts-10
Keywords: robot-assisted thoracoscopic surgery, sternotomy, thymectomy, systematic review, meta-analysis
Citation: Wang C, Wang J, Liu F and Wang W (2023) Robot-assisted thoracoscopic surgery vs. sternotomy for thymectomy: A systematic review and meta-analysis. Front. Surg. 9:1048547. doi: 10.3389/fsurg.2022.1048547
Received: 19 September 2022; Accepted: 25 October 2022;
Published: 6 January 2023.
Edited by:
Calvin Sze Hang Ng, The Chinese University of Hong Kong, ChinaReviewed by:
Firas Abu Akar, Wolfson Medical Center, IsraelPiotr Yablonskii, St-Petersburg Research Institute of Phthisiopulmonology, Russia
Takashi Suda, Fujita Health University Okazaki Medical Center, Japan
© 2023 Wang, Wang, Liu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei Wang d2FuZ3dlaXR4enpAMTYzLmNvbQ==
Specialty Section: This article was submitted to Thoracic Surgery, a section of the journal Frontiers in Surgery
 Cheng-qian Wang1,2
Cheng-qian Wang1,2 Wei Wang
Wei Wang