
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Surg., 13 January 2023
Sec. Orthopedic Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.1047974
This article is part of the Research TopicAdvances in Research of Degenerative Orthopedic Conditions: from Basic to Clinical ResearchView all 32 articles
Background: Intradural lumbar disc herniation (ILDH), especially upper lumbar intradural disc herniation, is a rare type of lumbar disc herniation (LDH). However, it may have severe and complex symptoms, causing serious impact on the patients. Additionally, it is difficult to be diagnosed with limited experience. Few studies on L2–L3 ILDH have been reported in the literature. This study presents such a case and reviews the incidence, etiology, symptoms, diagnosis and treatment of this disease, so as to provide guidance and experience for clinicians.
Case presentation: A 27-year-old male patient had a one-month history of severe lower back pain and left lower extremity weakness after lumbar sprain. He could not walk due to progressive symptoms. Physical examination revealed that straight leg raising and femoral nerve stretch tests on the left side were positive. Magnetic resonance imaging of lumbar showed an intradural disc protruding into the ventral dural sac at the L2–L3 level. He was diagnosed ILDH of L2–L3, finally. An urgent operation was performed to remove the intradural disc fragment. The patient's symptoms improved significantly, postoperatively. After eight months of follow-up, he returned to normal life with only slight lower back pain.
Conclusions: ILDH at the L2–L3 level is an extremely rare type of LDH. Its diagnosis often requires a combination of symptom, physical examination, and imaging examination due to no typical symptoms or imaging features. A detailed preoperative plan including the definition of the position, calcification, migration, and adhesion of intradural intervertebral discs to decrease the risk of surgery, prevent the occurrence of complications, and promote postoperative prognosis of patients.
Intradural lumbar disc herniation (ILDH) is a rare type of lumbar disc herniation (LDH), and its incidence is 0.04–0.33% of LDH (1). ILDH occurs more rarely in the upper lumbar spine than the lower lumbar spine (1). The etiology of ILDH is still uncertain. The most widely accepted mechanism is adhesion between the posterior longitudinal ligament (PLL) and ventral dural sac. For ILDH, there are atypical and complex symptoms, such as low back pain, radiation pain, or lower extremity weakness. More seriously, ILDH may cause cauda equina syndrome (CES) (2). Prompt surgery is used in the treatment of ILDH, so as to alleviate severe symptoms, avoid aggravation of the condition, and prevent adverse events. ILDH may be misunderstood as intradural extramedullary tumor, hematomas, or synovial cyst based on preoperative radiographic imaging (3, 4). It is difficult to make definitive preoperative diagnosis, which increases the risk of surgery and reduces the prognosis. According to literature reports, there have been few studies on L2–L3 ILDH. The purpose of this study is to describe a case with L2–L3 ILDH, to review the incidence, etiology, symptoms, diagnosis and treatment of this disease, and to provide guidance and experience for orthopedic surgeons.
A 27-year-old male patient who suffered from severe lower back pain and left lower extremity pain due to lumbar sprain a month ago. The patient accepted some conservative treatments such as non-steroidal anti-inflammatory drugs and bed rest. However, the symptoms did not alleviate, or even worsened. He experienced the left lower extremity weakness, and then he could not walk due to progressive symptoms. No further treatment was adopted. The movement was limited, and the patient failed to take part in social activities or even look after himself. Therefore, the patient was admitted to our hospital for treatment. He denied having a similar medical history and a family history of genetic disorders. Physical examination revealed muscle weakness in the left lower extremity, especially left ankle dorsiflexion and great toe dorsiflexion. The left-side straight leg raising and femoral nerve stretch tests were positive. The bowel and bladder functions were normal. Lumbar computed tomography (CT) showed that intervertebral disc herniation, loss of disc height, and osteophyte hyperplasia at the L2–L3 level (Figures 1A,B). Lumbar magnetic resonance imaging (MRI) demonstrated that extruded intervertebral disc, loss of continuity of the PLL, and intradural masses at the L2–L3 level (Figures 1C–F). The masses with T1-weighted and T2-weighted signals equaled to those of intervertebral discs. ILDH was preoperative diagnosis on the basis of medical history, symptoms, physical examination, and radiographic findings. Its differential diagnosis, such as intradural tumor and cyst, still needs to be considered. A laminectomy was performed under general anesthesia. The dura sac in the spinal canal was exposed by removing the ligamentum flavum. Extruded intervertebral disc was not found in the extradural space, but there were tight adhesions between the PLL and the ventral dural sac. A durotomy of the dorsal dural sac was completed and the nerve rootlets were separated. There was a mass revealed disc-like substance in the dura sac (Figure 2). A defect of the ventral dural sac was observed after the mass was removed. The dorsal and ventral dural sacs were sutured continuously. Cerebrospinal fluid (CSF) leakage was not discovered, and there was no obvious compression of the nerve root and dural sac after careful inspection. Transforaminal lumbar interbody fusion and transpedicular screw fixation were performed to prevent the recurrence of ILDH and spinal instability. Subsequently, the incision was sutured and the drainage was placed. Antibiotics were injected intravenously for 3 days after the surgery. Postoperative radiographs revealed that the extruded intervertebral disc was removed and the position of internal fixation was good (Figure 3). The patient's pain improved significantly, postoperatively. The patient was followed up by outpatient review. Lower extremity weakness gradually improved, and no complications such as infection, cerebrospinal fluid leakage, or epidural hematoma were found during the follow-up period. Eight months postoperatively, the patient could return to normal life, walk freely, and participate in social activities with only slight lower back pain. Physical examination showed the muscle strength of the left lower extremity was significantly improved compared with that before surgery. The left-side straight leg raising and femoral nerve stretch tests were negative. The visual analogue scale score and the Oswestry disability index significantly improved from 7 and 72 preoperatively to 2 and 18, respectively. The patient was satisfied with the efficacy.
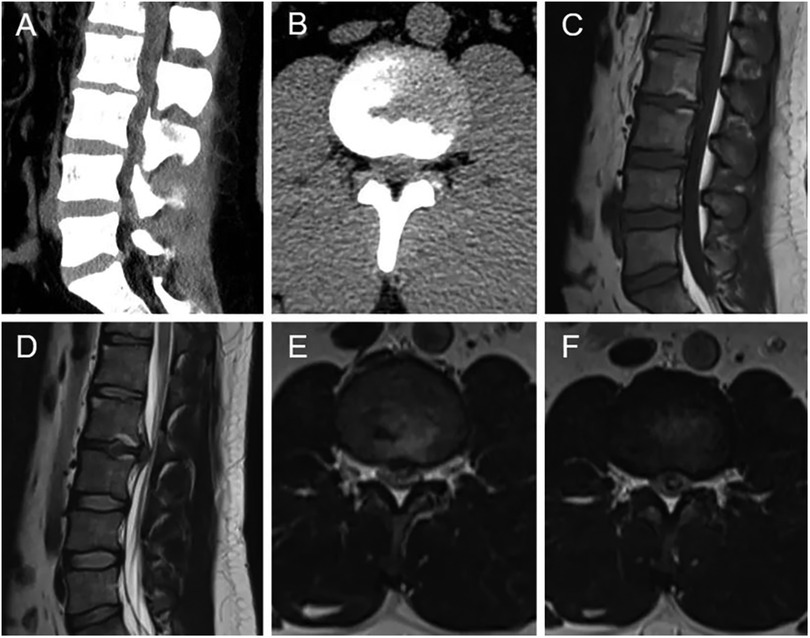
Figure 1. Preoperative radiographic images (A–F). (A,B) CT showed intervertebral disc herniation, loss of disc height, and osteophyte hyperplasia at the L2–L3 level. Sagittal T1-weighted (C) and T2-weighted (D) MRI revealed extruded intervertebral disc, and loss of continuity of the PLL at the L2–L3 level. (E,F) Axial T2-weighted MRI demonstrated the intradural mass.
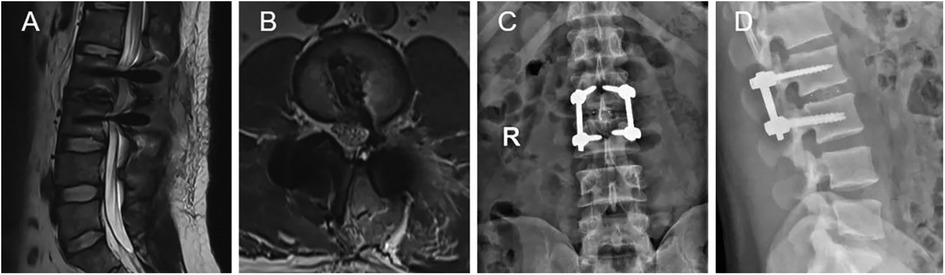
Figure 3. Postoperative radiographic images (A–D). (A,B) MRI revealed that the extruded lumbar intervertebral disc was removed. (C,D) Plain radiographs showed interbody fusion with posterior instrumentation.
ILDH was first described by Dandy in 1942 (5). ILDH is rare with an incidence of 0.04–0.33% of LDH, however, ILDH at the L2–L3 level is even rarer with an incidence of only 9.5% of all ILDH (1). To our knowledge, there are 21 patients with ILDH at L2–L3 level in the literature (Table 1). ILDH often occurs in patients over 50 years old, and it is more common in men than in women (1). We reported a male patient with ILDH at the L2–L3 level who was only 27 years old.
The etiology of ILDH remains uncertain. Adhesions of the PLL and the ventral dural sac may be a predisposing factor for ILDH and could occur in congenital conditions such as congenital lumbar spinal stenosis, or in chronic degenerative diseases (17, 26–28). The adhesion may cause dural erosion, followed by herniation of the intervertebral disc into the dural sac. D'Andrea et al. (16) found that 33.3% of ILDH patients had a history of previous surgery. Previous surgery may contribute to intradural disc herniation due to postoperative adhesions of the PLL and the ventral dural sac. Jang et al. (29) revealed that an acute trauma may lead to the occurrence of ILDH. The symptoms of ILDH are atypical and complex, including low back pain, radiation pain, or lower extremity weakness, which is more serious than epidural disc herniation. Moreover, the incidence of CES in ILDH is higher than extradural lumbar disc herniation (2).
The diagnosis of ILDH is still difficult and challenging. Some characteristics of imaging should be noticed to rule out some differential diagnoses. Hidalgo-Ovejero et al. (9) demonstrated that an intradural herniated disc was associated with the presence of epidural gas on CT scans and suggested that ILDH should be considered when epidural gas was observed. Sasaji et al. (10) reported that the “Y sign” formed by the ventral dura and arachnoid on sagittal T2-weighted MRI could contribute to the diagnosis of ILDH. Choi et al. (30) found that the “hawk-beak sign” on the axial imaging and loss of continuity of the PLL on T2-weighted sagittal MRI could indicate the occurrence of ILDH. Wasserstrom et al. (31) reported that ILDH was diagnosed by rim enhancement of herniated disc on gadolinium-enhanced MRI. Rim enhancement on gadolinium-enhanced MRI were used to rule out some differential diagnoses such as meningioma and schwannoma (32, 33). Note that rim enhancement of herniated disc occurred due to peripheral neovascularization and chronic granulation tissue (33). Myelography could be used to diagnose ILDH. Kataoka et al. (1) revealed that 71% and 15% of ILDH patients showed complete block and incomplete block in myelogram, respectively. However, myelography failed to rule out intradural tumors and huge central herniation (34, 35).
The optimal and effective treatment of ILDH is surgery that completely removes intradural intervertebral discs. Laminectomy is considered as the mainstream procedure and is widely used to treat ILDH. CSF leakage may be a serious complication. Pedaballe et al. (36) concluded that the defect of the ventral dura should be sutured. Some hemostatic materials should be placed on the ventral dural sac to prevent the occurrence of CSF leakage (37). A study by Serikyaku et al. (38) demonstrated that no postoperative CSF leakage was found in all patients of ventral durotomy without repair. The treatment of ventral dural defect remains controversial. Note that intradural migration of intradural disc fragment was easily misdiagnosed as intradural extramedullary tumor, and also increased the risk of surgical failure (22). Kobayashi et al. (15) reported that transforaminal lumbar interbody fusion was performed to treat ILDH, so as to prevent recurrence. Recently, Kim et al. (12) has been found that percutaneous endoscopic lumbar discectomy was successfully conducted in the treatment of ILDH. However, Moon et al. (11) reported the conversion to microscopic surgery after the failure of percutaneous endoscopic lumbar discectomy for treatment of ILDH.
There are some limitations to our study. First, pathological examination of extruded intervertebral disc was not performed. Second, the follow-up period of the patient was short. Third, only one case was analyzed in this study.
ILDH at the L2–L3 level is an extremely rare type of LDH. The etiology of ILDH is multifaceted. Its symptoms and preoperative radiological findings are often atypical. The diagnosis of ILDH is often based on the combination of symptom, physical examination, and imaging examination, and is confirmed during operation. Orthopedic surgeons should make detailed preoperative plans including the definition of the position, calcification, migration, and adhesion of intradural intervertebral discs to decrease the risk of surgery, prevent the occurrence of complications, and promote postoperative prognosis of patients.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by China-Japan Union Hospital of Jilin University. The patients/participants provided their written informed consent to participate in this study.
XC and HW: contributed to the conception and design of the study. XC: collected the clinical data and wrote the manuscript. YC: designed the figures and provided valuable comments. XC and HW: revised the manuscript. The final manuscript was approved by all authors. All authors contributed to the article and approved the submitted version.
This work was supported by a grant from the Science and Technology Development Plan of Jilin Province. (No. 20200404187YY).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ILDH, intradural lumbar disc herniation; LDH, lumbar disc herniation; PLL, posterior longitudinal ligament; CES, cauda equina syndrome; CSF, cerebrospinal fluid; CT, computed tomography; MRI, magnetic resonance imaging; CFS, cerebrospinal fluid.
1. Kataoka O, Nishibayashi Y, Sho T. Intradural lumbar disc herniation. Report of three cases with a review of the literature. Spine. (1989) 14(5):529–33. doi: 10.1097/00007632-198905000-00011
2. Singh PK, Shrivastava S, Dulani R, Banode P, Gupta S. Dorsal herniation of cauda equina due to sequestrated intradural disc. Asian Spine J. (2012) 6(2):145–7. doi: 10.4184/asj.2012.6.2.145
3. Aydin MV, Ozel S, Sen O, Erdogan B, Yildirim T. Intradural disc mimicking: a spinal tumor lesion. Spinal Cord. (2004) 42(1):52–4. doi: 10.1038/sj.sc.3101476
4. Montalvo Afonso A, Mateo Sierra O, Gil de Sagredo Del Corral OL, Vargas Lopez AJ, Gonzalez-Quarante LH, Sola Vendrell E, et al. Misdiagnosis of posterior sequestered lumbar disc herniation: report of three cases and review of the literature. Spinal Cord Ser Cases. (2018) 4:61. doi: 10.1038/s41394-018-0100-9
5. Dandy WE. Serious complications of ruptured intervertebral disks. JAMA. (1942) 119:474–7. doi: 10.1001/jama.1942.02830230008002
6. Cantini R, Ravelli V. Intradural lumbar disc hernia. Case report. Ital J Orthop Traumatol. (1986) 12(2):267–70.3793465
7. Lee G, Han MS, Lee SK, Moon B, Lee JK. Traumatic intradural ruptured lumbar disc with a spinal compression fracture: a case report. Medicine. (2020) 99(7):e19037. doi: 10.1097/MD.0000000000019037
8. Crivelli L, Dunet V. Intradural lumbar disc herniation detected by 3D CISS MRI. BMJ Case Rep. (2017) 2017:bcr2017221728. doi: 10.1136/bcr-2017-221728
9. Hidalgo-Ovejero AM, Garcia-Mata S, Gozzi-Vallejo S, Izco-Cabezon T, Martinez-Morentin J, Martinez-Grande M. Intradural disc herniation and epidural gas: something more than a casual association? Spine. (2004) 29(20):E463–7. doi: 10.1097/01.brs.0000142433.21912.0d
10. Sasaji T, Horaguchi K, Yamada N, Iwai K. The specific sagittal magnetic resonance imaging of intradural extra-arachnoid lumbar disc herniation. Case Rep Med. (2012) 2012:383451. doi: 10.1155/2012/383451
11. Moon SJ, Han MS, Lee GJ, Lee SK, Moon BJ, Lee JK. Unexpected intradural lumbar disk herniation found during transforaminal endoscopic surgery. World Neurosurg. (2020) 134:540–3. doi: 10.1016/j.wneu.2019.11.121
12. Kim HS, Pradhan RL, Adsul N, Jang JS, Jang IT, Oh SH. Transforaminal endoscopic excision of intradural lumbar disk herniation and dural repair. World Neurosurg. (2018) 119:163–7. doi: 10.1016/j.wneu.2018.07.244
13. Karabekir HS, Guzey FK, Atar EK, Yildizhan A. Intraradicular lumbar disc herniation: report of two cases. Spinal Cord. (2006) 44(5):318–21. doi: 10.1038/sj.sc.3101860
14. Koc RK, Akdemir H, Oktem IS, Menku A. Intradural lumbar disc herniation: report of two cases. Neurosurg Rev. (2001) 24(1):44–7. doi: 10.1007/pl00011967
15. Kobayashi K, Imagama S, Matsubara Y, Yoshihara H, Hirano K, Ito Z, et al. Intradural disc herniation: radiographic findings and surgical results with a literature review. Clin Neurol Neurosurg. (2014) 125:47–51. doi: 10.1016/j.clineuro.2014.06.033
16. D'Andrea G, Trillo G, Roperto R, Celli P, Orlando ER, Ferrante L. Intradural lumbar disc herniations: the role of MRI in preoperative diagnosis and review of the literature. Neurosurg Rev. (2004) 27(2):75–80. doi: 10.1007/s10143-003-0296-3
17. Han I-H, Kim K-S, Jin B-H. Intradural lumbar disc herniations associated with epidural adhesion: report of two cases. J Korean Neurosurg Soc. (2009) 46(2):168–71. doi: 10.3340/jkns.2009.46.2.168
18. Daffner SD, Sedney CL, Rosen CL. Migratory intradural disk herniation and a strategy for intraoperative localization. Global Spine J. (2015) 5(1):55–8. doi: 10.1055/s-0034-1381728
19. Whittaker CK, Bernhardt M. Magnetic resonance imaging shows gadolinium enhancement of intradural herniated disc. Spine. (1994) 19(13):1505–7. doi: 10.1097/00007632-199407000-00016
20. Hida K, Iwasaki Y, Abe H, Shimazaki M, Matsuzaki T. Magnetic resonance imaging of intradural lumbar disc herniation. J Clin Neurosci. (1999) 6(4):345–7. doi: 10.1054/jocn.1997.0072
21. Sakai T, Tsuji T, Asazuma T, Yato Y, Matsubara O, Nemoto K. Spontaneous resorption in recurrent intradural lumbar disc herniation. Case report. J Neurosurg Spine. (2007) 6(6):574–8. doi: 10.3171/spi.2007.6.6.11
22. Kim H-S, Eun J-P, Park J-S. Intradural migration of a sequestrated lumbar disc fragment masquerading as a spinal intradural tumor. J Korean Neurosurg Soc. (2012) 52(2):156–8. doi: 10.3340/jkns.2012.52.2.156
23. Tempel Z, Zhu X, McDowell MM, Agarwal N, Monaco EA 3rd. Severe intradural lumbar disc herniation with cranially oriented free fragment migration. World Neurosurg. (2016) 92:582.e1–e4. doi: 10.1016/j.wneu.2016.06.024
24. Chen J, Ni H-J, Xue F, Fan Y-S, Li X-F, Chen X-Z, et al. Upper lumbar intradural disc herniation: a rare case report and etiologic analysis. J Pain Res. (2021) 14:1475–81. doi: 10.2147/JPR.S297304
25. Pholprajug P, Wiratapesuporn T, Satayasoontorn K, Atiprayoon S, Kotheeranurak V. Intradural disc herniation of L2/3: a case report and literature review. N Am Spine Soc J. (2022) 11:100138. doi: 10.1016/j.xnsj.2022.100138
26. Ghaffari-Rafi A, Nosova K, Kim K, Goodarzi A. Intradural disc herniation in the setting of congenital lumbar spinal stenosis. Neurochirurgie. (2022) 68(3):335–41. doi: 10.1016/j.neuchi.2021.04.006
27. Yildizhan A, Pasaoglu A, Okten T, Ekinci N, Aycan K, Aral O. Intradural disc herniations pathogenesis, clinical picture, diagnosis and treatment. Acta Neurochir. (1991) 110(3-4):160–5. doi: 10.1007/BF01400685
28. Floeth F, Herdmann J. Chronic dura erosion and intradural lumbar disc herniation: CT and MR imaging and intraoperative photographs of a transdural sequestrectomy. Eur Spine J. (2012) 21 Suppl 4(Suppl 4):S453–7. doi: 10.1007/s00586-011-2073-2
29. Jang J-W, Lee J-K, Seo B-R, Kim S-H. Traumatic lumbar intradural disc rupture associated with an adjacent spinal compression fracture. Spine. (2010) 35(15):E726–9. doi: 10.1097/BRS.0b013e3181c64ca7
30. Choi JY, Lee WS, Sung KH. Intradural lumbar disc herniation–is it predictable preoperatively? A report of two cases. Spine J. (2007) 7(1):111–7. doi: 10.1016/j.spinee.2006.02.025
31. Wasserstrom R, Mamourian AC, Black JF, Lehman RA. Intradural lumbar disk fragment with ring enhancement on MR. AJNR Am J Neuroradiol. (1993) 14(2):401–4.8456719
32. Liu CC, Huang CT, Lin CM, Liu KN. Intradural disc herniation at L5 level mimicking an intradural spinal tumor. Eur Spine J. (2011) 20 Suppl 2(Suppl 2):S326–9. doi: 10.1007/s00586-011-1772-z
33. Jain SK, Sundar IV, Sharma V, Goel RS, Gupta R. Intradural disc herniation—a case report. Turk Neurosurg. (2013) 23(3):389–91. doi: 10.5137/1019-5149.JTN.5437-11.1
34. Arnold PM, Wakwaya YT. Intradural disk herniation at L1–L2: report of two cases. J Spinal Cord Med. (2011) 34(3):312–4. doi: 10.1179/2045772311Y.0000000007
35. Holtas S, Nordstrom CH, Larsson EM, Pettersson H. MR Imaging of intradural disk herniation. J Comput Assist Tomogr. (1987) 11(2):353–6. doi: 10.1097/00004728-198703000-00034
36. Pedaballe AR, Mallepally AR, Tandon V, Sharma A, Chhabra HS. An unusual case of transdural herniation of a lumbar intervertebral disc: diagnostic and surgical challenges. World Neurosurg. (2019) 128:385–9. doi: 10.1016/j.wneu.2019.05.103
37. Ducati LG, Silva MV, Brandao MM, Romero FR, Zanini MA. Intradural lumbar disc herniation: report of five cases with literature review. Eur Spine J. (2013) 22:S404–8. doi: 10.1007/s00586-012-2516-4
Keywords: lumbar disc herniation, intradural lumbar disc herniation, lower back pain, lower extremity weakness, case report
Citation: Chen X, Cheng Y and Wu H (2023) Intradural lumbar disc herniation of L2–L3: A case report and literature review. Front. Surg. 9:1047974. doi: 10.3389/fsurg.2022.1047974
Received: 19 September 2022; Accepted: 23 December 2022;
Published: 13 January 2023.
Edited by:
Fang Fang Yu, Zhengzhou University, ChinaReviewed by:
Jiaxing Lv, Kaifeng Central Hospital, China© 2023 Chen, Cheng and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Han Wu d3VfaGFuQGpsdS5lZHUuY24=
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.