- 1Department of Anesthesiology, Fuwai Hospital, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China
- 2Department of Anesthesiology, Shunde Hospital of South Medical University, Foshan, China
- 3Department of Anesthesiology, Fujian Medical University Affiliated First Quanzhou Hospital, Quanzhou, China
- 4Department of Anesthesiology, Fuwai Yunnan Cardiovascular Hospital, Kunming, China
- 5Department of Cardiovascular Surgery, Fujian Medical University Union Hospital, Fuzhou, China
Objectives: To summarize the anesthetic management of patients undergoing mediastinal mass operation.
Methods: Electronic databases were searched to identify all case reports of patients undergoing mediastinal mass operation. Information such as clinical characteristics, perioperative management and patients’ outcomes were abstracted and analyzed.
Results: Seventy-seven case reports with 85 patients aging from 34 days to 81 years were included. Mediastinal masses were located in anterior (n = 48), superior (n = 15), middle (n = 9) and posterior (n = 9) mediastinum, respectively. Clinical manifestations included dyspnea (n = 45), cough (n = 29), chest or radiating pain (n = 12), swelling (n = 8), fever (n = 7) and chest distress (n = 4). Most patients (n = 75) had signs of compression or invasion of vital structures. General anesthesia (n = 76) was the most commonly used method of anesthesia. Muscle relaxants were administered in 35 patients during anesthesia induction and spontaneous respiration was maintained in 37 patients. Mediastinal mass syndrome (MMS) occurred in 39 cases. Extracorporeal circulation was utilized in 20 patients intraoperatively. Three patients experienced cardiac arrest after ventilation failure and two patients died intraoperatively and one postoperatively.
Conclusions: Peri-operative management of patients undergoing mediastinal mass operation could be challenging. Pre-operative multi-disciplinary discussion, well-planned anesthetic management and pre-determined protocols for emergency situations are all vital to patient safety.
Introduction
Peri-operative management of patients undergoing mediastinal mass operation could be challenging. Mediastinal mass syndrome (MMS), initially described by Bittar in the 1970 s, is caused by a mediastinal mass, which can quickly deteriorate to acute respiratory and hemodynamic decompensation and is associated with increased morbidity and mortality (1, 2). Therefore, thorough pre-operative assessment, meticulous intra-operative management and multi-disciplinary collaboration are essential when managing patients undergoing mediastinal masses operation (3). Due to absence of guidelines, we performed a literature review of relevant published case reports, to summarize the clinical characteristics, anesthetic management and outcomes of patients undergoing mediastinal mass operation.
Materials and methods
Search strategy
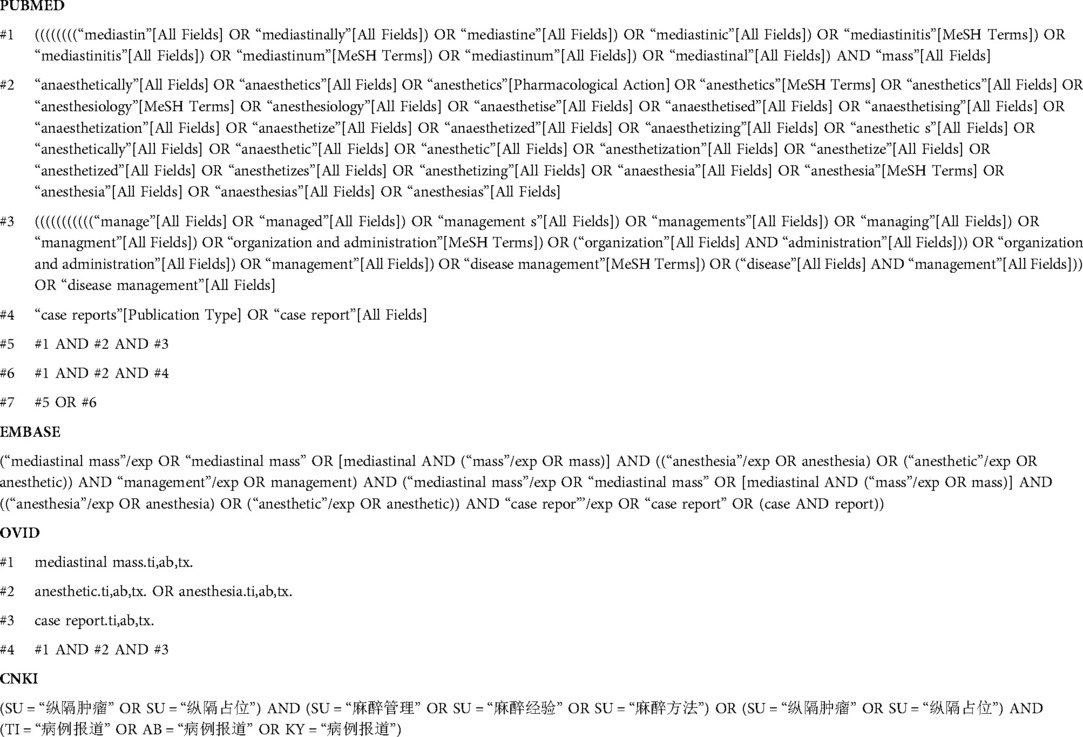
Relevant case reports were identified through computerized searches of PubMed, Embase and Ovid databases until May 15th, 2020, using different combinations of search terms “mediastinal mass”, “anesthesia” and “case” (Appendix). Chinese database CNKI was also searched (from the inception to May 15th, 2020). Databases search was updated on August 12th, 2020. Two authors (J.C.T. and P.S.L.) independently reviewed the titles and abstracts of all identified reports for eligibility, with obviously ineligible ones excluded. The eligibility of those remaining reports for final inclusion was determined further by examining the full text. Exclusion criteria included the following: (1) review articles, (2) animal studies, (3) duplicate publications, (4) studies lacking outcomes of interest.
Data abstraction
The following data from the included case reports were abstracted to a data collection form by two authors (J.C.T. and P.S.L.) independently: (1) literature information (author and year of publication); (2) patients characteristics (age, sex); (3) mediastinal mass features (location, size, pathology) and clinical manifestations (symptoms, signs and examination findings); (4) perioperative management (anesthesia techniques, extracorporeal circulation preparation) and (5) patients' outcomes. Disagreements were resolved by discussion among all authors during the process of data abstraction.
Results
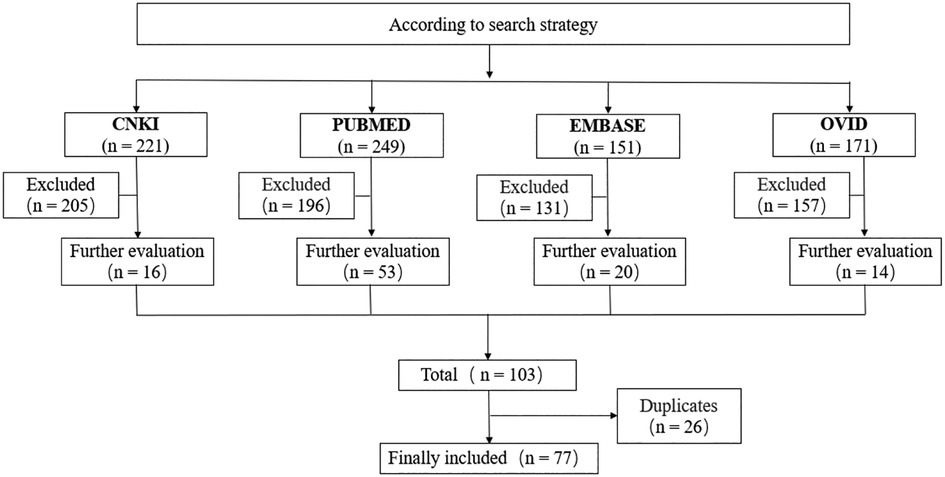
As depicted in the flow chart (Figure 1), the database search identified 103 potentially qualified articles. Seventy-seven case reports (85 patients in total) were determined eligible and included, 66 of which were written in English and the other 11 in Chinese. Descriptive analyses of these cases were presented in Table 1 (4–80).
The 85 patients aged between 34 days and 81 years, of whom 42 were males and 39 females (4 cases did not describe sex). Forty-eight (59.3%) cases of masses were located in anterior mediastinum, 15 (28.5%) in superior mediastinum, 9 (11.1%) in middle mediastinum and 9 (11.1%) in posterior mediastinum. The mass sizes ranged from 35mm × 44mm × 42 mm to 200mm × 200mm × 180 mm. Anterior mediastinum masses were usually bigger than those of other origins. Lymphoma (28/85, 32.9%) was the most common pathological type, followed by teratoma or seminoma (9/85, 10.5%). Of the 85 patients, 45 (59.2%) presented with dyspnea, 29 (38.1%) with cough, 12 (15.8%) with chest or radiating pain, 8 (10.5%) with swelling, 7 (9.2%) with fever, 4 (5.2%) with chest distress and 6 (7.8%) patients were asymptomatic. Seventy-five cases had signs of compression or invasion of trachea (60/85, 70.6%), bronchia (55/85, 64.7%), superior vena cava (43/85, 50.6%) and heart (26/85, 30.6%). Examination such as Computed tomography (CT), transthoracic echocardiogram (TTE), pulmonary function testing (PFT) and magnetic resonance imaging (MRI) were performed in 84 (97.4%), 24 (28.2%), 10 (11.8%), and 5 (5.9%) patients, respectively. Fifty-one (60.0%) patients underwent open thoracotomy, 28 (32.9%) patients underwent video-assisted thoracoscopic surgery (VATS) and 6 (7.1%) patients underwent other surgery. Fifty-seven (67.1%) patients had mass resection, 27(31.8%) patients received mass biopsy and 1(1.1%) case did not report surgical procedure.
Seventy-six (89.4%) patients were operated under general anesthesia (GA), 8 (9.4%) patients under sedation and 1 (1.2%) patient under local anesthesia. Fentanyl (n = 23), midazolam (n = 21), propofol (n = 19), ketamine (n = 15) and sevoflurane (n = 12) were most frequently used agents, followed by dexmedetomidine (n = 6), halothane (n = 5), remifentanil (n = 4), etomidate (n = 3), nitrous oxide (n = 3), diazepam (n = 2) and isoflurane (n = 2). Muscle relaxants were reported to be administered in 35 of the 85 included patients during anesthesia induction and in 5 patients after sternotomy, respectively. Succinylcholine (9/20, 45%) was the most commonly used muscle relaxant before endotracheal intubation. As for airway management, 66 (77.6%) patients were intubated with single lumen tube (SLT) including 1 with bronchial blocker (BB), 5 (5.9%) with double lumen tube (DLT), 4 (4.7%) with laryngeal mask airway (LMA) and 9 (10.6%) patients were tubeless. Spontaneous respiration was maintained in 32 (37.6%) patients, including 23 with spontaneous ventilation (SV) and 9 with assisted ventilation (AV).
Thirty-nine (45.9%) included patients developed MMS, 2 (2.4%) cases occurred before anesthetic induction, 13 (15.3%) cases after non-paralytic (without muscle relaxant) endotracheal intubation, 3 (3.5%) cases after muscle relaxant administration, 10 (11.8%) cases during position change, 10 (11.8%) cases during mass dissection, 3 (3.5%) cases during post-anesthesia recovery, respectively. Extracorporeal circulation (ECC) technique was applied in 20 (23.5%) patients: 2 initiated before anesthesia induction and 18 just with ECC standby. Three patients underwent ECC support due to severe intraoperative cardiopulmonary collapse. One patient experienced severe oxygen desaturation as the airway collapsed after endotracheal intubation without muscle relaxant and the operation was finally cancelled (12). Three patients died: 2 patients died from cardiopulmonary arrest as a result of ventilation failure during the anesthesia induction (37, 80); 1 patient had cardiac arrest intraoperatively due to suddenly increased airway resistance which deteriorated to sustained ventilation failure. The patient died on postoperative day 10 (75).
Discussion
Anesthetic management of mediastinal mass operation could be complicated by MMS characterized by acute respiratory and hemodynamic decompensation, which is caused by mechanical compression of mediastinal structures (81). However, no relevant guidelines for management of patients undergoing mediastinal mass operation is currently available. In the present study, we summarized the clinical characteristics, anesthetic management and outcomes of 85 patients undergoing mediastinal mass operation.
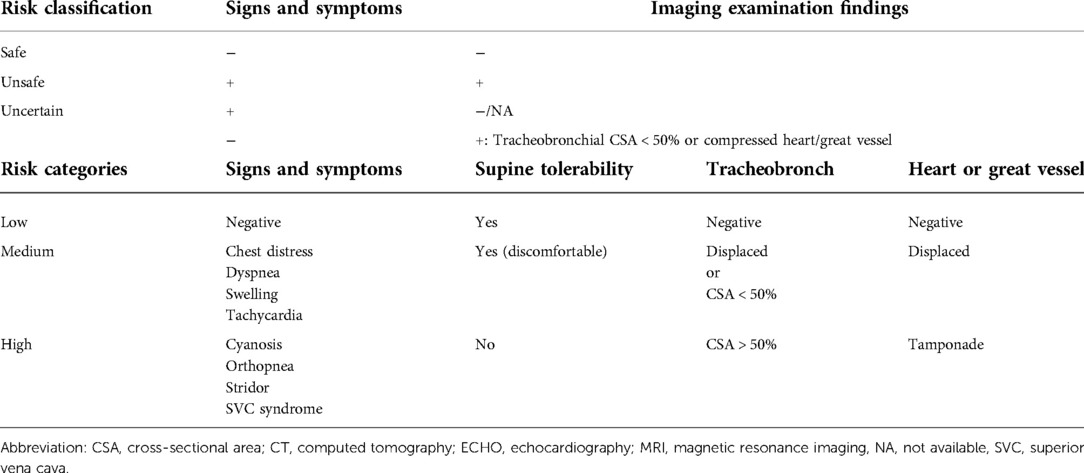
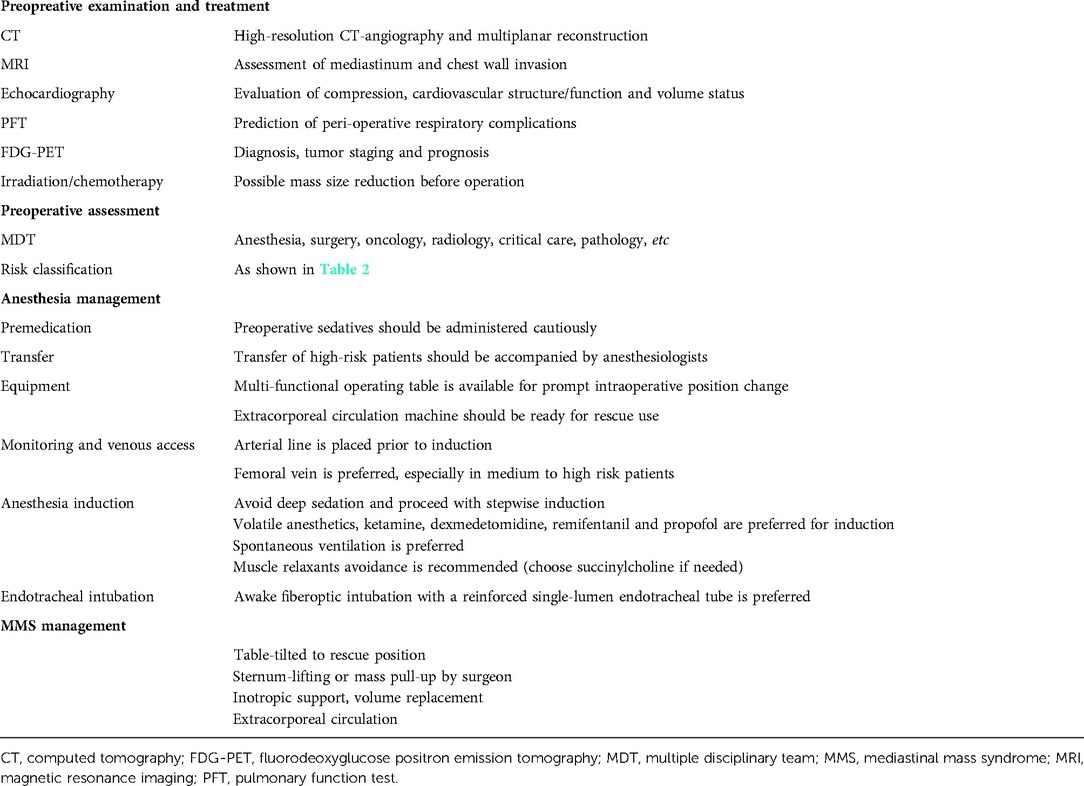
Comprehensive preoperative assessment is crucial in the management of patients with mediastinal mass (14, 39). Some risk stratifications have been proposed based on patients' preoperative signs and symptoms and the degree of major vessel or airway compression (2). CT scan, as an initial choice, provides anatomical details of masses and their relations with surrounding structures and helps in the creation of a deliberate plan for anesthetic and surgical management (28, 34). Compared with CT scan, MRI is more sensitive in soft tissue differentiation and delineating tissue boundaries. Echocardiography evaluates cardiac structural and functional alterations, which might influence anesthetic and surgical decision making (36). PFT, a tool to assess respiratory dysfunction and airway obstruction, may be of less value since there is conflicting evidence regarding the utility of PFT in risk stratification of mediastinal mass patients (7). By integrating the existing data of patients with mediastinal mass (2, 82, 83), we propose a classification to help categorize patients into three categories s of risk (Table 2). A detailed preoperative multidisciplinary team (MDT) discussion is of vital importance (14, 37).
Some authors (5, 7, 8, 12, 24, 35, 44, 49, 57) have outlined some suggestions for the anesthetic management of mediastinal mass patients undergoing surgery. For example, avoidance of general anesthesia (especially paralytic agents) or maintenance of SV has been recommended (35, 69). It is a consensus to proceed with stepwise induction and avoid deep sedation (37). It has been agreed that, no single agent is superior to another one, and that any agent should be used judiciously in consideration of retaining SV. Frawley et al. (74) reported a lower incidence of respiratory depression when ketamine was used alone or when combined with midazolam, provided the dose of the latter was kept low (0.1 mg/kg). Propofol can maintain spontaneous respiration when given slowly (40), even though when combined with remifentanil which may result in increased PaCO2 (83). Basem et al. (56) concluded that maintaining with dexmedetomidine (dose range of 0.2–0.7 µg/kg/h) could be very helpful and may reduce the risk of complete airway obstruction in the anesthetic management of mediastinal mass. Of the 85 patients, although 54(63.5%) did not receive muscle relaxant in induction, the rate of MMS was not lower than that of patients who received muscle relaxant. A retrospective study by Ng et al. (84) found that positive-pressure ventilation and intubation (though no muscle relaxation) was used in all cases that reported complications.
Virtually all reported cases of severe MMS occurred after abolition of SV (1). Dubey (11) suggested that maintaining SV until sternotomy is a safer approach. If a muscle relaxant is required, manually assisted ventilation should be done firstly, to assure that positive-pressure ventilation is possible and then a short-acting muscle relaxant can be administered (12, 24). However, the return of spontaneous breathing is not quick enough in critical situations (2). As a result, we advocate no muscle relaxant and maintenance of SV in anesthetic induction. Of note, maintenance of SV cannot assure airway patency during anesthesia. Gardner (48) considered that partial upper airway obstruction may generate sufficiently negative intraluminal pressure to collapse the compromised segment in the rapidly spontaneously breathing patient, which explains why the dynamic airway collapse and the inability to ventilate despite maintenance of SV.
Opinions about airway management in patients with MMS differed among authors. Kafrouni et al. (12) suggested that both lungs ventilation via a reinforced SLT was preferred. In the current study, more than 60% cases were intubated with SLT. Sulen (24) advised that for patients with airway obstruction, the safest option was to place a bronchial blocker (BB) or double lumen tracheal (DLT) tube when patients remained awake. Compared with conventional intubation method, extraluminal use of BB has more advantages (6). DLT intubation was suitable for low risk of airway compression (30). Since the increased availability of fiberoptic bronchoscopy (FOB) in many institutions, awake intubation guided by FOB has become another useful option for airway management in mediastinal masses patients (especially those with airway compression). In Rajagopalan (32) and Miyauchi's view (51), LMA or bi-level positive airway pressure (BiPAP) in sedation anesthesia can be used in patients with mediastinal mass that needs an incisional biopsy while maintaining SV. It is important to adhere to the general principles of maintaining effective ventilation and hemodynamic stability during induction and maintenance of anesthesia regardless of the technique used.
MMS can occur in every stage of perioperative period (2). Airway compression can occur in preoperatively asymptomatic adults with mediastinal mass (48). Acute respiratory decompensation may be precipitated by positional changes (8). Positioning change may help to relieve the mass effect of tumors (31, 37, 43, 46). It is vital to identify comfortable position in terms of respiration and hemodynamics in those symptomatic patients prior to surgery. The right lateral decubitus position can prevent MMS when the sitting position is not effective during general anesthesia (52). When intraoperative MMS does occur due to mass dissection, operation should be paused and compression be relieved immediately (81).
In high-risk patients classified as unsafe, decompensation after anesthesia induction should be expected and the option of connection to an extracorporeal circulation must always be provided (8, 52, 66). In the current study, ECC was prepared in 15 medium to high risk patients and 3 of them completed the operation with ECC when there was a severe cardiopulmonary failure intraoperatively. ECC were established before anesthesia induction and completed the operation successfully in 2 high risk patients. Three patients died of acute respiratory failure without ECC support and 1 patient's operation was canceled because of the cardiopulmonary system unsteadiness, also with an absence of ECC preparation. Tempe et al. (66) cannulated the femoral vessels and kept ECC ready because it was thought that there was a definite danger of the patient developing airway obstruction. Maria et al. (26) and Brandon (21) provided a successful example of ECC used in this context to assist with high-risk MMS patients with impending respiratory collapse. Recently, extracorporeal membrane oxygenation (ECMO) has become popular, which could be utilized as an easy form of ECC supporting circulatory and/or pulmonary functions in high-risk MMS patients.
Following surgery, patients in the unsafe risk category should be transferred to an intensive care unit (ICU). The extent of postoperative monitoring for patients in the uncertain risk category should be decided depending on preoperative findings and intraoperative course (2). It is worth noting that completion of the operation does not mean that the alert could have been lifted. Unexpectedly, 2 (28, 79) patients experienced MMS in recovery period. One had failed extubation and was transferred to ICU and the other one had tracheal compression with ventilation obstruction. The sitting position is preferable for resuscitation in the presence of an airway obstruction (52). By combining the above-mentioned practice and suggestions, a recommended management protocol (Table 3) and flowcharted (Figure 2) was formed for patients undergoing mediastinal mass operation.
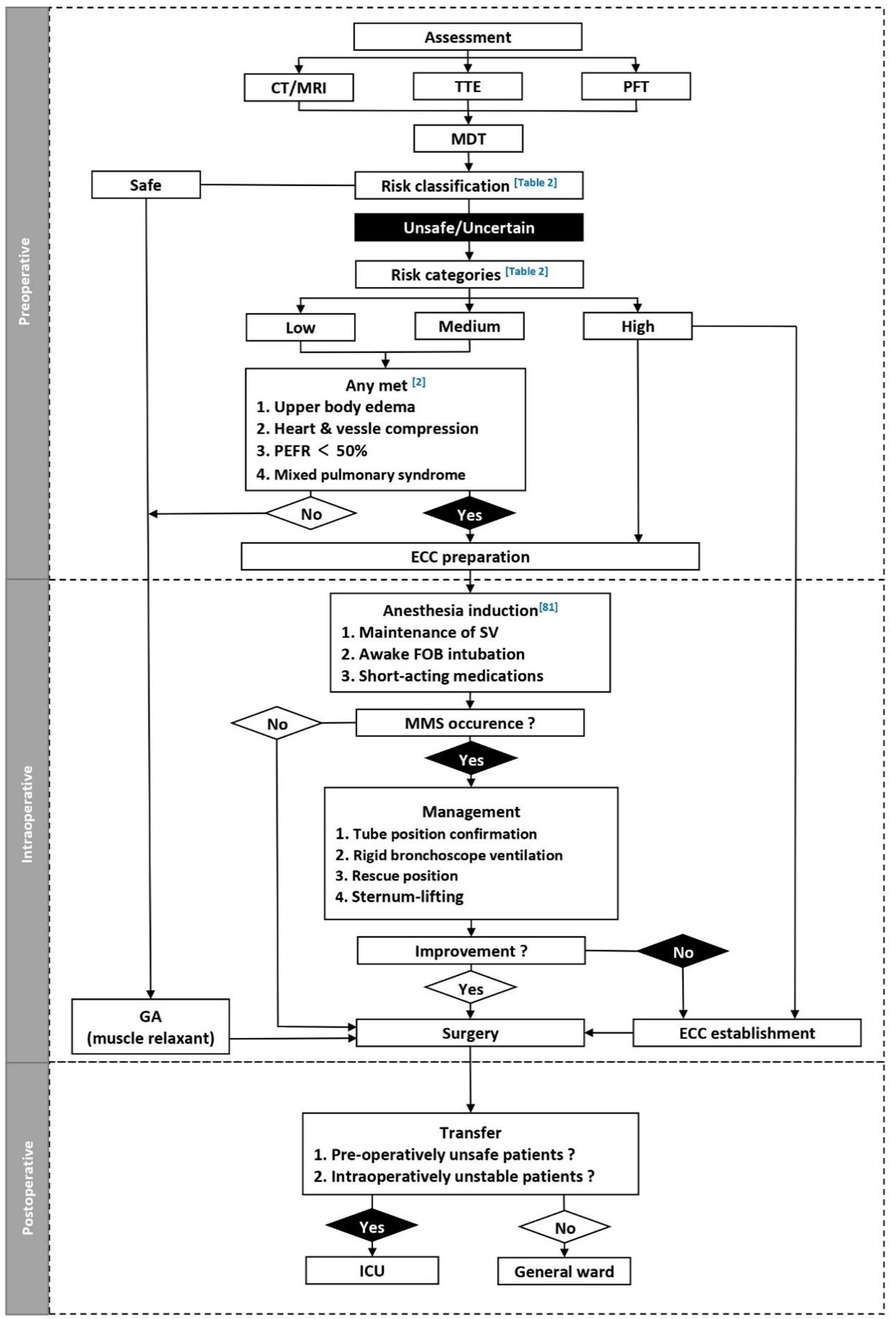
Figure 2. Perioperative management of patients with mediastinal mass. CT, computed tomography; ECC, extracorporeal circulation; FOB, fiber optic bronchoscope; GA, general anesthesia; ICU, Intensive care unit; MDT, multidisciplinary team; MMS, mediastinal mass syndrome; PEFR, peak expiratory flow rate; PFT, pulmonary function testing; SV, spontaneous ventilation; TTE, transthoracic echocardiogram.
Conclusions
To sum up, pre-operative multi-disciplinary discussion, well-planned anesthetic management and pre-determined protocols for emergency situations are all vital to patient safety.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author contributions
JcT: Methodology, Software, Data curation, Writing-original draft, Validation. PsL: Methodology, Writing-Validation. LxH: Methodology, Writing-Validation. YL: Methodology, Writing-Validation. YtY: Conceptualization, Methodology, Data curation, Writing—original draft, Validation. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bittar D. Respiratory obstruction associated with induction of general anesthesia in a patient with mediastinal Hodgkin's disease. Anesth Analg. (1975) 54:399–403. doi: 10.1213/00000539-197505000-00038
2. Erdos G, Tzanova I. Perioperative anaesthetic management of mediastinal mass in adults. Eur J Anaesthesiol. (2009) 26:627–32. doi: 10.1097/EJA.0b013e328324b7f8
3. Pearson JK, Tan GM. Pediatric anterior mediastinal mass: a review article. Semin Cardiothorac Vasc Anesth. (2015) 19:248. doi: 10.1177/1089253215578931
4. Yang Z, Shi Q, Bao F. A case of an unexpected posterior mediastinal functional paraganglioma: case report and literature review. BMC Anesthesiol. (2020) 20:109. doi: 10.1186/s12871-020-01026-6
5. Armas A, Primm AN. Anesthetic management of a patient with an anterior mediastinal mass undergoing endoscopic retrograde cholangiopancreatography in the prone position: a case report. A A Pract. (2020) 14:25–7. doi: 10.1213/XAA.0000000000001142
6. Liu Z, Jia Q, Yang X. Awake intubation and extraluminal use of uniblocker for one-lung ventilation in a patient with a large mediastinal mass a case report. BMC Anesthesiol. (2020) 20:125. doi: 10.1186/s12871-020-01041-7
7. Mohammad HG, Saman A, Arjang K. Anesthetic management of a patient with a giant pericardial cyst compressing the right atrium. Case Rep Anesthesiol. (2019) 2019:2320879. doi: 10.1155/2019/2320879
8. Jeong YI, Jun IG, Ha SS, Kwon HJ, Lee YM. Extracorporeal membrane oxygenation for the anesthetic management of a patient with a massive goiter causing severe tracheal obstruction with positional symptoms. Medicine. (2019) 98:e17650. doi: 10.1097/MD.0000000000017650
9. Diwan S, Patil S, Jadhav S, Nair AS. Comprehensive perioperative management of an infant with huge mediastinal mass. Saudi J Anaesth. (2019) 13:246–8. doi: 10.4103/sja.SJA_788_18
10. Dubey PK, Tripathi N. Anesthetic considerations in a patient with large anterior mediastinal mass. J Cardiothorac Vasc Anesth. (2019) 33:1073–5. doi: 10.1053/j.jvca.2018.03.023
11. Hartigan PM, Ju-Mei N, Gill RR. Anesthesia in a patient with a large mediastinal mass. N Engl J Med. (2018) 379:587–8. doi: 10.1056/NEJMc1804797
12. Kafrouni H, Saroufim J, Massih MA. Intraoperative tracheal obstruction management among patients with anterior mediastinal masses. Case Rep Med. (2018) 2018:4895263. doi: 10.1155/2018/4895263
13. Brenn BR, Reddy SK, Van Arendonk KJ, Morgan WM. Perioperative management of an anterior mediastinal teratoma in an infant: one more tool in the toolbox. BMJ Case Rep. (2018) 2018:bcr2018227022. doi: 10.1136/bcr-2018-227022
14. Liu X, Li XH, Zuo YX. Exacerbation of mediastinal tumor syndrome during general anesthesia for a large posterior mediastinal tumor in children: a case report. J Clin Anesthesiol. (2018) 34:1142–3. doi: 10.12089/jca.2018.11.026
15. Golmohammadi M, Salehi S, Haghi R, Radvar M. Anesthetic management of an infant presenting with an intrapericardial tumor: a case report. J Tehran Heart Cent. (2018) 13:76–9.30483317
16. Liu Z, Wang L, Yuan L. Anaesthesia management of mediastinal tumor with severe compression of trachea: a case report. J Clin Med. (2017) 4:15820. doi: 10.3877/j.issn.2095-8242.2017.80.145
17. Freed JK, Dyer AJ, Olund TJ, Veldheer DJ, Boettcher BT, Pagel PS. An unusual finding in a woman undergoing resection of a large anterior mediastinal mass. J Cardiothorac Vasc Anesth. (2018) 32:1090–2. doi: 10.1053/j.jvca.2017.03.037
18. Saipriya T, Puneet G, Amit R. Anesthetic challenges of extrinsic trachea-bronchial compression due to posterior mediastinal mass our experience with a large esophageal mucocele. Ann Card Anaesth. (2017) 20:359–61. doi: 10.4103/aca.ACA_194_16
19. Kusajima K, Ishihara S, Yokoyama T, Katayama K. Anesthetic management of cesarean section in a patient with a large anterior mediastinal mass: a case report. JA Clin Rep. (2017) 3:e1–4. doi: 10.1186/s40981-017-0098-1
20. Muñoz-Largacha JA, Glocker RJ, Moalem J, Singh MJ, Litle VR. Incidental posterior mediastinal paraganglioma: the safe approach to management, case report. Int J Surg Case Rep. (2017) 35:25–8. doi: 10.1016/j.ijscr.2017.03.040
21. Nokes BT, Vaszar L, Jahanyar J, Swanson KL. VV-ECMO-assisted high-risk endobronchial stenting as rescue for asphyxiating mediastinal mass. J Bronchology Interv Pulmonol. (2018) 25:144–7. doi: 10.1097/LBR.0000000000000435
22. Wang L, Wang H, Zhang HM, Han H. Anaesthesia management for giant thyroidectomy. World Latest Med Inf (Electronic Version). (2017) 17:190. doi: 10.3969/j.issn.1671-3141.2017.33.155
23. Ayşe ÇT, Pınar K, Güner K. Anaesthetic management of a child with a massive mediastinal mass. Turk J Anaesthesiol Reanim. (2017) 45:374–6. doi: 10.5152/TJAR.2017.81557
24. Sulen N, Petani B, Bacić I, Morović D. Anesthetic management of a patient with central airway compression due to posterior mediastinal mass. Acta Clin Croat. (2016) 55:103–7.27276782
25. Dudley M, Lipnick M. Multidisciplinary management of an adult with a mediastinal mass. Crit Care Med. (2016) 44:487. doi: 10.1097/01.ccm.0000510322.61298.fb
26. Maria E, Jeffrey M, Jae-O B, Fraser JD. Use of a sternal elevator to reverse complete airway obstruction secondary to anterior mediastinal mass in an anesthetized child. J Pediatr Surg Case Rep. (2016) 8:42–5. doi: 10.1016/j.epsc.2016.03.019
27. Wooles NR, Hoskison E, Elloy M. An unusual cause of stridor in an adult: mediastinal foregut duplication cyst. BMJ Case Rep. (2015) 2015:bcr2014208533. doi: 10.1136/bcr-2014-208533
28. Scheele B, Ascher K, Carolina DLC, Csete M. Prone positioning for cardiorespiratory collapse in an adult patient with anterior mediastinal mass after general anesthesia. Chest. (2015) 148:23A–B. doi: 10.1378/chest.2254405
29. Al-Mubarak G, Bryant AS, Crawford JH, Dukes CM, Kelly DR, Young DW, et al. Surgical and anesthetic management of a mediastinal fatty tumor: lipoblastoma. Ann Thorac Surg. (2015) 100:97–8. doi: 10.1016/j.athoracsur.2015.04.103
30. Lee J, Rim YC, In J. An anterior mediastinal mass: delayed airway compression and using a double lumen tube for airway patency. J Thorac Dis. (2014) 6:99–103. doi: 10.3978/j.issn.2072-1439.2014.04.30
31. Thakur P, Bhatia P, Sitalakshmi N, Virmani P. Anaesthesia for mediastinal mass. Indian J Anaesth. (2014) 58:215–7. doi: 10.4103/0019-5049.130840
32. Rajagopalan S, Harbott M, Ortiz J, Bandi V. Anesthetic management of a large mediastinal mass for tracheal stent placement. Braz J Anesthesiol. (2016) 66:215–8. doi: 10.1016/j.bjan.2014.01.009
33. Said SM, Telesz BJ, Makdisi G, Quevedo FJ, Suri RM, Allen MS, et al. Awake cardiopulmonary bypass to prevent hemodynamic collapse and loss of airway in a severely symptomatic patient with a mediastinal mass. Ann Thorac Surg. (2014) 98:87–90. doi: 10.1016/j.athoracsur.2014.06.104
34. Brain C. Cardiovascular collapse and hypoxemia in a man with a right-sided mediastinal mass, undiagnosed atrial septal defect, and right-to-left shunt. J Clin Anesth. (2014) 26:688–92. doi: 10.1016/j.jclinane.2014.05.011
35. Fabbro M, Patel PA, Ramakrishna H, Valentine E, Ochroch EA, Agoustides JG. Challenging perioperative management of a massive anterior mediastinal mass in a symptomatic adult. J Cardiothorac Vasc Anesth. (2014) 28:819–25. doi: 10.1053/j.jvca.2013.12.029
36. Ward EW, Sean MM. Novel use of a guidewire to facilitate intubation in an obstructing anterior mediastinal mass. Can J Anaesth. (2014) 61:660–3. doi: 10.1007/s12630-014-0163-4
37. Al-Sanouri I, Shaban M, Al-Shahid M, Abdulaziz S. A 21-year-old woman with mediastinal mass and cardiac arrest. BMJ Case Rep. (2013) 2013:bcr2013009020. doi: 10.1136/bcr-2013-009020
38. Sola C, Choquet O, Prodhomme O, Capdevila X, Dadure C. Management of mediastinal syndromes in pediatrics: a new challenge of ultrasound guidance to avoid high-risk general anesthesia. Paediatr Anaesth. (2014) 24:534–7. doi: 10.1111/pan.12300
39. Lalwani P, Chawla R, Kumar M, Tomar AS, Raman P. Posterior mediastinal mass: do we need to worry much? Ann Card Anaesth. (2013) 16:289–92. doi: 10.4103/0971-9784.119183
40. Rim SK, Son YB, Kim JI, Lee JH. Propofol and remifentanil total intravenous anesthesia and the preservation of spontaneous respiration for a patient with mediastinal mass. Korean J Anesthesiol. (2013) 65:583–4. doi: 10.4097/kjae.2013.65.6.583
41. Miyauchi Y, Matsubara H, Uchida T, Matsuoka H, Ichihara T, Matsumoto M. Successful thoracoscopic removal of a giant teratoma following extraction of cystic conponents: a case report. Asian J Endosc Surg. (2014) 7:79–81. doi: 10.1111/ases.12067
42. Han CB, Zhou QH, Gao M, et al. Mass resection of posterior mediastinal castleman disease in a patient with severe paraneoplastic pemphigoid: a case report. Chin J Anesthesiol. (2013) 33:1497–8. doi: 10.3760/cma.j.issn.0254-1416.2013.12.025
43. Peter CST, Esa N. Anesthesia for massive retrosternal goiter with severe intrathoracic tracheal narrowing: the challenges imposed -A case report. Korean J Anesthesiol. (2012) 62:474–8. doi: 10.4097/kjae.2012.62.5.474
44. Chaudhary K, Gupta A, Wadhawan S, Jain D, Bhadoria P. Anesthetic management of superior vena cava syndrome due to anterior mediastinal mass. J Anaesthesiol Clin Pharmacol. (2012) 28:242–6. doi: 10.4103/0970-9185.94910
45. Scott JP, Troshynski TJ, Clarke WR, Woods RK, Lal DR, Berens RJ, Tower RL. Case report: giant cardiac malignancy in a nine-year-old female. Can J Anaesth. (2012) 59:1048–51. doi: 10.1007/s12630-012-9780-y
46. Gautam PL, Kaur M, Singh RJ, Gupta S. Large mediastinal tumor in a neonate: an anesthetic challenge. J Anesth. (2012) 26:124–7. doi: 10.1007/s00540-011-1251-z
47. Yao WL, Dai JZ, Liao MF. Anaesthesia treatment of bilateral thorax and anterior mediastinal giant tumor resection: case report. Chin J Postgrad Med. (2012) 35:77–8. doi: 10.3760/cma.j.issn.1673-4904.2012.27.032
48. Gardner JC, Royster RL. Airway collapse with an anterior mediastinal mass despite spontaneous ventilation in an adult. Anesth Analg. (2011) 113:239–42. doi: 10.1213/ANE.0b013e31821f9c95
49. Shi D, Webb CA, Wagner M, Dizdarevic A. Anesthetic evaluation and perioperative management in a patient with new onset mediastinal mass syndrome presenting for emergency surgery. Case Rep Anesthesiol. (2011) 2011:782391. doi: 10.1155/2011/782391
50. Geniets B, van de Ven CP, Maat AP, Scohy TV. Intraoperative transesophageal echocardiography for mediastinal mass surgery improves anesthetic management in pediatric patients. Paediatr Anaesth. (2011) 21:1276–8. doi: 10.1111/j.1460-9592.2011.03681.x
51. Bassanezi BS, Oliveira-Filho AG, Miranda ML, Soares L, Aguiar SS. Use of BiPAP for safe anesthesia in a child with a large anterior mediastinal mass. Paediatr Anaesth. (2011) 21:985–7. doi: 10.1111/j.1460-9592.2011.03607.x
52. Choi WJ, Kim YH, Mok JM, Choi SI, Kim HS. Patient repositioning and the amelioration of airway obstruction by an anterior mediastinal tumor during general anesthesia -A case report-. Korean J Anesthesiol. (2010) 59:206–9. doi: 10.4097/kjae.2010.59.3.206
53. Chen MH. A case of anaesthesia management for giant nodular goiter. Beijing: China Academic Journal Electronic Publishing House (2010). 20:104 p.
54. Yang J. Anesthetic management of giant with mediastinal tumor resection in 4 case [C]. Beijing: China Academic Journal Electronic Publishing House (2009). 2:389–40 p.
55. Mourad OM, Andrade FM, Abrahão P, Monnerat A, Judice LF. Asymptomatic giant mediastinal mass: a rare case of thymolipoma. J Bras Pneumol. (2009) 35:1049–52. doi: 10.1590/S1806-37132009001000012
56. Abdelmalak B, Marcanthony N, Abdelmalak J, Machuzak MS, Gildea TR, Doyle DJ. Dexmedetomidine for anesthetic management of anterior mediastinal mass. J Anesth. (2010) 24:607–10. doi: 10.1007/s00540-010-0946-x
57. Wang G, Lin S, Yang L, Wang Z, Sun Z. Surgical management of tracheal compression caused by mediastinal goiter: is extracorporeal circulation requisite? J Thorac Dis. (2009) 1:48–50.22263003
58. Zhang DH, Xu J, Jin YW. Anesthesia experience in 2 patients with large mediastinal tumor. J ShanDong Med. (2007) 24:74. CNKI:SUN:SDYY.0.2007-24-063
59. Frey TK, Chopra A, Lin RJ, Levy RJ, Gruber P, Rheingold SR, Hoehn KS. A child with anterior mediastinal mass supported with veno-arterial extracorporeal membrane oxygenation. Pediatr Crit Care Med. (2006) 7:479–81. doi: 10.1097/01.PCC.0000235247.10880.F8
60. Gopp AR. Anesthetic management of a patient with a mediastinal foregut duplication cyst: a case report. AANA J. (2005) 73:55–61.15727285
61. Qu YQ. A case of severe traumatic diaphragmatic hernia in children under anesthesia. J YunNan Med. (2005) 4:397–8. CNKI:SUN:YNYY.0.2005-04-059
62. Cho Y, Suzuki S, Yokoi M, Shimada M, Kuwabara S, Murayama A. Lateral position prevents respiratory occlusion during surgical procedure under general anesthesia in the patient of huge anterior mediastinal lymphoblastic lymphoma. Jpn J Thorac Cardiovasc Surg. (2004) 52:476–9. doi: 10.1007/s11748-004-0144-6
63. Dilworth K, Jenny T. Anaesthetic consequences for a child with complex multilevel airway obstruction—recommendations for avoiding life-threatening sequelae. Paediatr Anaesth. (2003) 13:620–3. doi: 10.1046/j.1460-9592.2003.01011.x
64. Li FY, Yuan KS, Wang DH. 1 Case of congenital diaphragmatic hernia in infant: anesthesia experience. J Hebei Med. (2003) 04:265. CNKI:SUN:HBYZ.0.2003-04-020
65. Dilworth KE, McHugh K, Stacey S, Howard RF. Mediastinal mass obscured by a large pericardial effusion in a child: a potential cause of serious anaesthetic morbidity. Paediatr Anaesth. (2001) 11:479–82. doi: 10.1046/j.1460-9592.2001.00664.x
66. Tempe DK, Arya R, Dubey S, Khanna S, Tomar AS, Grover V, et al. Mediastinal mass resection: femorofemoral cardiopulmonary bypass before induction of anesthesia in the management of airway obstruction. J Cardiothorac Vasc Anesth. (2001) 15:233–6. doi: 10.1053/jcan.2001.21988
67. Shi PP, Wang HG. Anaesthesia management for resection of a large anterior mediastinal tumor:a case report. J FuJian Med. (2000) 1:132. doi: 10.3969/j.issn.1002-2600.2000.01.150
68. Vas L, Naregal F, Naik V. Anaesthetic management of an infant with anterior mediastinal mass. Paediatr Anaesth. (1999) 9:439–43. doi: 10.1046/j.1460-9592.1999.00413.x
69. Licker M, Schweizer A, Nicolet G, Hohn L, Spiliopoulos A. Anesthesia of a patient with an obstructing tracheal mass: a new way to manage the airway. Acta Anaesthesiol Scand. (1997) 41:84–6. doi: 10.1111/j.1399-6576.1997.tb04617.x
70. Goh MH, Liu XY, Goh YS. Anterior mediastinal masses: an anaesthetic challenge. Anaesthesia. (1999) 54:670–4. doi: 10.1046/j.1365-2044.1999.00961.x
71. Furst SR, Burrows PE, Holzman RS. General anesthesia in a child with a dynamic, vascular anterior mediastinal mass. Anesthesiology. (1996) 84:976–9. doi: 10.1097/00000542-199604000-00026
72. Polaner DM. The use of heliox and the laryngeal mask airway in a child with an anterior mediastinal mass. Anesth Analg. (1996) 82:208–10. doi: 10.1097/00000539-199601000-00037
73. Hattamer SJ, Dodds TM. Use of the laryngeal mask airway in managing a patient with a large anterior mediastinal mass: a case report. AANA J. (1996) 64:497–500.9124033
74. Frawley G, Low J, Brown TC. Anaesthesia for an anterior mediastinal mass with ketamine and midazolam infusion. Anaesth Intensive Care. (1995) 23:610–2. doi: 10.1177/0310057X9502300515
75. Viswanathan S, Campbell CE, Cork RC. Asymptomatic undetected mediastinal mass: a death during ambulatory anesthesia. J Clin Anesth. (1995) 7:151–5. doi: 10.1016/0952-8180(94)00028-3
76. Wang QD, Zhang YM, Dong HL. Anesthesia for resection of a giant mediastinal teratoma: a case report. J Fourth Milit Med Univ. (1995) 5:361.
77. Montange F, Truffa-Bachi J, Pichard E. Airway obstruction during anaesthesia in a child with a mediastinal mass. Can J Anaesth. (1990) 37:271–2. doi: 10.1007/BF03005493
78. John RE, Narang VP. A boy with an anterior mediastinal mass. Anaesthesia. (1988) 43:864–6. doi: 10.1111/j.1365-2044.1988.tb05601.x
79. Prakash UB, Abel MD, Hubmayr RD. Mediastinal mass and tracheal obstruction during general anesthesia. Mayo Clin Proc. (1988) 63:1004–11. doi: 10.1016/S0025-6196(12)64915-5
80. Neuman GG, Weingarten AE, Abramowitz RM, Kushins LG, Abramson AL, Ladner W. The anesthetic management of the patient with an anterior mediastinal mass. Anesthesiology. (1984) 60:144–7. doi: 10.1097/00000542-198402000-00012
81. Li WW, van Boven WJ, Annema JT, Eberl S, Klomp HM, de Mol BA. Management of large mediastinal masses: surgical and anesthesiological considerations. J Thorac Dis. (2016) 8:E175–84. doi: 10.21037/jtd.2016.02.55
82. Blank RS, Souza DG. Anesthetic management of patients with an anterior mediastinal mass: continuing professional development. Can J Anaesth. (2011) 58:853–67. doi: 10.1007/s12630-011-9539-x
83. Brenn RB, Hughes AK. The anesthetic management of anterior mediastinal masses in children: a review. Int Anesthesiol Clin. (2019) 57:e24–41. doi: 10.1097/AIA.0000000000000247
Keywords: mediastinal mass, anesthetic management, complications, risk stratificacion, airway management
Citation: Tan J-c, Lin P-s, He L-x, Lin Y, Yao Y-t and the Evidence in Cardiovascular Anesthesia(EICA) Group (2022) Anesthetic management of patients undergoing mediastinal mass operation. Front. Surg. 9:1033349. doi: 10.3389/fsurg.2022.1033349
Received: 31 August 2022; Accepted: 4 October 2022;
Published: 28 October 2022.
Edited by:
Shuben Li, First Affiliated Hospital of Guangzhou Medical University, ChinaReviewed by:
Sandeep Sainathan, University of Miami Health System, United StatesFilippo Tommaso Gallina, Regina Elena National Cancer Institute, Hospital Physiotherapy Institutes (IRCCS), Italy
© 2022 Tan, Lin, He, Lin and Yao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yun-tai Yao eXVudGFpeWFvQDEyNi5jb20=
Specialty Section: This article was submitted to Thoracic Surgery, a section of the journal Frontiers in Surgery
 Jie-chao Tan1,2
Jie-chao Tan1,2 Pei-shuang Lin
Pei-shuang Lin Yun-tai Yao
Yun-tai Yao