Introduction
The transverse cervical artery (transverse artery of the neck or transverse colli artery) is an artery in the neck and a branch of the thyrocervical trunk, running at a higher level than the suprascapular artery (1). It passes transversely above the inferior belly of the omohyoid muscle to the anterior margin of the trapezius, beneath which it divides into superficial and deep branches (2). The branches from the transverse cervical artery are widely distributed in the skin and soft tissue of the chest and shoulder, which are adjacent to the face and neck. Therefore, the branches of the transverse cervical artery are important donor vessels in the reconstruction of the face and neck. However, in recent years, the nomenclature of the flap near the clavicle supplied by the cutaneous branches of the transverse cervical artery has been controversial. Based upon our previous anatomical and clinical research, and after comparison with other nomenclatures, this article proposes a nomenclature based on the anatomy of the region. We believe that the flap near the clavicle supplied by the cutaneous branch of the transverse cervical artery should be referred to as the transverse cervical artery cervical cutaneous branch (TCACCB) flap.
Anatomical studies
The transverse cervical artery appears stable in anatomy, with a length ranging from 4.0 to 7.0 cm, and a mean diameter of 2.65 mm (1). The transverse cervical vein was present in 61 of 72 cadaveric specimens, with a length ranging from 4.0 to 7.0 cm, and a mean diameter of 2.90 mm (1). As early as the 1940 s, an anatomical atlas suggested that the superficial branch of the transverse cervical artery might supply blood to the skin near the clavicle (3). In 1979, Lamberty confirmed through anatomical and clinical research that the skin in the supraclavicular region was supplied by a stable cutaneous branch of the transverse cervical artery and that this skin could be made into an axial flap (3). He first referred to this flap as the “supra-clavicular axial patterned flap” (3). However, early anatomical studies only found the acromion branch among the cutaneous branches of the cervical segment of the transverse cervical artery, and research on the upper thoracic branch is limited.
Since 1988, we have performed detailed autopsies of the flap near the clavicle supplied by the cutaneous branch of the transverse cervical artery, and found that this branch at the cervical segment supplied blood to the skin in the anterior chest and supraclavicular regions (2). The transverse cervical artery travels outward to the deep side of sternocleidomastoid muscle and scapulohyoid muscle. The vessel then extends deep into the trapezius muscle and enters the dorsal segment of the back. The supraclavicular artery perforates the intersection of sternocleidomastoid muscle and scapulohyoid muscle. It then extends through the fat of the posterior cervical triangle of the neck and enters the subcutaneous layer of the supraclavicular region. Finally, it separates outward and downward into two branches. The first branch, the deltoid branch, extends into the acromial region. The thoracic branch extends into the anterior infraclavicular and thoracic regions (Schematic diagram of TCACCB flap was showed in Supplementary Figure S1) (4). In addition, according to the definition of perforator flap, we believe that the thoracic cutaneous branch of transverse cervical artery can be considered as a perforator vessel. The results of Chin et al. are similar to those of our research group. They found that the cutaneous branch of the transverse cervical artery emanates from the posterior cervical triangle and not only sends out perforating branches through the trapezius muscle to the skin above but also to the skin of the anterior chest (5).
Nomenclature
Consequent to more research on the flap near the clavicle supplied by the cutaneous branch of the transverse cervical artery in recent years, this flap has been increasingly used; however, there is still no consensus regarding the nomenclature used to refer to this flap, among different articles, as summarized in Table 1.
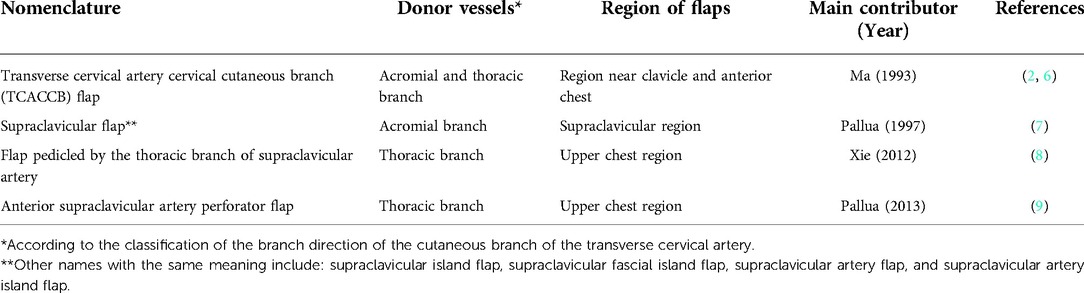
Table 1. Nomenclature for the flap near the clavicle supplied by the cutaneous branch of the transverse cervical artery.
Nutrient vessels to transverse cervical artery cervical cutaneous branch (TCACCB) flap are “the cutaneous branch of transverse cervical artery”. The TCACCB flap we propose includes the supraclavicular flap. The extent of the supraclavicular flap in the past was limited to the supraclavicular region (10). The TCACCB flap covers the region near the clavicle and anterior chest; therefore, the scope of the TCACCB flap is larger. The name of the TCACCB flap was first proposed by us, and compared to other names in the literature, not only was it proposed earlier, but it was also more consistent with the anatomic distribution of the blood vessels; therefore, it is a more rational name. Other reasons for proposing this nomenclature are as follows:
• The blood vessels are homologous. The supraclavicular and TCACCB flaps originate from the transverse cervical artery. Mizerny et al. found cutaneous branches of the transverse cervical artery supplying blood to the region near the clavicle by perfusing methylene blue into the transverse cervical artery (11).
• Due to the limitations of the study, the anterior thoracic branch was not dissected, which may be related to issues in the imaging method (12).
• Our study has proven that there are branches from the cervical segment of the transverse cervical artery to the shoulder and anterior chest, and anastomoses between the branches of the transverse cervical artery and the anterior perforating branch of the internal thoracic artery and the thoracoacromial artery have also been found (4).
• It has been proven in our clinical applications that the practical usable range of TCACCB flaps includes the region near the clavicle and anterior chest (13).
Discussion
The TCACCB flap can be used for the following clinical applications: (1) Neck scar or defect: The TCACCB flap, which is similar to the skin of the neck, can provide a large flap with a matching color and texture, yielding a good clinical effect after repairing neck scars or defects (14). If pre-expansion is performed, the flap area can be significantly increased, the flap becomes thinner, and the donor area does not require skin grafting for repair (15). (2) Chin defect: Choi et al. used the propeller TCACCB flap to repair a defect after resection of a mass in the chin (16). (3) Facial scar: Since the pedicle of the TCACCB flap is located closer to the face, the flap could be designed as an island flap to repair facial scars (17). (4) Oropharyngeal defects: Wang et al. used a TCACCB flap to repair oropharyngeal defects after resection of head and neck squamous cell carcinoma and obtained satisfactory repair results (18). Yang et al. also used this flap to repair a tracheal-laryngeal-hypopharynx defect after thyroidectomy with satisfactory results (19). (5) Since there is extensive anastomosis between the cutaneous branch of the cervical segment of the transverse cervical artery and the cutaneous branch of the thoracoacromial artery, as well as the second and third perforating branches of the internal thoracic artery, a trans-regional blood supply flap can be designed across regions with a single blood supply artery (20, 21).
For better clinical results, the TCACCB flap was combined with tissue expansion, such that the donor area was increased, and the flap was made thinner and more compatible with the recipient area (22–24). Xu et al. placed expanders of 300 or 350 ml in the anterior thoracic region and over-injected them 2–3 times. After expansion, a 20–25 × 7 cm–9 cm expanded TCACCB flap was obtained for the repair of facial scars, and the donor site could be directly sutured (25). Hou et al. expanded the usable area of the expanded TCACCB flap, using the expanded thoracic flap to repair the donor site, and obtained satisfactory curative effects in the repair of large-area facial and neck scars (26).
The advantages of the TCACCB flap include the following: (1) Rich blood supply: Because of the axial blood supply of this flap, the overall blood supply is good, and it can survive well even if there are superficial scars in the donor site. The flap is similar to the face and neck in color, texture, and thickness and has a good postoperative appearance, which is accepted by patients. (2) Convenient rotation: Since an island flap is formed, it could be rotated 90–180° without leaving a dog ear. (3) Ease of operation: Because of the clear structure of the soft tissues in the neck and chest, the flap can be separated under the deep fascia, making it easy to operate. (4) Good sensation: The flap contains the supraclavicular nerve; therefore, the flap retains sensation even after surgery (27).
Although we previously studied the anatomy and clinical application of the TCACCB flap in our department, the name of this flap has always been controversial (28). The absence of uniform names for this flap not only causes confusion in the recognition of the TCACCB flap by plastic surgeons, but also hinders wider applications of this flap. Therefore, we believe that the flap near the clavicle supplied by the cutaneous branch of the transverse cervical artery should be universally referred to as the TCACCB flap. This nomenclature will help the academic community reach a consensus on the naming of this flap, which will greatly promote its clinical application.
Author contributions
CD, conducting the study, writing the manuscript; YZ, concept of the study and editing the manuscript; XM, concept of the study and writing/editing the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.1029065/full#supplementary-material.
References
1. Tessler O, Gilardino MS, Bartow MJ, St Hilaire H, Womac D, Dionisopoulos T, et al. Transverse cervical artery: consistent anatomical landmarks and clinical experience with its use as a recipient artery in Complex head and neck reconstruction. Plast Reconstr Surg. (2017) 139:745e–51e. doi: 10.1097/PRS.0000000000003085
2. Ma X, Lu K, Ai Y. Microsurgical anatomy of the transverse cervical artery cervical cutaneous branch flap. Chin J of Clin Anat. (1994) 12:81–4. CNKI:SUN:ZLJZ.0.1994-02-000
3. Lamberty BG. The supra-clavicular axial patterned flap. Br J Plast Surg. (1979) 32:207–12. doi: 10.1016/s0007-1226(79)90033-x
4. Ma X, Zheng Y, Xia W, Fan X, Li Y, Guo S, et al. An anatomical study with clinical application of one branch of the supraclavicular artery. Clin Anat. (2009) 22:215–20. doi: 10.1002/ca.20742
5. Chin T, Ogawa R, Murakami M, Hyakusoku H. An anatomical study and clinical cases of “super-thin flaps” with transverse cervical perforator. Br J Plast Surg. (2005) 58:550–5. doi: 10.1016/j.bjps.2004.11.001
6. Ma X. The use of an axial flap with cutaneous branch of cervical segment of transverse cervical artery. Chin J Plast Surg Burns. (1993) 9:22–4. CNKI:SUN:ZHSA.0.1993-01-012
7. Pallua N, Machens HG, Rennekampff O, Becker M, Berger A. The fasciocutaneous supraclavicular artery island flap for releasing postburn mentosternal contractures. Plast Reconstr Surg. (1997) 99:1878–84. doi: 10.1097/00006534-199706000-00011
8. Xie F, Wang J, Li Q, Zhou S, Zan T, Gu B, et al. Resurfacing large skin defects of the face and neck with expanded subclavicular flaps pedicled by the thoracic branch of the supraclavicular artery. Burns. (2012) 38:924–30. doi: 10.1016/j.burns.2012.01.001
9. Pallua N, Wolter TP. Moving forwards: the anterior supraclavicular artery perforator (a-SAP) flap: a new pedicled or free perforator flap based on the anterior supraclavicular vessels. J Plast Reconstr Aesthet Surg. (2013) 66:489–96. doi: 10.1016/j.bjps.2012.11.013
10. Nthumba PM. The supraclavicular artery flap: a versatile flap for neck and orofacial reconstruction. J Oral Maxillofac Surg. (2012) 70:1997–2004. doi: 10.1016/j.joms.2011.08.043
11. Mizerny BR, Lessard ML, Black MJ. Transverse cervical artery fasciocutaneous free flap for head and neck reconstruction: initial anatomic and dye studies. Otolaryngol Head Neck Surg. (1995) 113:564–8. doi: 10.1177/019459989511300507
12. Vinh VQ, Van Anh T, Ogawa R, Hyakusoku H. Anatomical and clinical studies of the supraclavicular flap: analysis of 103 flaps used to reconstruct neck scar contractures. Plast Reconstr Surg. (2009) 123:1471–80. doi: 10.1097/PRS.0b013e3181a205ba
13. Ma X, Li Y, Wang L, Li W, Dong L, Xia W, et al. Reconstruction of cervical scar contracture using axial thoracic flap based on the thoracic branch of the supraclavicular artery. Ann Plast Surg. (2014) 73(Suppl 1):S53–6. doi: 10.1097/SAP.0000000000000257
14. Li G, Zhang Z, Li YY, Wang JL. Clinical effects of flaps with cervical cutaneous branch of transverse cervical artery in repairing neck radiation ulcers. Chin J Burns. (2021) 37:1116–21. doi: 10.3760/cma.j.cn501120-20200807-00371
15. Ma X, Li Y, Wang L, Li W, Dong L. Repair of cervical scar contracture with flaps containing cervical cutaneous branch of the transverse cervical artery. Chin J Burns. (2012) 28:256–9. doi: 10.3760/cma.j.issn.1009-2587.2012.04.005
16. Choi JY, Seo JH, Cha WJ, Seo BF, Jung SN. A propeller superficial transverse cervical artery perforator flap for defect coverage of the submental area: a case report. Arch Craniofac Surg. (2021) 22:341–4. doi: 10.7181/acfs.2021.00563
17. Wang X, Wang H. Nonexpanded prefabricated anterior perforator of transverse cervical artery flap for full facial reconstruction. J Craniofac Surg. (2019) 30:1206–7. doi: 10.1097/SCS.0000000000005061
18. Wang L, Ma CY, Shen Y, Fang J, Haugen TW, Guo B, et al. Transverse cervical artery anterior perforator flap for head and neck oncological reconstruction: preliminary study. Head Neck. (2021) 43:3598–607. doi: 10.1002/hed.26873
19. Yang L, Li W, Guan LP. Modified transverse cervical artery flap to repair the trachea-larynx-hypopharynx defect in advanced thyroid cancer: a case report. Chin J Otorhinolar Head Neck Surg. (2020) 55:263–5. doi: 10.3760/cma.j.issn.1673-0860.2020.03.014
20. Ma X, Lu K, Ai Y. Anatomy and clinical application of transcervicothoracic polyphyletic blood supply skin flap. Chin J Surg. (1995) 33:57–9. CNKI:SUN:ZHXW.0.1995-01-028 7774449
21. Song HF, Chai JK, Liu CM, Chi YF, Li DJ, Feng G, et al. Application of thoracic skin flap with multiple blood supply in repair of tissue defects and deformities in jaw and neck. Chin J Burns. (2009) 25:15–7. doi: 10.3760/cma.j.issn.1009-2587.2009.01.007
22. Song H, Chai J. Pre-expanded transverse cervical artery perforator flap. Clin Plast Surg. (2017) 44:41–7. doi: 10.1016/j.cps.2016.08.002
23. Ma X, Dong L, Li Y, Wang L, Li W. Clinical application of expanded flap based on the cutaneous branch of transverse cervical artery. Chin J Plast Surg. (2015) 31:165–7. doi: 10.3760/cma.j.issn.1009-4598.2015.03.002
24. Chen B, Song H, Xu M, Gao Q. Reconstruction of cica-contracture on the face and neck with skin flap and expanded skin flap pedicled by anterior branch of transverse cervical artery. J Craniomaxillofac Surg. (2016) 44:1280–6. doi: 10.1016/j.jcms.2016.04.020
25. Xu P, Wang S, Yan X, Lin Y, Ge H, Tan Q. Reconstruction of postburn facial scar contracture deformity with expanded flap containing cervical cutaneous branch of transverse cervical artery. Chin J Burns. (2016) 32:458–62. doi: 10.3760/cma.j.issn.1009-2587.2016.08.004
26. Hou J, Song HF, Chen BG, Xu MH, Gao QW, Wang J, et al. Clinical effects of pre-expanded anterior perforator flap of transverse cervical artery and pre-expanded thoracic random flap in reconstructing extensive facial and cervical scar in relay. Chin J Burns. (2021) 37:350–5. doi: 10.3760/cma.j.cn501120-20201023-00445
27. Ma X, Lu K, Ai Y. Clinical application of the transverse cervical artery cervical cutaneous branch island flap. Chin J Microsurg. (1995) 18:54–5. CNKI:SUN:ZHXW.0.1995-01-028
Keywords: transverse cervical artery, cutaneous branch, flap, anatomy, nomenclature
Citation: Dong C, Yu Z and Ma X (2023) The transverse cervical artery cervical cutaneous branch flap: An anatomy-based nomenclature. Front. Surg. 9:1029065. doi: 10.3389/fsurg.2022.1029065
Received: 26 August 2022; Accepted: 26 October 2022;
Published: 6 January 2023.
Edited by:
Biao Cheng, General Hospital of Southern Theater Command of PLA, ChinaReviewed by:
Lingli Guo, People's Liberation Army General Hospital, ChinaXiaohong Chen, Capital Medical University, China
© 2023 Dong, Yu and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xianjie Ma bWFqaW5nQGZtbXUuZWR1LmNu
Specialty Section: This article was submitted to Reconstructive and Plastic Surgery, a section of the journal Frontiers in Surgery
 Chen Dong
Chen Dong Zhou Yu
Zhou Yu Xianjie Ma*
Xianjie Ma*