- 1Department of Urology Surgery, Kunming Children's Hospital, Kunming, China
- 2Yunnan Key Laboratory of Children's Major Disease Research, Yunnan Province Clinical Research Center for Children's Health and Disease, Kunming, China
Aim: To explore the treatment experience of the duplex kidney.
Method: A case of the complete bilateral duplex kidney with severe hydronephrosis and ureterectasis in the upper moiety of the kidney diagnosed in the Department of Urology of Kunming Children's Hospital from 2021 to 2022 was retrospectively analyzed and relevant literature was reviewed.
Results: A 2-month-old baby girl was admitted to the hospital because of hydronephrosis of bilateral kidneys found by prenatal ultrasound for 3 months and fever for 3 days. After being given the relevant examinations, the girl was diagnosed with complete bilateral duplex kidneys with severe hydronephrosis and ureterectasis in the upper moiety, and urinary tract infection. The patient's urinary tract infection was poorly controlled after positive anti-infective therapy, so a bilateral ureterostomy was performed. After the surgery, urinary tract infection was soon cured. A bilateral ureteroureterostomy was performed 13 months later, and the patient recovered after 7 days.
Conclusion: Cutaneous ureterostomy combined with late ureteroureterostomy for children with complete bilateral duplex kidneys with severe hydronephrosis in the upper moiety and ureter are not only beneficial to caregivers’ nursing after the operation, but also have significance for salvaging renal function.
Background
Duplex kidney is a common disease in pediatric urology. There are many controversies due to the children's deformities and treatment methods are diverse and complicated (1). We report a case of severe hydronephrosis and ureterectasis in the upper moiety of bilateral duplex kidney with ectopic ureter on the left side and ureterocele on the right side, and summarize the characteristics of the disease for improving the understanding of pediatricians of the disease.
Clinical material
Patient information
The patient's parents informed and agreed to this case report: A 2-month-old baby girl was admitted to the hospital because of hydronephrosis of bilateral kidneys found by prenatal ultrasound for 3 months and had a fever for 3 days. The child was found to have bilateral hydronephrosis in her mother's late pregnancy, and ultrasound was not regularly performed after birth. The child had a fever for 3 days without an obvious cause, and the highest temperature was 39°C. After treatment in a local hospital, the child still had a recurrent high fever. After being referred to Kunming Children's Hospital, the child was given relevant examinations.
Physical examination
No positive signs were found.
Laboratory examination
Urine test revealed white blood cell: +++, white blood cell enzyme (+), nitrite (+). Urine culture: Escherichia coli.
Imaging examination
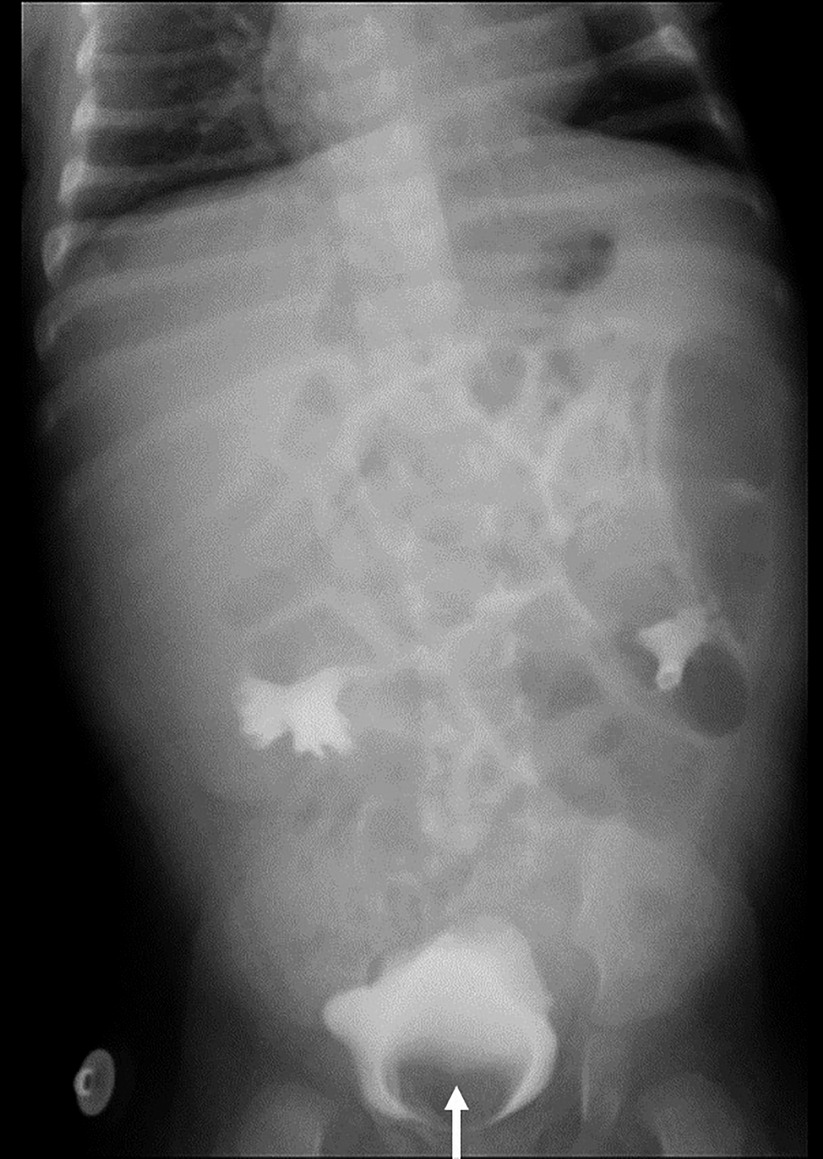
Ultrasound of urinary system showed bilateral duplex kidney (Figure 1). Severe hydronephrosis and ureterectasis were found in the bilateral upper moiety. Intravenous pyelography (IVP) showed there was an ureterocele in the bladder (Figure 2). Computerized tomography (CT) revealed severe hydronephrosis and ureterectasis of bilateral upper moiety, left ureteral opening was ectopic in location, and the right ureterocele was found (Figure 3).
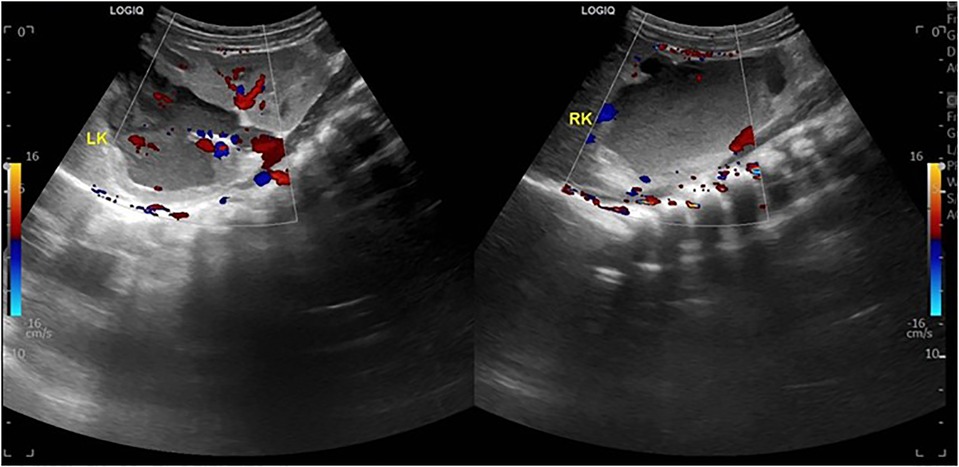
Figure 1. Preoperative ultrasound showed severe hydronephrosis and ureterectasis of bilateral upper moiety.
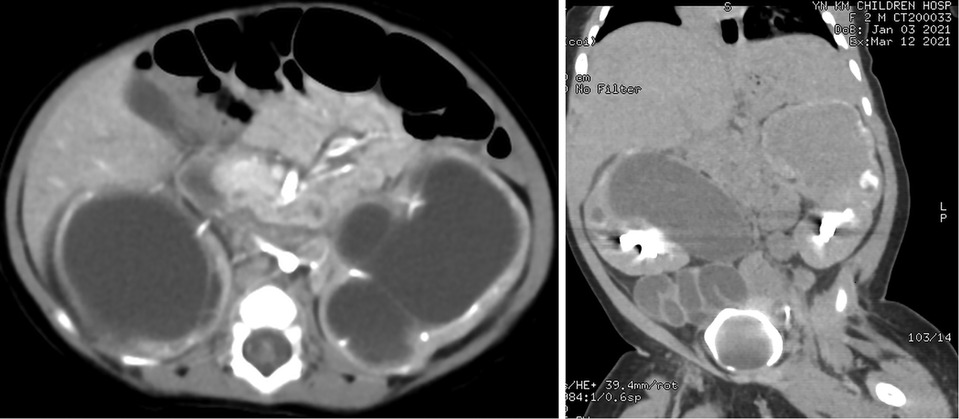
Figure 3. Results of preoperative CT showed severe hydronephrosis and ureterectasis of bilateral upper moiety, left ureteral opening, and the right ureterocele.
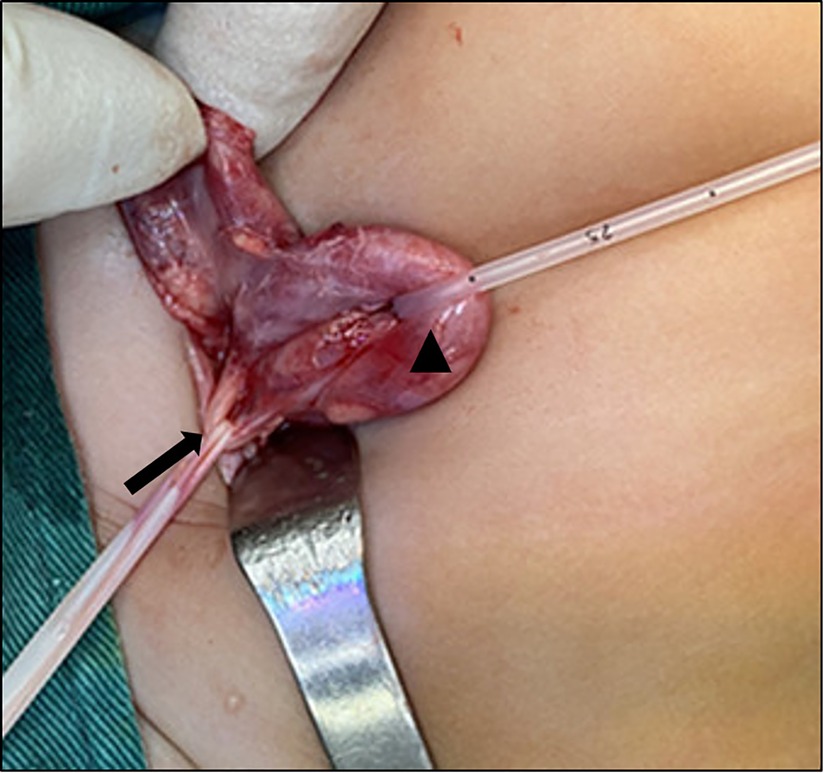
After discussion, cystoscopy and bilateral cutaneous ureterostomy was performed for the patient (Figure 4). In cystoscopy, ectopic insertion of lift upper moiety ureter and ureterocele of right upper moiety ureter were found. The patient's urinary tract infection (UTI) was cured soon after bilateral cutaneous ureterostomy, and she was discharged 5 days later (Figure 5).
No UTI a Figure 5 fever occurred in the patient during discharge. The results of routine urine examination were normal, and ultrasound indicated that bilateral hydronephrosis was relieved obviously. 13 months after the ureterostomy, the child was returned to the hospital for further surgery. IVP showed no hydronephrosis in bilateral duplex kidney (Figure 6). Voiding cystourethrography (VCU) showed mild vesicoureteral reflux (VUR) on the right lower moiety ureter (Figure 7). The patient recovered and was discharged on the 7th day after bilateral ureteroureterostomy. The D-J tubes were removed 1 month after operation (Figure 8).

Figure 7. Result of VCU before ureteroureterostomy showed mild vesicoureteral reflux (VUR) on the right lower moiety ureter.
Discussion
Prenatal ultrasound is necessary for both pregnant and fetus. With the continuous development and maturity of ultrasound technology, it not only helpful for diagnosing an obstruction of the urinary tract in pregnancies, but also meaningful for permitting the prenatal anatomical assessment of most congenital anomalies of the kidney and urinary tract during the second or third trimester (2, 3). The incidence of duplex kidney malformation is about 0.8% and it is common to women (4, 5). Among children diagnosed with hydronephrosis before birth, 5%–7% are due to duplex kidney (6). The duplex kidney can be divided into incomplete type (Y type) and complete type. The incidence of complete ureteral deformity is about 0.2% (7). According to Weigert-Meyer-Rule, the upper pole is normally seen as ectopic and therefore dysplastic due to obstruction, whereas the lower pole is related to vesicoureteral reflux (8–10).
Fetal interventions include ultrasound-guided bladder puncture and drainage and transurethral incision of ureterocele under fetal cystoscope. Although the decompression effect is good, there are risks of premature rupture of membranes, premature delivery, infection, bleeding, and fetal death, which need to be carefully evaluated and considered (11, 12). Nearly 60% of patients with duplex kidney are asymptomatic and need no treatment after birth. Patients with ectopic ureteral opening, ureteroceles, hydronephrosis, calcuil, urinary tract infection, or non-functional need surgical treatment (13). Treatment for duplex kidney needs to be individualized, and hemi-nephroureterectomy is the earliest technique used in duplex kidney therapy. If the duplex kidney function is good and there is no dysplasia, the upper moiety can be reserved. Common surgical methods include ureteric reimplantation, ureteroureterostomy, pelopureteroplasty, etc. (14). The objective of treatment is to prevent urinary tract infection, and renal damage and to achieve urinary continence (15).
The surgical indication for hemi-nephroureterectomy is upper renal function <10% due to recurrent urinary tract infection with vesicoureteral reflux, or severe obstruction (16, 17). And most scholars agree that upper moiety resection should be performed in patients with recurrent urinary tract infection and ipsilateral abdominal pain (18). However, it is controversial whether the operation should be performed in patients with renal function <10% and no relevant clinical symptom. Proponents believe that surgical removal of non-functional or dysplasia renal tissue and ureters can prevent the long-term occurrence of hypertension or pyelonephritis (1, 19). On the contrary, the possibility of long-term hypertension and pyelonephritis in the non-functional kidney is low, and the operation will easily affect the blood supply and function of the lower kidney, leading to kidney loss (15, 20, 21).
Ureteroureterostomy is usually performed at the level of the iliac vessels to avoid dissociation of the colon, interference with the nerves and vessels of the bladder, and extensive dissociation of the ureter (22). The procedure is not only easier than common sheath ureteral reimplantation but also can protect bladder function from damage. Anastomotic fistula, anastomotic stenosis, and ureteral stump complications are the main postoperative complications of this procedure, and the overall incidence is similar to that of common sheath ureteral bladder replantation (23).
In duplicated ureters with VUR, without obstruction, and with the preserved function of both renal moieties, the gold standard surgical intervention is ureteral reimplantation. However, the incidence of surgical complications is as high as 10%–12.5%, and bladder function will inevitably be disturbed. Studies showed that about 10% of patients require a second surgery (21, 24).
For patients with severe hydronephrosis combined with severe urinary tract infection and sepsis, timely removal of obstruction and urine drainage are beneficial to the recovery of duplex kidney function and the retention of the kidney (25, 26). Common urine drainage methods include ① Pyelostomy: This method is simple and effective. But it requires indent and regular replacement of external drainage tube, and later nursing is relatively tough for patients with troublesome for the caregivers. ② Transurethral incision of ureterocele (TIU): TUI has an invasive, cosmetic, and no external drainage surgical effect. However, this method has secondary or aggravating risks of VUR on the affected side, and patients with large cysts may also have postoperative cyst wall prolapse in the urethra. ③ Cutaneous ureterostomy: This operation has a definite curative effect, no external drainage after the operation, and postoperative nursing of infants is relatively convenient.
In this case, considering that both external renal drainage tubes should be placed after pyelostomy, and unilateral TIU has no definite significance for the relief of obstruction on the other side, so bilateral ureterostomy was performed in this case. The patient's hydronephrosis was significantly relieved after cutaneous ureterostomy, and IVP showed that the development of both kidneys was normal after 13 months. It indicated that timely relief of obstruction was of significance to salvage renal function.
At present, it is still controversial whether ureteral bladder reimplantation should be performed for duplex kidney with lower moiety VUR. Due to the low grade of reflux, ureteric reimplantation was not performed in our case for the following reasons: On the one hand, mild reflux has the possibility of self-healing. On the other hand, if the patient's grade of VUR is aggravated or recurrent urinary tract infection occurs, only a single ureteral bladder reimplantation will be required in the future. Compare with common sheath ureteral reimplantation, it requires a smaller bladder capacity, ureter diameter, and bladder mucosal tunnel length, which is not only beneficial to reduce surgical trauma and bladder disturbance, but also has a higher surgical success rate (24).
When indicated, the type of surgery for children with the complicated duplex renal anomaly is based on renal moiety function and lower tract anatomy, and sequential treatment is meaningful to reduce bladder disturbance, reduce surgical trauma and improve the success rate of surgery.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
CW and FJ performed the surgery and drafted the original manuscript. HZ and ZY collected data and participated in to amend the manuscript. BY and LL designed the operation scheme and amended the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study did received the support from: Yunnan Province Clinical Research Center for Children’s Health and Disease.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Michaud JE, Akhavan A. Upper pole heminephrectomy versus lower pole ureteroureterostomy for ectopic upper pole ureters. Curr Urol Rep. (2017) 18(3):21. doi: 10.1007/s11934-017-0664-0
2. Lin S, Shi S, Huang L, Lei T, Cai D, Hu W, et al. Is an analysis of copy number variants necessary for various types of kidney ultrasound anomalies in fetuses. Mol Cytogenet. (2019) 12:31. doi: 10.1186/s13039-019-0443-3
3. Pepe F, Pepe P. Color Doppler ultrasound (CDU) in the diagnosis of obstructive hydronephrosis in pregnant women. Arch Gynecol Obstet. (2013) 288(3):489–93. doi: 10.1007/s00404-013-2768-1
4. Chacko JK, Koyle MA, Mingin GC, Furness PD 3rd. Ipsilateral ureteroureterostomy in the surgical management of the severely dilated ureter in ureteral duplication. J Urol. (2007) 178(4 Pt 2):1689–92. doi: 10.1016/j.juro.2007.05.098
5. O'Connor E, Teh J, Lawrentschuk N. Robot-assisted ipsilateral ureteroureterostomy in a duplex system utilizing intraoperative flexible ureteroscopy. Urol Case Rep. (2020) 31:101158. doi: 10.1016/j.eucr.2020.101158
6. Nguyen HT, Herndon CD, Cooper C, Gatti J, Kirsch A, Kokorowski P, et al. The society for fetal urology consensus statement on the evaluation and management of antenatal hydronephrosis. J Pediatr Urol. (2010) 6(3):212–31. doi: 10.1016/j.jpurol.2010.02.205
7. Hartman GW, Hodson CJ. The duplex kidney and related abnormalities. Clin Radiol. (1969) 20(4):387–400. doi: 10.1016/S0009-9260(69)80091-7
8. Kaplan WE, Nasrallah P, King LR. Reflux in complete duplication in children. J Urol. (1978) 120(2):220–2. doi: 10.1016/S0022-5347(17)57116-5
9. Doery AJ, Ang E, Ditchfield MR. Duplex kidney: not just a drooping lily. J Med Imaging Radiat Oncol. (2015) 59(2):149–53. doi: 10.1111/1754-9485.12285
10. Darr C, Krafft U, Panic A, Tschirdewahn S, Hadaschik BA, Rehme C. Renal duplication with ureter duplex not following Meyer-Weigert-rule with development of a megaureter of the lower ureteral segment due to distal stenosis: a case report. Urol Case Rep. (2020) 28:101038. doi: 10.1016/j.eucr.2019.101038
11. Chalouhi GE, Morency AM, De Vlieger R, Martinez JM, Blanc T, Hodges R, et al. Prenatal incision of ureterocele causing bladder outlet obstruction: a multicenter case series. Prenat Diagn. (2017) 37(10):968–74. doi: 10.1002/pd.5091
12. Persico N, Berrettini A, Fabietti I, Dallagiovanna C, Minoli D, Mosca F, et al. New minimally invasive technique for cystoscopic laser treatment of fetal ureterocele. Ultrasound Obstet Gynecol. (2017) 50(1):124–7. doi: 10.1002/uog.17296
13. Dino MS, Tefera AT, Gebreselassie KH, Akkasa SS, Mummed FO. Complete duplex of the left ureter with lower moiety hydronephrosis secondary to ureteral stone in adult. Case Rep Urol. (2022) 2022:6552889. doi: 10.1155/2022/6552889
14. Herz D, Smith J, McLeod D, Schober M, Preece J, Merguerian P. Robot-assisted laparoscopic management of duplex renal anomaly: comparison of surgical outcomes to traditional pure laparoscopic and open surgery. J Pediatr Urol. (2016) 12(1):44.e1–7. doi: 10.1016/j.jpurol.2015.04.046
15. Luo J, Tan XH, Liu X, He DW, Lin T, Li XL, et al. Anatomy and management of upper moiety vascular variation in children with duplex kidney. J Pediatr Surg. (2019) 54(10):2130–3. doi: 10.1016/j.jpedsurg.2019.04.011
16. Spinoit A, Ploumidis A, Novara G, Mottrie A. Robot-assisted single-site upper pole hemi-nephrectomy in an adult patient with a duplicated collecting system: is it feasible. Minerva Urol Nefrol. (2016) 68(5):466–8. doi: 10.1016/j.jpurol.2018.06.006
17. Mohan H, Kundu R, Dalal U. Renal cell carcinoma arising in ipsilateral duplex system. Turk J Urol. (2014) 40(3):185–8. doi: 10.5152/tud.2014.93708
18. Dönmez MI, Yazici MS, Abat D, Kara Ö, Bayazit Y, Bilen CY. Laparoscopic upper pole heminephrectomy in adults for treatment of duplex kidneys. Urol J. (2015) 12(2):2074–7.
19. Szklarz MT, Ruiz J, Moldes JM, Sentagne A, Tuchbaum V, Tessi C, et al. Laparoscopic upper-pole heminephrectomy for the management of duplex kidney: outcomes of a multicenter cohort. Urology. (2021) 156:245–50. doi: 10.1016/j.urology.2021.01.032
20. Wadham B, DeSilva A, Connolly T, Alshafei A, Keene D, Hennayake S. The place of retroperitoneoscopic hemi-nephroureterectomy for duplex kidney in children; risk of damage to the remnant moiety and strategies to reduce the risk. J Pediatr Urol. (2021) 17(5):708.e1–e8. doi: 10.1016/j.jpurol.2021.07.033
21. Lee YS, Im YJ, Shin SH, Bascuna RT Jr, Ha JY, Han SW. Complications after common sheath reimplantation in pediatric patients with complicated duplex system. Urology. (2015) 85(2):457–62. doi: 10.1016/j.urology.2014.10.014
22. Grimsby GM, Merchant Z, Jacobs MA, Gargollo PC. Laparoscopic-assisted ureteroureterostomy for duplication anomalies in children. J Endourol. (2014) 28(10):1173–7. doi: 10.1089/end.2014.0113
23. Gerwinn T, Gnannt R, Weber DM, Gobet R, Mazzone L. Laparoscopic ureteroureterostomy vs. common sheath ureteral reimplantation in children with duplex kidney anomalies. Front Pediatr. (2021) 9:637544. doi: 10.3389/fped.2021.637544
24. Rodriguez MV, Boysen WR, Gundeti MS. Robot-assisted laparoscopic common sheath ureteral reimplantation in duplex ureters: LUAA technique tips for optimal outcomes. J Pediatr Urol. (2018) 14(4):353–5. doi: 10.1016/j.jpurol.2018.06.006
25. Wong NC, Braga LH. Open ureteroureterostomy for repair of upper-pole ectopic ureters in children with duplex systems: is stenting really necessary. J Pediatr Urol. (2019) 15(1):72.e1–7. doi: 10.1016/j.jpurol.2018.10.014
Keywords: child, duplex kidney, renal malformation, ureterostomy, ureteroureterostomy
Citation: Wu C, Ji F, Zhang H, Yao Z, Li L and Yan B (2022) Treatment for complete bilateral duplex kidneys with severe hydronephrosis and ureterectasis of the upper moiety in a child: A case report and literature review. Front. Surg. 9:1019161. doi: 10.3389/fsurg.2022.1019161
Received: 14 August 2022; Accepted: 11 October 2022;
Published: 2 November 2022.
Edited by:
Chang Xu, West China Hospital, Sichuan University, ChinaReviewed by:
Tianqi Zhu, Huazhong University of Science and Technology, ChinaPietro Pepe, Cannizzaro Hospital, Italy
© 2022 Wu, Ji, Zhang, Yao, Li and Yan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bing Yan eWFuYmluZzI5QDE2My5jb20=
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Pediatric Surgery, a section of the journal Frontiers in Surgery
 Chengchuang Wu
Chengchuang Wu Fengming Ji
Fengming Ji Huangchenghao Zhang
Huangchenghao Zhang Zhigang Yao1
Zhigang Yao1