
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Surg. , 13 October 2022
Sec. Orthopedic Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.1014314
This article is part of the Research Topic Advances in Research of Degenerative Orthopedic Conditions: from Basic to Clinical Research View all 32 articles
Purpose: To compare the effectiveness and safety of oblique lateral interbody fusion (OLIF) and minimally invasive transforaminal lumbar interbody fusion (MI-TLIF) for degenerative lumbar disease.
Methods: We searched relevant studies in Embase, PubMed, Cochrane, and Web of Science databases comprehensively from inception to March 2022. The data were extracted from included studies, including operation indications, radiographic parameters, and clinical outcomes. Random or fixed-effects models were used in all meta-analyses according to the between-study heterogeneity.
Results: In total, 30 studies, including 2,125 patients, were included in this meta-analysis. Our study found similar disk height, length of hospital stay, visual analog scale (VAS), and Oswestry disability index(ODI) between the two groups. However, the OLIF showed an advantage in restoring lumbar lordotic angle compared with MI-TLIF, with the pooled mean change of 17.73° and 2.61°, respectively. Additionally, the operative time and blood loss in the OLIF group appeared to be less compared with the MI-TLIF group. Regarding complications, the rates of the two groups were similar (OLIF 14.0% vs. MI-TLIF 10.0%), but the major complications that occurred in these two procedures differed significantly.
Conclusion: The results of disk height, length of hospital stay, VAS, and ODI between the OLIF and MI-TLIF groups were similar. And the OLIF was superior in restoring lumbar lordotic angle, operative time, and blood loss. However, the OLIF group's complication rate was higher, although not significantly, than that in the MI-TLIF group.
With the increased human life expectancy around the world, the degenerative lumbar disease has a higher incidence, and it has become the leading cause affecting the quality of life in the elderly population (1). For patients with chronic low back pain or when the conservative treatment is ineffective, lumbar interbody fusion (LIF) is considered the most effective surgical procedure for degenerative lumbar disease (2), including degenerative spondylolisthesis, disc herniation, and deformity. Spinal fusion surgery can be performed to restore the disc height (DH) and immobilize unstable segments (3). According to different surgical approaches, LIF can be traditionally divided into the anterior, posterior, and open transforaminal types (4).
Although the classical surgical method can achieve satisfactory clinical efficacy, such iatrogenic complications as excessive blood loss, nerve injury, and muscular denervation induced by paravertebral muscle stripping cannot be avoided (5, 6). Besides, this surgical method also has the disadvantages of longer operative time and hospital stays. In recent years, minimally invasive techniques have achieved significant advancement, which contributes to fewer surgical complications and shorter hospital stays (6). Foley and Lefkowitz (7) proposed minimally invasive transforaminal lumbar interbody fusion (MI-TLIF) in 2002, which could minimize operative trauma compared with traditional open transforaminal LIF. In addition, Silvestre described oblique lateral LIF in 2012 to avoid nerve injury (8).
MI-TLIF and oblique lateral interbody fusion (OLIF) have achieved favorable efficacy in extensive clinical applications. However, the differences between OLIF and MI-TLIF have not been sufficiently explored. OLIF is a minimally invasive LIF with a surgical approach to the natural space in the lateral front of the body without damaging the muscle, ligament, and bone structure (8). MI-TLIF has a surgical approach through the intervertebral multifidus and longissimus muscle system of the lumbar paraspinal, which does not require extensive dissection. The intermuscular approach is characterized by less injury and less bleeding, and excessive traction of nerve roots and dual sacs would not be required for this approach, so it is safer to handle the intervertebral space (7). However, it remains unclear about the optimal surgical technique for treating these diseases. Therefore, to compare the radiographic and clinical outcomes of OLIF and MI-TLIF in treating degenerative lumbar disease, some relevant studies in recent years were summarized in the meta-analysis, thus providing the latest and most compelling evidence for clinicians.
The systematic review and meta-analysis comparing OLIF and MIS-TLIF in treating degenerative lumbar disease were conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement.
In the study, Embase, PubMed, Cochrane, and Web of Science were comprehensively retrieved to select relevant articles published from January 2019 to March 2022 based on an English language restriction condition. The combined text and MeSH terms included (“OLIF” or “oblique lumbar interbody fusion”), (“MIS-TLIF” or “minimally invasive transforaminal lumbar interbody fusion”), and (“degenerative scoliosis” or “degenerative spinal deformity”). Moreover, the reference lists were also checked by manual retrieval for relevant articles.
Two investigators independently conducted screening in respect of the title and abstract of articles, and the full text of relevant articles was reappraised according to the inclusion and exclusion criteria. A third investigator participated in the resolution in case of any disagreement. The inclusion criteria included: (1) target patients: a diagnosis of degenerative lumbar disease; (2) intervention: single spine surgery, OLIF or MI-TLIF; (3) outcomes: sufficient information including surgical indications (operative blood loss, operative time, and length of hospital stay), radiographic parameters (DH and lumbar lordotic angle [LLA]), visual analog scale (VAS), and Oswestry disability index (ODI). Reviews and case reports were not included in the meta-analysis. Duplicates or multiple publications of the same study were also excluded.
According to an established data abstraction form, two investigators independently extracted the following data from each included article: (1) study characteristics (author, year of publication, patient diagnosis, and number of patients); (2) radiographic parameters (DH and LLA); (3) surgical indications (operative blood loss, operative time, and length of hospital stay); (4) VAS and ODI.
Two investigators independently evaluated the literature quality according to the PRISMA recommendation. These studies were evaluated based on the Newcastle-Ottawa scale (NOS) (9), which was composed of nine items, including selection (four points), comparability (two points), and exposure (three points). A study awarded seven or more points can be considered high quality. The author’s name, institution, journal name, and other related information were hidden during the evaluation process to reduce the influence of subjective factors.
All statistical analyses were performed with Stata software (version 14.0). The heterogeneity among these studies was evaluated with the Cochran Q and I2 test (10). A fixed effects model was used if P > 0.05 or I2 < 50%; otherwise, a random effects model was employed (11). Additionally, a meta-regression model was used to investigate the contribution of age and follow-up duration to the radiographic and clinical outcomes. P-value <0.05 was considered statistically significant.
In this study, a total of 1,194 studies were screened from Embase, PubMed, Cochrane, and Web of Science. After duplicates were removed, 633 studies were involved in case reports, irrelevant studies, and reviews, and hence were excluded. Two investigators conducted a full-text assessment for the remaining 89 articles. Eventually, only 30 studies including 2,125 patients in total were eligible and included in this meta-analysis (Figure 1).
In this meta-analysis, a total of 30 studies were included. Among them, there were 15 retrospective pre-post studies related to the clinical efficacy of OLIF, 12 studies related to the clinical efficacy of MI-TLIF, and 3 retrospective cohort studies related to the comparison of the efficacy between OLIF and MI-TLIF. Specifically, 1,057 patients aged 50.8–69.7 years (mean 59.2 y) in 18 studies received OLIF, and 1,068 patients aged 50.9–66.4 years (mean 59.3 y) in 15 studies received MI-TLIF. The basic characteristics of these studies are listed in Tables 1, 2.
These 30 studies were independently evaluated by two investigators from the perspective of the risk of bias according to the NOS, their scores were all ≥6 points (Table 3). All studies included appropriate patients with a clear diagnosis and presented important outcomes after OLIF or MI-TLIF.
For OLIF, the length of hospital stay was reported in 5 studies (N = 228), and the pooled mean length of hospital stay was 4.73 days [95% CI (3.48, 5.99), P < 0.001; Figure 2A]. There was substantial heterogeneity between studies (I2 = 94.1%). For MI-TLIF, the length of hospital stay was reported in 12 studies (N = 653), and the pooled mean length of hospital stay was 6.27 days [95% CI (3.48, 5.99), P < 0.001; Figure 2B].
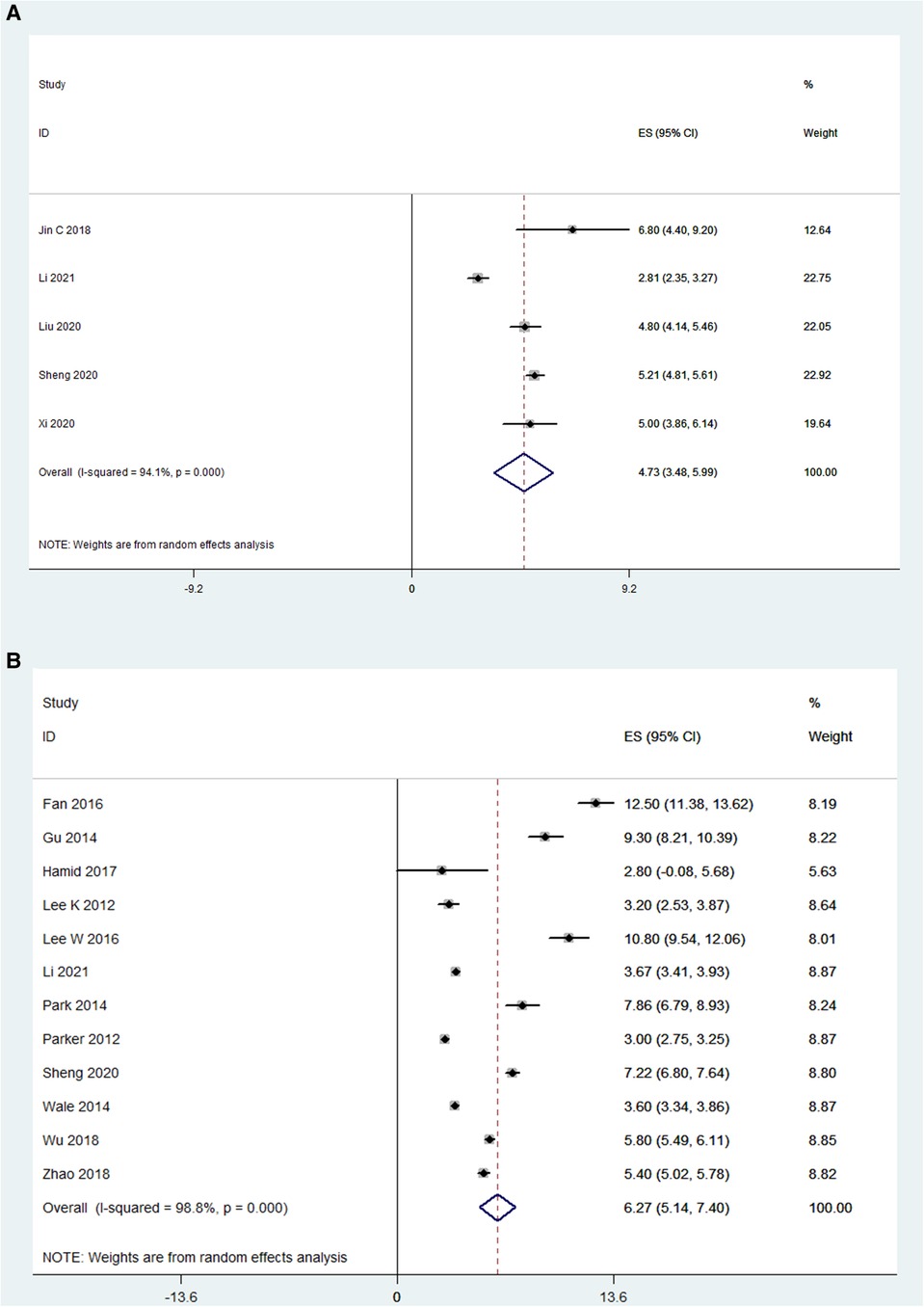
Figure 2. Forest plot and pooled estimates of the length of hospital stay. Outcomes assessed are (A) OLIF group; (B) MI-TLIF group.
The operative time was reported in 12 OLIF studies (N = 795) and 13 MI-TLIF studies (N = 692). Based on the random effects model, the mean operative time was 135.4 min in the OLIF group [95% CI (110.12, 160.65), P < 0.001; Figure 3A], compared with 188.9 min in the MI-TLIF group [95% CI (168.27, 209.52), P < 0.001; Figure 3B].
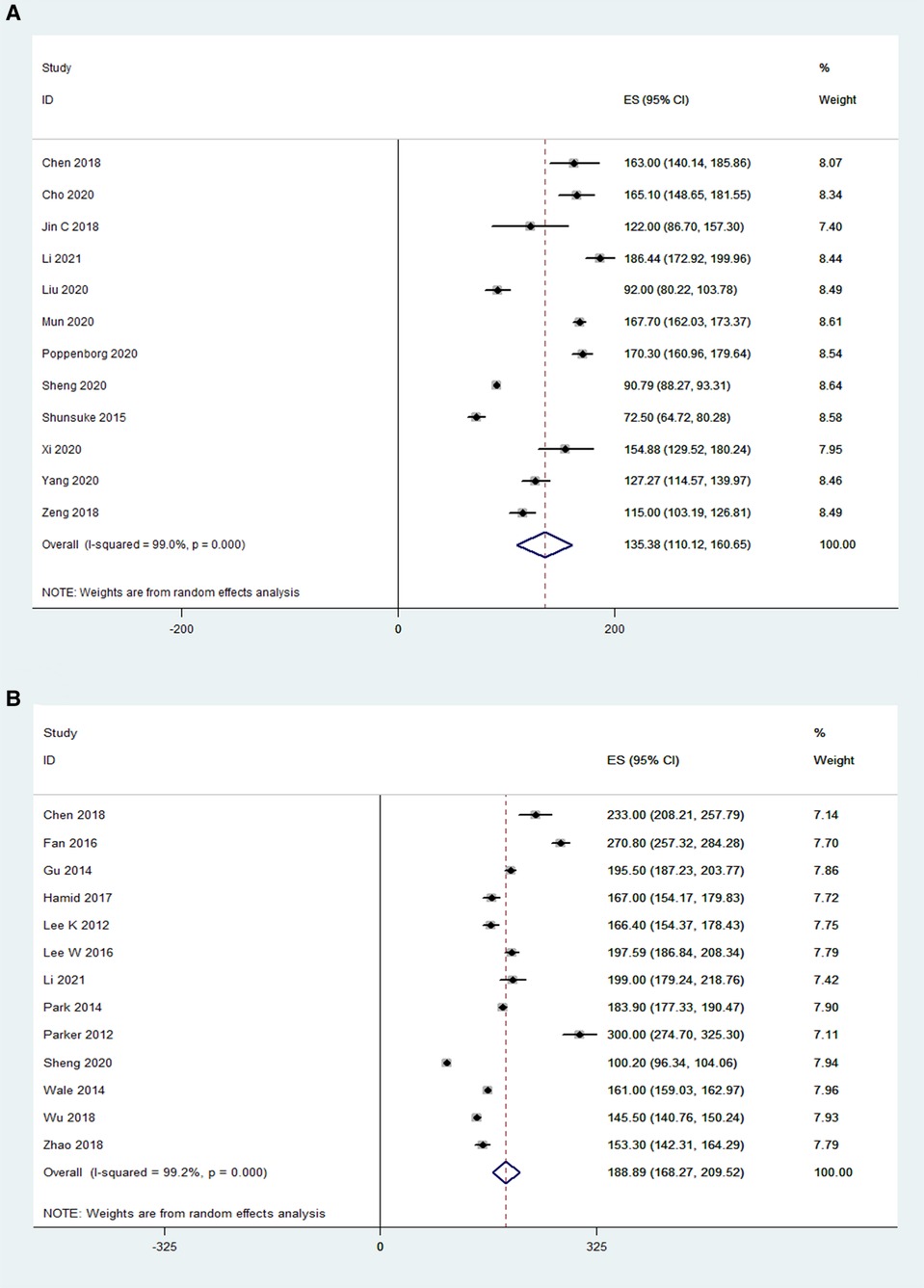
Figure 3. Forest plot and pooled estimates of operative time. Outcomes assessed are (A) OLIF group; (B) MI-TLIF group.
Blood loss was reported in 10 OLIF studies (N = 610) and 13 MI-TLIF studies (N = 692). According to the pooled analysis results, the mean blood loss in the OLIF group was 107.1 ml [95% CI (81.90, 132.22), P < 0.001; Figure 4A], compared with 243.52 ml in the MI-TLIF group [95% CI (200.35, 286.69), P < 0.001; Figure 4B].
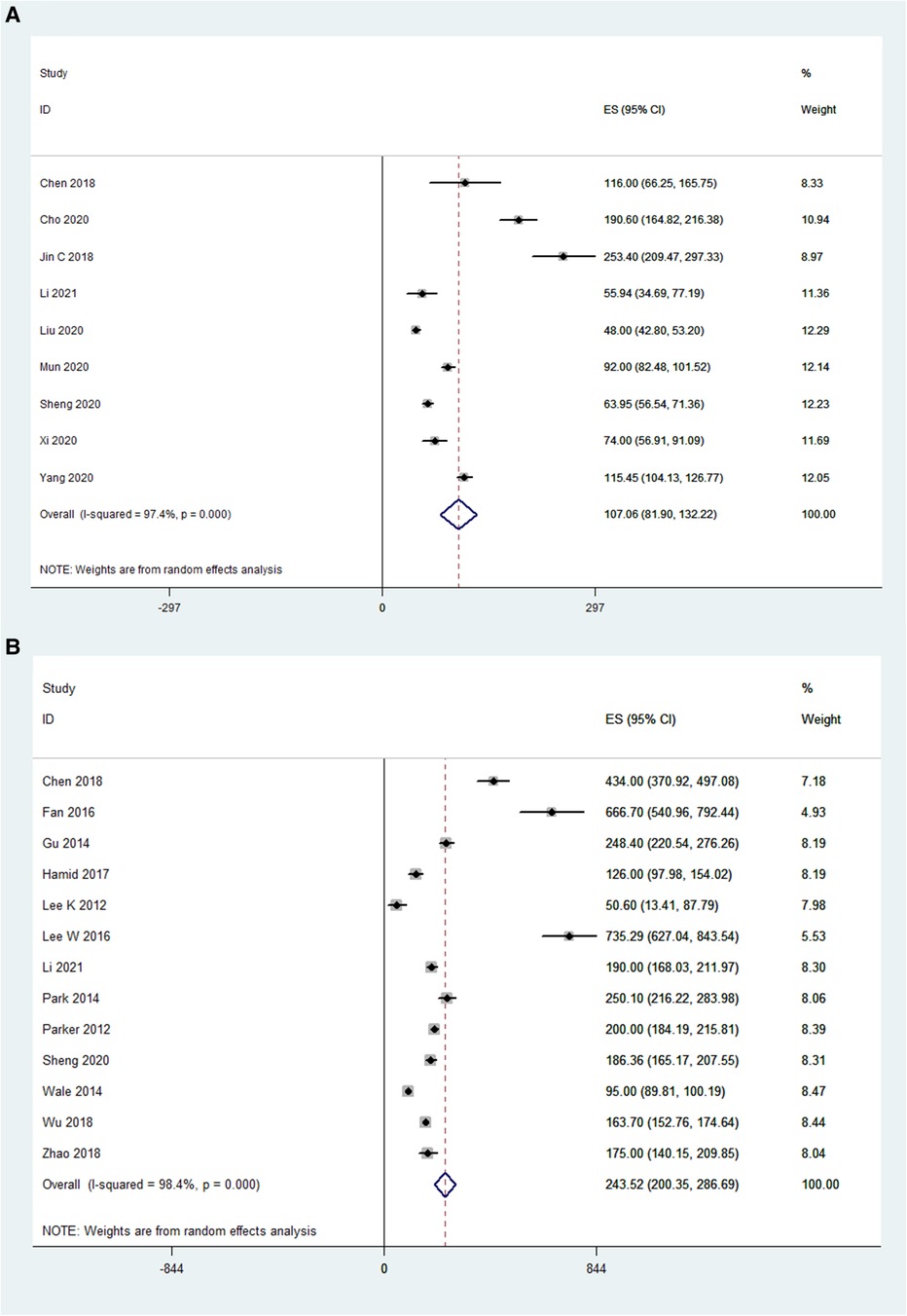
Figure 4. Forest plot and pooled estimates of blood loss. Outcomes assessed are (A) OLIF group; (B) MI-TLIF group.
The pooled analysis results of 7 OLIF studies (N = 226) showed that OLIF induced a mean increase in the disc height, and the weighted mean difference (WMD) was −4.88 [95% CI (−5.71, −4.06), P < 0.001; Figure 5A]. While, the pooled analysis results of 3 MI-TLIF studies (N = 286) also showed a mean increase in the DH caused by MI-TLIF, and the weighted mean difference (WMD) was −3.01 [95% CI (−4.86, −1.16), P = 0.001; Figure 5B]. The surgical effect can be evaluated by subtracting the postoperative DH from the preoperative DH. Hence, larger negative values represented more significant surgical effects. Of note, before the pooled analysis of the DH, the number of operative levels between both study groups was compared. The results showed that the mean number of OLIF-operated levels was 1.31 ± 0.3, and that of MI-TLIF-operated levels was 1.29 ± 0.44. There was no significant difference between these surgery techniques (P = 0.55).
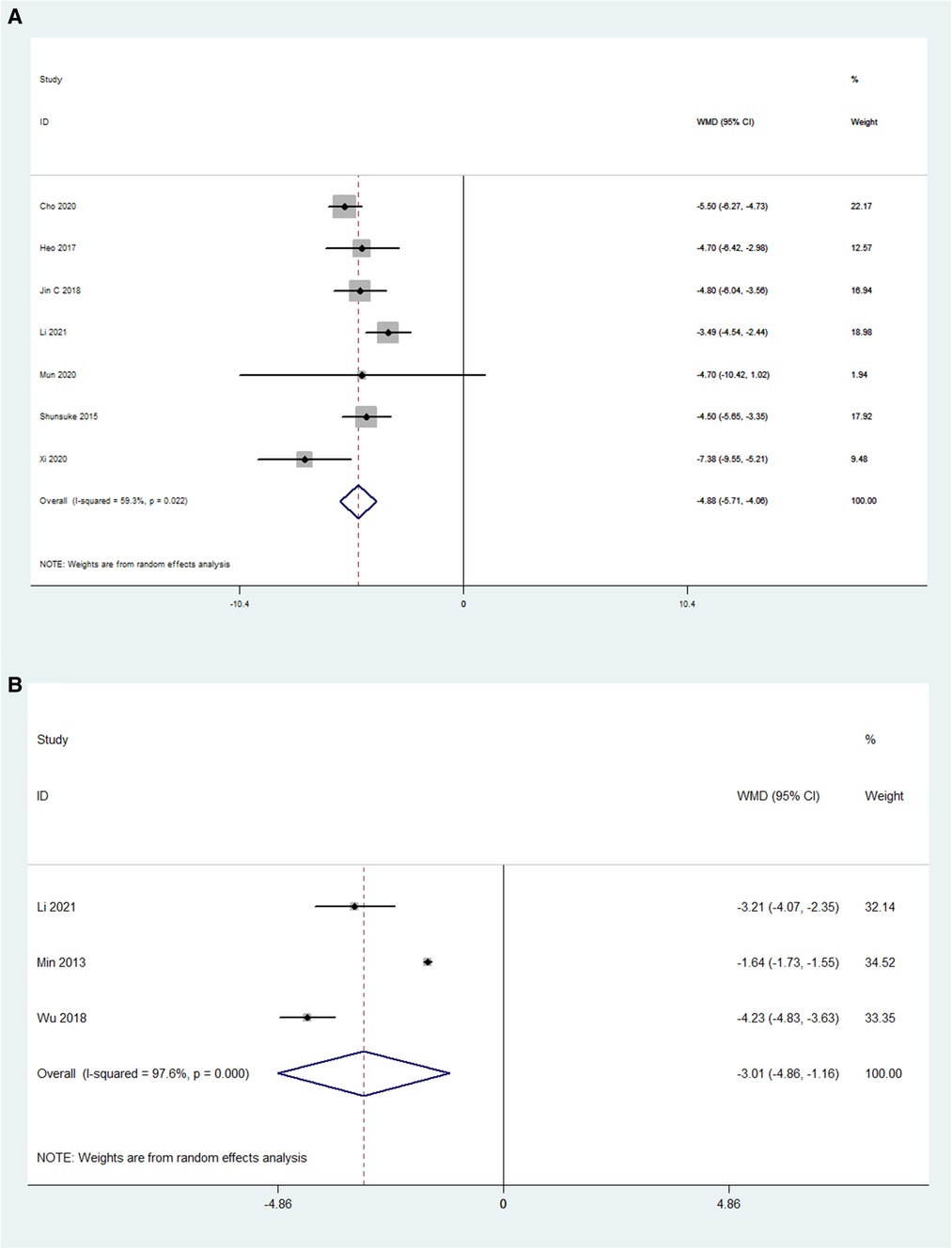
Figure 5. Forest plot and pooled estimates of disk height. Outcomes assessed are (A) OLIF group; (B) MI-TLIF group.
The preoperative and postoperative LLAs were also compared in 6 OLIF studies (N = 133) and 4 MI-TLIF studies (N = 303). The pooled analysis results of these OLIF studies showed the WMD was −17.73 [95% CI (-30.19, −5.27), P < 0.001; Figure 6A]. The pooled analysis results of these MI-TLIF studies showed the WMD was −2.61 [95% CI (−3.05, −2.16), P < 0.001; Figure 6B]. The changes in the LLA can be evaluated by subtracting the postoperative LLA from the preoperative LLA. Hence, larger negative values represented more significant surgical effects. The WMD in both groups was positive, indicating that LLA was improved after surgery.
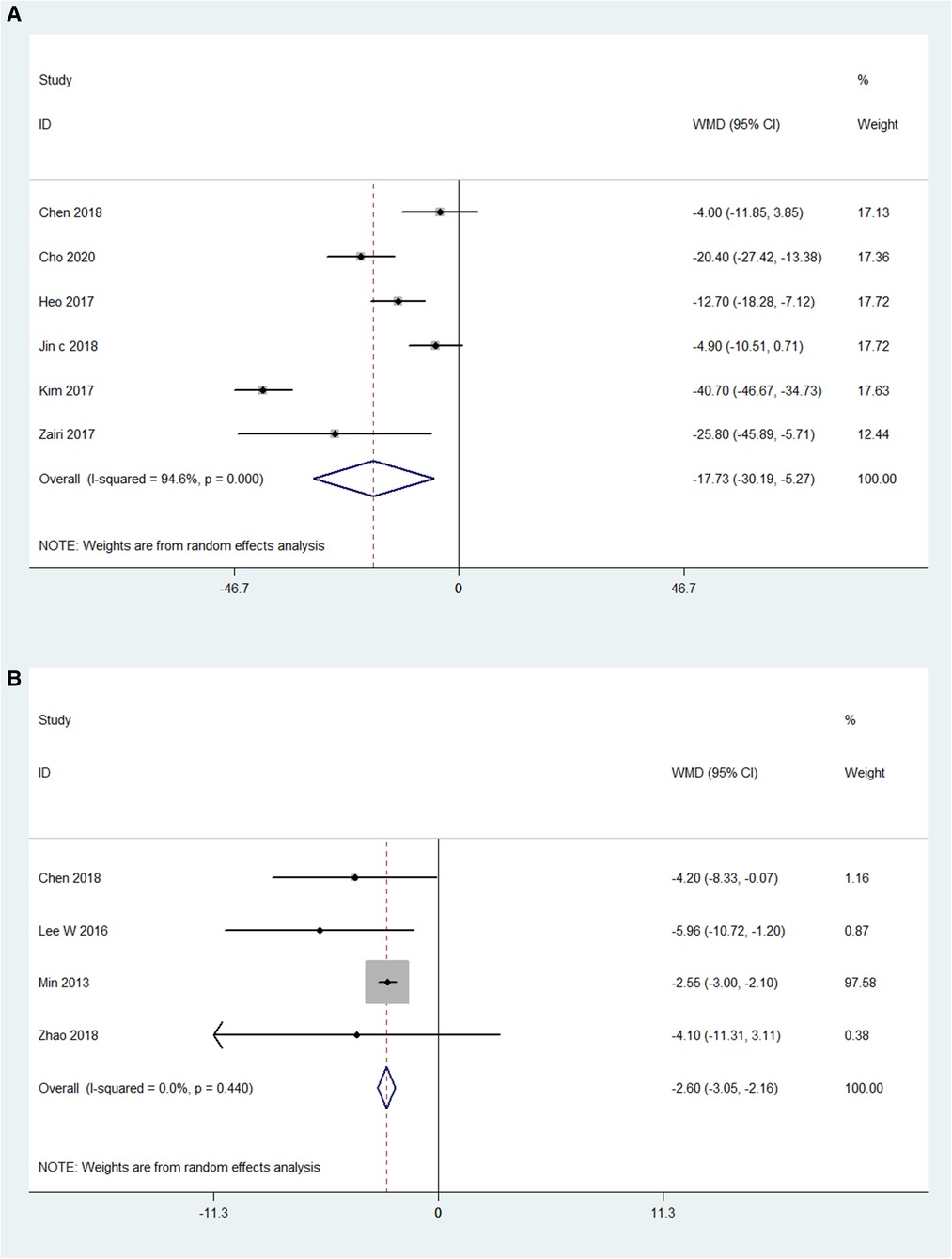
Figure 6. Forest plot and pooled estimates of lumbar lordotic angle. Outcomes assessed are (A) OLIF group; (B) MI-TLIF group.
For OLIF surgery, the VAS was reported in 11 studies (N = 692), and the preoperative VAS and postoperative VAS were compared in these studies (I2 = 98%). The pooled analysis results showed that the WMD was 4.51 [95% CI (3.16, 5.85), P < 0.001; Figure 7A]. For MI-TLIF surgery, the VAS was reported in 12 studies (N = 752). The pooled analysis results showed that there was a significant difference in VAS before and after MI-TLIF surgery [WMD = 3.24, 95% CI (0.22, 6.27), P < 0.001; Figure 7B]. In addition, the WMD in both groups was positive, indicating that the VAS score was improved after surgery.

Figure 7. Forest plot and pooled estimates of visual analog scale. Outcomes assessed are (A) OLIF group; (B) MI-TLIF group.
The preoperative ODI and postoperative ODI were compared in 11 OLIF studies (N = 1,289). The pooled WMD was 34.05 [95% CI (21.99, 46.08), P < 0.001; Figure 8A]. While, the preoperative ODI and postoperative ODI were compared in 12 MI-TLIF studies (N = 752). The pooled WMD was 28.30 [95% CI (24.03, 32.56), P < 0.001; Figure 8B]. The improvement of ODI can be evaluated by subtracting the postoperative ODI from the preoperative ODI. Hence, larger positive values represented more significant surgical effects. The WMD in both groups was positive, indicating that ODI was improved after surgery.
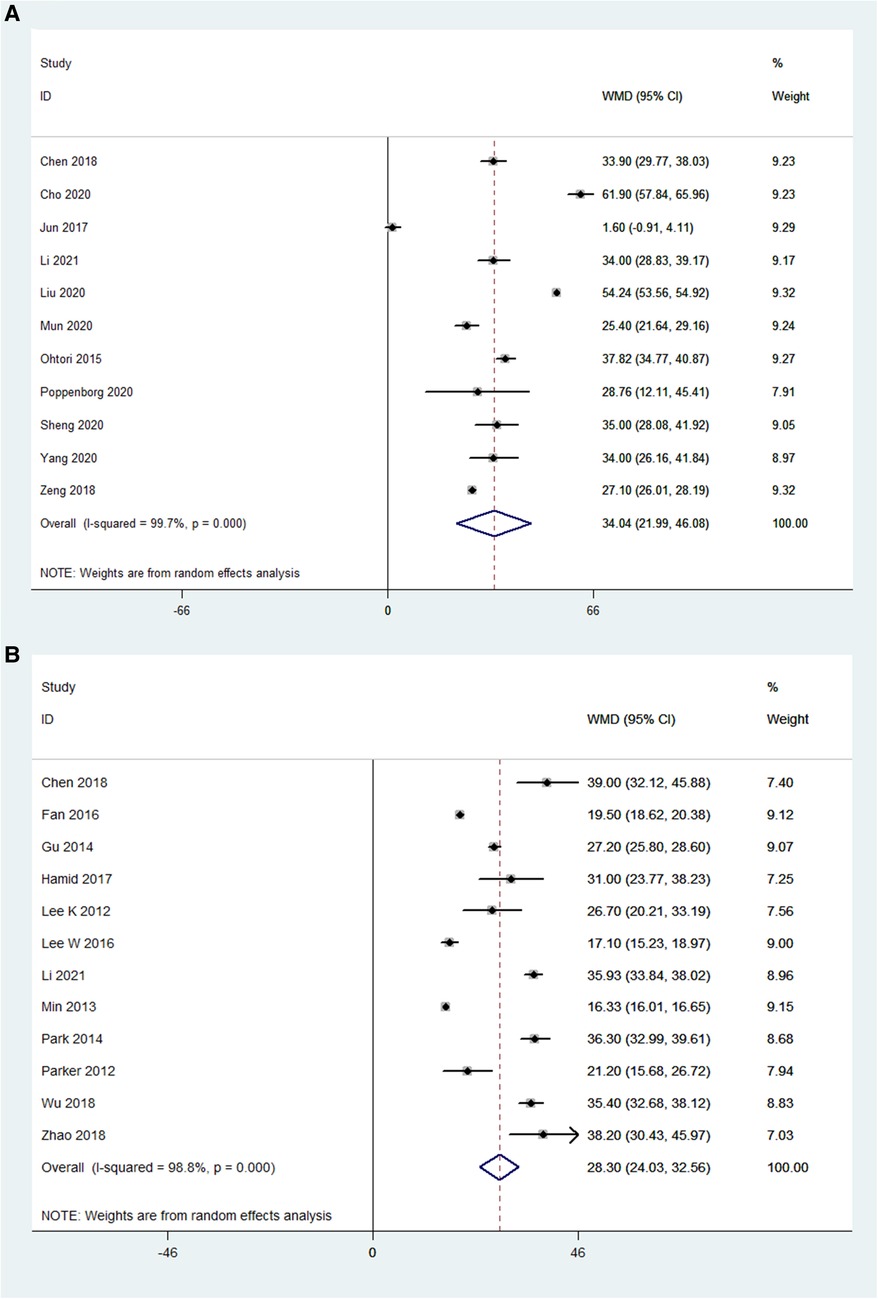
Figure 8. Forest plot and pooled estimates of Oswestry disability index. Outcomes assessed are (A) OLIF group; (B) MI-TLIF group.
The number of complications was reported in 11 OLIF studies (N = 726) (I2 = 85.6%). The pooled analysis results of these OLIF studies showed that the incidence of complications was 14.5% [95% CI (12.0%, 16.9%), P < 0.001], with individual study estimates ranging from 5.4% to 28.6% (Figure 9A). The most common complication was thigh pain/numbness (7.3%). Other main complications included endplate injury (5.4%), vascular injury (2.5%), and neurological injury (1.0%). The details of perioperative complications of OLIF are listed in Table 4. While, the number of complications was reported in 9 MI-TLIF studies (N = 544), accounting for a pooled prevalence of 10.0% [95% CI (7.1%, 12.3%), P < 0.001], with individual study estimates ranging from 7.2% to 17.1% (Figure 9B). The most common complication was endplate injury (3.41%). Other main complications included neurological injury (1.0%), wound infection (0.85%), and thigh pain/numbness (0.61%). The details of perioperative complications of MI-TLIF are also listed in Table 4.
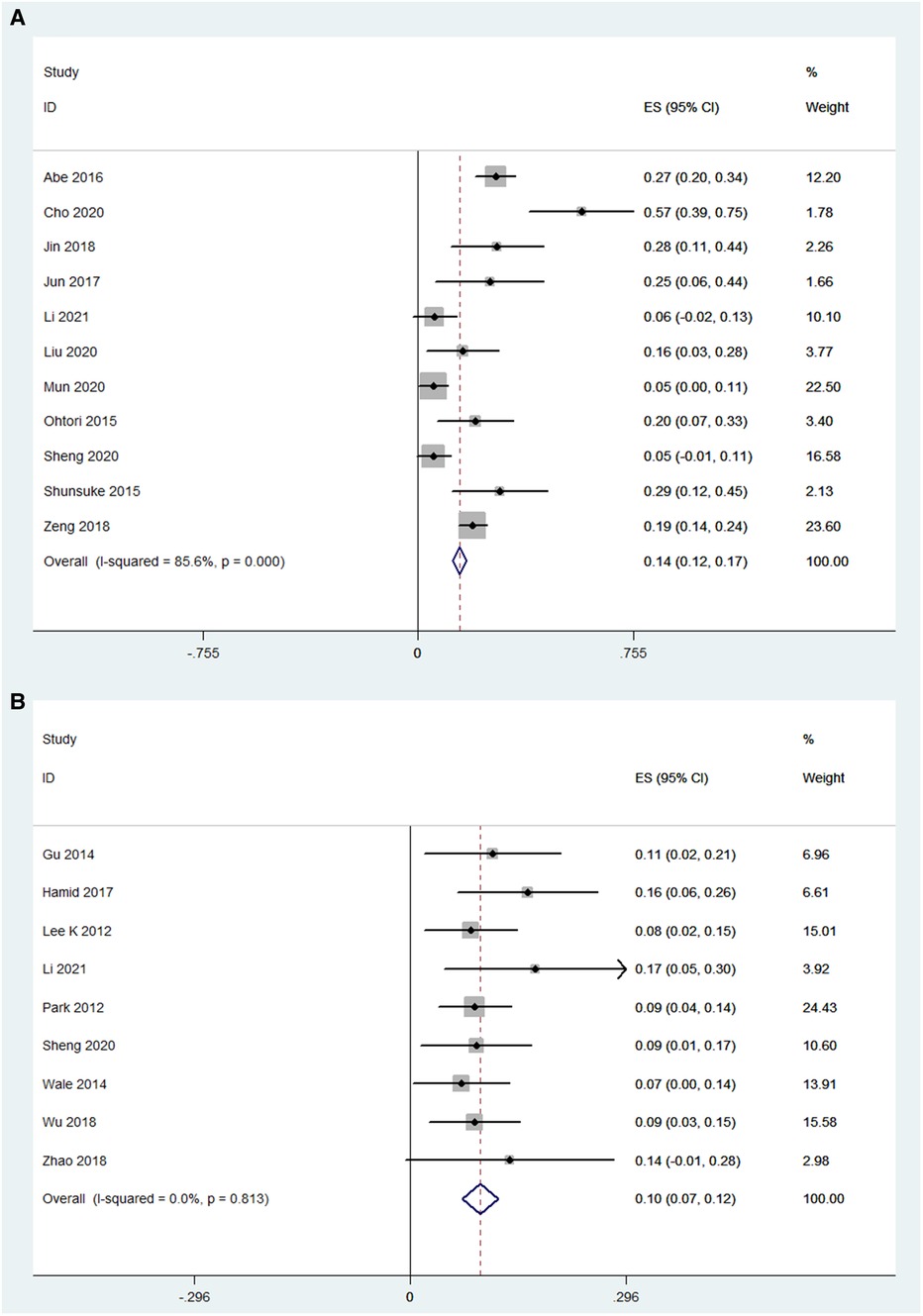
Figure 9. Forest plot and pooled estimates of complications. Outcomes assessed are (A) OLIF group; (B) MI-TLIF group.
The meta-regression analysis results showed that the age of patients would not affect the DH, LLA, VAS, and ODI scores in both OLIF and MI-TLIF groups. However, the follow-up duration was associated with the DH and postoperative ODI scores in the OLIF group (Table 5).
The optimal surgical procedure for treating degenerative lumbar disease has not been established for years. There are various disadvantages for traditional open surgical methods (for instance anterior, posterior, and transforaminal LIF), such as more iatrogenic complications, longer operative time, and longer hospital stays. Thus, OLIF and MI-TLIF can be widely used in treating degenerative lumbar disease with the significant advancement of minimally invasive surgical techniques. As per many studies (28, 41), both OLIF and MI-TLIF can achieve satisfactory clinical outcomes. However, the effectiveness and safety of both surgical techniques remain controversial and have not been systematically confirmed. Thus, relevant studies in the last three years were included in this study to evaluate and compare the effectiveness and safety of OLIF and MI-TLIF during the treatment of degenerative lumbar disease, thus providing the latest and most compelling evidence for clinicians. In the past three years, MIS TLIF and OLIF have achieved rapid and significant development with the advancement of instruments, the increased quantity of surgery, the popularization of techniques, and the popularization of training courses. Compared with conventional surgical techniques, there was no update on the general review. In the complete literature review, only the articles published in the last three years were included and updated for analysis.
Among these included studies, the length of hospital stay was evaluated in 5 OLIF studies and 12 MI-TLIF studies. There was a similar length of hospital stay between the OLIF (4.73 days) and MI-TLIF (6.27 days) groups. As is reported in some studies (42, 43), OLIF can reduce the length of hospital stay compared with conventional surgical techniques, such as posterior LIF. Nevertheless, there was no significant difference between OLIF and minimally invasive procedures, such as MI-TLIF (44, 45). This result was consistent with our findings. In one recent meta-analysis (46), the length of stay in the MI-TLIF group was significantly shorter than that in the Open-TLIF group. However, Sulaiman et al. (37) and Lau et al. (47) found no significant difference between the two groups. Besides, Hey et al. (48) also found no significant difference in the length of hospital stay between Open-TLIF and MI-TLIF at a single level.
The operative time and blood loss in the OLIF group appeared to be less than those in the MI-TLIF group. According to a study of Jin et al. (49), it may be attributed to a smaller surgical incision due to the muscle-splitting approach in the OLIF, which may result in shorter operative time. In addition, the retroperitoneal space was reached by blunt dissection during OLIF, which may lead to less bleeding. However, the screw placement and combination at multiple levels during MI-TLIF may need much operative time.
To evaluate the improvement in radiographic parameters by OLIF and MI-TLIF, the DH and LLA in these studies were analyzed. The analysis results showed that OLIF and MI-TLIF achieved similar improvement in the DH, with the pooled mean change being 4.88 and 3.01 mm, respectively. Besides, the postoperative DH in both groups was not significantly higher than the preoperative one. This finding was consistent with the results of previous studies, which indicated that OLIF and MI-TLIF might not restore the DH significantly (13, 50).
Moreover, the pooled analysis results showed that the OLIF group achieved more significant improvement in the LLA than the MI-TLIF group, with the pooled mean change being 17.73° and 2.61°, respectively. This result partly differed from that of some previous studies. In a recent review, Li et al. (51) reported high similarities in the restoration of LLA in both groups. The difference can be explained in several ways. According to the findings of Sato et al. (17), LLA can be restored effectively by OLIF with posterior supplement fixation. In this study, most patients had undergone posterior supplement fixation. Besides, the OLIF technique can more easily reach the anterior column and might use cages with higher lordotic angles (5).
In this study, VAS and ODI were employed to measure clinical outcomes. The pooled analysis results showed that both OLIF and MI-TLIF can significantly decrease VAS (for back pain) and ODI scores. There were similar VAS results between the OLIF and MI-TLIF groups (4.51 vs. 3.24). In theory, however, OLIF would significantly reduce the postoperative VAS score due to minor trauma compared with MI-TLIF. The use of analgesics may partially contribute to similar results. Furthermore, it was also found that the ODI scores in the OLIF group had a more significant decrease compared with the MI-TLIF group (34.05 vs. 28.30).
According to the meta-analysis results, there was no significant difference in the incidence of complications between the OLIF group (14.0%) and the MI-TLIF group (10.0%). However, the major complications that occurred in these two procedures differed significantly. The most common complication of OLIF was thigh pain/numbness (7.3%), and other main complications included hardware failure (5.4%), vascular injury (2.5%), and neurological injury (1.0%). This result was consistent with that of a previous study (52). Considering the anatomy of the psoas muscle (complicated nerve plexuses), it can be prone to damage these nerve plexuses during the transpsoas approach. Of course, the incidence of thigh pain/numbness was lower than that in those traditional procedures, such as LLIF (53). Most of these complications are transient and can recover during the follow-up period. While, the most common complication of MI-TLIF was hardware failure (3.41%), and other main complications included neurological injury (1.0%), wound infection (0.85%), and thigh pain/numbness (0.61%). According to a study of Zeng et al. (28), endplate injury, cage subsidence, and shifting can be induced by multiple factors, such as over-distraction and aggressive endplate reaming. Besides, obesity and osteoporosis could also partially explain the endplate-related complications in these two surgery techniques (54). Furthermore, it had been reported that posterior fixation, which can enhance segmental stability, should be applied in case of endplate injury (55). Overall, these surgical procedures should be selected properly, and imaging guidance with high accuracy may be helpful.
There are several highlights in this meta-analysis, such as containing the latest studies in the last three years and analyzing the complications in detail. However, some limitations should also be mentioned. Firstly, most of these included studies are short of a controlled group, and hence it is difficult to directly compare the effect or complications between OLIF and MI-TLIF. Besides, posterior fixation was applied in some patients, which may affect the reliability of the conclusion.
The OLIF and MI-TLIF can achieve similar results in the length of hospital stay, DH, and VAS. OLIF is superior to MI-TLIF in respect of operative time, blood loss, LLA restoration, and ODI scores. Moreover, although the incidence of complications is similar between OLIF and MI-TLIF, there are significant differences in the main complications between both surgical techniques.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
JW: Conceptualization, Methodology, Writing-Original draft preparation; JL: Data curation, Writing- Original draft preparation; YZ: Data collecting and analysis; YH and LZ Supervision. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Diebo BG, Shah NV, Boachie-Adjei O, Zhu F, Rothenfluh DA, Paulino CB, et al. Adult spinal deformity. Lancet. (2019) 394:160–72. doi: 10.1016/S0140-6736(19)31125-0
2. Lenz M, Mohamud K, Bredow J, Oikonomidis S, Eysel P, Scheyerer MJ. Comparison of different approaches in lumbosacral spinal fusion surgery: a systematic review and meta-analysis. Asian Spine J. (2022) 16(1):141–9. doi: 10.31616/asj.2020.0405
3. Asil K, Yaldiz C. Retrospective comparison of radiological and clinical outcomes of PLIF and TLIF techniques in patients who underwent lumbar spinal posterior stabilization. Medicine (Baltimore). (2016) 95:e3235. doi: 10.1097/MD.0000000000003235
4. Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. (2015) 1:2–18. doi: 10.3978/j.issn.2414-469X.2015.10.05
5. Ohtori S, Mannoji C, Orita S, Yamauchi K, Eguchi Y, Ochiai N, et al. Mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for degenerated lumbar spinal kyphoscoliosis. Asian Spine J. (2015) 9:565–72. doi: 10.4184/asj.2015.9.4.565
6. Cui JM, Wang JR, Zheng ZM, Liu H, Wang H, Li ZM. Lateral-anterior lumbar interbody fusion (LaLIF) for lumbar degenerative disease: technical notes, surgical system, and mid-term outcomes. J Orthop Translat. (2021) 28:12–20. doi: 10.1016/j.jot.2020.12.001
7. Foley KT, Lefkowitz MA. Advances in minimally invasive spine surgery. Clin Neurosurg. (2002) 49:499–517. doi: 10.1007/3-540-29490-2_1
8. Silvestre C, Mac-Thiong JM, Hilmi R, Roussouly P. Complications and morbidities of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lumbar interbody fusion in 179 patients. Asian Spine J. (2012) 6:89–97. doi: 10.4184/asj.2012.6.2.89
9. Wells G, Shea B, O’Connell J. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Health Research Institute Web site 7 (2014).
10. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
11. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
12. Abe K, Orita S, Mannoji C, Motegi H, Aramomi M, Ishikawa T, et al. Perioperative complications in 155 patients who underwent oblique lateral interbody fusion surgery: perspectives and indications from a retrospective, multicenter Survey. Spine (Phila Pa 1976). (2017) 42:55–62. doi: 10.1097/BRS.0000000000001650
13. Chen YL, Zhu ZH, Wang YK, Fan SW, Fang XQ, Wan SL, et al. Effects of oblique lateral interbody fusion and transforaminal lumbar interbody fusion for lordosis correction in degenerative lumbar diseases. Zhonghua Yi Xue Za Zhi. (2018) 98:1990–5. doi: 10.3760/cma.j.issn.0376-2491.2018.25.005
14. Cho MS, Seo EM. Efficacy and radiographic analysis of oblique lumbar interbody fusion in treating lumbar degenerative spondylolisthesis with sagittal imbalance. Neurosurg Rev. (2021) 44(4):2181-9. doi: 10.1007/s10143-020-01390-4
15. Heo DH, Kim JS. Clinical and radiological outcomes of spinal endoscopic discectomy-assisted oblique lumbar interbody fusion: preliminary results. Neurosurg FocuS. (2017) 43:E13. doi: 10.3171/2017.5.FOCUS17196
16. Jin C, Jaiswal MS, Jeun SS, Ryu KS, Hur JW, Kim JS. Outcomes of oblique lateral interbody fusion for degenerative lumbar disease in patients under or over 65 years of age. J Orthop Surg Res. (2018) 13:38. doi: 10.1186/s13018-018-0740-2
17. Sato J, Ohtori S, Orita S, Yamauchi K, Eguchi Y, Ochiai N, et al. Radiographic evaluation of indirect decompression of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for degenerated lumbar spondylolisthesis. Eur Spine J. (2017) 26:671–8. doi: 10.1007/s00586-015-4170-0
18. Kim KT, Jo DJ, Lee SH, Seo EM. Oblique retroperitoneal approach for lumbar interbody fusion from L1 to S1 in adult spinal deformity. Neurosurg Rev. (2018) 41:355–63. doi: 10.1007/s10143-017-0927-8
19. Li R, Shao X, Li X, Liu Y, Jiang W. Comparison of clinical outcomes and spino-pelvic sagittal balance in degenerative lumbar spondylolisthesis: minimally invasive oblique lumbar interbody fusion (OLIF) versus transforaminal lumbar interbody fusion (TLIF). Medicine (Baltimore). (2021) 100:e23783. doi: 10.1097/MD.0000000000023783
20. Liu J, He Y, Huang B, Zhang X, Shan Z, Chen J, et al. Reoccurring discogenic low back pain (LBP) after discoblock treated by oblique lumbar interbody fusion (OLIF). J Orthop Surg Res. (2020) 15:22. doi: 10.1186/s13018-020-1554-6
21. Mun HY, Ko MJ, Kim YB, Park SW. Usefulness of oblique lateral interbody fusion at L5-S1 level compared to transforaminal lumbar interbody fusion. J Korean Neurosurg Soc. (2020) 63:723–9. doi: 10.3340/jkns.2018.0215
22. Poppenborg P, Liljenqvist U, Gosheger G, Schulze BA, Lampe L, Schmeil S, et al. Complications in TLIF spondylodesis-do they influence the outcome for patients? A prospective two-center study. Eur Spine J. (2021) 30(5):1320–8. doi: 10.1007/s00586-020-06689-w
23. Sheng S, Geng Y, Zhou K, Wu A, Wang X, Ni W. Minimally invasive surgery for degenerative spondylolisthesis: transforaminal or oblique lumbar interbody fusion. J Comp Effect Res. (2020) 9:45–51. doi: 10.2217/cer-2019-0055
24. Fujibayashi S, Hynes RA, Otsuki B, Kimura H, Takemoto M, Matsuda S. Effect of indirect neural decompression through oblique lateral interbody fusion for degenerative lumbar disease. Spine (Phila Pa 1976). (2015) 40:E175–82. doi: 10.1097/BRS.0000000000000703
25. Xi Z, Burch S, Chang C, Ruan H, Eichler CM, Mummaneni PV, et al. Anterior lumbar interbody fusion (ALIF) versus oblique lateral interbody fusion (OLIF) at L5-S1: a comparison of two approaches to the lumbosacral junction. Neurosurgery. (2019) 661:83. doi: 10.1016/j.jocn.2020.10.043
26. Yang Z, Chang J, Sun L, Chen C, Feng H. Comparing oblique lumbar interbody fusion with lateral screw fixation and transforaminal full-endoscopic lumbar discectomy (OLIF-TELD) and posterior lumbar interbody fusion (PLIF) for the treatment of adjacent segment disease. Biomed Res Int. (2020) 2020:4610128. doi: 10.1155/2020/4610128
27. Zairi F, Sunna TP, Westwick HJ, Weil AG, Wang Z, Boubez G, et al. Mini-open oblique lumbar interbody fusion (OLIF) approach for multi-level discectomy and fusion involving L5-S1: preliminary experience. Orthop Traumatol Surg Res. (2017) 103:295–9. doi: 10.1016/j.otsr.2016.11.016
28. Zeng ZY, Xu ZW, He DW, Zhao X, Ma WH, Ni WF, et al. Complications and prevention strategies of oblique lateral interbody fusion technique. Orthop Surg. (2018) 10:98–106. doi: 10.1111/os.12380
29. Fan G, Wu X, Yu S, Sun Q, Guan X, Zhang H, et al. Clinical outcomes of posterior lumbar interbody fusion versus minimally invasive transforaminal lumbar interbody fusion in three-level degenerative lumbar spinal stenosis. Biomed Res Int. (2016) 2016:9540298. doi: 10.1155/2016/9540298
30. Luo Z, Rao H, Huang D, Li G, Liu C, Dong S, et al. Comparison of minimally invasive using a tubular retraction system versus open transforaminal lumbar interbody fusion for the treatment of lumbar degenerative diseases. Zhonghua Yi Xue Za Zhi. (2015) 95:2681–5. doi: 10.3760/cma.j.issn.0376-2491.2015.33.007
31. Bin ARH, Dhoke P, Tay KS, Yeo W, Yue WM. Single-level minimally invasive transforaminal lumbar interbody fusion provides sustained improvements in clinical and radiological outcomes up to 5 years postoperatively in patients with neurogenic symptoms secondary to spondylolisthesis. Asian Spine J. (2017) 11:204–12. doi: 10.4184/asj.2017.11.2.204
32. Lee KH, Yue WM, Yeo W, Soeharno H, Tan SB. Clinical and radiological outcomes of open versus minimally invasive transforaminal lumbar interbody fusion. Eur Spine J. (2012) 21:2265–70. doi: 10.1007/s00586-012-2281-4
33. Lee WC, Park JY, Kim KH, Kuh SU, Chin DK, Kim KS, et al. Minimally invasive transforaminal lumbar interbody fusion in multilevel: comparison with conventional transforaminal interbody fusion. World Neurosurg. (2016) 85:236–43. doi: 10.1016/j.wneu.2015.09.009
34. Min SH, Yoo JS. The clinical and radiological outcomes of multilevel minimally invasive transforaminal lumbar interbody fusion. Eur Spine J. (2013) 22:1164–72. doi: 10.1007/s00586-012-2619-y
35. Park Y, Ha JW, Lee YT, Sung NY. Minimally invasive transforaminal lumbar interbody fusion for spondylolisthesis and degenerative spondylosis: 5-year results. Clin Orthop Relat Res. (2014) 472:1813–23. doi: 10.1007/s11999-013-3241-y
36. Parker SL, Adogwa O, Bydon A, Cheng J, McGirt MJ. Cost-effectiveness of minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis associated low-back and leg pain over two years. World Neurosurg. (2012) 78:178–84. doi: 10.1016/j.wneu.2011.09.013
37. Sulaiman WA, Singh M. Minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis grades 1-2: patient-reported clinical outcomes and cost-utility analysis. Ochsner J. (2014) 14:32–7. doi: 10.1016/j.wneu.2013.01.041
38. Wang J, Zhou Y. Perioperative complications related to minimally invasive transforaminal lumbar fusion: evaluation of 204 operations on lumbar instability at single center. SPINE J. (2014) 14:2078–84. doi: 10.1016/j.spinee.2013.12.016
39. Wu AM, Hu ZC, Li XB, Feng ZH, Chen D, Xu H, et al. Comparison of minimally invasive and open transforaminal lumbar interbody fusion in the treatment of single segmental lumbar spondylolisthesis: minimum two-year follow up. Ann Transl Med. (2018) 6:105. doi: 10.21037/atm.2018.02.11
40. Zhao Y, Liang Y, Mao K. Radiographic and clinical outcomes following MIS-TLIF in patients with adult lumbar degenerative scoliosis. J Orthop Surg Res. (2018) 13:93. doi: 10.1186/s13018-018-0764-7
41. Wang HW, Hu YC, Wu ZY, Wu HR, Wu CF, Zhang LS, et al. Minimally invasive transforaminal lumbar interbody fusion and unilateral fixation for degenerative lumbar disease. Orthop Surg. (2017) 9:277–83. doi: 10.1111/os.12345
42. Patel NP, Birch BD, Dement SE, Elbert GA. The mini-open anterolateral approach for degenerative thoracolumbar disease. Clin Neurol Neurosurg. (2010) 112:853–7. doi: 10.1016/j.clineuro.2010.07.008
43. Tu Z, Li L, Wang B, Li Y, Lv G, Dai Y. Stand-alone anterolateral interbody fusion versus extended posterior fusion for symptomatic adjacent-segment degeneration: a retrospective study of 2 Years’ follow-up. World Neurosurg. (2018) 115:e748–55. doi: 10.1016/j.wneu.2018.04.165
44. Sembrano JN, Tohmeh A, Isaacs R. Two-year comparative outcomes of MIS lateral and MIS transforaminal interbody fusion in the treatment of degenerative spondylolisthesis: part I: clinical findings. Spine (Phila Pa 1976). (2016) 41(Suppl 8):S123–32. doi: 10.1097/BRS.0000000000001471
45. Keorochana G, Setrkraising K, Woratanarat P, Arirachakaran A, Kongtharvonskul J. Clinical outcomes after minimally invasive transforaminal lumbar interbody fusion and lateral lumbar interbody fusion for treatment of degenerative lumbar disease: a systematic review and meta-analysis. Neurosurg Rev. (2018) 41:755–70. doi: 10.1007/s10143-016-0806-8
46. Hammad A, Wirries A, Ardeshiri A, Nikiforov O, Geiger F. Open versus minimally invasive TLIF: literature review and meta-analysis. J Orthop Surg Res. (2019) 14(1):229. doi: 10.1186/s13018-019-1266-y
47. Lau D, Lee JG, Han SJ, Lu DC, Chou D. Complications and perioperative factors associated with learning the technique of minimally invasive transforaminal lumbar interbody fusion (TLIF). J Clin Neurosci. (2011) 18:624–7. doi: 10.1016/j.jocn.2010.09.004
48. Hey HW, Hee HT. Open and minimally invasive transforaminal lumbar interbody fusion: comparison of intermediate results and complications. Asian Spine J. (2015) 9:185–93. doi: 10.4184/asj.2015.9.2.185
49. Jin C, Xie M, He L, Xu W, Han W, Liang W, et al. Oblique lumbar interbody fusion for adjacent segment disease after posterior lumbar fusion: a case-controlled study. J Orthop Surg Res. (2019) 14:216. doi: 10.1186/s13018-019-1276-9
50. Kim MC, Chung HT, Kim DJ, Kim SH, Jeon SH. The clinical and radiological outcomes of minimally invasive transforaminal lumbar interbody single level fusion. Asian Spine J. (2011) 5:111–6. doi: 10.4184/asj.2011.5.2.111
51. Li HM, Zhang RJ, Shen CL. Radiographic and clinical outcomes of oblique lateral interbody fusion versus minimally invasive transforaminal lumbar interbody fusion for degenerative lumbar disease. World Neurosurg. (2019) 122:e627–38. doi: 10.1016/j.wneu.2018.10.115
52. Segawa T, Koga H, Oshina M, Ishibashi K, Takano Y, Iwai H, et al. Clinical evaluation of microendoscopy-assisted oblique lateral interbody fusion. Medicina (Kaunas). (2019)14(1):229. doi: 10.3390/medicina57020135
53. Li HM, Zhang RJ, Shen CL. Differences in radiographic and clinical outcomes of oblique lateral interbody fusion and lateral lumbar interbody fusion for degenerative lumbar disease: a meta-analysis. BMC Musculoskelet Disord. (2019) 20:582. doi: 10.1186/s12891-019-2972-7
54. Wu J, Ge T, Zhang N, Li J, Tian W, Sun Y. Posterior fixation can further improve the segmental alignment of lumbar degenerative spondylolisthesis with oblique lumbar interbody fusion. BMC Musculoskelet Disord. (2021) 22:218. doi: 10.1186/s12891-021-04086-y
Keywords: degenerative lumbar disease, OLIF, MI-TLIF, meta-analysis, systematic review
Citation: Wang J, Liu J, Hai Y, Zhang Y and Zhou L (2022) OLIF versus MI-TLIF for patients with degenerative lumbar disease: Is one procedure superior to the other? A systematic review and meta-analysis. Front. Surg. 9:1014314. doi: 10.3389/fsurg.2022.1014314
Received: 8 August 2022; Accepted: 22 September 2022;
Published: 13 October 2022.
Edited by:
Xiaojian Wang, Shanxi Provincial People’s Hospital, ChinaReviewed by:
Gao Fei, Affiliated Hospital of Hebei University, China© 2022 Wang, Liu, Hai, Zhang and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yong Hai eW9uZy5oYWlAY2NtdS5lZHUuY24= Lijin Zhou ZG9jdG9yemhvdWxpamluQDE2My5jb20=
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.