
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Surg. , 17 January 2023
Sec. Orthopedic Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.1008358
 Ahmad Alhaskawi1,†
Ahmad Alhaskawi1,† Haiying Zhou1,†
Haiying Zhou1,† Yanzhao Dong1
Yanzhao Dong1 Jingtian Lai2
Jingtian Lai2 Zewei Wang2
Zewei Wang2 Sohaib Hasan Abdullah Ezzi3
Sohaib Hasan Abdullah Ezzi3 Vishnu Goutham Kota2
Vishnu Goutham Kota2 Mohamed Hasan Abdulla Hasan Abdulla2
Mohamed Hasan Abdulla Hasan Abdulla2 Zhenyu Sun1
Zhenyu Sun1 Hui Lu1*
Hui Lu1*
An intraosseous epidermoid cyst at the distal phalanx of the index finger is extremely rare. These cysts are asymptomatic unless ruptured, severely infected, or transformed into malignant squamous cell carcinoma. We present a case of a single clubbing finger in an adult diagnosed with an intraosseous epidermoid cyst in the distal phalanx of the left index finger with no history of pulmonary or cardiovascular diseases. Preoperative MRI showed an expansile lytic lesion with a sclerotic margin. Histopathological examination indicates that there is keratinous cell debris in the cyst with a wall of stratified squamous epithelium, which was the key to the correct diagnosis of an intraosseous epidermoid cyst. Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Intraosseous epidermoid cysts are also known as pseudotumors or keratin cysts. They were first reported in 1923 (1). They are rare benign bone lesions that occur mostly in the skull, face, neck, toe, and finger phalanges, especially the distal phalanges (2). It is quite challenging to diagnose this disease as it has no specificity in clinical and imaging presentations. An expansile lytic lesion with a sclerotic margin is usually shown in a radiological image (3). However, this radiological feature is shared with other diseases, such as enchondroma, giant cell tumors, subungual melanoma, aneurysmal bone cysts, and chondroma (4, 5). Therefore, a correct diagnosis is usually achieved by histopathologic examination (6, 7). A clubbing finger or Hippocratic finger is a finger deformity characterized by enlargement of the fingertips and the curved nails around the fingertips, which often signify poor cardiopulmonary function in patients (8). However, in this article, we report the first case of a single clubbing finger in an adult patient as a result of an infected intraosseous epidermoid cyst in the distal phalanx of the left index finger.
In 2021, a 50-year-old female patient came to our outpatient department complaining of severe pain in the left index finger. Physical examination showed obvious swelling, redness, and tenderness on the eponychium of the left index finger, with nail root deformity, which looked similar to a clubbing finger, and the remaining fingers appeared normal (Figure 1). She denied a history of pulmonary and cardiovascular diseases except for a history of trauma in that she injured her left index finger 3 years ago and then the finger enlarged gradually and painlessly for the first few months after the injury. During this period, the fingernail of the left index finger fell off naturally twice. Six months ago, the patient visited a local hospital complaining of pain and intermittent infection, where the doctor considered the possibility of paronychia and gave her an antibiotic (celixin, the exact dosage, and usage are unknown) as the proper treatment. Unfortunately, the patient's pain was only relieved for a short period and became worse later on. Therefore, she visited our outpatient department for further treatment. After finishing the main outpatient check-up, a tumor at a distal phalanx of the left index finger was considered; thereby, the patient was hospitalized, and further examinations were required.

Figure 1. Preoperative view showing the swelling, redness, and tenderness on the eponychium of the left index finger.
After admission, slightly limited mobility during flexion and circulation of the affected finger was observed and all blood tests were normal. Magnetic resonance imaging (MRI) revealed a lucent lytic lesion involving the distal phalanx that led to cortical thinning and bone expansion (Figure 2); thus, a tumor-like lesion was considered. Given her chronic severe pain and well-defined lesions on imaging, surgical excision was performed. After applying brachial plexus block anesthesia, we made a fish mouth flap incision in the distal phalanx of the left index finger, which allowed us to see the thinned phalangeal cortex and a cyst. A window was opened in the thinned cortex, where a creamy material was released, and then we performed curettage. After radical debridement, the skin was adjusted and the nail bed was sutured (Figure 3). Postoperative histopathological analysis of the lesion showed a cyst that contained a cavity of keratinized material and a wall of stratified squamous cells. These findings confirmed that the patient had an intraosseous epidermoid cyst (Figure 4), which previously had been misdiagnosed. Postoperative recovery was uneventful; the patient was allowed to have full motion of the left index finger 3 days after surgery. After 6 months of surgery, bone regeneration was noted radiographically and the patient was able to do full-weight exercises. After 1 year of clinical and radiological follow-up, the patient shows no sign of recurrence.
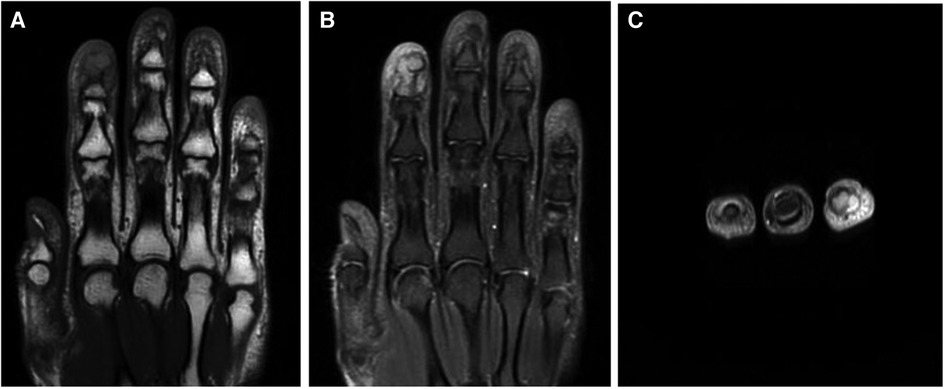
Figure 2. MRI of the distal phalanx of the left index finger. T1 (A) and T2 (B,C) showing a well-defined osteolytic lesion with a clear boundary.

Figure 3. Creamy material removed from the cyst of the left index finger during the intraoperative curettage.
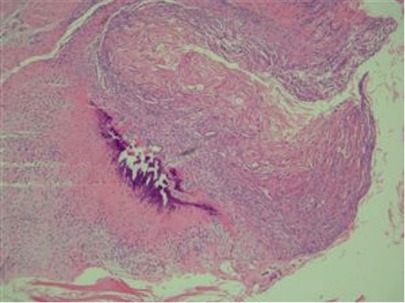
Figure 4. Histopathological examination revealing a wall of stratified squamous epithelium and keratinized material inside a cyst.
An intraosseous epidermal cyst or a squamous epithelial cyst is a lesion with keratinous debris surrounded by a wall of squamous epithelium in a bone. The cysts arise more frequently in men than women, and the left middle finger is involved most frequently (9). It is clinically presented as a painless, reddish, tender, and swollen lesion (2, 10, 11).
Many researchers have debated the real etiology of intraosseous epidermal cysts. The majority of previous studies found that trauma, such as crush injuries, is the common cause, and the epithelial cells could be embedded into the bone to form epidermoid cysts (11). Other studies mentioned congenital reasons why the inclusion of ectodermal tissue occurs during fetal development (12). All these etiologies ultimately point to the possibility of iatrogenic alteration of the epithelial cells within the bone, which leads to the formation of epidermoid cysts (11, 13).
Intraosseous epidermoid cysts are generally difficult to get diagnosed, depending on clinical examination and radiological findings, because their appearances and other characteristics are similar to those of other diseases, such as enchondroma, giant cell tumors, synovial cysts, aneurysmal bone cysts, and gout (14). Radiological imaging of an intraosseous epidermoid cyst shows a well-defined lytic lesion with circumscribed margin in a bone (2, 4). This imaging evidence lacks the specificity required for the definitive diagnosis of an intraosseous epidermoid cyst. Therefore, a histopathological test of the lesion tissue is the final resort to confirm the diagnosis of intraosseous epidermoid cysts among the various differential diagnoses. The histopathological analysis presents that an intraosseous epidermoid cyst contains keratinous cell debris surrounded by a wall of the stratified squamous epithelium (2). The most reliable treatments for intraosseous epidermoid cysts are curettage, which avoids recurrence, and bone graft, which reconstructs the wound (3, 15).
The noteworthy point found in our patient is that only her affected finger, a single finger, showed the clubbing finger changes. Clubbing finger changes often appear in multiple fingers and are a sign of multiple severe diseases, such as lung cancer, cystic fibrosis, sarcoidosis, cirrhosis, and cardiovascular diseases, which occur gradually over the years (16–19). Single clubbing finger occurs extremely rarely. A few cases have been reported, and all of them were linked to enchondroma, a type of benign bone tumor (19–21), except one formed as a result of superficial acral fibromyxoma (22) (Table 1).
The mechanism of the clubbing finger remains ambiguous. A few theories, such as vascular endothelial growth factor (VEGF) (23), platelet-derived growth factor (PDGF) (24), and neurocirculatory reflex (25), are postulated to be participating in the formation of clubbing finger. Clubbing does not occur suddenly, and it has different stages. It starts as periungual erythema with a soft sensation, and then the angle between the proximal nail fold and the nail bed will increase. Clubbing causes the nail to be convex in shape, the skin at the fingertip to be shiny, and the possibility of hyperextension of the interphalangeal joint (26).
We here present the first case of a single clubbing finger associated with intraosseous epidermoid cysts. This case report intends to inspire clinicians that the differential diagnosis of the clubbing finger, especially in the case of a single clubbing finger, should include intraosseous epidermoid cysts.
The original contributions presented in the study are included in the article/Supplementary Material; further inquiries can be directed to the corresponding author/s.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
HL, ZW, JL, VK: designed the study, collected data, and analyzed the results. YD, HZ, MA, SE, ZS, and AA drafted the manuscript. All authors contributed to the article and approved the submitted version.
The study was funded by the Zhejiang Provincial Natural Science Foundation (grant number LS21H060001), Alibaba Youth Studio Project (grant number ZJU-032), and Zhejiang Province Medical and Health Science and Technology Program (grant numbers 2022KY1455 and 2022RC136). The funding bodies had no role in the design of the study; in the collection, analysis, and interpretation of data; and in drafting the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Hammann VI. Traumatische epithelcysten an den fingerknochen. Deutsche Ztschrift Für Chirurgie. (1930) 223(4–5):308–17.
2. Simon K, Leithner A, Bodo K, Windhager R. Intraosseous epidermoid cysts of the hand skeleton: a series of eight patients. J Hand Surg Eur. (2011) 36(5):376–8. doi: 10.1177/1753193411401987
3. Belusa M. Intra-osseous epidermoid cyst. Handchir Mikrochir Plast Chir. (1991) 23(4):200–1.1937184
4. Kozlowski K, Azouz EM, Campbell J, Marton D, Morris L, Padovani J, Sprague P, Beluffi G, Berzero GF, Cherubino P. Primary bone tumours of the hand. Report of 21 cases. Pediatr Radiol. (1988) 18(2):140–8. doi: 10.1007/BF02387558
5. Patel K, Bhuiya T, Chen S, Kenan S, Kahn L. Epidermal inclusion cyst of phalanx: a case report and review of the literature. Skeletal Radiol. (2006) 35(11):861–3. doi: 10.1007/s00256-005-0058-0
6. Carroll RE. Epidermoid (epithelial) cyst of the hand skeleton. Am J Surg. (1953) 85(3):327–34. doi: 10.1016/0002-9610(53)90617-5
7. Musharrafieh RS, Tawil AN, Saghieh SS, Macari G, Atiyeh BS. Epidermoid cyst of the thumb. Orthopedics. (2002) 25(8):862–3. doi: 10.3928/0147-7447-20020801-20
8. Spicknall KE, Zirwas MJ, English JC 3rd. Clubbing: an update on diagnosis, differential diagnosis, pathophysiology, and clinical relevance. J Am Acad Dermatol. (2005) 52(6):1020–8. doi: 10.1016/j.jaad.2005.01.006
9. Nakajo M, Ohkubo K, Nandate T, Nagano Y, Shirahama H, Nakajo M. Intraosseous epidermal cyst of the distal phalanx of the thumb: radiographic and magnetic resonance imaging findings. Radiat Med. (2005) 23(2):128–32. PMID: 15827532
10. Fisher ER, Gruhn J, Skerrett P. Epidermal cyst in bone. Cancer. (1958) 11(3):643–8. doi: 10.1002/1097-0142(195805/06)11:3%3C643::AID-CNCR2820110328%3E3.0.CO;2-O
11. Schajowicz F, Aiello CL, Slullitel I. Cystic and pseudocystic lesions of the terminal phalanx with special reference to epidermoid cysts. Clin Orthop Relat Res. (1970) 68:84–92. doi: 10.1097/00003086-197001000-00014
12. Niccoli C, Mambelli V. Intra-osseous epithelial cyst of the phalanx. Arch Putti Chir Organi Mov. (1978) 29:395–404.757494
13. Hamad AT, Kumar A, Anand Kumar C. Intraosseous epidermoid cyst of the finger phalanx: a case report. J Orthop Surg. (2010) 2010:340–2. doi: 10.1177/230949900601400322
14. Ruchelsman DE, Laino DK, Chhor KS, Steiner GC, Kenan S. Digital intraosseous epidermoid inclusion cyst of the distal phalanx. J Hand Microsurg. (2010) 2(1):24–7. doi: 10.1007/s12593-010-0001-z
15. Kurosawa K, Kobayashi R, Takagishi K. Distal phalangeal reconstruction for recurrent intraosseous epidermoid cyst of the finger—a case report. Hand Surg. (2011) 16(3):375–7. doi: 10.1142/S0218810411005734
16. Burcovschii S, Aboeed A. Nail clubbing, in StatPearls. Treasure island (FL): StatPearls Publishing LLC (2022).
17. Yanardag H, Tetikkurt C, Bilir M. Finger clubbing and cirrhosis in a sarcoidosis patient. Monaldi Arch Chest Dis. (2019) 89(3):1–4.
18. Epstein O, Dick R, Sherlock S. Prospective study of periostitis and finger clubbing in primary biliary cirrhosis and other forms of chronic liver disease. Gut. (1981) 22(3):203–6. doi: 10.1136/gut.22.3.203
19. Hui Lu, Qiang Chen, Hui Shen, Hu Yang, Weifeng Ji. Enchondroma in the distal phalanx of the thumb with infection resulting in clubbing felon. Hangzhou China: International Journal of Clinical and Experimental Medicine (IJCEM) (2018)
20. Nishio J, Naito M. Single clubbed finger caused by an enchondroma of the distal phalanx: an unusual clinical presentation. Hand Surg. (2012) 17(3):405–8. doi: 10.1142/S0218810412720422
21. Coto-Segura P, Mallo-Garcia S, Braña A, Santos-Juanes J. Single hippocratic (clubbed) finger revealing an underlying enchondroma. J Am Acad Dermatol. (2008) 59(2 Suppl 1):S34–5. doi: 10.1016/j.jaad.2007.07.041
22. Crestani L, Fasciani IA, Kakizaki P, Valente NYS. Case for diagnosis. Single-digit clubbing. An Bras Dermatol. (2020) 95(4):524–6. doi: 10.1016/j.abd.2020.01.006
23. Atkinson S, Fox SB. Vascular endothelial growth factor (VEGF) – a and platelet-derived growth factor (PDGF) play a central role in the pathogenesis of digital clubbing. J Pathol. (2004) 203(2):721–8. doi: 10.1002/path.1565
24. Dickinson CJ, Martin JF. Megakaryocytes and platelet clumps as the cause of finger clubbing. Lancet. (1987) 2(8573):1434–5. doi: 10.1016/S0140-6736(87)91132-9
Keywords: intraosseous epidermoid cyst, distal phalanx, clubbing, single clubbing finger, enchondroma
Citation: Alhaskawi A, Zhou H, Dong Y, Lai J, Wang Z, Hasan Abdullah Ezzi S, Goutham Kota V, Hasan Abdulla Hasan Abdulla M, Sun Z and Lu H (2023) The first case report of an intraosseous epidermoid cyst in the distal phalanx of the index finger with infection resulting in single clubbing finger: A case report and review of the literature. Front. Surg. 9:1008358. doi: 10.3389/fsurg.2022.1008358
Received: 31 July 2022; Accepted: 27 December 2022;
Published: 17 January 2023.
Edited by:
Berardo Di Matteo, Humanitas Research Hospital, ItalyReviewed by:
Ilker Sengul, Giresun University, Türkiye© 2023 Alhaskawi, Zhou, Dong, Lai, Wang, Hasan Abdullah Ezzi, Goutham Kota, Hasan Abdulla Hasan Abdulla, Sun and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hui Lu aHVpbHVAemp1LmVkdS5jbg==
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.