- 1Department of Obstetrics and Gynecology, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou, China
- 2Clinical Research Design Division, Clinical Research Center, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou, China
Purpose: Heterotopic pregnancy (HP) is a rare disease with the coexistence of an intrauterine and ectopic embryos. There is no consensus on the optimal treatment of HP at present. This research aimed to compare the perioperative and pregnancy outcomes of laparoscopic (LA) and open approach (OA) in patients with HP after embryo transfer.
Methods: Women with HP receiving surgical treatment (LA or OA) were retrospectively recruited in this study between October 2006 and December 2020. The demographic, perioperative and obstetric data were collected and compared between LA and OA group.
Results: Totally, 86 patients were included in this study. Among these patients, 62 underwent LA and 24 underwent OA. There was an increase in the adoption of LA between the 2006–2012 period and the 2013–2020 period [25% (6/24) vs. 90% (56/62), p < 0.001]. Compared with OA, patients treated by LA had much less blood loss [20 (10–50) vs. 30 (20–50) ml, p = 0.036] and fewer days of hospital stay [5.0 (4.0–7.3) vs. 9.5 (7–15.3) days, p < 0.001], but a relatively higher cost (15,580 ± 3196¥ vs. 11,717 ± 3820¥, p < 0.001). During the laparoscopic procedure, no one needed to be converted to open surgery. However, the rates of first trimester miscarriage, preterm, cesarean section, birth weight, 1- and 5-min Apgar were similar between LA and OA group (all p > 0.05).
Conclusions: Compared with open approach, laparoscopy was shown to provide a comparable pregnancy outcomes and a better performance on perioperative outcomes in the treatment of HP patients with embryo transfer.
Introduction
Heterotopic pregnancy (HP) is defined as the coexistence of an intrauterine and ectopic embryos (1). HP rarely occurs with an incidence of 1/7,000–1/30,000 of natural conception (2, 3). However, the risk of HP is substantially increased in women with assisted reproductive techniques (ART). The prevalence of HP in women with ART ranged from 1/100 to 1/500 (4, 5). Compared with those with ectopic pregnancy (EP), women with HP are at a greater risk of hypovolemic shock (1). The timely and effective treatment for HP is necessary to ensure the safety of the mother and intrauterine fetus (6, 7).
Currently, there are no clinical guidelines or expert consensus to provide the standard management recommendation for HP due to its rarity. Surgery has been the most common treatment of choice in patients with HP, especially for those with unstable clinical sign or EP ruptures (8–11). Open approach (OA) is the traditional surgical method for HP. With the advance of technology, laparoscopic approach (LA) has attracted more attention from clinicians because of its better visualization and exposure, shorter hospital stays, and less suffering (12, 13). However, the question about the preferred surgical approach for HP patients remains unsolved. Only few case-series and case-report studies have demonstrated that LA could be safely performed in HP patients (10, 11, 14), even for heterotopic interstitial or cornual pregnancies (15–18). In contrast, several studies have found that LA would increase the risk of fetal loss in HP patients (7, 19). The evidence in previous studies were limited by small sample size and lack of comparison between LA and OA in perioperative and pregnancy outcomes of HP patients.
Therefore, the aim of this study was to compare the safety and efficacy of LA and OA in patients with HP after embryo transfer.
Materials and methods
Patients
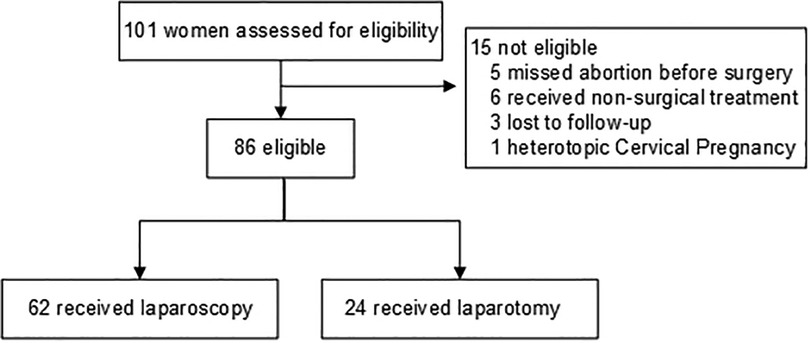
This retrospective cohort study was conducted at Sun Yat-Sen Memorial Hospital between October 2006 to December 2020. Women with HP following embryo transfer and receiving surgical treatment (LA or OA) were enrolled in this study. The diagnosis of HP was confirmed based on both transvaginal ultrasonography (TVS) and histopathological examination. Patients will be excluded if the intrauterine fetal was failed before surgery, or diagnosed with non-tubal HP or lost to follow-up without the perioperative or obstetric data. There were 101 women diagnosed with HP following embryo transfer, among which, 15 patients were excluded. Finally, 86 patients were included in this study. The details of selection is shown in Figure 1.
The study has obtained ethical approval from local ethical committee (Approval number: SYSEC-KY-KS-2020–044). Informed consent was obtained from each patient after explaining the benefits, harms, and possible morbidities of surgery in detail.
Surgical procedures
The surgical indications for HP in our department were hemodynamic instability, signs of intraperitoneal bleeding, suspected rupture of EP (sudden or persistent abdominal pain) or detectable fetal heartbeat of EP, or an ectopic mass diameter larger than 3 cm or progressively increasing.
Surgeries were performed by surgeons with more than eight years of surgical experience under general anesthesia or spinal anesthesia. Vital signs of patients such as blood pressure, electrocardiogram, blood oxygen saturation and end-tidal CO2 pressure were constantly monitored. Laparoscopic and open resections of ectopic mass were performed following the same principles and procedures. During laparoscopy, the abdomen was inflated with CO2 while maintaining a pneumoperitoneum pressure of 10–13 mmHg. Salpingectomy was conducted for tubal non-interstitial pregnancy, and cornuostomy for interstitial pregnancy with harmonic scissors. In order to control bleeding of interstitial surgery, a Vicryl loop was sometimes placed laterally to the pregnancy as reported by Soriano et al. (20). The cornual defect was repaired with simple interrupted stitches using a 2–0 synthetic, absorbable, Vicryl sutures (Ethicon, lnc) to reduce the risk of uterine rupture during the ongoing pregnancy.
Data collection
The data of demographic and clinical characteristics at baseline, perioperative and obstetrical outcomes of all patients were collected via medical records or telephone follow-up. The baseline characteristics included age (years), gestational age (days), indication for ART (with vs. without tubal factor), clinical manifestations (vaginal bleeding, abdominal pain), heartbeat of Intrauterine pregnancy (IUP) (with vs. without), site of EP (interstitial vs. non-interstitial), abortion history (yes vs. no), history of pelvic adhesions (yes vs. no) and surgical history (yes vs. no).
The operative time, blood loss, preoperative and postoperative hemoglobin levels were recognized as perioperative outcomes. Besides, the record of blood transfusion, the conversion from laparoscopy to open surgery, and hospital stays were also collected from medical records. Early miscarriage was defined as first trimester fetal loss before gestational age of 14 weeks. Among patients with live birth, delivery mode (cesarean section vs. vaginal deliver), postpartum hemorrhage (yes vs. no), the birth weight, and 1 min and 5 min Apgar for infants were also considered as obstetrical outcomes.
Statistical analysis
Continuous variables were presented as mean with standard deviation, or median with quartile according to the results of the Kolmogorov–Smirnov test and categorical data as numbers (percentages). Chi-square test or Fisher exact test for categorical variables (treatment period, abortion history, pelvic adhesions, surgical history, history of EP, indication for ART, clinical manifestations, site of EP, yolk sac of EP and heartbeat of EP) and the student's t-test (age) or Mann–Whitney U test (gestational age) for continuous variables were used to evaluate the difference between laparoscopy and open surgery group, respectively. A p value of < 0.05 (two-sided) was considered statistically significant. SPSS 22.0 software (IBM Corporation, Amonk, NY, USA) was used to analyze all data.
Results
Patients' characteristics
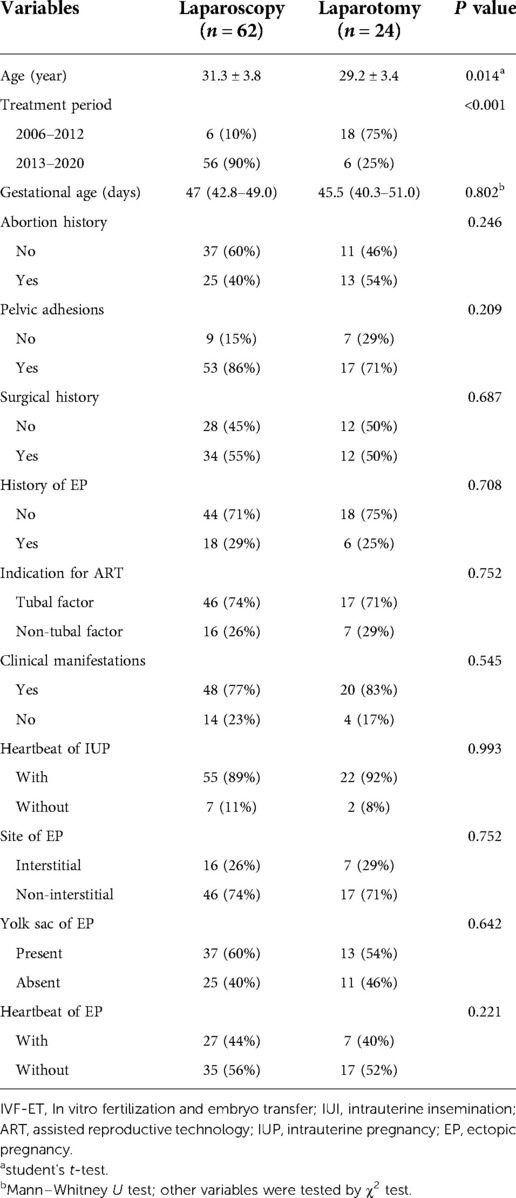
Among 86 patients with HP after embryo transfer, 62 underwent LA and 24 with OA. The demographic and clinical characteristics of these two groups is shown in Table 1. 68 patients had clinical manifestation (56 only with vaginal bleeding, 7 only with abdominal pain and 5 with both), while the remaining 18 were asymptomatic at admission. Among all HP patients, only two had intrauterine twin gestation. One patient had a live birth after selective fetal reduction, while another one gave live twin birth. There were no statistically significant differences between LA and OA (all p > 0.05), except for age and treatment period. Patients with OA were younger than those with LA (29.2 ± 3.4 vs. 31.3 ± 3.8, p = 0.014). The adoption of laparoscopic treatment of HP was significantly increased from the period of 2006–2012 (6/24, 25%) to the period of 2013–2020 (56/62, 90%) (p < 0.001).
Perioperative outcomes
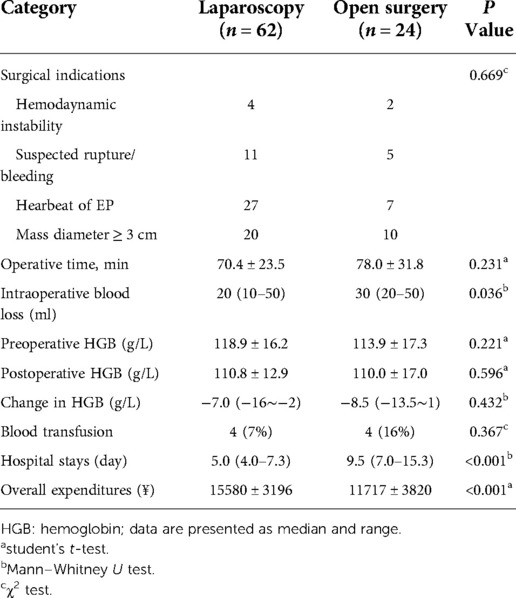
Table 2 presents a comparison of perioperative outcomes between the two groups. Compared with those in the OA group, patients in the LA group had less blood loss [20 (10–50) vs. 30 (20–50) ml, p = 0.036] and fewer days of hospital stay [5.0 (4.0–7.3) vs. 9.5 (7.0–15.3) days, p < 0.001], but a relatively higher cost (15,580 ± 3196¥ vs. 11,717 ± 3820¥, p < 0.001). The surgical indications, hemoglobin levels before and after surgery, as well as changes in hemoglobin level, the operative time, and the percentage of patients receiving blood transfusion were not significantly different between LA and OA group (all p > 0.05). No conversion from LA to OA was performed.
Obstetrical outcomes
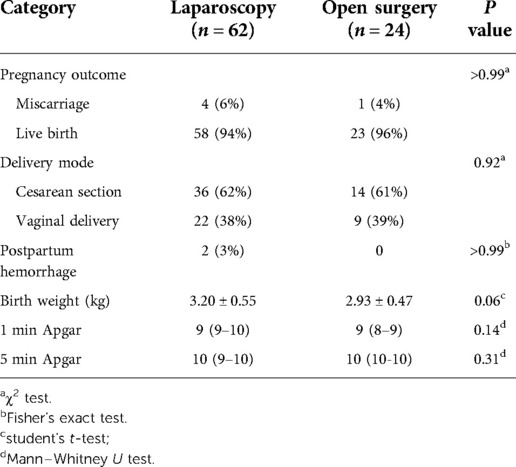
Pregnancy outcomes are listed in Table 3. After surgery, there were no significant differences in the rates of miscarriage [6% (4/62) vs. 4% (1/24), p > 0.99]. Among patients with live birth, the birth weight (3.20 ± 0.55 vs. 2.93 ± 0.47 kg, p = 0.06), 1 min Apgar (9 (9–10) vs. 9 (8–9), p = 0.14) and 5 min Apgar (10 (10–10) vs. 10 (10–10), p = 0.31) of the infants were also similar in the laparoscopic and open surgery group. Also, there were no differences in the delivery mode (p = 0.92) between the two groups. No congenital abnormalities were observed.
Discussion
In this retrospective cohort study, we found that the LA had less blood loss, shorter hospital stays and comparable obstetrical outcomes than OA in women with HP after after embryo transfer.
The standard management for HP remains unknown due to the rarity of this disease. Surgical treatment is the most frequently choice for HP (8–11). With the development of equipment and techonology, clinicians have put more and more attention to laparoscopy, rather than open surgery (21–23). In the present study, LA was performed for patients with HP in only 25% (6/24) of cases during the 2006–2012 period. This proportion significantly increased to 90% (56/62) during 2013–2020 period, which was consistent with the result reported in a review (24).
However, there are inconsistent conclusions on the efficacy and safety of LA no matter for treatment of HP or pregnancy with surgical diseases, such as appendicitis and cholecystitis. Several studies have found for patients with appendicitis, an increased rate of fetal loss in the laparoscopic appendectomy compared with the open appendectomy (25–27). Nevertheless, some studies reported that laparoscopic cholecystectomy was associated with decreased risks for fetal, maternal, and surgical complications in patients with symptomatic cholelithiasis (28, 29). Besides, in gynecologic field, several case report or case-series studies have indicated that the feasibility and safety of laparoscopic approach in HP patients. Jiang et al. reported the obstetric outcomes of 7 patients with heterotopic interstitial pregnancy treated by LA and found that all patients were full-term delivery except one without obstetric data (15). Jeong et al. summarized the obstetric outcomes of the laparoscopic approach for 17 HP patients. The authors stated that 13 delivered 14 healthy babies, and only two failed to maintain their pregnancies (30). Li et al. also reported the pregnancy outcome of laparoscopic cornual resection for 8 HP patients, and found that LA may be a potential risk factor for abortion with a miscarriage rate (12.5%) (21). The evidence of inconsistent results found in these studies were limited due to its small sample size and without comparison with open surgery.
In this study, we found that compared with OA, the LA demonstrated less intraoperative blood loss and fewer days of hospital stay, which reflected the advantages of laparoscopic minimally invasive therapy. Although LA showed shorter hospital days, the hospital stays in our study were relatively longer than that in western countries, may be mainly explained by the fact that these women were kept hospitalized for fetal surveillance. Because most of women had the history of miscarriage or ectopic pregnancy or conceived via ART and thus experienced great emotional burdens. Taking into account of concerns for miscarriage after surgery, women are willing to require prolonged hospitalization. Besides, this may be related to Chinese traditional customs of tocolysis. A similar hospital stay of HP patients was reported in another study from China (31).
In addition, compared with OA, LA demonstrated less intraoperative bleeding. This finding is expected due to larger surgical incisions and more urgent situation in OA increasing the possibility of blood loss. Despite this, the total amount of intraoperative bleeding in both surgical methods was little, which could be reflected by 76 (88%) cases with bleeding less than 50 ml and the similar changes in hemoglobin levels before and after surgery. In our study, no statistically significant difference in operative time between two types of surgical methods was found, which is consistent with existing studies on adnexal masses or torsion and interstitial pregnancy treated by LA and OA (32–35). With the standardization of laparoscopic surgery and accumulation of experience, the operative time of LA has been significantly reduced in recent years. Besides, often experienced, the operating time was increased by larger surgical incisions for patients underwent OA. Thus, we found similar operative time between LA and OA groups.
In this study, the average total cost for LA was relatively higher than that of OA. It may be caused by the additional instruments and corresponding expenditures needed in LA. However, laparoscopy may actually have greater economic advantages because of the quicker recovery and earlier back to work from a long-term perspective.
For HP treatment, the safety of intrauterine fetus is another concern. Clayton et al. (7) claimed surgical management of the EP could increase the likelihood of intrauterine abortion. In our study, most women (81/86, 94%) had successful delivery for live birth, which was consistent with previous studies (31, 36, 37). Our HP live birth rate was higher than the live birth rate (66%–69%) reported by other studies (5, 8, 38). The ratio of first trimester miscarriage after the operation was only 6% (4/62) and 4% (1/24) in LA and OA, respectively. The high live birth rate in our study may be related to the timely diagnosis and intervention by experienced doctors. Moreover, no significant differences of pregnancy outcomes (first trimester miscarriage, birth weight, cesarean section rate and Apgar score) were found between the LA and the OA groups. Our results suggested the similar pregnancy outcome in patients with LA or OA for treating HP.
The strength of our work is the first study with a relatively large sample size to compare the two surgical approaches on perioperative and pregnancy outcomes in the treatment of HP for patients after embryo transfer by taking into account of its rarity. Compared with existed case reports and case-series studies, this study could provide a relatively higher level of evidence for clinician to choose laparoscopic surgery for those patients with HP. Besides, this study could provide some insight to focus on the efficacy and safety of different types of laparoscopy, such as a natural orifice transluminal endoscopic surgery (NOTES) reported in a case report (39), in the future.
The present study also had some limitations. First, it's a retrospective study. However, the data from medical records was collected objectively, which may to some extent reduce the retrospective bias. Frankly, it's extremely difficult to carry out a prospective study due to the rarity of this disease. In addition, the findings may not be generalizable due to the single-center design of this study, as well as sociocultural aspects and health care policies. Therefore, more studies from different centers are needed to validate our results.
Conclusions
Laparoscopy maybe a safe and feasible procedure for treating HP patients. Compared with open approach, it showed a more favorable perioperative outcomes and similar pregnancy outcomes. If surgery is indicated and conditions permit, Laparoscopy could be a preferred method for the treatment of patients with HP.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by The institutional review board (IRB) of Sun Yat-Sen Memorial Hospital. The patients/participants provided their written informed consent to participate in this study.
Author contributions
CSF and ZYY drafted the manuscript. CSF and ZYY performed the statistical analysis. CSF and ZYY helped in the verification of patients’ data and revised the manuscripts. CSF and XMQ conceived of the study, and participated in its design. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by Sun Yat-Sen University Clinical Research 5010 Program (2017014).
Acknowledgments
We appreciate to professor Pheier Saw for her help in the language editing and Yanfang Ye for her help in the statistical analysis of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Soriano D, Shrim A, Seidman DS, Goldenberg M, Mashiach S, Oelsner G. Diagnosis and treatment of heterotopic pregnancy compared with ectopic pregnancy. J Am Assoc Gynecol Laparosc. (2002) 9:352–8. doi: 10.1016/S1074-3804(05)60416-1
2. Kriplani A, Lunkad AS, Sharma M, Ammini AC. Recurrent ectopic pregnancy with heterotopic pregnancy in a patient of hypogonadotropic hypogonadism: a case report. J Reprod Med. (2011) 56:274–6.21682126
3. Anastasakis E, Jetti A, Macara L, Daskalakis G. A case of heterotopic pregnancy in the absence of risk factors. A brief literature review. Fetal Diagn Ther. (2007) 22:285–8. doi: 10.1159/000100792
4. Korkontzelos I, Antoniou N, Stefos T, Kyparos I, Lykoudis S. Ruptured heterotopic pregnancy with successful obstetrical outcome: a case report and review of the literature. Clin Exp Obstet Gynecol. (2005) 32:203–6.16433167
5. Xiao S, Mo M, Hu X, Zhang H, Xu S, Wang Z, et al. Study on the incidence and influences on heterotopic pregnancy from embryo transfer of fresh cycles and frozen-thawed cycles. J Assist Reprod Genet. (2018) 35:677–81. doi: 10.1007/s10815-017-1109-x
6. Fernandez H, Gervaise A. Ectopic pregnancies after infertility treatment: modern diagnosis and therapeutic strategy. Hum Reprod Update. (2004) 10:503–13. doi: 10.1093/humupd/dmh043
7. Clayton HB, Schieve LA, Peterson HB, Jamieson DJ, Reynolds MA, Wright VC. A comparison of heterotopic and intrauterine-only pregnancy outcomes after assisted reproductive technologies in the United States from 1999 to 2002. Fertil Steril. (2007) 87:303–9. doi: 10.1016/j.fertnstert.2006.06.037
8. Barrenetxea G, Barinaga-Rementeria L, Lopez de Larruzea A, Agirregoikoa JA, Mandiola M, Carbonero K. Heterotopic pregnancy: two cases and a comparative review. Fertil Steril. (2007) 87:417–e9. doi: 10.1016/j.fertnstert.2006.05.085
9. Wu Z, Zhang X, Xu P, Huang X. Clinical analysis of 50 patients with heterotopic pregnancy after ovulation induction or embryo transfer. Eur J Med Res. (2018) 23:17. doi: 10.1186/s40001-018-0316-y
10. Guan Y, Ma C. Clinical outcomes of patients with heterotopic pregnancy after surgical treatment. J Minim Invasive Gynecol. (2017) 24:1111–5. doi: 10.1016/j.jmig.2017.03.003
11. Solangon SA, Otify M, Gaughran J, Holland T, Ross J, Jurkovic D. The risk of miscarriage following surgical treatment of heterotopic extrauterine pregnancies. Hum Reprod Open. (2022) 1:hoab046. doi: 10.1093/hropen/hoab046
12. Jiang Z, Du G, Wang X, Zhai X, Zhang G, Jin B, et al. Laparoscopic versus open surgery for hepatic caudate lobectomy: a retrospective study. Surg Endosc. (2022). doi: 10.1007/s00464-022-09631-x. [Epub ahead of print]
13. Ehrenberg-Buchner S, Sandadi S, Moawad NS, Pinkerton JS, Hurd WW. Ectopic pregnancy: role of laparoscopic treatment. Clin Obstet Gynecol. (2009) 52:372–9. doi: 10.1097/GRF.0b013e3181b0be24
14. Soriano D, Vicus D, Schonman R, Mashiach R, Shashar-Levkovitz D, Schiff E, et al. Long-term outcome after laparoscopic treatment of heterotopic pregnancy: 19 cases. J Minim Invasive Gynecol. (2010) 17:321–4. doi: 10.1016/j.jmig.2010.01.016
15. Jiang Y, Chen J, Zhou H, Zheng M, Han K, Ling J, et al. Management and obstetric outcomes of 17 heterotopic interstitial pregnancies. BMC Pregnancy Childbirth. (2018) 18:78. doi: 10.1186/s12884-018-1700-x
16. Kim MJ, Jung YW, Cha JH, Seok HH, Han JE, Seong SJ, et al. Successful management of heterotopic cornual pregnancy with laparoscopic cornual resection. Eur J Obstet Gynecol Reprod Biol. (2016) 203:199–203. doi: 10.1016/j.ejogrb.2016.04.026
17. Balafoutas D, Diessner J, Kiesel M, Woeckel A, Joukhadar R. Laparoscopic management of a heterotopic pregnancy in the tubal stump. J Minim Invasive Gynecol. (2021) 28:752–3. doi: 10.1016/j.jmig.2020.07.008
18. Xu W, Lin X, Huang D, Zhang S. Laparoscopic treatment of cornual heterotopic pregnancy: a retrospective cohort study. Int J Surg. (2018) 53:98–102. doi: 10.1016/j.ijsu.2018.03.025
19. Li J, Luo X, Yang J, Chen S. Treatment of tubal heterotopic pregnancy with viable intrauterine pregnancy: analysis of 81 cases from one tertiary care center. Eur J Obstet Gynecol Reprod Biol. (2020) 252:56–61. doi: 10.1016/j.ejogrb.2020.06.005
20. Soriano D, Vicus D, Mashiach R, Schiff E, Seidman D, Goldenberg M. Laparoscopic treatment of cornual pregnancy: a series of 20 consecutive cases. Fertil Steril. (2008) 90:839–43. doi: 10.1016/j.fertnstert.2007.07.1288
21. Li S, Cao M, Liu H, He Y, Liu J. Management of 14 patients with cornual heterotopic pregnancy following embryo transfer: experience from the past decade. Reprod Biol Endocrinol. (2021) 19:152. doi: 10.1186/s12958-021-00834-w
22. Chen L, Sun WJ, Hao LJ, Lin Y. Successfully managing cornual heterotopic pregnancy:a case report and literature review. Chin Med Sci J. (2021) 36:161–70. doi: 10.24920/003963
23. Delgado SI, Koythong T, Guan X. Minimally invasive surgical management of a cornual ectopic pregnancy, with and without a concurrent intrauterine pregnancy. Fertil Steril. (2021) 116:1189–90. doi: 10.1016/j.fertnstert.2021.06.007
24. Dendas W, Schobbens JC, Mestdagh G, Meylaerts L, Verswijvel G, Van Holsbeke C. Management and outcome of heterotopic interstitial pregnancy: case report and review of literature. Ultrasound. (2017) 25:134–42. doi: 10.1177/1742271X17710965
25. McGory ML, Zingmond DS, Tillou A, Hiatt JR, Ko CY, Cryer HM. Negative appendectomy in pregnant women is associated with a substantial risk of fetal loss. J Am Coll Surg. (2007) 205:534–40. doi: 10.1016/j.jamcollsurg.2007.05.025
26. Wilasrusmee C, Sukrat B, McEvoy M, Attia J, Thakkinstian A. Systematic review and meta-analysis of safety of laparoscopic versus open appendicectomy for suspected appendicitis in pregnancy. Br J Surg. (2012) 99:1470–8. doi: 10.1002/bjs.8889
27. Chakraborty J, Kong JC, Su WK, Gourlas P, Gillespie C, Slack T, et al. Safety of laparoscopic appendicectomy during pregnancy: a systematic review and meta-analysis. ANZ J Surg. (2019) 89:1373–8. doi: 10.1111/ans.14963
28. Sedaghat N, Cao AM, Eslick GD, Cox MR. Laparoscopic versus open cholecystectomy in pregnancy: a systematic review and meta-analysis. Surg Endosc. (2017) 31:673–9. doi: 10.1007/s00464-016-5019-2
29. Nasioudis D, Tsilimigras D, Economopoulos KP. Laparoscopic cholecystectomy during pregnancy: a systematic review of 590 patients. Int J Surg. (2016) 27:165–75. doi: 10.1016/j.ijsu.2016.01.070
30. Eom JM, Choi JS, Ko JH, Lee JH, Park SH, Hong JH, et al. Surgical and obstetric outcomes of laparoscopic management for women with heterotopic pregnancy. J Obstet Gynaecol Res. (2013) 39:1580–6. doi: 10.1111/jog.12106
31. Yu Y, Xu W, Xie Z, Huang Q, Li S. Management and outcome of 25 heterotopic pregnancies in zhejiang, China. Eur J Obstet Gynecol Reprod Biol. (2014) 180:157–61. doi: 10.1016/j.ejogrb.2014.04.046
32. Cagino K, Li X, Thomas C, Delgado D, Christos P, Acholonu U Jr. Surgical management of adnexal masses in pregnancy: a systematic review and meta-analysis. J Minim Invasive Gynecol. (2021) 28:1171–82. doi: 10.1016/j.jmig.2021.01.020
33. Ngu SF, Cheung VY, Pun TC. Surgical management of adnexal masses in pregnancy. JSLS. (2014) 18:71–5. doi: 10.4293/108680813X13693422521007
34. Bras R, Braga J, Tome A, Ferreira H. Adnexal torsion in the first trimester of pregnancy: diagnosis, laparoscopic management, and review of the literature. Surg Technol Int. (2017) 30:210–4.28537347
35. Marchand G, Taher Masoud A, Sainz K, Azadi A, Ware K, Vallejo J, et al. A systematic review and meta-analysis of laparotomy compared with laparoscopic management of interstitial pregnancy. Facts Views Vis Obgyn. (2021) 12:299–308.33575679
36. Lyu J, Ye H, Wang W, Lin Y, Sun W, Lei L, et al. Diagnosis and management of heterotopic pregnancy following embryo transfer: clinical analysis of 55 cases from a single institution. Arch Gynecol Obstet. (2017) 296:85–92. doi: 10.1007/s00404-017-4384-y
37. Cookingham LM, Goossen RP, Sparks AET, Van Voorhis BJ, Duran EH. Successful treatment algorithm for evaluation of early pregnancy after in vitro fertilization. Fertil Steril. (2015) 104:932–7. doi: 10.1016/j.fertnstert.2015.07.1133
38. Shang J, Peng R, Zheng J, Lin M. The indicator of clinical outcomes for patients with heterotopic pregnancy following in-vitro fertilization with embryo transfer. Taiwan J Obstet Gynecol. (2019) 58:827–32. doi: 10.1016/j.tjog.2019.09.018
Keywords: heterotopic pregnancy, laparoscopy, open surgery, perioperative outcome, pregnancy outcome
Citation: Chen S, Zhu Y and Xie M (2022) Comparison of laparoscopic and open approach in the treatment of heterotopic pregnancy following embryo transfer. Front. Surg. 9:1006194. doi: 10.3389/fsurg.2022.1006194
Received: 29 July 2022; Accepted: 6 October 2022;
Published: 1 November 2022.
Edited by:
Tai-Ho Hung, Taipei Chang Gung Memorial Hospital, TaiwanReviewed by:
Charalampos Theofanakis, School of Health Sciences, National and Kapodistrian University of Athens, Greece Cihan Kaya© 2022 Chen, Zhu and Xie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Meiqing Xie eGllbXFAbWFpbC5zeXN1LmVkdS5jbg== Yingying Zhu emh1eXk3OUBtYWlsLnN5c3UuZWR1LmNu
Specialty Section: This article was submitted to Obstetrics and Gynecological Surgery, a section of the journal Frontiers in Surgery
 Shengfu Chen
Shengfu Chen Yingying Zhu
Yingying Zhu Meiqing Xie
Meiqing Xie