- 1Department of Obstetrics and Gynecology, The Affiliated Nanchong Central Hospital of North Sichuan Medical College, Nanchong, China
- 2Department of Obstetrics and Gynecology, Si Chuan Mian Yang 404 Hospital, Mianyang, China
Objective: To compare the return to work (RTW) time between single-port laparoscopic surgery (SPLS) and multiport laparoscopic surgery (MPLS) for benign ovarian tumors.
Methods: A cross-sectional cohort study was conducted, which consisted of 335 women of reproductive age with benign ovarian tumors and who were keen on returning to work as early as possible. Surgical outcomes, postoperative pain score, postoperative satisfaction with the cosmesis score (CS), and the RTW time of the SPLS group were compared with those of the MPLS group. Besides, the RTW time and CS were calculated from the questionnaire survey by a single specialized gynecologist.
Results: Women who met the inclusion criteria were included in the SPLS (n = 106) and MPLS groups (n = 229). The RTW time in the SPLS group (22.13 ± 27. 06 days) was significantly shorter than that in the MPLS group (46.08 ± 57.86 days) (P < 0.001). The multivariate Cox analysis results showed that age (HR = 0.984, 95% CI, 0.971−0.997, P = 0.020), SPLS (HR = 3.491, 95% CI, 2.422−5. 032, P < 0.001), and return to normal activity time (HR = 0.980, 95% CI, 0.961−0.998, P = 0.029) were independent factors of the RTW time.
Conclusions: SPLS may be advantageous in terms of shortening the RTW time for women with benign ovarian tumors.
Introduction
Benign ovarian tumors are the most common condition in women of reproductive age; of these, 7% are urgent candidates for surgery (1). Single-port laparoscopic surgery (SPLS) has become a common procedure for treating benign ovarian tumors (2). Studies by Capozzi et al. (3) and Yi (4) have shown that single-site surgery seems to be a feasible and safe gynecological procedure for women with benign ovarian tumors. However, Bonollo et al. (5) have reported that current evidence does not seem to demonstrate a clear superiority of laparoendoscopic single-site surgery over multiport laparoscopic surgery (MPLS), except for producing cosmetic results in benign gynecological surgery. Thus, no consensus has been reached on the advantages of SPLS for benign ovarian tumors, including whether it contributes to a shorter return to work (RTW) time (2, 6–8).
Women with benign ovarian tumors, especially single mothers, must return to work as quickly as possible, because their employment income is the main source of family income. Delayed RTW lowers the postoperative quality of life of young women and imposes undue yet substantial costs on society owing to the lost working hours (8). Therefore, it is of great importance to choose a surgical plan that helps women with benign ovarian tumors to reduce their RTW time.
We retrospectively analyzed the data of women with benign ovarian tumors, aiming to explore the potential relationship between the RTW time and SPLS and to identify the potential factors affecting the RTW time of SPLS.
Materials and methods
Study population
A cross-sectional cohort study was conducted on 335 women with operative indications for benign ovarian tumors at the Affiliated Nanchong Central Hospital of North Sichuan Medical College between January 2019 and January 2021. According to medical records, 106 women in the SPLS group and 229 women in the MPLS group were analyzed retrospectively. This study was approved by the institutional review board of Nanchong Central Hospital (No. 03053/2019). The need for consent was waived because of data anonymization and the retrospective nature of the study.
Inclusion criteria were patients who received SPLS or MPLS for benign ovarian tumors; who were satisfied with their work and eager to return to work; had a pelvic ultrasound or magnetic resonance imaging to indicate benign ovarian tumors before surgery; had a normal level of tumor markers, including serum carbohydrate antigen 125 (CA125) and human epididymis protein 4 (HE4); were evaluated as according to the American Society of anesthesiologists (ASA) classification I–II; were confirmed to have a benign ovarian tumor by postoperative histopathology.
The exclusion criteria were patients who were unemployed; who received open surgery for benign ovarian tumors; had no intention of returning to work; had severe pain before operation; were obese with a body mass index (BMI) > 30 kg/m2 (9); had an obviously malignant tumor on imaging or high serum CA125 levels (500 U/ml) or postoperative histopathology (10); had other concurrent tumors; had severe internal surgical diseases or a history of abdominal surgery.
Surgical technique
The surgery was performed by two consultant gynecologists who had prior training in performing SPLS. The trial management committee reviewed two unedited laparoscopic videos and patient outcomes to ensure the adequacy of the surgeon's technique (11). All patients underwent the same preoperative preparation and general anesthesia during surgery, with endotracheal intubation and placement in the supine position with the legs slightly separated. Patients underwent surgery with an open Hasson approach for abdominal entry via a single 2 cm vertical umbilical incision. (12). Upon abdominal entry, a multi-instrument access port was used. Single laparoscopic surgery instruments were used for the surgery. The surgical technique for the MPLS procedure conformed to that used by Richards et al. (13). In addition, the pneumoperitoneum was maintained at 12 mmHg. At the end of each surgery, the fascia was identified and closed with a delayed absorbable suture.
Parameters analyzed
RTW was defined as the time from the date of surgery to the date of time to return to work. The return-to-work questionnaire survey, which included demographics such as age, work status, and specific questions on returning to work, was peer-reviewed and focus-grouped. Participants were requested to they lived far away from our answer the reason for returning to work, job satisfaction ratings and the time to general activity, including sexual intercourse. The participants were suggested regular follow-up. From August 2021 to September 2021, 335 patients completed the questionnaire survey either at our hospital or by telephone because they they lived far away from our hospital.
BMI was categorized by standard criteria by the WHO, while ASA was classified by standard criteria of the American Society of Anesthesiologists’ classification. Data collection included surgical options, histological subtypes, and surgical outcomes. The major surgical outcome was the RTW time; the others were estimated blood loss, specimen retrieval time, operation duration, postoperative pain score, return to normal activity time, postoperative hospitalization, and cosmetic outcomes. The postoperative pain score was assessed using the Numerical Rating Scale (NRS, range: 0–10, 0 = no pain, 10 = unbearable pain) 48 h after surgery. Postoperative cosmesis satisfaction (CS) was evaluated by using the scar satisfaction score (range: 0–10, 0 = not satisfactory, 10 = totally satisfactory). In addition, the questionnaire survey was used to calculate the RTW time and CS.
Data analysis
Statistical analyses were performed using SPSS software (SPSS 20, Armonk, NY, United States). Quantitative variables with normal distribution were described as mean ± standard deviation. We compared the continuous data by conducting the unpaired Student's t-test, while binomial data used Chi-squared tests to show the baseline characteristics of the participants and assess the differences between the two groups. The Chi-square test and Cox regression were adopted to illustrate whether the selected surgical approach affected the RTW time. The Kaplan–Meier method was used to evaluate the value of SPLS in predicting the RTW time for women with benign ovarian tumors. In addition, P < 0.05 was defined as statistically significant.
Results
Clinicopathological features
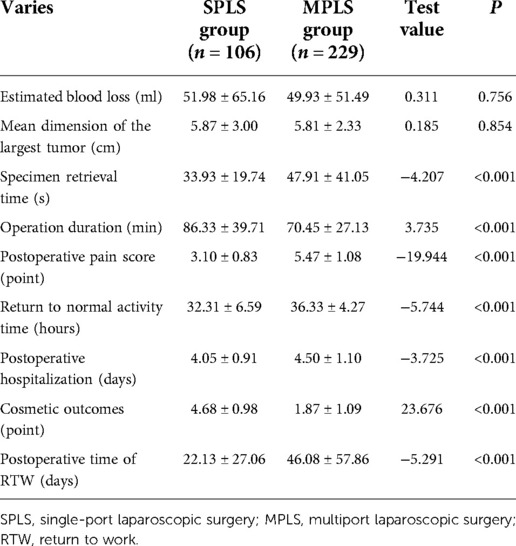
A total of 335 patients with benign ovarian tumors were included in this cross-sectional cohort study, out of which 106 (31.64%) were included in the SPLS group and 229 (68.46%) in the MPLS group, according to medical records. There were no differences in terms of age, BMI, ASA rank, surgical options, and histological subtypes between the two groups (P > 0.05), and these are summarized in Table 1.
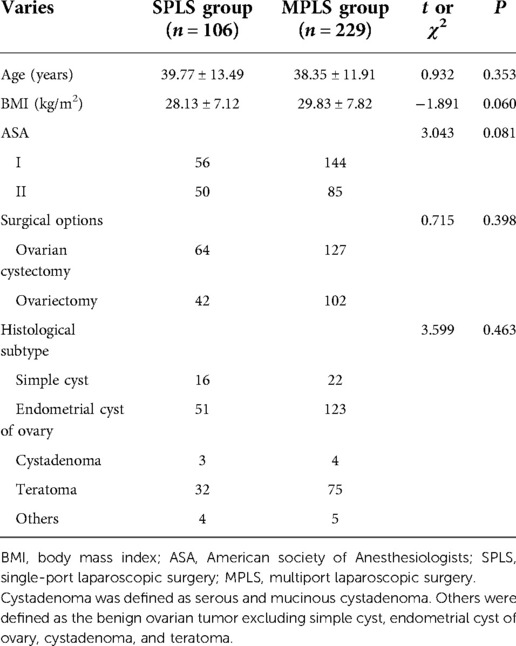
Table 1. Clinical characteristics of patients with benign ovarian tumor compared between the SPLS and the MPLS groups.
Surgical outcomes
The RTW time was shorter in the SPLS group (22.13 ± 27.06 days) than in the MPLS group (46.08 ± 57.86 days). Specimen retrieval time and the postoperative pain score were shorter in the SPLS group than in the MPLS group (P < 0.05, Table 2). The operation duration and CS were higher in the SPLS group than in the MPLS group (P < 0.05, Table 2). The mean estimated blood loss in the two groups was similar (P > 0.05, Table 2). Moreover, there was no conversion to laparotomy, abdominal wall vascular, nerve injury, urinary system injury, lymphatic leakage, and other complications between the two groups.
Factors influencing return to work time
In the multivariate cox logistic regression, age, ASA, surgical approaches, postoperative pain score, and return to normal activity time were associated with the RTW time (P < 0.05, Table 3). Besides, multivariate cox regression analysis showed that age (HR = 0.984, 95% CI, 0.971–0.997, P = 0.020), SPLS (HR = 3.491, 95% CI, 2.422–5.032, P < 0.001), and return to normal activity time (HR = 0.980, 95% CI, 0.961–0.998, P = 0.029) were associated with the RTW time for women with benign ovarian tumors (Table 3).
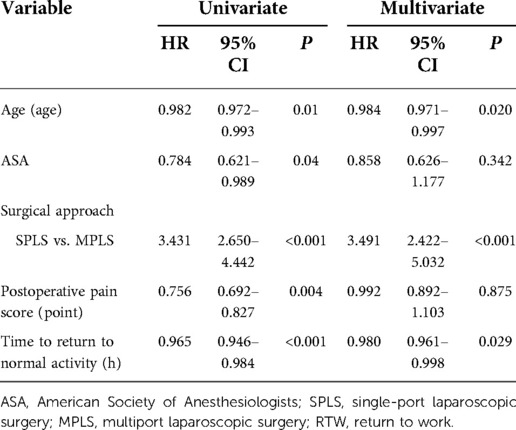
Table 3. Univariate and multivariate Cox proportional hazards analysis of postoperative time of RTW.
The magnitude of SPLS for return to work time
In the Kaplan−Meier analysis, the estimated medium time of RTW was significantly shorter in the SPLS group than in the MPLS group (18.6 vs. 37.0 days, P < 0.001, as shown in Figure 1).
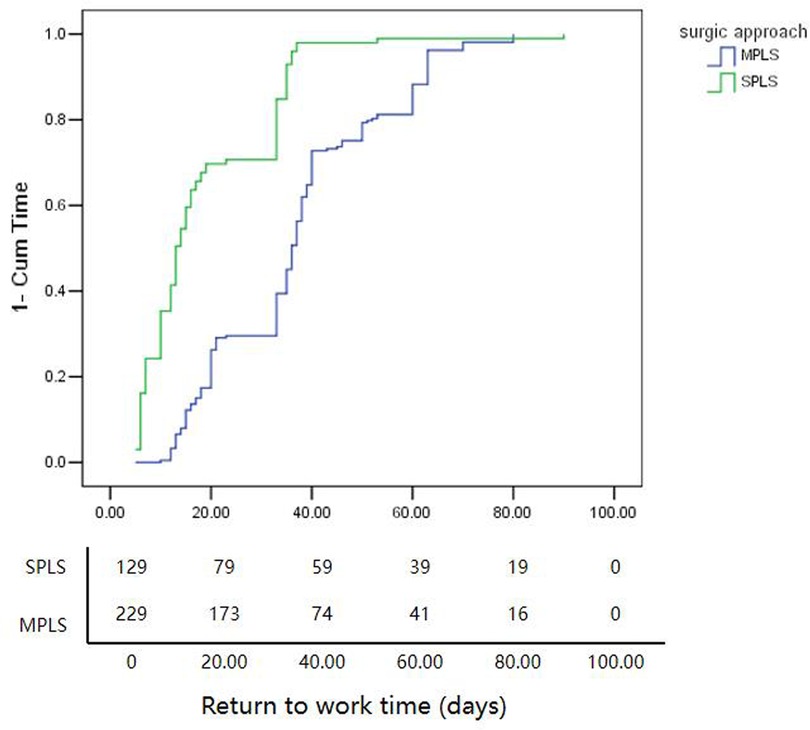
Figure 1. The magnitude of SPLS for RTW. The estimated medium time of RTW in the SPLS group was significantly shorter than those in the MPLS group (18.6 days vs 37.0 days, P < 0.001). SPLS, single-port laparoscopic surgery; RTW, return to work time.
Discussion
In this cross-sectional cohort study, we discovered that SPLS was more likely to reduce the RTW time than conventional surgery. Moreover, we showed that SPLS might help reduce specimen retrieval time, gain lower postoperative pain scores, and achieve a superior CS. In addition, our research identified that beyond age and return to normal activity time, SPLS was an independent factor for the RTW time.
Huff et al. (14) showed that return to normal activity time and BMI significantly influenced the time taken for women to work after laparoscopic myomectomy. However, the data on the association between SPLS and RTW after surgery are insufficient. At present, there are no guidelines for the surgeons to chose which one from SPLS and MPLS for resecting benign ovarian tumors. Also, a consensus on the advantages of SPLS in gynecological surgery has not yet been reached. Al-Badawi et al. (15) reported that SPLS was almost feasible and potentially safe, given that no patient required the addition of extra parts or conversion to conventional multiaccess laparoscopy or laparotomy and that patients were satisfied over their reduced postoperative pain. Capozzi et al. (3) reported that a robotic single-port platform seemed feasible and safe for all gynecological surgical procedures. However, higher conversion and complication rates would be considered safe for patients with malignant diseases.
Nevertheless, Schmitt et al. (7) found no significant difference between the two groups in terms of laparotomy conversion rate, postoperative pain, intraoperative blood loss, mean hospitalization, and cosmetic results via systematic review and meta-analysis to compare the advantages of SPLS over conventional laparoscopy for surgery. Bonollo et al. (5) also reported that laparoendoscopic single-site surgery does not seem to demonstrate a clear superiority over MPLS, except for better cosmetic results in benign gynecological surgery. Yi (4) reported that single-site incision laparoscopic surgery for adnexal surgery is a safe technique. However, a certain training period for learning the technique is required. In our study, although we did not use a learning curve, we invited the trial management committee to ensure the adequacy of the surgeon's technique. In addition, our results showed the advantages of SPLS in terms of specimen retrieval time, postoperative pain score, cosmetic outcomes, and reduced RTW time in women with benign ovarian tumors.
Admittedly, the majority of patients with benign ovarian tumors are women of reproductive age, especially single mothers with great economic pressure and family responsibilities who are eager to return to work as early as possible. Delayed time to RTW may increase the risks of prolonged sick leave and lower quality of life in postoperative women of reproductive age and lead to undue and substantial costs for society through lost working hours (8). The average RTW time of patients undergoing MPLS in our study was 37 days, meaning most patients had no financial resources during this period. However, the average RTW time in the SPLS group was 18.5 days, which reduced the RTW time to a great extent. Therefore, we can infer that SPLS may reduce the RTW time and be conducive to reducing the economic pressure of family and social burden.
The underlying mechanisms of the benefits of SPLS for benign ovarian tumors have not yet been clarified. However, we attempted to explain the potential mechanisms. First, SPLS might be conducted for postoperative pain relief. Postoperative pain is self-limiting, while the greatest intensity falls on the first and second postoperative days, with much less intensity during the third and fourth postoperative days (16). The probability of shorter pain relief time in the SPLS group is that the likelihood of injury of microvascular nerves and other tissues during surgery is less, with only a slight stimulation to the pain area of the cerebral cortex (17, 18). Second, SPLS conforms to the concept of rapid recovery. As the concept of rapid recovery had successfully demonstrated benefits to surgical patients in the late 20th century, the clinical application of rapid recovery pathways aims at improving surgical outcomes in gynecology (17, 19). SPLS may be conducted to reduce the return to normal activity time and postoperative hospitalization, which is conducive to the rapid recovery of patients and reduces the possibility of cross-infection in hospitals due to long hospitalization days (20). Third, SPLS is more advantageous with regard to specimen retrieval time since its puncture hole is larger than that of MPLS, which provides excellent protection against abdominal wall metastasis and cyst fluid leakage, and also reducing the possibility of metastasis and incision implantation, which might be caused by specimen removal rupture (21). In addition, SPLS maximizes the use of the umbilical folds to cover the scar left by the incision, thus hiding wound healing; a better cosmetic outcome (22), which is more popular with women of reproductive age. Finally, consistent with the results given by Hoyer-Sorensen et al. (23), although the operation duration of SPLS was prolonged in our study due to the “chopsticks effect,” reduced visualization, and the interference between instruments (7), estimated blood loss was minimal and complications such as injury to the nerves and the urinary system did not arise. Therefore, it can be concluded that SPLS is safe and feasible for treating benign ovarian tumors.
However, our study has some limitations. First, the cross-sectional cohort design makes it difficult to state that SPLS is a protective factor for the postoperative time of RTW. However, our study provides details of the clinical strategy for benign ovarian tumors. Second, the potential bias arising out of the influence of the differences of surgical skills on outcomes cannot be completely eliminated; however, we asked the trial management committee to ensure the adequacy of the surgeon's technique. Third, vaginal natural orifice transluminal endoscopic surgery (V-NOTES) is an alternative laparoscopic technique that provides single surgical access without leaving abdominal scars. We did not compare the clinical effects between SPLS and V-NOTES. However, in the future, we plan to conduct another study to compare the time to return to work between V-NOTES and SPLS. The other limitation is that the primary outcome might be susceptible to bias because the RTW time was self-reported by women (8), but data were collected on time. However, we believe that the advantages of SPLS will be of interest to clinicians when devising clinical strategies.
Conclusion
In summary, our preliminary results showed that beyond age and return to normal activity time, SPLS was conducive to a shorter RTW time in benign ovarian tumors, which meant that it was advantageous in terms of rapid recovery after surgery.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study was reviewed and approved by the institutional review board of Nanchong Central Hospital (NO. 03053/2019). Written informed consent for participation was not required for this study in accordance with the national legislation and institutional requirements.
Author contributions
YT was responsible for manuscript conception and writing. M-bW was responsible for manuscript conception, data collection, and examination. BS was responsible for manuscript conception, data analysis, and editing. HW performed data analysis and edited the manuscript. X-mZ was responsible for data collection and manuscript conception. M-tY wrote the manuscript. SY and FX edited the manuscript. H-qH was in charge of project development and responsible for writing the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Natural Science Foundation of China (No. 81872506), the Foundation of the State Key Laboratory of Ultrasound in Medicine and Engineering (Grant Nos. 2020KFKT003 and 2021KFKT022), and the Bureau of Science and Technology Nanchong City Program (Nos. 20SXQT0320, 22SXQT0254, and 22SXQT034).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wang D, Liu H, Li D, Qiu L, Dai J, Sun D, et al. Comparison of the impact of single-port laparoscopic and conventional laparoscopic ovarian cystectomy on the ovarian reserve in adult patients with benign ovarian cysts. Minim Invasive Ther Allied Technol. (2020) 29(4):224–31. doi: 10.1080/13645706.2019.1624575
2. Moulton L, Jernigan AM, Carr C, Freeman L, Escobar PF, Michener CM. Single-port laparoscopy in gynecologic oncology: seven years of experience at a single institution. Am J Obstet Gynecol. (2017) 217(5):610.e1–8. doi: 10.1016/j.ajog.2017.06.008
3. Capozzi VA, Armano G, Rosati A, Tropea A, Biondi A. The robotic single-port platform for gynecologic surgery: a systematic review of the literature and meta-analysis. Updates Surg. (2021) 73(3):1155–67. doi: 10.1007/s13304-020-00812-8
4. Yi SW. Learning curve analysis of single-site incision laparoscopic adnexal surgery performed by a single surgeon. Ginekol Pol. (2022). doi: 10.5603/GP.a2022.0041
5. Bonollo M, Bellaminutti S, Gasparri ML, Papadia A. Is it time to leave multi- for single-port laparoscopy in benign gynecologic surgery? A systematic review of randomized clinical trials. Minerva Obstet Gynecol. (2021). doi: 10.23736/s2724-606x.21.04957-5
6. Sangnier E, Lallemant M, Gnofam M, Bednarczyk L, Mereb E, Graesslin O, et al. Single port laparoscopy (SPL): retrospective study evaluating postoperative pain in comparison with conventional laparoscopy (CL). J Gynecol Obstet Hum Reprod. (2018) 47(8):365–9. doi: 10.1016/j.jogoh.2018.04.006
7. Schmitt A, Crochet P, Knight S, Tourette C, Loundou A, Agostini A. Single-port laparoscopy vs conventional laparoscopy in benign adnexal diseases: a systematic review and meta-analysis. J Minim Invasive Gynecol. (2017) 24(7):1083–95. doi: 10.1016/j.jmig.2017.07.001
8. Vonk Noordegraaf A, Anema JR, Louwerse MD, Heymans MW, van Mechelen W, Brölmann HA, et al. Prediction of time to return to work after gynaecological surgery: a prospective cohort study in The Netherlands. BJOG. (2014) 121(4):487–97. doi: 10.1111/1471-0528.12494
9. So KA, Lee JK, Song JY, Kim JW, Lee NW, Ki KD, et al. Tissue injuries after single-port and multiport laparoscopic gynecologic surgeries: a prospective multicenter study. Exp Ther Med. (2016) 12(4):2230–6. doi: 10.3892/etm.2016.3600
10. Abu Saadeh F, Norris L, O’Toole S, Gleeson N. Venous thromboembolism in ovarian cancer: incidence, risk factors and impact on survival. Eur J Obstet Gynecol Reprod Biol. (2013) 170(1):214–8. doi: 10.1016/j.ejogrb.2013.06.004
11. Ramirez PT, Frumovitz M, Pareja R, Lopez A, Vieira M, Ribeiro R, et al. Minimally invasive versus abdominal radical hysterectomy for cervical cancer. N Engl J Med. (2018) 379(20):1895–904. doi: 10.1056/NEJMoa1806395
12. Wang SY, Yin L, Guan XM, Xiao BB, Zhang Y, Delgado A. Single Port Transumbilical Laparoscopic Surgery versus Conventional Laparoscopic Surgery for Benign Adnexal Masses: A Retrospective Study of Feasibility and Safety. Chin Med J (Engl). (2016) 129(11):1305–10. doi: 10.4103/0366-6999.182829
13. Richards L, Healey M, Cheng C, Reddington C, Robson-Hamond C, Dior U. Risk factors and outcomes of conversion to open surgery in benign gynecologic laparoscopies: a case-control study. J Minim Invasive Gynecol. (2021) 28(10):1786–94. doi: 10.1016/j.jmig.2021.03.013
14. Huff K, Aref-Adib M, Magama Z, Vlachodimitropoulou E, Oliver R, Odejinmi F. Returning to work after laparoscopic myomectomy: a prospective observational study. Acta Obstet Gynecol Scand. (2018) 97(1):68–73. doi: 10.1111/aogs.13246
15. Al-Badawi IA, AlOmar O, Albadawi N, Abu-Zaid A. Single-port laparoscopic surgery for benign salpingo-ovarian pathology: a single-center experience from Saudi Arabia. Ann Saudi Med. (2016) 36(1):64–9. doi: 10.5144/0256-4947.2016.26.1.1200
16. Wordliczek J, Zajaczkowska R, Dziki A, Jackowski M, Richter P, Woron J, et al. Postoperative pain relief in general surgery—recommendations of the Association of Polish Surgeons, Polish Society of Anaesthesiology and Intensive Therapy, Polish Association for the Study of Pain and Polish Association of Regional Anaesthesia and Pain Treatment. Pol Przegl Chir. (2019) 91(1):47–68. doi: 10.5604/01.3001.0013.1088
17. Kaye AD, Urman RD, Cornett EM, Hart BM, Chami A, Gayle JA, et al. Enhanced recovery pathways in orthopedic surgery. J Anaesthesiol Clin Pharmacol. (2019) 35(Suppl 1):S35–S9. doi: 10.4103/joacp.JOACP_35_18
18. Tolner EA, Chen SP, Eikermann-Haerter K. Current understanding of cortical structure and function in migraine. Cephalalgia. (2019) 39(13):1683–99. doi: 10.1177/0333102419840643
19. Bisch S, Nelson G, Altman A. Impact of nutrition on enhanced recovery after surgery (ERAS) in gynecologic oncology. Nutrients. (2019) 11(5):1088. doi: 10.3390/nu11051088
20. Liu X, Li JB, Shi G, Guo R, Zhang R. Systematic review of single-incision versus conventional multiport laparoscopic surgery for sigmoid colon and rectal cancer. World J Surg Oncol. (2018) 16(1):220. doi: 10.1186/s12957-018-1521-4
21. Ki EY, Park EK, Jeong IC, Bak SE, Hwang HS, Chung YH, et al. Laparoendoscopic single site surgery for the treatment of huge ovarian cysts using an angiocatheter needle. Yonsei Med J. (2019) 60(9):864–9. doi: 10.3349/ymj.2019.60.9.864
22. Scheib SA. A laparoendoscopic single-site surgical approach to laparoscopic salpingectomy. J Minim Invasive Gynecol. (2018) 25(2):326–7. doi: 10.1016/j.jmig.2017.03.013
Keywords: single-port laparoscopic surgery (SPLS), benign, ovarian tumor, return to work (RTW), surgery
Citation: Tang Y, Wen M, Su B, Wang H, Zheng X, Yang M, Yin S, Xu F and Hu H (2022) Early return to work: Single-port vs. multiport laparoscopic surgery for benign ovarian tumor. Front. Surg. 9:1005898. doi: 10.3389/fsurg.2022.1005898
Received: 28 July 2022; Accepted: 13 October 2022;
Published: 8 October 2022.
Edited by:
Vito Andrea Capozzi, University Hospital of Parma, ItalyReviewed by:
Elisa Scarpelli, University Hospital of Parma, ItalyMirko Bertozzi, Hospital of Santa Maria della Misericordia in Perugia, Italy
© 2022 Tang, Wen, Su, Wang, Zheng, Yang, Yin, Xu and Hu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hui-quan Hu MzYzMTE3NzNAcXEuY29t
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Obstetrics and Gynecological Surgery, a section of the journal Frontiers in Surgery.
 Ying Tang
Ying Tang Ming-bo Wen
Ming-bo Wen Bin Su1
Bin Su1 Fan Xu
Fan Xu