- 1Department of Orthopedics, Sichuan Provincial People's Hospital, Chengdu, China
- 2Department of Postgraduate, Chengdu Medical College, Chengdu, China
- 3Department of Interventional Therapy, Affiliated Hospital of Qinghai University, Xining, China
- 4Department of Postgraduate, Qinghai University, Xining, China
Background: This systematic review and meta-analysis was performed to summarize available evidence of anterior transposition of the ulnar nerve for patients with distal humerus fractures.
Materials and Methods: The databases were searched from PubMed, Cochrane, Embase, Scopus, Web of Science, Chinese National Knowledge Infrastructure (CNKI), Chongqing VIP Database (VIP), and Wan Fang Database up to June 2022. The clinical outcome included operation time, fracture healing time, hospital stays, elbow joint function, and ulnar neuritis rate. Statistical analysis was performed with Review Manager 5.3 (Cochrane Collaboration).
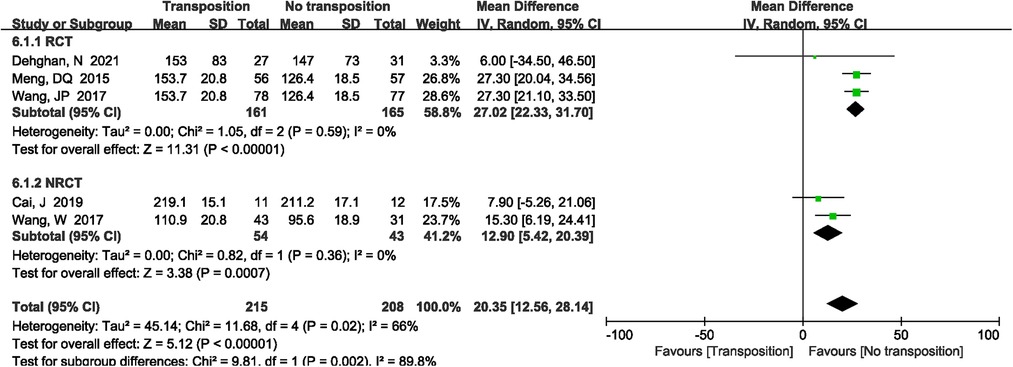
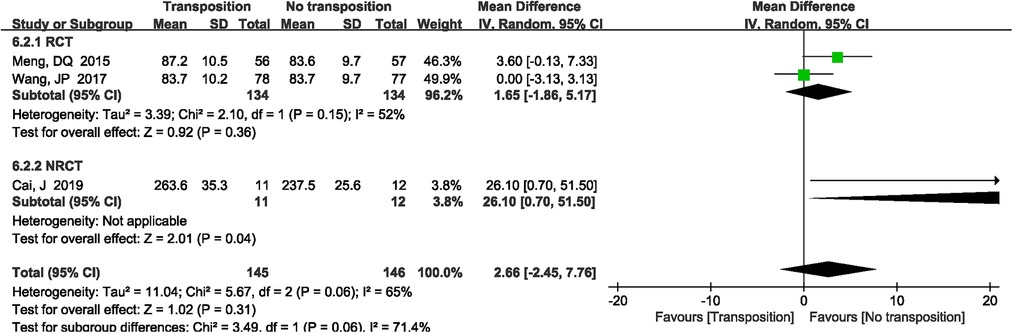
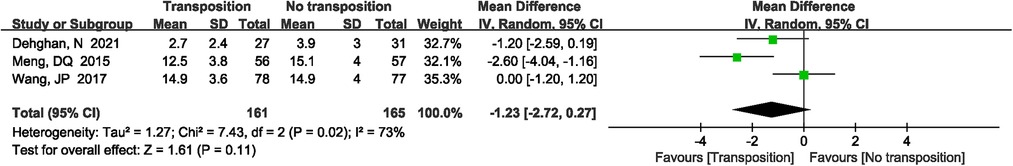
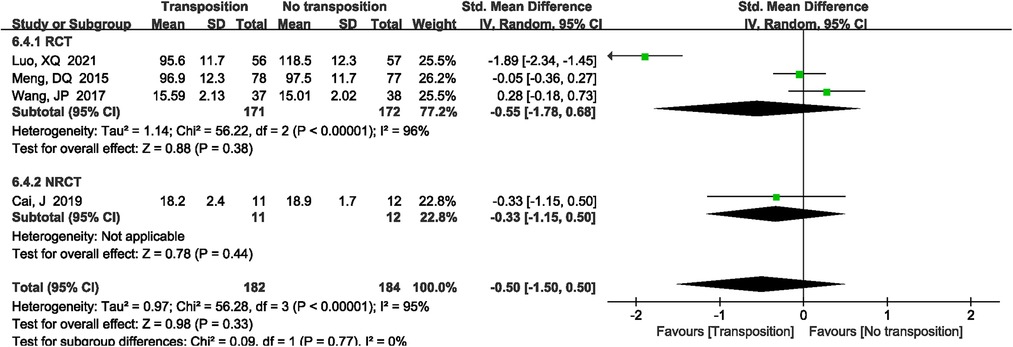
Results: A total of 17 studies were included (8 RCTs and 9 retrospective studies), and 1280 patients were analyzed. The results of this meta-analysis showed anterior transposition group had longer operation time (MD = 20.35 min, 95%CI: 12.56–28.14, P < 0.00001). There was no significant difference in fracture healing time (SMD = −0.50, 95%CI: −1.50–0.50, P = 0.33), hospital stays (MD = −1.23 days, 95%CI: −2.72–−0.27, P = 0.11), blood loss (MD = 2.66 ml, 95%CI: −2.45–7.76, P = 0.31), and ulnar neuritis rate (OR = 1.23, 95%CI: 0.63–2.42, P = 0.54) between two groups. Finally, elbow joint motion, elbow joint function, fracture nonunion, and post-operative infection (P > 0.05) between two groups were not significantly statistic difference.
Conclusion: This meta-analysis showed that anterior transposition group is not superior to non-transposition group for patients with distal humerus fractures without ulnar nerve injury. On the contrary, non-transposition group have shorter operation time than that of anterior transposition group. Non-transposition group did not increase the post-operative ulnar neuritis rate. Therefore, both anterior transposition group and non- transposition group are the treatment options for patients with distal humerus fractures without ulnar nerve injury. Besides, these findings need to be further verified by multi-center, double-blind, and large sample RCTs.
1. Introduction
Elbow joint fractures account for approximately 7% of adult fractures, with distal humerus fractures accounting for 30% of all elbow joint fractures (1). When open reduction and internal fixation (ORIF) is performed, several complications such as fracture nonunion, loss of functional motion, and ulnar neuropathy have been reported (2, 3). Ulnar neuropathy in particular poses a unique challenge. The incidence of ulnar neuropathy following ORIF of distal humerus fractures has been reported between 0%–51% in previously described studies (4). Some literatures have reported that when the patients with distal humerus fracture complicated with ulnar nerve injury, anterior transposition of the ulnar nerve was more effective in promoting postoperative nerve rehabilitation (5, 6). Duo to the ideal clinical effect of anterior transposition of the ulnar nerve, most orthopedic surgeons have taken an anterior transposition of the ulnar nerve as a treatment for distal humeral fractures to reduce the possibility of postoperative ulnar nerve disorders (7).
However, in recent years, there has been some different views on whether the anterior transposition of the ulnar nerve is necessary in patients without ulnar nerve injuries. Chen et al. (8) reported a retrospective study of 137 distal humeral fractures patients who had no ulnar nerve injuries before surgery, and their results showed that the incidence of postoperative ulnar nerve disorders was 4 times higher in the anterior transposition group than in the non-transposition group. On the contrary, Ruan et al. (9) reported that according to Bishop rating system, postoperative excellent results of ulnar nerve function were achieved in patients (86.7%) in the transposition group, compared with patients (57.1%) in the decompression group (P < 0.05).
However, it is still controversial whether the anterior transposition of the ulnar nerve is necessary for patients without ulnar nerve injuries before surgery. We aim to conduct a systematic review and meta-analysis including current literature to assess the benefits and risks by comparing anterior transposition of the ulnar nerve with non-transposition treatment for patients with distal humerus fractures.
2. Material and methods
2.1. Study design
This meta-analysis was by the PRISMA statement (10).
2.2. Search strategy
The following relational databases were searched up to June 2022 such as PubMed, Cochrane, Embase, Scopus, Web of Science, CNKI, VIP, and Wan Fang. All RCTs and retrospective studies comparing anterior transposition of the ulnar nerve and non-transposition for the treatment of distal humerus fractures were collected. The retrieval method adopted the combination of subject words and free words, and English retrieval words and Chinese versions include: (((Anterior ulnar nerve [Title/Abstract]) OR (Ulnar neuritis [Title/Abstract])) OR (Ulnar nerve [Mesh])) AND ((((humerus fracture [Mesh]) OR (Humeral supracondylar fracture [Title/Abstract])) OR (Humeral intercondylar fracture [Title/Abstract])) OR (Distal humerus fractures [Title/Abstract])). In addition, the references of the included literature were reviewed to supplement the relevant studies.
2.3. Inclusion and exclusion criteria
2.3.1. Inclusion criteria
Studies were eligible for inclusion if they met the following criteria: (1) P: all patients were diagnosed by clinical and radiographic confirmation of distal humerus fractures without ulnar nerve injury. (2) I: interventions group used a plate fixation plus anterior transposition of the ulnar nerve for patients with distal humerus fractures. (3) C: control method used a plate fixation plus non-transposition of the ulnar nerve for patients with distal humerus fractures. (4) O: availability of adequate raw data for categorical outcomes. (5) S: study design included RCTs and retrospective studies.
2.3.2. Exclusion criteria
Studies were ineligible if they met the following criteria: (1) studies cannot extract data studies so that the study could not be analyzed; (2) duplicate studies; (3) other interventions or no-operation treatment; (4) relevant clinical outcome were not reported; (5) animal studies, duplicate publications of one trial, case report, case series, letter, technology note, commentaries, reviews, withdraw trails and meta-analysis.
2.4. Data extraction
Two researchers independently read potential studies based on the inclusion and exclusion criteria. The data were extracted as follows: the basic information of the study sample (name, year, gender, the number of participants, intervention method, control method, etc.), study design type (RCTs and NRCTs), study duration, AO fracture classification, Surgery approach etc. What's more, we extracted the following data from each selected study: operation time, blood loss, hospital stays, elbow joint function, elbow joint motion, fracture healing time, and ulnar neuritis rate. When information was missing, we attempted to contact the primary author via email to seek clarification or exclude the study.
2.5. Risk of bias assessment
Using the Cochrane risk of bias tool to evaluated the risk of bias in the included studies for RCTs. And using Newcastle-Ottawa Scale to evaluated retrospective study. The studies with scored ≥ 6 were considered to be high-quality articles for retrospective studies. The bias assessment was conducted by two independent researchers. Any unresolved disagreements between reviewers were resolved through discussion or assessment by a third reviewer.
2.6. Statistical analysis
The Revman 5.4 software package was used. We reported continuous outcomes for mean difference (MD) or standardized mean difference (SMD) with 95% confidence interval (CI), and the dichotomous outcomes were reported by odds ratio (odds ratio, OR) with 95% CI. Chi-square test was used to test the heterogeneity of the included research results. There was heterogeneity between studies if P < 0.1 or I2 > 50%, and a random effect model was used. If P ≥ 0.1 and I2 ≤ 50%, it showed that there was no heterogeneity. Therefore, a fixed-effect model was used. We also performed a sensitivity analysis to determine the resource of the heterogeneity. Publication bias was assessed by the funnel plot.
3. Results
3.1. Search result
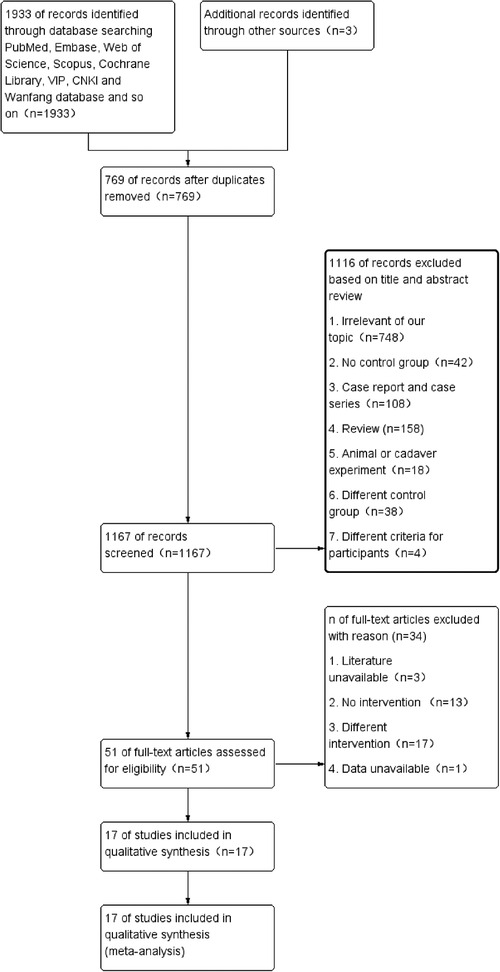
The initial search produced 1936 records, from which we excluded 769 records due to the duplication. After reading the full-text articles, 17 potentially eligible studies were included. Figure 1 shows the selection algorithm, numbers of included and excluded studies. All titles, abstracts, and text were dually and independently reviewed by the authors based on the inclusion and exclusion criteria to minimize bias.
3.2. Study characteristic
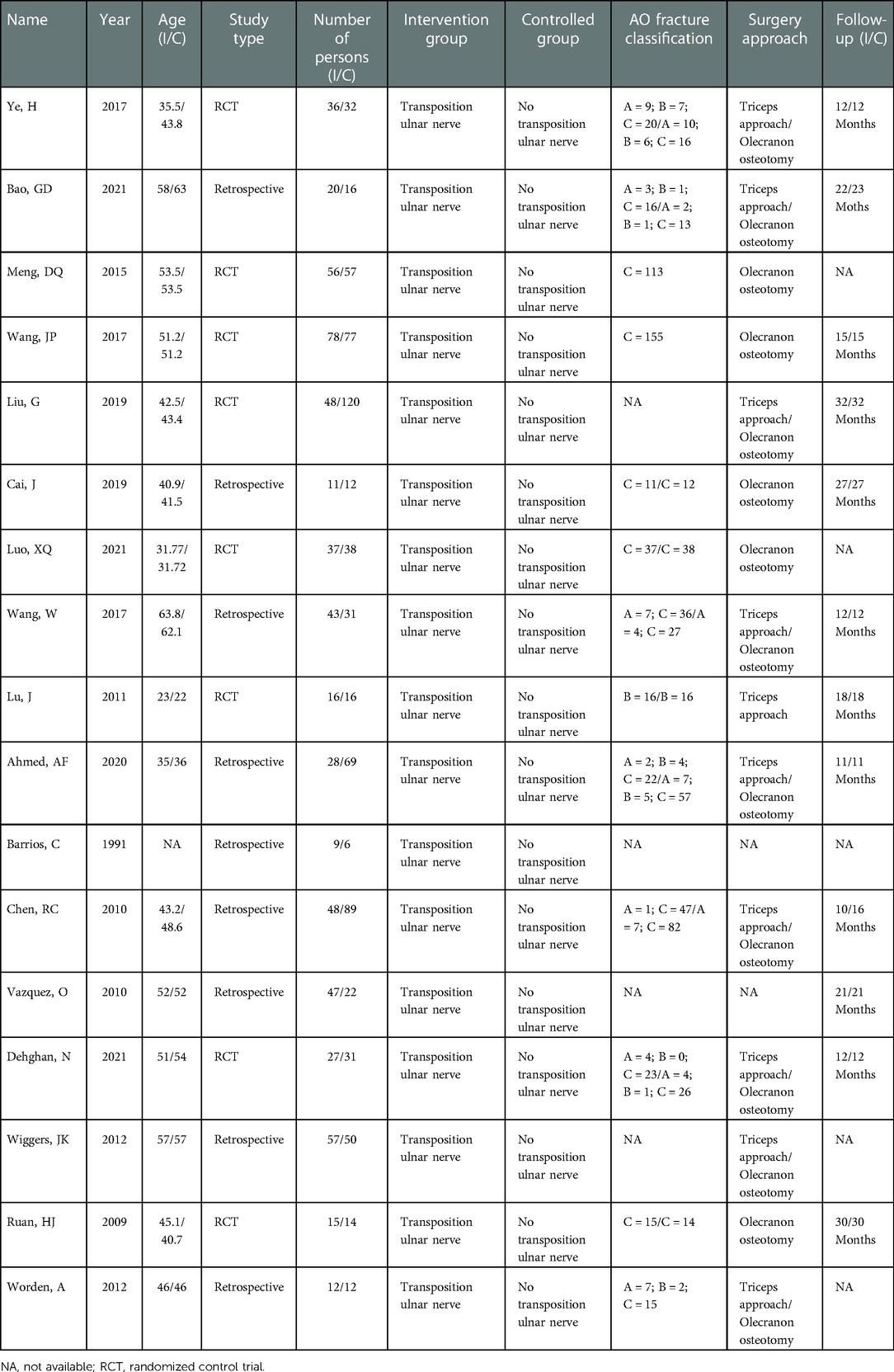
Among the included studies, 8 were RCTs (9, 11–17) and 9 were retrospective studies (7, 8, 18–24). There were 1280 patients included in this meta-analysis. After the application of the inclusion criteria, 8 trials published in English and 9 trials published in Chinese were included in this meta-analysis. The main basic characteristics of the included literature were shown in Table 1.
3.3. The bias risk assessment results of the included studies
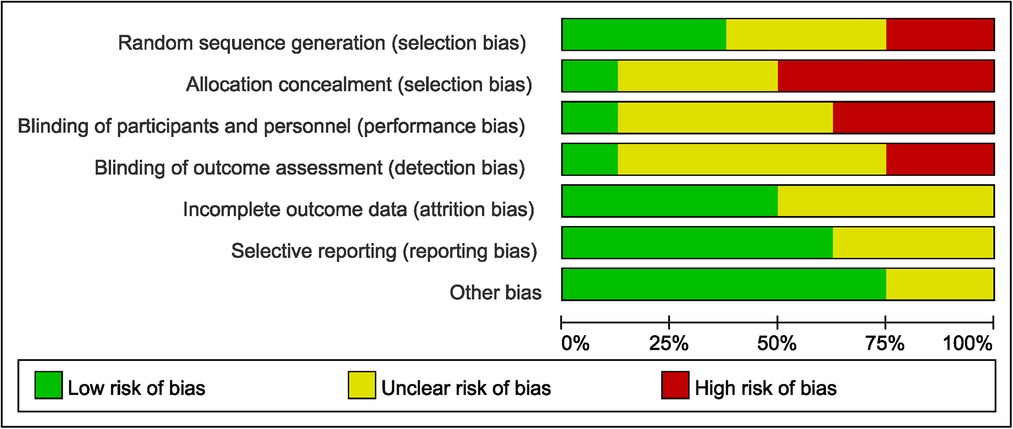
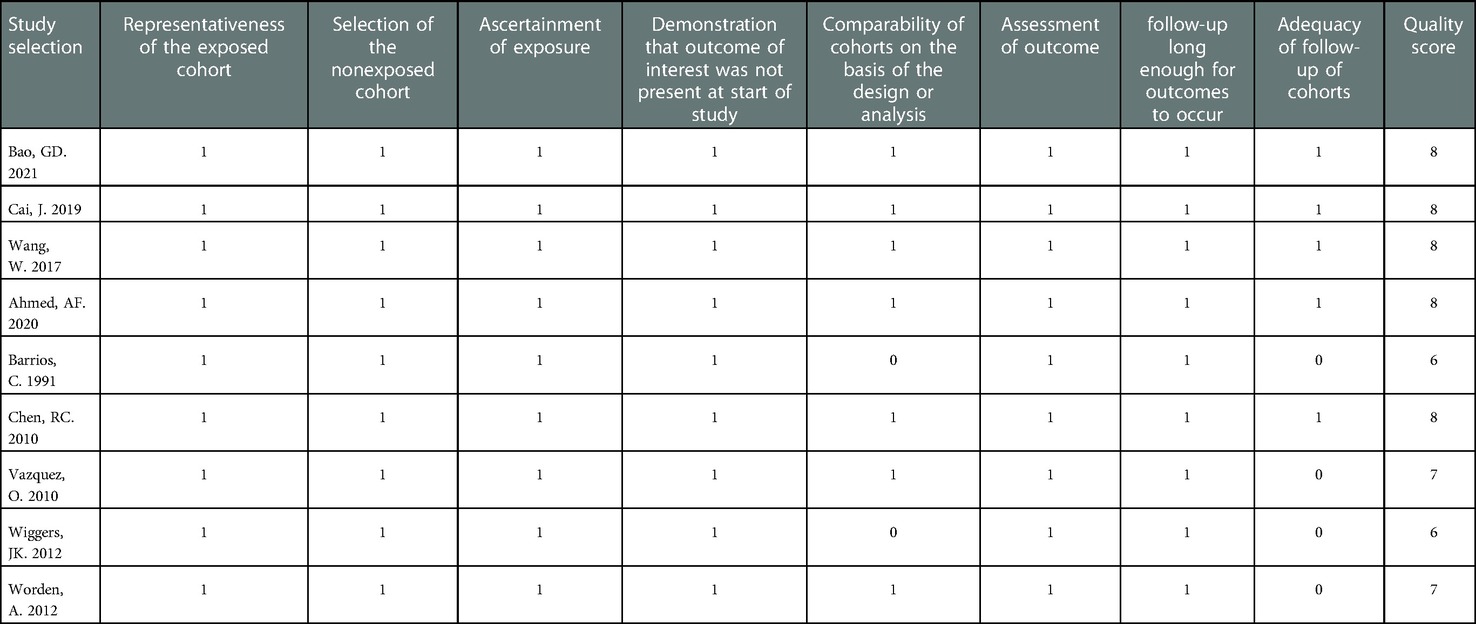
In the retrospective studies, NOS scale was used to evaluate the risk of bias. The included retrospective studies met most of the quality assessment criteria, and the total scores of all studies were ≥ 6, which indicated a low risk of bias. The detail of the information could be seen in Table 2. RCTs were evaluated by using the Cochrane risk of bias tool. The quality assessment of included studies was shown in Figure 2 for details.
3.4. Meta-analysis results
3.4.1. Operation time
A total of 5 studies (12, 13, 17, 19, 20) reported the operation time. There was significant heterogeneity in the study (P = 0.02, I2 = 66%). Random effects model was performed. The results showed that anterior transposition group had longer operation time compared with non-transposition of the ulnar nerve (MD = 20.35 min, 95%CI: 12.56–28.14, P < 0.00001, Figure 3). The subgroup analysis showed that non-transposition group had lower operation time for RCTs and retrospective studies, and there was no significant heterogeneity in the study (I2 = 0%, Figure 3).
3.4.2. Blood loss
A total of 3 studies (12, 13, 19) reported intraoperative blood loss. There was significant heterogeneity in the study (P = 0.06, I2 = 65%). Random effects model was performed. Meta-analysis results showed that there was no significant difference between anterior transposition group and non-transposition group (MD = 2.66 ml, 95%CI: −2.45–7.76, P = 0.31, Figure 4).
3.4.3. Hospital stays
A total of 3 studies (12, 13, 17) reported the hospital stays. There was significant heterogeneity in the study (P = 0.02, I2 = 73%). Random effects model was performed. Results showed that anterior transposition group was not superior to non-transposition group (MD = −1.23 day, 95%CI: −2.72 ∼ 0.27, P = 0.11, Figure 5).
3.4.4. Fracture healing time
A total of 4 studies (12, 13, 15, 19) reported fracture healing time. There was significant heterogeneity in the study (P < 0.00001, I2 = 95%). Random effects model was performed. There was no significant difference between two groups (SMD = −0.50, 95%CI: −1.50–0.50, P = 0.33, Figure 6).
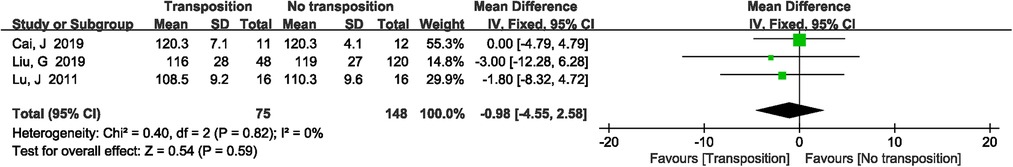
3.4.5. Elbow joint motion
A total of 3 studies (14, 16, 19) reported the elbow joint motion. There was no significant heterogeneity in the study (P = 0.82, I2 = 0%). Fixed effects model was performed. There was no significant difference between two groups (MD = −0.98, 95%CI: −4.55–2.58, P = 0.59, Figure 7).
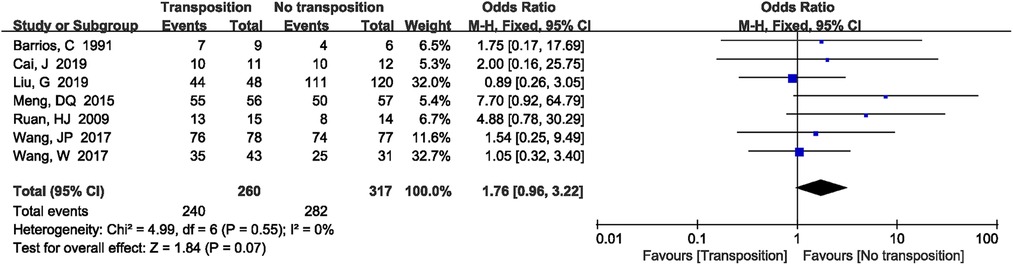
3.4.6. Elbow joint function
A total of 7 studies (9, 12–14, 19, 20, 22) reported elbow joint function. There was no significant heterogeneity in the study (P = 0.55, I2 = 0%). Fixed effects model was performed. There was no significant difference between two groups (OR = 1.76, 95%CI: 0.96–3.22, P = 0.07, Figure 8).
3.5. Safety
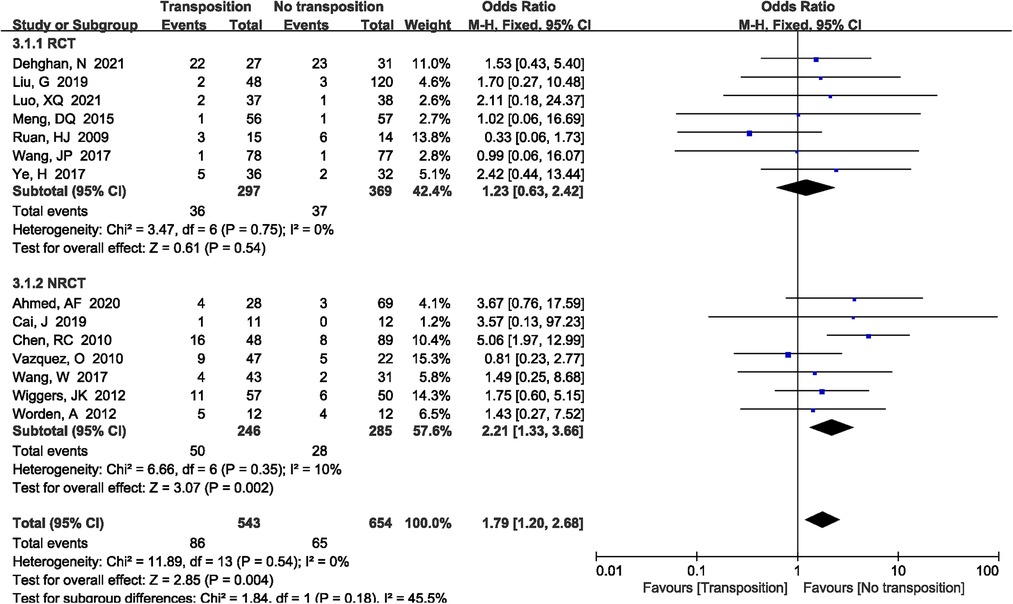
3.5.1. Ulnar neuritis
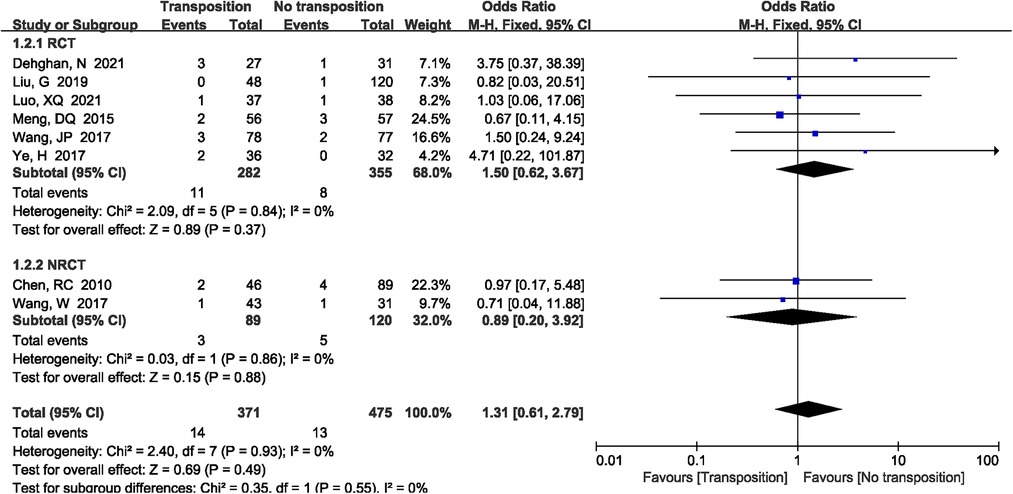
A total of 14 studies (7–9, 11–15, 17, 19–21, 23, 24) reported the incidence of ulnar neuritis included in the study. The results demonstrated that non-transposition group had lower ulnar neuritis rate compared with anterior transposition group (OR = 1.79, 95%CI: 1.20–2.68, P = 0.004, Figure 9). There was no significant heterogeneity (P = 1.00, I2 = 0%), and the fixed-effects model was performed. However, the subgroup analysis showed that there was no significant difference when only RCTs were included between two group (P = 0.54).
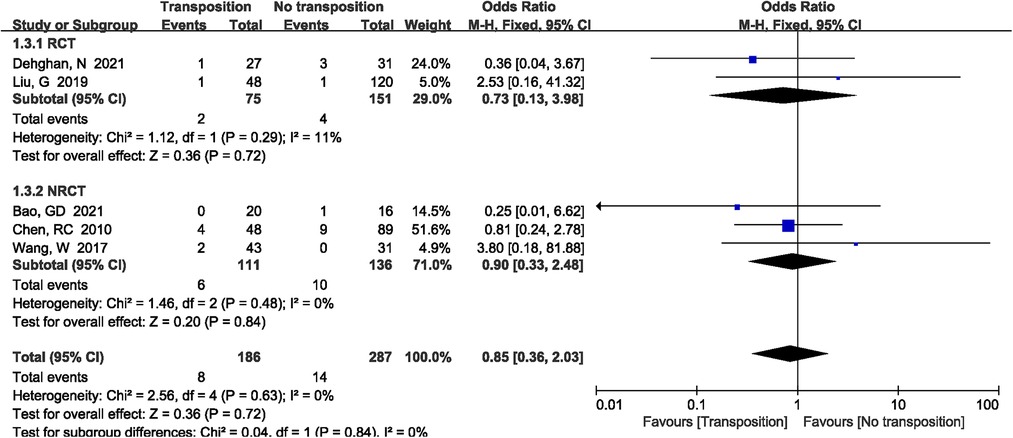
3.5.2. Humerus nonunion
A total of 5 studies (8, 14, 17, 18, 20) reported the incidence of humerus nonunion included in the study. The results demonstrated that there was no significant difference between two groups (OR = 0.85, 95%CI: 0.36–2.03, P = 0.72, Figure 10). There was no significant heterogeneity (P = 0.63, I2 = 0%), and the fixed-effects model was performed.
3.5.3. Infection
A total of 8 studies (8, 11–15, 17, 20) reported the incidence of infection included in the study. The results demonstrated that there was no significant difference between two groups (OR = 1.31, 95%CI: 0.61–2.79, P = 0.49, Figure 11). There was no significant heterogeneity (P = 0.93, I2 = 0%), and the fixed-effects model was performed.
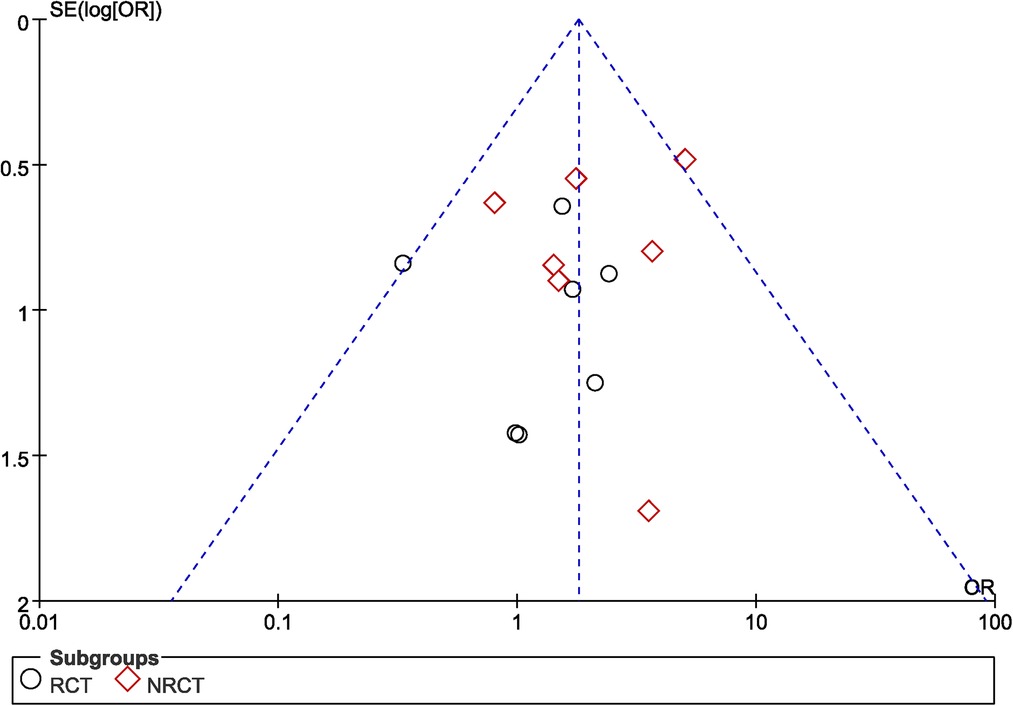
3.6. Publication bias
The funnel plot was used to evaluate the publication bias of studies. For the study of ulnar neuritis rate (Figure 12), the funnel plot was not symmetrical. It indicated the possibility of publication bias.
4. Discussion
Despite advances in the management of distal humerus fractures, complications, such as ulnar neuropathy still pose a challenge to clinicians. Regardless of whether there was ulnar nerve injury before surgery, orthopedic surgeons should routinely dissociate the ulnar nerve before reducing the fracture to protect the ulnar nerve, fully expose the fracture site, and avoid the difficulties of internal fixation and implantation (25–27). At present, many scholars believed that if there is ulnar nerve injury before surgery, it is necessary to take an anterior transposition of the ulnar nerve to avoid compression of the ulnar nerve, which can reduce the occurrence of postoperative ulnar neuritis (28, 29). However, in recent years, there were many different opinions on whether anterior transposition of the ulnar nerve was necessary in patients without ulnar nerve injury before surgery, as some study reported higher incidence of ulnar neuritis when transposition was performed (8). According to these scholars, compared with the anterior transposition of the ulnar nerve, only in site placement of the ulnar nerve could not only simplify surgery procedures, but also reduce the probability of iatrogenic injury. Therefore, the intraoperative management of the ulnar nerve in patients without preoperative ulnar nerve injury was controversial. The purpose of this meta-analysis was to evaluate the benefits and risks by comparing anterior transposition of the ulnar nerve with non-transposition treatment for patients with distal humerus fractures.
Our meta-analysis demonstrated that transposition group and non-transposition group had no statistical significance in blood loss, hospital stays, and fracture healing time (respectively P = 0.31, P = 0.11 and P = 0.33). However, we found that non-transposition group had shorter operation time than transposition group (P < 0.00001). Compared with in situ placement of the ulnar nerve, anterior transposition of the ulnar nerve was an additional surgical procedure on the basis of ORIF, so the operation time was relatively longer. Anterior transposition of ulnar nerve did not increase blood loss, hospital stays, and fracture healing time, as these were often related to the degree of fracture, soft tissue injury, and the level of operation of the surgeon (30). What's more, we found that there was no heterogeneity after subgroup analysis for operation time. However, blood loss, hospital stays, and fracture healing time had a large heterogeneity, and subgroup analysis also found no the source of heterogeneity. Therefore, the source of heterogeneity is mainly related to the difference of surgical level among different surgeons.
After distal humerus injury, there was a large number of local bone defect, and there was a risk of delayed or even non-union (31, 32). Some studies have shown that the delay fracture recovery rate could reach 2%–10% after ORIF (33). What's more, Chen RC et al. (8) reported that anterior transposition group and non-transposition group had no statistical difference in nonunion (respectively, 9.1% vs. 11.3%, P = 0.73). Our meta-analysis also demonstrated that anterior transposition group was not superior to non-transposition group in fracture nonunion. Fracture nonunion often has a certain relationship with infection. Due to the severe soft tissue injury of the elbow joint, the relatively thin soft tissue envelope, and the shear forces generated during early exercise, there is a risk of serious wound complications in the elbow joint after surgery (34). Lawrence et al. reported 89 distal humerus fractures which were treated with internal fixation. Fourteen patients (15.7%) developed a severe wound complication requiring on average 2.5 (rang, 1–6) additional surgical procedures (6). A multiple-center randomized controlled trial also demonstrated that 3 patients in the transposition group and 1 patients in the situ group had superficial wound infections (respectively, 11.11% vs. 3.23%), which was no statistical difference between two groups (17). Our meta-analysis also found same clinical outcomes for wound infections between two groups.
Three literatures evaluated elbow joint function according to Mayo scores, and four literatures evaluated elbow joint function according to Cassebaum score. The Mayo Elbow Performance Score (MEPS) and Cassebaum score were used as an objective measure of overall outcome by assessing motion ability, joint stability and pain level (35, 36). Most of the studies on improving postoperative elbow function focus on surgical approach, internal fixation device and functional rehabilitation exercise. Some studies had reported that the average MEPS score was slightly better in the triceps sparing approach group (86.56 ± 10.66) compared with olecranon osteotomy approach group (83.57 ± 10.96) but it was statistically not significant (P = 0.289) (30). And postoperative rehabilitation exercise was an important treatment that could not be ignored. Early functional exercise could prevent joint ossification and bone loss, and could accelerate the recovery of elbow function (37). Therefore, our meta-analysis also found that anterior transposition group was no superior non-transposition group in elbow joint function and elbow joint motion (respectively, P = 0.07 and P = 0.59).
Treatment of the ulnar nerve remains an unsettled issue. Some studies showed a complication rate of up to 44% in patients with distal humerus fracture after internal fixation, including neuropathies, mechanical failure and wound dehiscence (38). However, the ulnar neuropathy as a complication of distal humerus fracture has been reported with a magnitude ranging from 0% to 51% (7, 39). Shin et al. reported a 22% rate of postoperative ulnar nerve palsies despite performing adequate release and nerve transposition (40). The ulnar neuropathies were caused by the scar tissue development, thickening in the fibro-osseous tunnel, and swelling. Although anterior transposition nerve could reduce the incidence of postoperative ulnar neuritis, some authors found that anterior transposition ulnar nerve actually increased the incidence of postoperative ulnar neuritis. Because anterior transposition of the ulnar nerve had longer operation time compared with in situ placement group, which might increase the duration of the tourniquet. Thus, the ulnar nerve ischemia and hypoxia time are prolonged, which increased the incidence of ulnar neuritis. In a recent meta-analysis, it found that incidence of neuropathy in the transposition group was higher (23.5%) as compared with the in situ group (15.3%) as it only included five retrospective studies (41). What's more, our meta-analysis also showed that anterior transposition group had higher the incidence of postoperative ulnar neuritis than non-transposition group (P = 0.004). However, the subgroup analysis showed that there was no significant difference when only RCTs were included between two group (P = 0.54). What's more, randomized controlled trials have a higher level of experimental evidence, and it can reduce selection bias, report bias, and observation bias. Therefore, the meta-analysis demonstrated that non-transposition group did not add the incidence of postoperative ulnar neuritis compared with anterior transposition group.
However, there are also a few limitations in our study: (1) Some pooled results from included studies were strongly subjective, which may influence the results due to the different experiences from doctors. (2) Most of the included studies were retrospective studies, which have a great impact on the experimental results. (3) Inclusion and exclusion criteria of some studies are different. (4) Heterogeneity among the included studies was unavoidable because of racial differences, age difference, and fracture type, and surgical approach. Therefore, physicians around the world should be careful to interpret our results in clinical practice.
5. Conclusion
Current evidence suggests that anterior transposition of the ulnar nerve is not superior to non-transposition of the ulnar nerve for patients with distal humerus fractures. On the contrary, non-transposition group had shorter operation time than anterior transposition group and non-transposition group might decrease the incidence of postoperative ulnar neuritis. In patients with postoperative ulnar neuropathy after ORIF of the distal humerus, anterior transposition and non-transposition groups seems to be an effective treatment. Considering that dynamic stabilization device group also has its limitations, large sample, double-blind and multi-center RCTs are needed to verify our conclusion.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author contributions
TL and JY: wrote the original manuscript; JH and C X: collected relevant data; QR, FW, and XL: were responsible for English editing and reviewing the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was financially supported by the Sichuan Provincial People's Hospital Research Fundings (30420200035 and ZYGX2021YGLH021), and Key Project of Sichuan Science and Technology Department (2021YFS0383).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Pollock JW, Faber KJ, Athwal GS. Distal humerus fractures. Orthop Clin North Am. (2008) 39(2):187–200. doi: 10.1016/j.ocl.2007.12.002
2. McKee MD, Veillette CJ, Hall JA, Schemitsch EH, Wild LM, McCormack R, et al. A multicenter, prospective, randomized, controlled trial of open reduction–internal fixation versus total elbow arthroplasty for displaced intra-articular distal humeral fractures in elderly patients. J Shoulder Elbow Surg. (2009) 18(1):3–12. doi: 10.1016/j.jse.2008.06.005
3. Ring D, Jupiter JB. Complex fractures of the distal humerus and their complications. J Shoulder Elbow Surg. (1999) 8(1):85–97. doi: 10.1016/S1058-2746(99)90063-0
4. Huang JI, Paczas M, Hoyen HA, Vallier HA. Functional outcome after open reduction internal fixation of intra-articular fractures of the distal humerus in the elderly. J Orthop Trauma. (2011) 25(5):259–65. doi: 10.1097/BOT.0b013e3181dfd348
5. McKee MD, Jupiter JB, Bosse G, Goodman L. Outcome of ulnar neurolysis during post-traumatic reconstruction of the elbow. J Bone Joint Surg Br. (1998) 80(1):100–5. doi: 10.1302/0301-620X.80B1.0800100
6. Lawrence TM, Ahmadi S, Morrey BF, Sánchez-Sotelo J. Wound complications after distal humerus fracture fixation: incidence, risk factors, and outcome. J Shoulder Elbow Surg. (2014) 23(2):258–64. doi: 10.1016/j.jse.2013.09.014
7. Worden A, Ilyas AM. Ulnar neuropathy following distal humerus fracture fixation. Orthop Clin North Am. (2012) 43(4):509–14. doi: 10.1016/j.ocl.2012.07.019
8. Chen RC, Harris DJ, Leduc S, Borrelli JJ, Tornetta P, Ricci WM. Is ulnar nerve transposition beneficial during open reduction internal fixation of distal humerus fractures? J Orthop Trauma. (2010) 24(7):391–4. doi: 10.1097/BOT.0b013e3181c99246
9. Ruan HJ, Liu JJ, Fan CY, Jiang J, Zeng BF. Incidence, management, and prognosis of early ulnar nerve dysfunction in type C fractures of distal humerus. J Trauma. (2009) 67(6):1397–401. doi: 10.1097/TA.0b013e3181968176
10. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. Br Med J. (2009) 339:b2700. doi: 10.1136/bmj.b2700
11. Ye H, Lin QR, Yao XD, Lin JK, Wu WH. Clinical study on whether the ulnar nerve is taken an anterior transposition during operation for distal humeral fractures. Chin J Hand Surg. (2017) 33(2):142–3. doi: 10.3760/cma.j.issn.1005-054x.2017.02.025
12. Meng DQ, Liu DC, Zhang XC. Effect analysis of anterior transposition of the ulnar nerve for double locking plate fixation in the treatment of patients with humeral intercondylar fracture. J Trauma Surg. (2015) 17(1):36–8.
13. Wang JP. Effect analysis of anterior transposition or not of the ulnar nerve for double plate fixation in the treatment of patients with humeral intercondylar fracture. Master's degree: Tianjin Medical university. (2017).
14. Liu G, Li T, Chen C, Zha YJ, Gong MQ, Jiang XY. Is anterior transposition of ulnar nerve beneficial during open reduction and internal fixation for intercondylar humerus fractures. China J Orthop Trauma. (2019) 32(4):296–301. doi: 10.3969/j.issn.1003-0034.2019.04.002
15. Luo XQ. Comparison the clinical effect through olecranon osteotomy of in situ reinforcing ulnar nerve and anterior transposition the ulnar nerve for C2 and C3 humeral intercondylar fractures. Medical Forum. (2021) 25(20):2835–6. doi: 10.19435/j.1672-1721.2021.20.012
16. Lu J. Management and prognosis of the ulnar nerve in aged type B2 distal humerus fractures. Chin Comm Doctors. (2011) 32(13):271–2. doi: 10.3969/j.issn.1007-614x.2011.32.265
17. Dehghan N, Nauth A, Hall J, Vicente M, McKee MD, Schemitsch EH. In situ placement versus anterior transposition of the ulnar nerve for distal humerus fractures treated with plate fixation: a multicenter randomized controlled trial. J Orthop Trauma. (2021) 35(9):465–71. doi: 10.1097/BOT.0000000000002066
18. Bao GD. Management and prognosis of ulnar nerve after open reduction and internal fixation of distal humerus fracture. Master's degree: Wenzhou Medical University. (2021).
19. Cai J, Qi YJ, Gu XM. Efficacy comparison between plate fixation with in situ reinforcing ulnar nerve and anterior transposition for humeral intercondylar fracture. Chin J Trauma. (2019) 35(7):638–43. doi: 10.3760/cma.j.issn.1001-8050.2019.07.010
20. Wang W, Huang J, Liu LM. Therapeutic effect of ulnar nerve with or without transposition during open reduction and internal fixation of distal humerus fractures. Chin J Trauma. (2017) 33(5):404–7. doi: 10.3760/cma.j.issn.1001-8050.2017.05.004
21. Ahmed AF, Parambathkandi AM, Kong WJG, Salameh M, Mudawi A, Abousamhadaneh M, et al. The role of ulnar nerve subcutaneous anterior transposition during open reduction and internal fixation of distal humerus fractures: a retrospective cohort study. Int Orthop. (2020) 44(12):2701–8. doi: 10.1007/s00264-020-04745-0
22. Barrios C, Ganoza C, de Pablos J, Cañadell J. Posttraumatic ulnar neuropathy versus non-traumatic cubital tunnel syndrome: clinical features and response to surgery. Acta Neurochir. (1991) 110(1-2):44–8. doi: 10.1007/BF01402047
23. Vazquez O, Rutgers M, Ring DC, Walsh M, Egol KA. Fate of the ulnar nerve after operative fixation of distal humerus fractures. J Orthop Trauma. (2010) 24(7):395–9. doi: 10.1097/BOT.0b013e3181e3e273
24. Wiggers JK, Brouwer KM, Helmerhorst GT, Ring D. Predictors of diagnosis of ulnar neuropathy after surgically treated distal humerus fractures. J Hand Surg Am. (2012) 37(6):1168–72. doi: 10.1016/j.jhsa.2012.02.045
25. Min W, Anwar A, Ding BC, Tejwani NC. Open distal humerus fractures–review of the literature. Bull NYU Hosp Jt Dis. (2010) 68(4):257–61.21162702
26. Islam S U, Glover AW, Waseem M. Challenges and solutions in management of distal humerus fractures. Open Orthop J. (2017) 11:1292–307. doi: 10.2174/1874325001711011292
27. Athanaselis ED, Komnos G, Deligeorgis D, Hantes M, Karachalios T, Malizos KN, et al. Double plating in type C distal humerus fractures: current treatment options and factors that affect the outcome. Strategies Trauma Limb Reconstr. (2022) 17(1):7–13. doi: 10.5005/jp-journals-10080-1546
28. Schwartz A, Oka R, Odell T, Mahar A. Biomechanical comparison of two different periarticular plating systems for stabilization of complex distal humerus fractures. Clin Biomech. (2006) 21(9):950–5. doi: 10.1016/j.clinbiomech.2006.04.018
29. Wang KC, Shih HN, Hsu KY, Shih CH. Intercondylar fractures of the distal humerus: routine anterior subcutaneous transposition of the ulnar nerve in a posterior operative approach. J Trauma. (1994) 36(6):770–3. doi: 10.1097/00005373-199406000-00003
30. Ansari MF, Khan NA, Atif AM. Management of type 13C2 distal humerus fractures by olecranon osteotomy approach versus triceps sparing approach-our experience with sixty cases. Int Orthop. (2020) 44(12):2735–42. doi: 10.1007/s00264-020-04785-6
31. Ku KH, Baek JH, Kim MS. Risk factors for non-union after open reduction and internal fixation in patients with distal humerus fractures. J Clin Med. (2022) 11(10):2679. doi: 10.3390/jcm11102679
32. Hausman M, Panozzo A. Treatment of distal humerus fractures in the elderly. Clin Orthop Relat Res. (2004) 425:55–63. doi: 10.1097/01.blo.0000131485.47685.8c
33. Raja S, Mittal D, Bale S. Unstable nonunions of the distal part of the humerus. J Bone Joint Surg Am. (2004) 86(1):184.; author reply -5. doi: 10.2106/00004623-200401000-00030
34. Choudry UH, Moran SL, Li S, Khan S. Soft-tissue coverage of the elbow: an outcome analysis and reconstructive algorithm. Plast Reconstr Surg. (2007) 119(6):1852–7. doi: 10.1097/01.prs.0000259182.53294.67
35. Turchin DC, Beaton DE, Richards RR. Validity of observer-based aggregate scoring systems as descriptors of elbow pain, function, and disability. J Bone Joint Surg Am. (1998) 80(2):154–62. doi: 10.2106/00004623-199802000-00002
36. Puchwein P, Wildburger R, Archan S, Guschl M, Tanzer K, Gumpert R. Outcome of type C (AO) distal humeral fractures: follow-up of 22 patients with bicolumnar plating osteosynthesis. J Shoulder Elbow Surg. (2011) 20(4):631–6. doi: 10.1016/j.jse.2010.12.019
37. Cao J, Zheng HJ, Sun JH, Zhu HY, Gao C. Case report: unusual presentation of myositis ossificans of the elbow in a child who underwent excessive postoperative rehabilitation exercise. Front Pediatr. (2021) 9:757147. doi: 10.3389/fped.2021.757147
38. Obert L, Ferrier M, Jacquot A, Mansat P, Sirveaux F, Clavert P, et al. Distal humerus fractures in patients over 65: complications. Orthop Traumatol Surg Res. (2013) 99(8):909–13. doi: 10.1016/j.otsr.2013.10.002
39. Korner J, Lill H, Müller LP, Hessmann M, Kopf K, Goldhahn J, et al. Distal humerus fractures in elderly patients: results after open reduction and internal fixation. Osteoporos Int. (2005) 16(Suppl 2):S73–9. doi: 10.1007/s00198-004-1764-5
40. Shin SJ, Sohn HS, Do NH. A clinical comparison of two different double plating methods for intraarticular distal humerus fractures. J Shoulder Elbow Surg. (2010) 19(1):2–9. doi: 10.1016/j.jse.2009.05.003
Keywords: meta-analysis, anterior transposition, ulnar nerve (MeSH), distal humerus fractures, effect
Citation: Li T, Yan J, Ren Q, Hu J, Wang F, Xiao C and Liu X (2023) Efficacy and safety of anterior transposition of the ulnar nerve for distal humerus fractures: A systematic review and meta-analysis. Front. Surg. 9:1005200. doi: 10.3389/fsurg.2022.1005200
Received: 16 August 2022; Accepted: 14 December 2022;
Published: 6 January 2023.
Edited by:
Federico Canavese, Centre Hospitalier Regional et Universitaire de Lille, FranceReviewed by:
Osvaldo Mazza, Bambino Gesù Children's Hospital (IRCCS), ItalyYejun ZHA, Beijing Jishuitan Hospital, China
© 2023 Li, Yan, Ren, Hu, Wang, Xiao and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xilin Liu YWlyb3RhQDEyNi5jb20= Chengwei Xiao Y2FyYmluZ2VyQDE2My5jb20=
†These authors share first authorship
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Ting Li
Ting Li Jingxin Yan
Jingxin Yan Qiuyu Ren
Qiuyu Ren Jiang Hu
Jiang Hu Fei Wang1
Fei Wang1 Xilin Liu
Xilin Liu