- 1Department of Thoracic Surgery, Weifang Second People's Hospital, Weifang, China
- 2Department of Oral and Maxillofacial Surgery, Weifang Second People's Hospital, Weifang, China
Background and Purpose: Transverse abdominis plane (TAP) block has been suggested to reduce post-operative pain after laparoscopic cholecystectomy (LC). However, the literature is divided on whether ultrasound (USG)-guided TAP block is effective for pain control after LC. The present meta-analysis therefore evaluated the efficacy of USG-guided TAP block vs. controls and port site infiltration for pain control after LC.
Methods: A comprehensive literature search of online academic databases was performed for published randomized controlled trials (RCTs) for studies published to January 31, 2021. The primary outcome analyzed was post-operative pain score at 0, 6, 12, and 24 h post-surgery, both during rest and while coughing. Secondary outcomes included morphine consumption and post-operative nausea and vomiting (PONV) incidence.
Results: A total of 23 studies with data on 1,450 LC patients were included in our meta-analysis. A reduction in pain intensity at certain post-operative timepoints was observed for USG-guided TAP block patients compared to control group patients. No reduction in pain intensity was observed for patients receiving USG-guided TAP block patients vs. conventional Port site infiltration.
Conclusion: This meta-analysis concludes that TAP block is more effective than a conventional pain control, but not significatively different from another local incisional pain control that is port site infiltration. Additional prospective randomized controlled trials are required to further validate our findings.
Introduction
Laparoscopic cholecystectomy (LC) is currently the gold standard treatment for symptomatic gall bladder disorders, including cholelithiasis and cholecystitis (1, 2). However, LC, while minimally invasive, is associated with post-operative pain, especially within the first 24 h. This pain is routinely managed using opiates, which are associated with a number of side effects, including excessive sedation and post-operative nausea and vomiting (PONV). As these side effects may increase hospital stay durations, proper pain control and management are therefore critical for improving clinical outcomes and promoting earlier ambulation post-surgery (3–5).
Transversus abdominis plane (TAP) block is a regional anesthetic technique that has gradually become an alternative for post-operative pain control. It involves the infusion of local anesthetic into the fascial plane of the abdominal wall where the T6 to L1 nerves are found (5). Conventionally, TAP block was performed using anatomical landmarks, but ultrasound (USG)-guided TAP block has become more popular in recent years (6–10).
A previously published meta-analysis detailing seven randomized controlled trials (RCTs) showed TAP block to be effective when compared with standard analgesia in adults undergoing LC (11). However, they lacked evidence to compare the efficacy of TAP block against conventional port site infiltration for post-LC pain control. The current study aims to systematically review all available RCTs to evaluate the efficacy of USG-guided TAP block against conventional analgesia and port site infiltration in LC patients.
Materials and Methods
Search Strategy
This meta-analysis was performed using Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines (12). A comprehensive literature search for RCTs published prior to January 31, 2021 was conducted using the following electronic databases: PubMed, Google scholar, Cochrane Library, Scopus, and TRIP. The following search terms were employed: “Transabdominal abdominis plane block” OR “Tap block” OR “Plane Block” OR “Ultrasound guided TAP block” AND “Laparoscopic cholecystectomy” AND “Pain Control” AND “Analgesic” OR “Local Anesthesia” OR “Infiltration anesthesia.” Literature cited by included studies were also manually searched for additional eligible studies. The literature search did not restrict for language.
Study Eligibility Criteria
RCTs involving adult patients undergoing elective LC that compared the efficacy of USG-guided TAP block against either control or port-site infiltration groups were included. Studies that did not report pain outcomes were not included. Studies where full-texts were not available were not included.
Data Collection and Analysis
All eligible studies were screened by two independent reviewers using the selection criteria listed above. Screening first entailed abstract review, followed by full-text review. Any discrepancies were settled through discussion with a third reviewer. Articles published in a language other than English were machine translated using Google Translate and considered for inclusion. The following information was extracted from each included study: number of patients, investigation groups, types of analgesia used, outcome measurements, treatments, interventions, and adverse effects.
Primary Outcome
The primary outcome evaluated in this study was pain control in LC patients, as measured using 1–10 rating scales such as the visual analog scale (VAS) or numerical rating scale (NRS). Measurements at 0, 6, 12, and 24 h post-operation, both at rest and while coughing, were noted.
Secondary Outcomes
Secondary outcomes in this study included morphine consumption and post-operative nausea and vomiting (PONV) incidence.
Quality Assessment
Studies were assessed for quality using a modified JADAD score (13) that evaluated study methods, randomization approaches, blinding, withdrawals and dropouts, inclusion and exclusion criteria, approaches used to assess adverse effects, and statistical analysis. Scores ranged from 0 (lowest quality) to 8 (highest quality). Study quality was assessed independently by two reviewers. All discrepancies were resolved through discussion.
Publication Bias
Publication bias was assessed using funnel plot analysis. Funnel plot asymmetry was assessed using Egger's regression test (14, 15).
Statistical Analysis
Mean difference (MDs) with 95% confidence intervals (CIs) was calculated for the continuous outcome. Risk ratios (RR) with 95% CIs were calculated for categorical outcomes to estimate pooled findings. Study heterogeneity was evaluated using the I2 statistic. For I2 values >50%, a random-effects model was applied. For I2 values below 50%, a fixed-effect model was applied. Statistical analyses were conducted using Review Manager software (Version 5.3, Copenhagen: The Nordic Cochrane Center, The Cochrane Collaboration 2014).
Results
Literature Search
Primary screening yielded 118 candidate articles. Of these, 47 underwent full-text screening and review. Ultimately, 23 studies containing data on 1,450 patients met inclusion criteria (Figure 1).
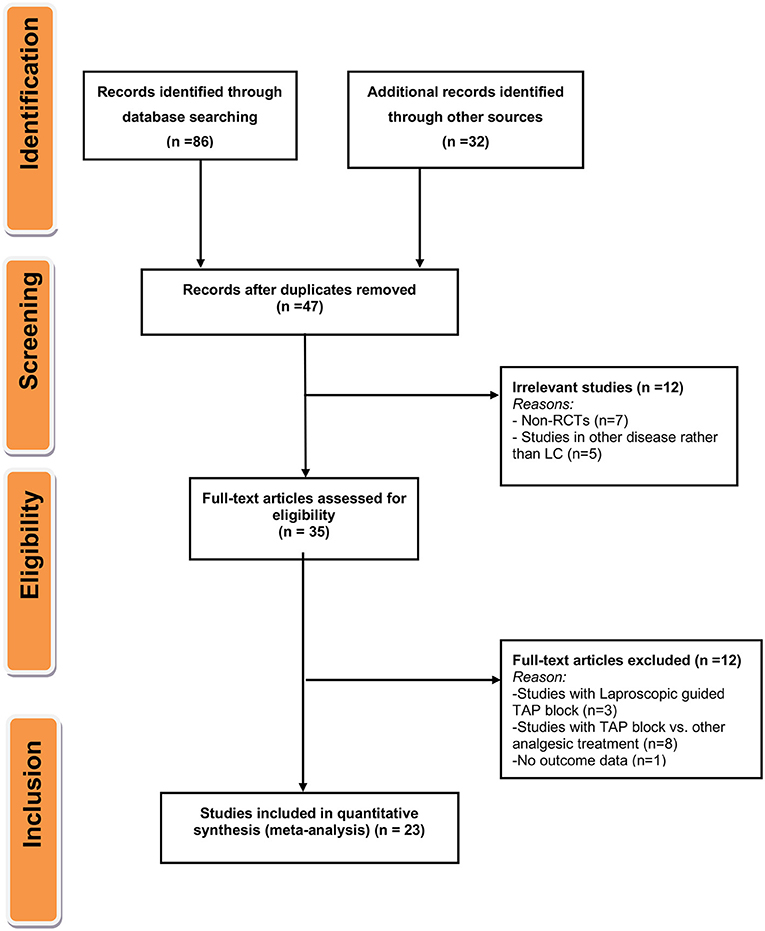
Figure 1. Flow diagram for the selection of studies and specific reasons for exclusion from the present meta-analysis.
Characteristics of Included Studies
A full summary of extracted data from included studies is presented in Table 1. Included studies were published between 2009 and 2020, with individual study samples ranging from 40 to 120 individuals. All included studies were of moderate or high quality based on JADAD Score (Table 2). Out of 23 included studies, 14 studies (16–18, 23–25, 27, 30, 31, 34–38, 40) were conducted in Caucasian individuals, with the remaining nine studies (19–22, 26, 28, 29, 32, 33) were conducted on an Asian population.
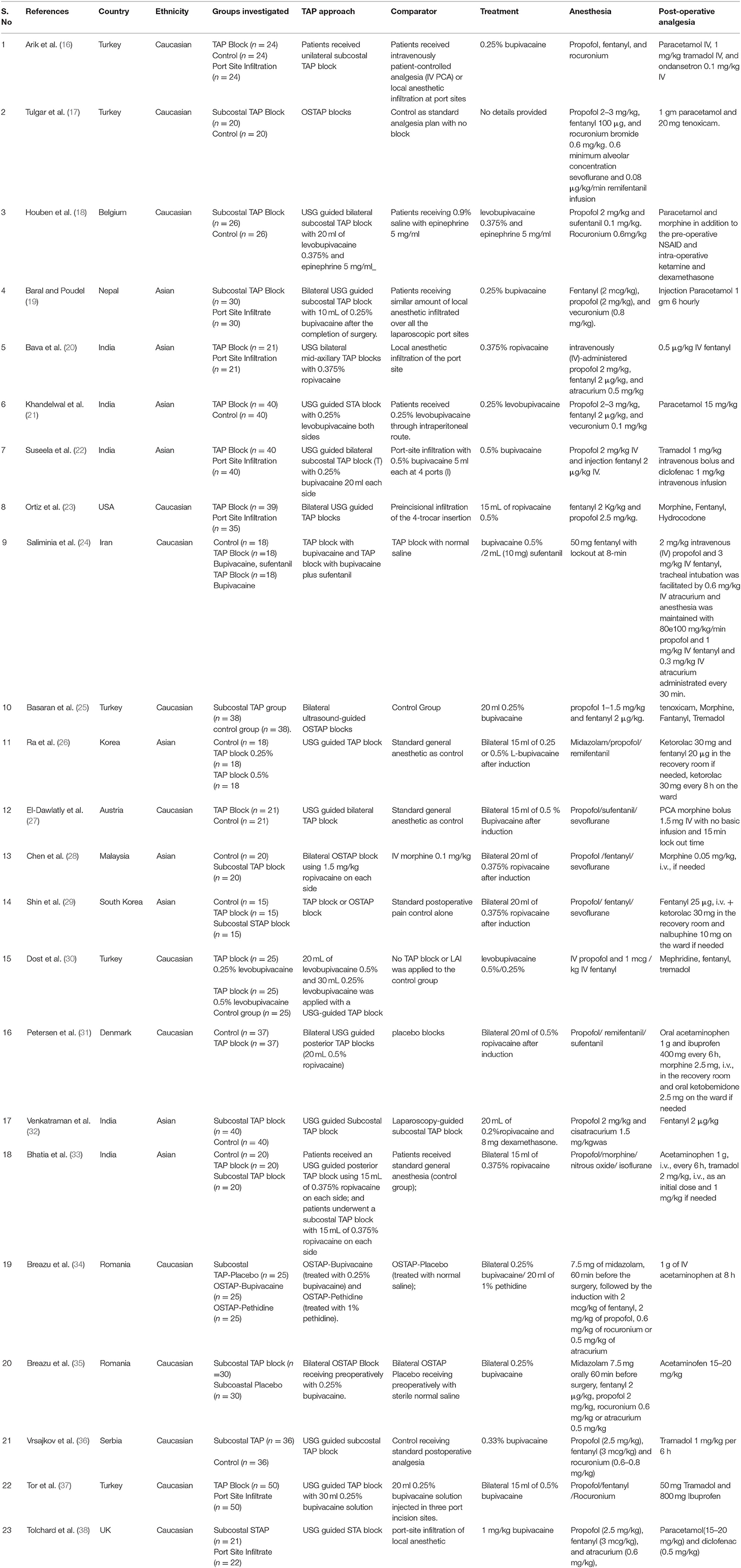
Table 1. Baseline and clinical characteristic of the included studies in the meta-analysis for the efficacy of transversus abdominis plane block for pain control after laparoscopic cholecystectomy.
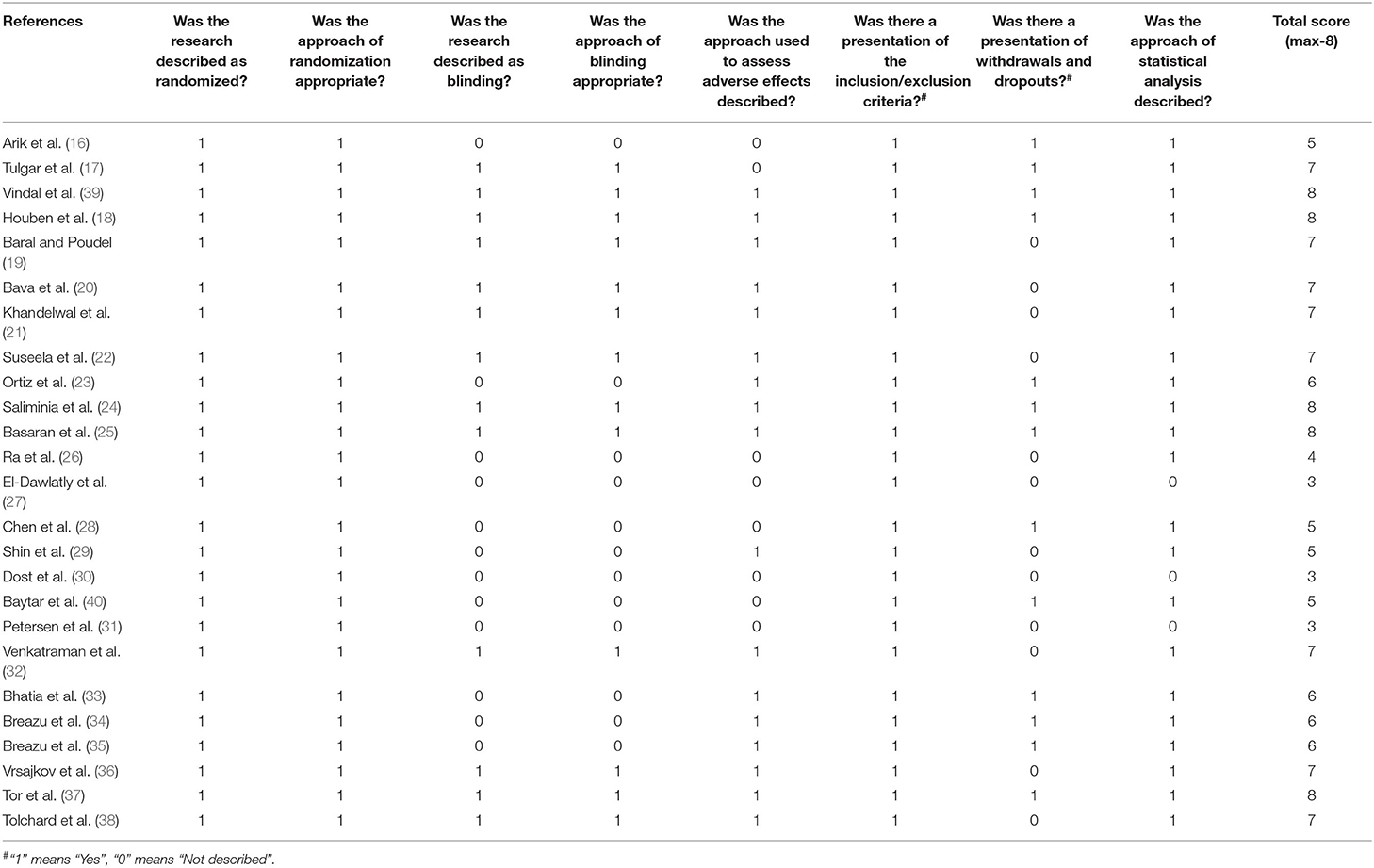
Table 2. Quality assessment using modified Jadad scores (Points 1–8) for the included studies in the meta-analysis.
For the primary outcome of pain control at rest and during coughing, out of 23 studies, 22 studies were included in the analysis for which references have been provided in Table 3. Some of the included studies had reported data only for one or two timepoints for post-operative pain score either for 0 or 6 or 12 or 24 h at rest or during coughing (17, 18, 20, 22–24, 26, 28, 30, 36–38). A single study by El-Dawlatly et al. (27) only provided the data for morphine consumption. PONV data was available for 12 studies (16, 18, 19, 21, 23, 25, 28, 29, 31, 33, 36, 37) (750 LC patients). Information on morphine consumption up to 24 h post-operation was reported by seven studies (16, 17, 23, 27–29, 31) (348 LC subjects).

Table 3. Summary of findings for the included studies investigating the efficacy of TAP block for pain control after LC.
Clinical Outcomes
Post-operative Pain Intensity at Rest
Analysis of the included studies suggested significantly reduced pain intensity in patients receiving USG-guided TAP block relative to control group patients at 0, 6, 12, and 24 h post-operation (Figures 2A–D). However, no such reduction was noted when USG-guided TAP block patients were compared to Port site infiltration group patients (Table 3). A high degree of heterogeneity was present in all included studies at all timepoints (0 h: I2 = 98%, p < 0.0001; 6 h: I2 = 94%, p < 0.0001; 12 h: I2 = 85%, p < 0.0001; 24 h: I2 = 87%, p < 0.0001).
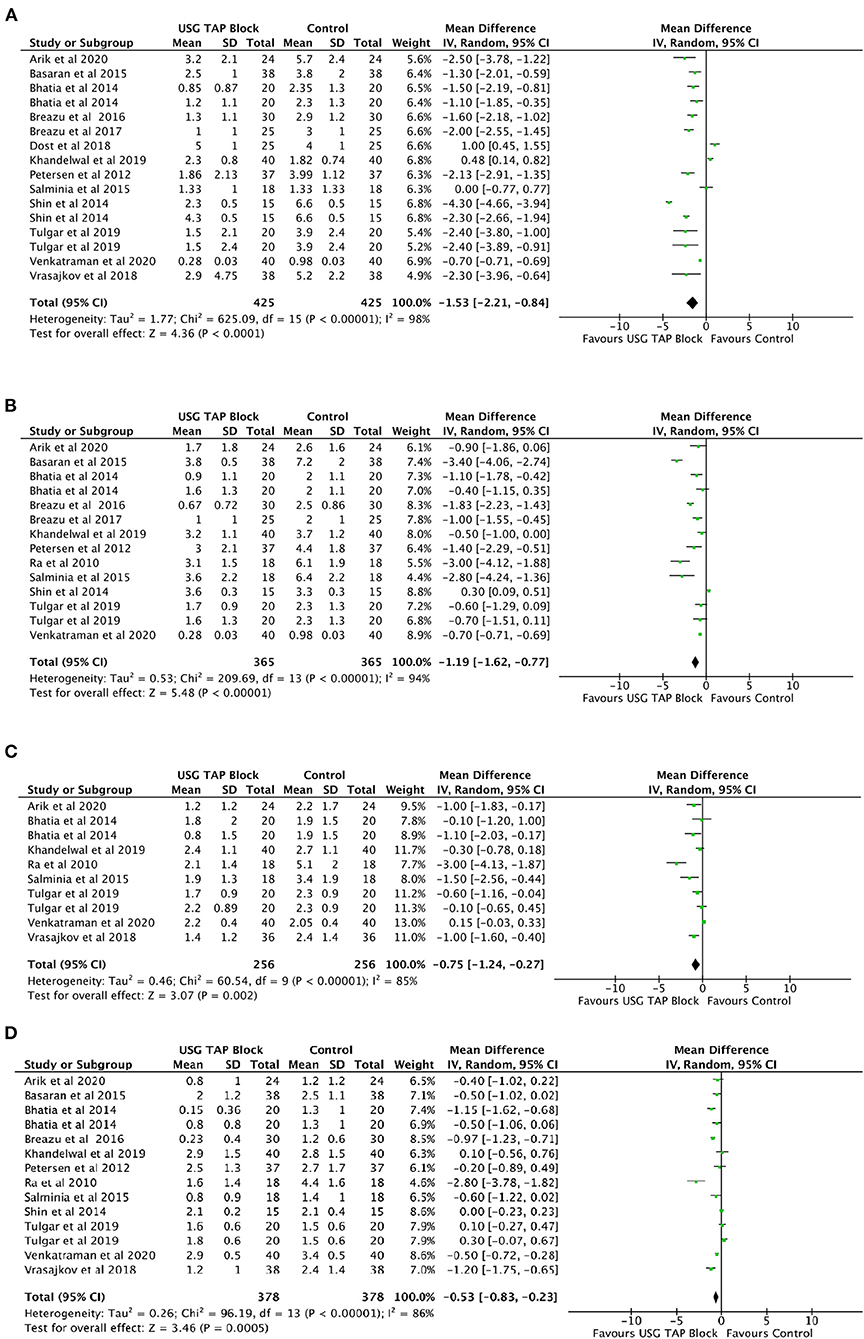
Figure 2. (A–D) Forest plot representing for Pain Intensity at Rest for USG guided TAP block vs. control group at (A) 0 h; (B) 6 h; (C) 12 h and (D) 24 h timepoints after operation.
Post-operative Pain Intensity While Coughing
A significant reduction in pain intensity while coughing was observed at 0, 6, and 24 h post-operation in USG-guided TAP block patients relative to control group patients (Figures 3A–D). No significant change in pain intensity was noted at 12 h post-operation. No significant changes were noted when comparing USG-guided TAP block patients to Port site infiltration group patients at all post-operative time-point (Table 3).
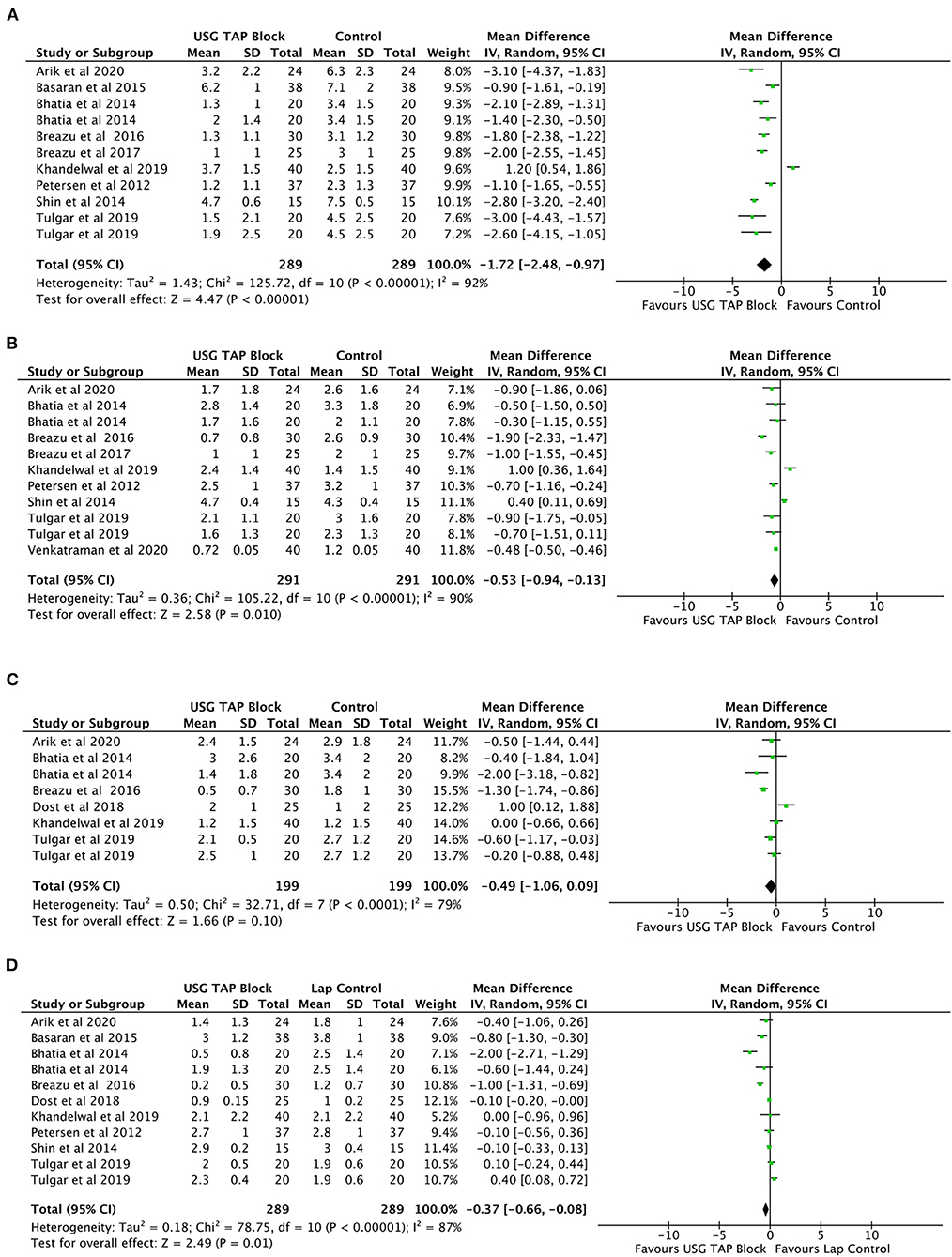
Figure 3. (A–D) Forest plot representing for Pain Intensity after operation during coughing for USG TAP block vs. control group (A) 0 h; (B) 6 h; (C) 12 h and (D) 24 h.
Morphine Consumption During 24 h After Operation
Analysis of seven studies (16, 17, 23, 27–29, 31) involving 348 LC subjects showed a significant reduction in morphine consumption during the first 24 h after surgery (MD = −1.76 mg, 95% CI: −3.28 to −0.24) in patients receiving TAP blocks compared to control subjects (Figure 4). A high degree of heterogeneity was observed (I2 = 91%, p < 0.0001).
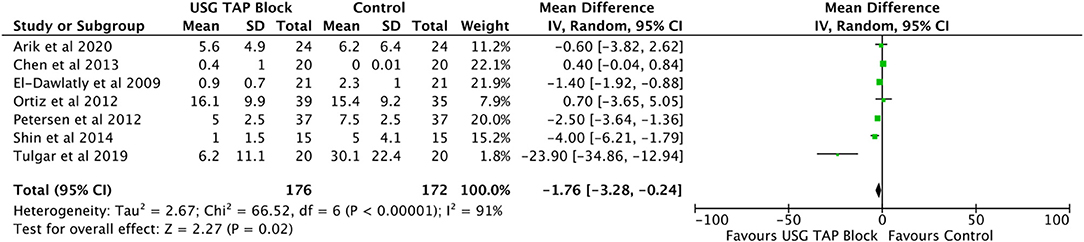
Figure 4. Forest plot representing for morphine consumption in the recovery room USG guided TAP block vs. control group.
Post-operative Nausea and Vomiting (PONV) Incidence
Analysis of 12 studies (16, 18, 19, 21, 23, 25, 28, 29, 31, 33, 36, 37) involving 750 LC subjects showed a decreased incidence of PONV in patients receiving USG guided TAP blocks compared to control subjects (RR = 0.69, 95% CI: 0.54–0.89) (Figure 5). No significant heterogeneity between the studies was observed (I2 = 9%, p = 0.36).
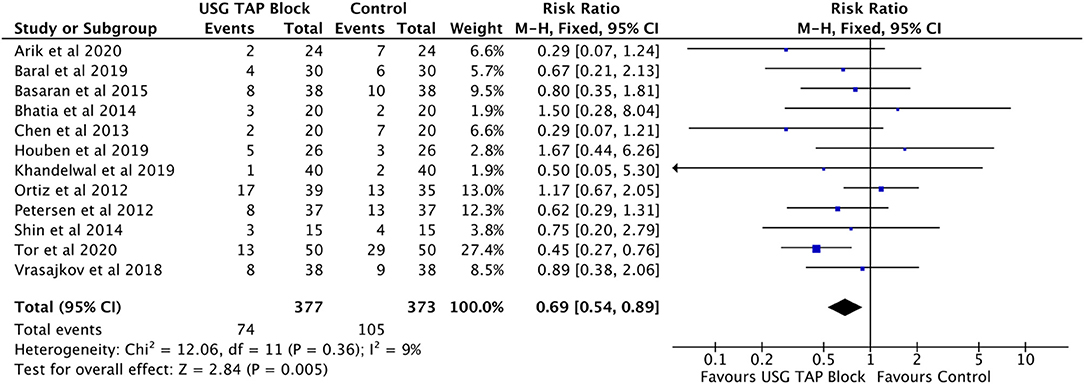
Figure 5. Forest plot representing for adverse events (PONV) in USG guided TAP block vs. control group.
Publication Bias
No significant publication bias was detected using Funnel plots or Egger's tests for (a) Post-Operative Pain Intensity at Rest for all timepoints (0 h: p = 0.54; 6 h: p = 0.32; 12 h: p = 0.98; 24 h: p = 0.63); (b) Post-Operative Pain Intensity during coughing for all timepoints (0 h: p = 0.12; 6 h: p = 0.76; 12 h; p = 0.91, 24 h: p = 0.17), (c) Morphine consumption during 24 h after operation (p = 0.36), (d) Post-operative nausea and vomiting (PONV) incidence (p = 0.71). All funnel plots showed symmetric shape for all the comparison.
Discussion
This study evaluated the efficacy of USG guided TAP block for reducing pain intensity at rest and while coughing in LC patients for up to 24 h post-operation. We noted a significant reduction in pain intensity in patients who received USG-guided TAP block relative to control group patients, as well as reduced morphine consumption and incidence of PONV. However, no such reduction was noted when USG-guided TAP block patients were compared to Port site infiltration group patients at rest and during coughing at all post-operative timepoints upto 24 h.
Severe pain for LC patients generally occurs during the first 24 h post-surgery, and is thought to arise mainly from visceral tissue damage and the surgical incision (with the latter taking precedent) (41). As such, analgesic planning must focus on incisional pain rather than visceral pain. The absence of significant difference of pain control after port site infiltration advocates too for an incisional pain control. Our results showed that USG-guided TAP block led to significantly reduced post-operative pain, as well as reduced morphine consumption and PONV incidence. These findings concur with a previous analysis of seven studies by Peng et al. (11). Recent RCTs have suggested that USG-guided TAP block plays an important role in multimodal pain therapy through proper visualization and improved accuracy. However, few studies have compared the effects of subcoastal TAP block with those of posterior TAP block. As such, our meta-analysis included RCTs that looked at both USG-guided TAP blocks and oblique subcostal TAP blocks. Nonetheless, we noted high heterogeneity between studies, suggesting that our meta-analysis results need to be treated with caution.
Our study has several limitations: (1) included studies had relatively small sample sizes; (2) extended follow-up data on chronic pain, long-term analgesic use, and adverse events was lacking; (3) multiple pain score scales were used; (4) a diverse range of anesthesia dosages were administered across the studies, and (5) insufficient study numbers for important factors such as laproscopic guided TAP block and fentanyl, tramadol, and opioid consumption, thereby precluding subgroup analysis.
Conclusion
This meta-analysis concludes that TAP block is more effective than a conventional pain control, but not significatively different from another local incisional pain control that is port site infiltration. Additional prospective randomized controlled trials are required to further validate our findings.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
WW conceived and designed the study. WW and LW did literature search and analyzed the data. YG wrote the paper, reviewed, and edited the manuscript. All authors have read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Keus F, de Jong JaF, Gooszen HG, van Laarhoven CJHM. Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst. Rev. (2006) 2006:CD006231. doi: 10.1002/14651858.CD006231
2. Bucher P, Pugin F, Buchs NC, Ostermann S, Morel P. Randomized clinical trial of laparoendoscopic single-site versus conventional laparoscopic cholecystectomy. Br J Surg. (2011) 98:1695–702. doi: 10.1002/bjs.7689
3. Barczyński M, Herman RM. A prospective randomized trial on comparison of low-pressure (LP) and standard-pressure (SP) pneumoperitoneum for laparoscopic cholecystectomy. Surg Endosc. (2003) 17:533–8. doi: 10.1007/s00464-002-9121-2
4. Bisgaard T. Analgesic treatment after laparoscopic cholecystectomy: a critical assessment of the evidence. Anesthesiology. (2006) 104:835–46. doi: 10.1097/00000542-200604000-00030
5. Rozen WM, Tran TMN, Ashton MW, Barrington MJ, Ivanusic JJ, Taylor GI. Refining the course of the thoracolumbar nerves: a new understanding of the innervation of the anterior abdominal wall. Clin Anat N Y N. (2008) 21:325–33. doi: 10.1002/ca.20621
6. Charlton S, Cyna AM, Middleton P, Griffiths JD. Perioperative transversus abdominis plane (TAP) blocks for analgesia after abdominal surgery. Cochrane Database Syst. Rev. (2010) 2010:CD007705. doi: 10.1002/14651858.CD007705.pub2
7. Siddiqui MRS, Sajid MS, Uncles DR, Cheek L, Baig MK. A meta-analysis on the clinical effectiveness of transversus abdominis plane block. J Clin Anesth. (2011) 23:7–14. doi: 10.1016/j.jclinane.2010.05.008
8. Johns N, O'Neill S, Ventham NT, Barron F, Brady RR, Daniel T. Clinical effectiveness of transversus abdominis plane (TAP) block in abdominal surgery: a systematic review and meta-analysis. Colorectal Dis Off J Assoc Coloproctology G B Irel. (2012) 14:e635–42. doi: 10.1111/j.1463-1318.2012.03104.x
9. Champaneria R, Shah L, Geoghegan J, Gupta JK, Daniels JP. Analgesic effectiveness of transversus abdominis plane blocks after hysterectomy: a meta-analysis. Eur J Obstet Gynecol Reprod Biol. (2013) 166:1–9. doi: 10.1016/j.ejogrb.2012.09.012
10. De Oliveira GS, Castro-Alves LJ, Nader A, Kendall MC, McCarthy RJ. Transversus abdominis plane block to ameliorate postoperative pain outcomes after laparoscopic surgery: a meta-analysis of randomized controlled trials. Anesth Analg. (2014) 118:454–63. doi: 10.1213/ANE.0000000000000066
11. Peng K, Ji F, Liu H, Wu S. Ultrasound-guided transversus abdominis plane block for analgesia in laparoscopic cholecystectomy: a systematic review and meta-analysis. Med Princ Pract Int J Kuwait Univ Health Sci Cent. (2016) 25:237–46. doi: 10.1159/000444688
12. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. (2015) 4:1. doi: 10.1186/2046-4053-4-1
13. Oremus M, Wolfson C, Perrault A, Demers L, Momoli F, Moride Y. Interrater reliability of the modified Jadad quality scale for systematic reviews of Alzheimer's disease drug trials. Dement Geriatr Cogn Disord. (2001) 12:232–6. doi: 10.1159/000051263
14. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. (1994) 50:1088–101. doi: 10.2307/2533446
15. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
16. Arik E, Akkaya T, Ozciftci S, Alptekin A, Balas S. Unilateral transversus abdominis plane block and port-site infiltration : comparison of postoperative analgesic efficacy in laparoscopic cholecystectomy. Anaesthesist. (2020) 69:270–6. doi: 10.1007/s00101-020-00746-1
17. Tulgar S, Kapakli MS, Kose HC, Senturk O, Selvi O, Serifsoy TE, et al. Evaluation of ultrasound-guided erector spinae plane block and oblique subcostal transversus abdominis plane block in laparoscopic cholecystectomy: randomized, controlled, prospective study. Anesth Essays Res. (2019) 13:50–6. doi: 10.4103/aer.AER_194_18
18. Houben AM, Moreau A-SJ, Detry OM, Kaba A, Joris JL. Bilateral subcostal transversus abdominis plane block does not improve the postoperative analgesia provided by multimodal analgesia after laparoscopic cholecystectomy: a randomised placebo-controlled trial. Eur J Anaesthesiol. (2019) 36:772–7. doi: 10.1097/EJA.0000000000001028
19. Baral B, Poudel PR. Comparison of analgesic efficacy of ultrasound guided subcostal transversus abdominis plane block with port site infiltration following laparoscopic cholecystectomy. J Nepal Health Res Counc. (2019) 16:457–61. doi: 10.33314/jnhrc.v16i41.1486
20. Bava EP, Ramachandran R, Rewari V, Chandralekha Bansal VK, Trikha A. Analgesic efficacy of ultrasound guided transversus abdominis plane block versus local anesthetic infiltration in adult patients undergoing single incision laparoscopic cholecystectomy: a randomized controlled trial. Anesth Essays Res. (2016) 10:561–7. doi: 10.4103/0259-1162.186620
21. Khandelwal H, Parag K, Singh A, Anand N, Govil N. Comparison of subcostal transversus abdominis block with intraperitoneal instillation of levobupivacaine for pain relief after laparoscopic cholecystectomy: a prospective study. Anesth Essays Res. (2019) 13:144–8. doi: 10.4103/aer.AER_3_19
22. Suseela I, Anandan K, Aravind A, Kaniyil S. Comparison of ultrasound-guided bilateral subcostal transversus abdominis plane block and port-site infiltration with bupivacaine in laparoscopic cholecystectomy. Indian J Anaesth. (2018) 62:497–501. doi: 10.4103/ija.IJA_55_18
23. Ortiz J, Suliburk JW, Wu K, Bailard NS, Mason C, Minard CG, et al. Bilateral transversus abdominis plane block does not decrease postoperative pain after laparoscopic cholecystectomy when compared with local anesthetic infiltration of trocar insertion sites. Reg Anesth Pain Med. (2012) 37:188–92. doi: 10.1097/AAP.0b013e318244851b
24. Saliminia A, Azimaraghi O, Babayipour S, Ardavan K, Movafegh A. Efficacy of transverse abdominis plane block in reduction of postoperation pain in laparoscopic cholecystectomy. Acta Anaesthesiol Taiwanica Off J Taiwan Soc Anesthesiol. (2015) 53:119–22. doi: 10.1016/j.aat.2015.07.003
25. Basaran B, Basaran A, Kozanhan B, Kasdogan E, Eryilmaz MA, Ozmen S. Analgesia and respiratory function after laparoscopic cholecystectomy in patients receiving ultrasound-guided bilateral oblique subcostal transversus abdominis plane block: a randomized double-blind study. Med Sci Monit Int Med J Exp Clin Res. (2015) 21:1304–12. doi: 10.12659/MSM.893593
26. Ra YS, Kim CH, Lee GY, Han JI. The analgesic effect of the ultrasound-guided transverse abdominis plane block after laparoscopic cholecystectomy. Korean J Anesthesiol. (2010) 58:362–8. doi: 10.4097/kjae.2010.58.4.362
27. El-Dawlatly AA, Turkistani A, Kettner SC, Machata A-M, Delvi MB, Thallaj A, et al. Ultrasound-guided transversus abdominis plane block: description of a new technique and comparison with conventional systemic analgesia during laparoscopic cholecystectomy. Br J Anaesth. (2009) 102:763–7. doi: 10.1093/bja/aep067
28. Chen CK, Tan PCS, Phui VE, Teo SC. A comparison of analgesic efficacy between oblique subcostal transversus abdominis plane block and intravenous morphine for laparascopic cholecystectomy. A prospective randomized controlled trial. Korean J Anesthesiol. (2013) 64:511–6. doi: 10.4097/kjae.2013.64.6.511
29. Shin H-J, Oh A-Y, Baik J-S, Kim J-H, Han S-H, Hwang J-W. Ultrasound-guided oblique subcostal transversus abdominis plane block for analgesia after laparoscopic cholecystectomy: a randomized, controlled, observer-blinded study. Minerva Anestesiol. (2014) 80:185–93.
30. Dost B, Yalçin Sezen G, Iskender A, Özlü O. A comparison of transversus abdominis plane block guided with ultrasonography and local anesthetic infiltration in laparoscopic cholecystectomy operations. Agri Agri Algoloji Derneginin Yayin Organidir J Turk Soc Algol. (2018) 30:51–7. doi: 10.5505/agri.2018.45822
31. Petersen PL, Stjernholm P, Kristiansen VB, Torup H, Hansen EG, Mitchell AU, et al. The beneficial effect of transversus abdominis plane block after laparoscopic cholecystectomy in day-case surgery: a randomized clinical trial. Anesth Analg. (2012) 115:527–33. doi: 10.1213/ANE.0b013e318261f16e
32. Venkatraman R, Saravanan R, Dhas M, Pushparani A. Comparison of laparoscopy-guided with ultrasound-guided subcostal transversus abdominis plane block in laparoscopic cholecystectomy - a prospective, randomised study. Indian J Anaesth. (2020) 64:1012–7. doi: 10.4103/ija.IJA_528_20
33. Bhatia N, Arora S, Jyotsna W, Kaur G. Comparison of posterior and subcostal approaches to ultrasound-guided transverse abdominis plane block for postoperative analgesia in laparoscopic cholecystectomy. J Clin Anesth. (2014) 26:294–9. doi: 10.1016/j.jclinane.2013.11.023
34. Breazu CM, Ciobanu L, Bartos A, Bodea R, Mircea PA, Ionescu D. Pethidine efficacy in achieving the ultrasound-guided oblique subcostal transversus abdominis plane block in laparoscopic cholecystectomy: a prospective study. Bosn J Basic Med Sci. (2017) 17:67–73. doi: 10.17305/bjbms.2016.1647
35. Breazu CM, Ciobanu L, Hadade A, Bartos A, Mitre C, Mircea PA, et al. The efficacy of oblique subcostal transversus abdominis plane block in laparoscopic cholecystectomy - a prospective, placebo controlled study. Romanian J Anaesth Intensive Care. (2016) 23:12–8. doi: 10.21454/rjaic.7518.231.obq
36. Vrsajkov V, Mančić N, Mihajlović D, Milićević ST, Uvelin A, Vrsajkov JP. O bloqueio do plano transverso abdominal subcostal pode melhorar a analgesia após colecistectomia laparoscópica. Braz J Anesthesiol. (2018) 68:149–53. doi: 10.1016/j.bjan.2017.10.006
37. Tor IH, Çelik EC, Aydin ME. Analgesic effect of combined transversus abdominis plane block and rectus sheath block in laparoscopic cholecystectomy: prospective randomized study. Ain-Shams J Anesthesiol. (2020) 12:58. doi: 10.1186/s42077-020-00108-4
38. Tolchard S, Davies R, Martindale S. Efficacy of the subcostal transversus abdominis plane block in laparoscopic cholecystectomy: comparison with conventional port-site infiltration. J Anaesthesiol Clin Pharmacol. (2012) 28:339–43. doi: 10.4103/0970-9185.98331
39. Vindal A, Sarda H, Lal P. Laparoscopically guided transversus abdominis plane block offers better pain relief after laparoscopic cholecystectomy: results of a triple blind randomized controlled trial. Surg Endosc. (2021) 35:1713–21. doi: 10.1007/s00464-020-07558-9
40. Baytar Ç, YIlmaz C, Karasu D, Topal S. Comparison of ultrasound-guided subcostal transversus abdominis plane block and quadratus lumborum block in laparoscopic cholecystectomy: a prospective, randomized, controlled clinical study. Pain Res Manage. (2019) 2019:2815301. doi: 10.1155/2019/2815301
Keywords: laparoscopic cholecystectomy, analgesia, transverse abdominis plane block, ultrasound, pain control
Citation: Wang W, Wang L and Gao Y (2021) A Meta-Analysis of Randomized Controlled Trials Concerning the Efficacy of Transversus Abdominis Plane Block for Pain Control After Laparoscopic Cholecystectomy. Front. Surg. 8:700318. doi: 10.3389/fsurg.2021.700318
Received: 26 April 2021; Accepted: 08 July 2021;
Published: 04 August 2021.
Edited by:
Stefano Pontone, Sapienza University of Rome, ItalyReviewed by:
Claude Bertrand, CHU UCL Namur Site Godinne, BelgiumKenan Yusif-zade, Independent Researcher, Baku, Azerbaijan
Copyright © 2021 Wang, Wang and Gao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Gao, bTE1MTY1NjAzNDU2QDE2My5jb20=
 Weihua Wang1
Weihua Wang1 Yan Gao
Yan Gao