
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg., 02 June 2021
Sec. Neurosurgery
Volume 8 - 2021 | https://doi.org/10.3389/fsurg.2021.690971
This article is part of the Research TopicPrioritizing Global Neurosurgery in the Focus of Global Public Health: The ethical, financial and clinical necessitiesView all 23 articles
A correction has been applied to this article in:
Corrigendum: Racial and Ethnic Inequities in Mortality During Hospitalization for Traumatic Brain Injury: A Call to Action
The health disparities which drive inequities in health outcomes have long plagued our already worn healthcare system and are often dismissed as being a result of social determinants of health. Herein, we explore the nature of these inequities by comparing outcomes for racial and ethnic minorities patients suffering from traumatic brain injury (TBI). We retrospectively reviewed all patients enrolled in the Trauma One Database at the Oregon Health & Science University Hospital from 2006 to October 2017 with an abbreviated injury scale (AIS) for the head or neck >2. Racial and ethnic minority patients were defined as non-White or Hispanic. A total of 6,352 patients were included in our analysis with 1,504 in the racial and ethnic minority cohort vs. 4,848 in the non-minority cohort. A propensity score (PS) model was generated to account for differences in baseline characteristics between these cohorts to generate 1,500 matched pairs. The adjusted hazard ratio for in-hospital mortality for minority patients was 2.21 [95% Confidence Interval (CI) 1.43–3.41, p < 0.001] using injury type, probability of survival, and operative status as covariates. Overall, this study is the first to specifically look at racial and ethnic disparities in the field of neurosurgical trauma. This research has demonstrated significant inequities in the mortality of TBI patients based on race and ethnicity and indicates a substantive need to reshape the current healthcare system and advocate for safer and more supportive pre-hospital social systems to prevent these life-threatening sequelae.
Structural disparities propagated against racial and ethnic minorities have long been known to drive inequities in health outcomes in the US yet are often dismissed as an unfortunate yet unavoidable consequences of what has been disguised as the social determinants of health. However, many of these inequities are formed long before our patients ever step foot into a healthcare facility and stem not from individual poor health decisions but from decades of structural racism and systematic oppression which leave minority patients at a disadvantage for health outcomes even from before birth (1–3). [It is important to state clearly at this point that we will discuss race and ethnicity not as biologically-based separations of persons but as socially-formed systematic manners of categorizing persons based on culture, geographic origin, language, etc. so as to provide financial, social, and political advantage over specific groups of persons with a long and evidence-based history of such action (3–8)]. These systemic factors have been extensively researched in the fields of public health, sociology, psychology, and more to demonstrate significant negative impacts on a minority persons lifelong risk for medical and psychological trauma (1–3, 9).
Specifically in the field of trauma, these inequities are then exacerbated by ongoing external factors such as insurance, access to level I trauma centers, mechanism of injury, time to surgical intervention, staffing of skilled providers, access to post-acute care and rehabilitation, and community or financial support (1, 10–14). In neurosurgical trauma, the crux of disease burden lies in traumatic brain injury (TBI) which is increasingly becoming a more prevalent global medical issue with devastating effects on both personal and healthcare sequelae (15–20). As with other healthcare fields, neurosurgery and neuro-trauma are not immune to the adverse effects of structural racism on racial and ethnic inequities (10, 21–24). Past research in this field has failed to identify or call out the specific role of sociological and systemic factors that influence these pervasive, persistent, and problematic disparities of health outcomes for our minority patients. In this study, we explore the racial and ethnic inequities in mortality during hospitalization following traumatic brain injury and will engage both a sociological and medical perspective to call to action a change in practice toward a more expansive and sympathetic understanding of the factors involved in minority health outcomes in neuro-trauma.
This study is a retrospective review of all patients entered into the Trauma One Database established in 2006 at the Oregon Health & Science University Hospital (OHSU), one of the two Level I Trauma centers in the state of Oregon. For our research, we included all patients ≥16 years-old entered into the system from 2006 to October of 2017. The dataset used for analysis contained all patient demographic and insurance characteristics, details regarding the mechanism of injury (MOI), treatments provided in the pre-hospital setting and throughout the hospital stay, comorbidities at the time of presentation, discharge disposition, and overall complications. This study follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines, and was approved by the OHSU Institutional Review Board (25).
TBI severity was classified according to the patient's Glasgow Coma Scale (GCS) score on arrival with the following classifications: severe as GCS <8, moderate as 8–12, and mild as ≥13. Minor trauma was defined by an Injury Severity Score (ISS) of ≤ 15. Racial and ethnic minority patients were defined as identifying as any non-White race or as being of Hispanic ethnicity. Mechanism of injury categories were assigned based on the Abbreviated Injury Scale (AIS), ISS, and ICD-9-CM, or ICD-10-CM codes (26). Probability of survival is calculated at our institution using the Trauma Injury Severity Score methodology with a weighted formula comprising of ISS, age, and Revised Trauma Score.
The primary outcome of interest was in-hospital mortality stratified by racial and ethnic minority status. The secondary outcome was the trend in mortality classified by arrival year, injury type, and the presence of work-related injuries.
Continuous variables were described using means and standard deviations (SD), and compared between groups using a two-sample Student's t-test. When appropriate for skewed variables, the geometric mean and geometric standard deviation were calculated and used for comparisons. Dichotomous and categorical variables were reported using counts and percentages and compared using Fisher's exact-test.
Due to the inherent potential for selection bias in this observational retrospective study, and to account for differences in baseline socioeconomic and demographic characteristics, a propensity-score (PS) matching model was employed. Age, sex, injury mechanism, and primary payor were included as the covariates in this final model, consistent with what has been done in the literature previously when examining racial and ethnic disparities (27, 28). Matching with a 1:1 ratio using nearest neighbor methodology was then performed using MatchIt Package in R, version 4.1.0 (29). Balance of baseline covariates and region of common support was then assessed using absolute standardized mean differences, jitter plots and histograms, provided in the Supplementary Materials.
A multivariate Cox Proportional Hazards regression model was then created using an iterative combined forward and backward stepwise selection procedure from the candidate covariates for the propensity-matched cohorts. Assumptions required for proportional hazards regression were assessed numerically for each covariate, and graphically by the plotting of scaled Schoenfeld residuals. The final model included injury type, probability of survival, and operative status as covariates. Since the AIS score covariate was found to violate the assumption of proportional hazards, the final model was stratified by this covariate. Goodness of fit of each model was then assessed using Cox-Snell residuals.
A p-value < 0.05 was considered to be statistically significant. All analyses were performed using R software, version 4.0.4 (R Foundation for Statistical Computing, Vienna, Austria). The final analysis was confirmed using Stata, version 16.1 (StataCorp, College Station, Texas).
There was a total of 6,352 patients included in the Trauma One database with 1,504 included in the racial/ethnic minority cohort and 4,848 patients in the White/non-Hispanic cohort. The clinical characteristics of the patients and propensity-matched patients are shown in Tables 1A, 1B, respectively. Following statistical PS matching, the maximum number of participants in each group was 1,500 (approximately equivalent to the total number of patients in the minority group).
Overall, the patients were 68.5% male and 31.5% female. There was a statistically significant difference in sex between the White/non-Hispanic and the minority cohorts with males making up 67.3% of the White/non-Hispanic group vs. 72.4% of the minority cohort (p < 0.001). The average age of all patients was 47.89 years old. There was a statically significant difference in the average ages based on cohorts with that of the White/non-Hispanic group as 49.66 years old and of the minority group as 42.61 years old (p < 0.001). By age group, the highest incidence of TBI overall and in the White/non-Hispanic cohort occurred in the 55–64 year old group (14.9% of overall patients, 15.8% of White/non-Hispanic patients) while the highest incidence for the minority cohort occurred in the 15–24 year old group (19.6% of minority patients).
Overall, there were 7 different categories for race/ethnicity included in the demographics of the database: White (86.9%), Black/African American (1.8%), American Indian or Alaskan Native (1.1%), Asian (2.5%), Hispanic/Latino (6.2%), Pacific Islander or Native Hawaiian (0.3%), and Other (1.2%). Of the minority sub-group, the patients were 13.4% Black, 7.9% American Indian/Alaskan Native, 19% Asian, 46.2% Hispanic/Latino, 2.0% Pacific Islander/Native Hawaiian, and 9.2% Other.
The overall in-hospital mortality rate was 9.9% with a statistically significant difference between in-hospital mortality rate of White/non-Hispanic patients (8.5%) and the in-hospital mortality rate of minority patients (14.6%) (p < 0.001). The adjusted hazard ratio for in-hospital mortality for minority patients in the propensity-matched cohort was 2.21 [95% Confidence Interval (CI) 1.43, 3.41] with p < 0.001 (Table 2). Examination of the absolute standardized mean differences, and of the region of common support indicated effective propensity-score matching (Supplementary Figures 1, 2). There was no statistically significant difference in the overall probability of survival prior to propensity matching, however the Kaplan-Meier curve of both the non-propensity matched and propensity matched patients (Figures 1A,B) demonstrates a visibly lower survival probability in the minority group. The overall length of hospital stay was 3.85 days with a larger standard deviation in the minority group (4.27 days) vs. the White/non-Hispanic group (3.30 days) (p < 0.001). The length of ICU stay in all groups was an average of 2.12 days (p = 0.007). There was no statistically significant difference in discharge disposition, with 58.5% overall discharged to home, 58.5% of White/non-Hispanic patients discharged home, and 60.0% of minority patients discharged home. There were slight differences in discharges to Skilled Nursing Facilities (SNFs) (17.9% of White/non-Hispanic patients vs. 12.2% of minority patients), Acute Care Facility-Hospitals (1.6% of White/non-Hispanic patients vs. 0.8% of minority patients), and Rehabilitation Facilities (5.2% of White/non-Hispanic patients vs. 4.7% of minority patients).
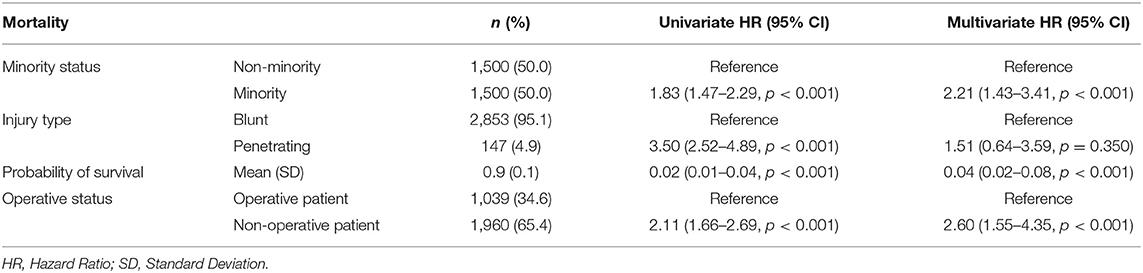
Table 2. Final cox proportional hazard regression models for overall survival using propensity-matched cohorts and robust standard error.
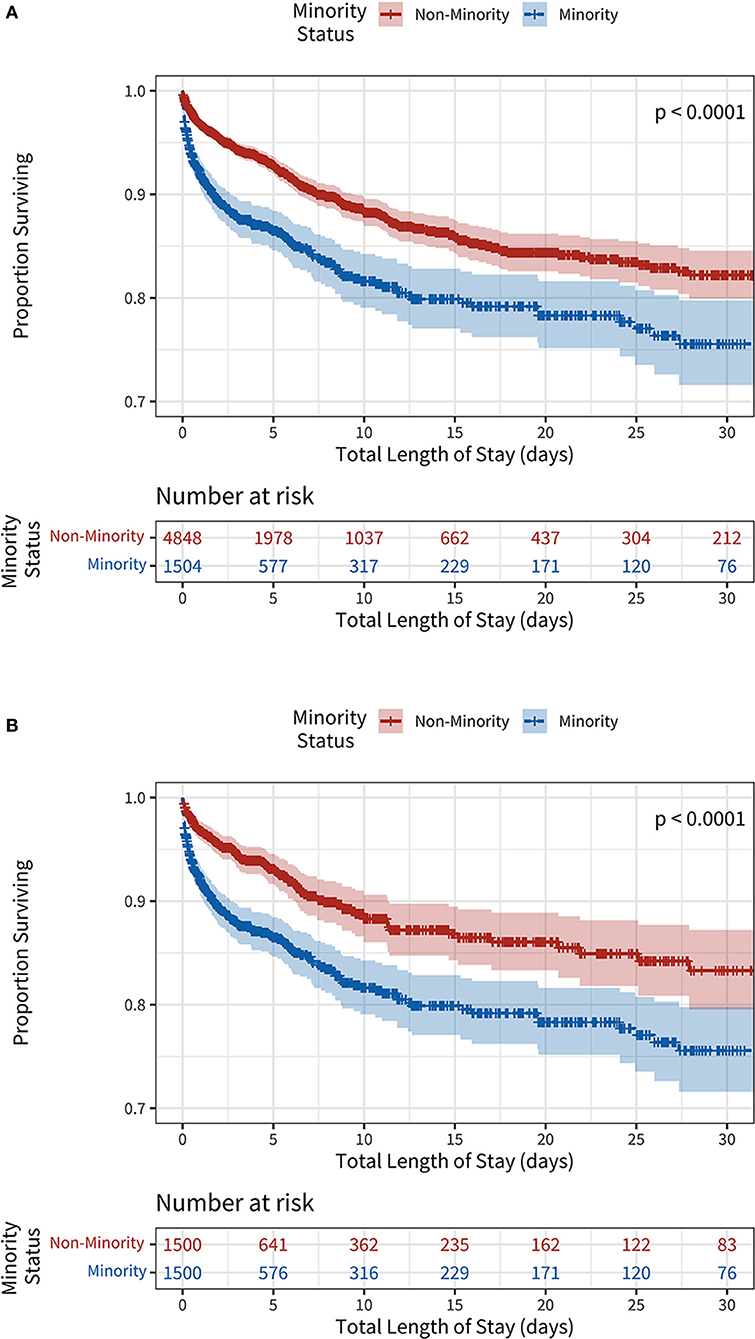
Figure 1. (A) Unadjusted Kaplan-Meier survival curves stratified by minority status. (B) Propensity-score weighted Kaplan-Meier survival curves stratified by minority status.
Out of all TBI admissions, 96.5% were due to blunt trauma and 3.5% were due to penetrating trauma. There was a statistically significant difference between percentage of blunt vs. penetrating trauma with only 2.9% of trauma being penetrating in the White/non-Hispanic group while 5.3% of trauma was penetrating in the minority group (p < 0.001). In all patients, the most common mechanism of injury was fall (47.5%), followed by occupant in a motor vehicle crash (MVC) (17.0%). In the White/non-Hispanic group, this trend was similar with 50% of trauma being due to fall and 15.8% being due to MVC; however, in the minority group, although the trend was similar, the percentage of fall (39.3%) was lower and the percentage of MVC trauma (20.9%) was higher than the White/non-Hispanic group. There was a statistically significant difference in work-relatedness of injury with 4.7% of the minority group's injuries being due to work vs. only 3.2% of the White/non-Hispanic group (p = 0.011).
There were many statistically significant differences in severity of presenting injury between the White/non-Hispanic group and the minority group. The presenting GCS in the White/non-Hispanic group was 11.33 while that in the minority group was 10.44 (p < 0.001). The ISS in the White/non-Hispanic group was 19.14 vs. 20.07 in the minority group (p < 0.001). The percentage of patients with AIS > 3 and 4 was similar between groups, however the percentage of patients with AIS > 5 was 18.5% in the White/non-Hispanic group vs. 22.5% in the minority group. The percentage of TBI severity (mild, moderate, and severe) was statistically significant with 5.8% moderate and 16.4% severe TBI in the White/non-Hispanic group vs. 7.2% moderate and 21.7% severe in the minority group (p < 0.001).
There was no statistically significant difference between groups regarding mode of transport to the hospital with each group arriving via ambulance around 77% of the time and a privately owned vehicle 1.3–1.4% of the time. Advanced directives were in place for 3.0% of White/non-Hispanic patients vs. 2.0% of minority patients. There were 92.5% of patients in the White/non-Hispanic group with neither an Advanced Directive nor POLST in place prior to injury vs. 94.4% of patients in the minority group with neither document in place. In the White/non-Hispanic group, 30.8% of the patients were operative vs. 34.5% of the patients in the minority group (p = 0.008). The time from presentation to OR for White/non-Hispanic patients was 1048.08 min vs. 735.71 for minority patients (p < 0.001).
The average total hospital charges for all patients was $44.689.2 vs. $44,613.48 for White/non-Hispanic patients and $44,934.16 for minority patients (p = 0.804). For the White/non-Hispanic group, commercial insurance was the most common primary payor at 31.5% of patients while for the minority group, the most common primary payor was vehicle insurance at 26.2% of patients. The second most common primary payor for White/non-Hispanic patients was Medicare at 21.4% while the second most common for minority patients was commercial insurance at 20.2%. Workman's compensation paid as the primary payor for 2.9% of White/non-Hispanic patients vs. 4.3% of minority patients. White/non-Hispanic patients utilized self-pay methods 7.3% of the time vs. 11.1% of the time for minority patients.
In this study, we explored the disparities between white/non-Hispanic and minority patients in mortality and adverse outcomes in traumatic brain injury patients presenting to a Level I trauma center in Portland, OR. Our results suggest that there are significant differences in mortality and adverse outcomes even given similar severity of injury, presenting factors, and financial factors. In our primary outcome, mortality, there was a large statistically significant difference between in-hospital death and hospital length of stay between groups. Accounting for potentially confounding factors such as severity of presenting injury, primary payor insurance mechanisms, hospital charges, and mechanism of injury, minority patients were at double the risk of in-hospital mortality than White/non-Hispanic patients. Regarding disparities in other aspects of care, there was no statistically significant difference in discharge disposition, though there was a trend toward higher rates of discharge to SNFs, Acute Care Facility-Hospitals, and Rehabilitation Facilities in the White/non-Hispanic group compared to the minority group. This could potentially demonstrate differences in access to such facilities, differences in insurance or payment methods, or even access to social work facilitation of these types of discharges.
Although there was no statistically significant difference in total hospital charges, our analyses did in fact show a trend regarding types of primary payors between the White/non-Hispanic patients and the minority patients in that the most common primary payor for White/non-Hispanic patients was commercial insurance vs. vehicle insurance for minority patients. This correlates well to our finding that there was a higher percentage of MVC-related injury in the minority group compared to the White/non-Hispanic group and may also help to explain their greater severity of injury at presentation. However, the additional increase in percentage of both Workman's compensation as well as self-pay seen in the minority group raises the concern that through these payor routes, minority patients may not have had similar access to discharge options such as SNFs or rehab facilities as did patients in the White/non-Hispanic group. Previous research has suggested that the influence of insurance is so strong that differences in coverage can increase the likelihood of availability to post-hospitalization care in less vulnerable populations (30). Yet later research has explored the extent of influence insurance has on discharge location and has found that despite similar insurance, minority patients were found to be discharged more frequently to home without care than to SNF or acute-care facility post-hospitalization. Similarly, these studies found that white patients with lower vulnerable group membership (VGM) were discharged quicker to SNF or acute-rehab facility, which has been shown to provide higher rates of functional recovery than home care, than patients of color with higher VGM scores (31–33).
There was a statistically significant difference in types of trauma between White/non-Hispanic patients and minority patients with minority patients presenting more often with penetrating trauma than their White/non-Hispanic counterparts. Minority patients also tended to have a higher rate of MVC as primary MOI and a higher rate of injury related to their work compared to the White/non-Hispanic patients. Minority patients tended to present with more severe injuries as demonstrated by both pure ISS as well as their tendency toward higher rates of more severe AIS at presentation. This may correlate to our findings that a higher number of minority patients were judged as operative patients compared to the White/non-Hispanic patients and similarly that minority patients had quicker times to OR than White/non-Hispanic patients. Although all of these findings as secondary outcomes are disparities in and of themselves, they do not explain the significant difference in our primary outcome of overall mortality between minority and White/non-Hispanic patients given that our primary analysis accounted for these severity factors.
It is well-studied in many other aspects of medicine and epidemiology that patients receive differing quality of healthcare and therefore have significantly different outcomes as a result of these health disparities. Not only do minority patients face persistent unconscious bias in the healthcare field and have differential access to baseline healthcare, it has also been shown that the healthcare that they do end up receiving likely is less adequate to handle surgically or medically complex issues due to shortages of necessary specialists, technology gaps, or timely access to services (24, 34). Previous research in neurosurgery and other surgically complex fields have demonstrated marked disparities in the procedural outcomes between minority and White/non-Hispanic patients (13, 22, 23, 35), however the current research regarding disparities in trauma management of minority patients still has yet to show the true inequality of care.
Among reasons that can be documented for these healthcare disparities in traumatic brain injury, one of the most likely explanations in our patient population was the sheer severity of injury at presentation and the likelihood of operation in our minority patients. This, alongside greater numbers of penetrative traumas and traumas related to MVC rather than fall, produced a much more severe clinical picture for our minority group than our White/non-Hispanic group. To explain these presenting findings, it is important to look at the history of trauma in regions and neighborhoods of predominantly minority persons. Through decades of housing red-lining, tax adjustments, and inequitable educational progress, neighborhoods primarily composed of minority persons in America have trended toward more dangerous, violent regions by no fault of the persons living in those regions (36–40). It is logical to assume that areas of increased risk of violence would have higher rates of violent trauma than those with better protections in place. Additionally, persons of minority status often live further from healthcare facilities adequately equipped to manage the complexity of the trauma with which the patient presents. Many studies have recently shown the extent of the disparities in both number and quality of providers but also the number and quality of the technology available at local or regional hospitals compared to the wealthier and often more academic hospitals placed in centers of higher economic advantage (12, 24, 34, 41).
However, there are many factors that could potentially influence a patient's mortality or secondary outcomes following a traumatic brain injury. The limitations of this paper lie in the fact that many of these factors are simply not recorded in our typical point of care healthcare system for trauma and therefore are much more difficult to study. Additionally, the retrospective nature of this study is a limitation. However, most epidemiological and sociological research looking at cultural and community-oriented factors related to healthcare can only be studied in a retrospective manner. In this paper, we were not able to examine all the pre-hospital factors influencing our patients outcomes and thus could only analyze the data points associated with the seemingly extensive Trauma One database for one of the two level 1 trauma centers in the state of Oregon, yet even with these data, there are numerous sociological, epidemiological, financial, psychological, and political factors at play that go unreported and therefore are under-researched (21). These factors typically thought of to be non-medical have consistently demonstrated pervasive, persistent, and poignant disparities between minority patients and White/non-Hispanic patients that have plagued our healthcare system in the United States (1, 3, 8, 10, 38, 42–44). These health disparities have been demonstrated to be independent of individual health choices; these inequalities are not biologically determined yet they plague only certain sects of our populations, permeating beyond healthcare. Not only do our minority patients have generations of well-documented medical trauma that prohibits a full trusting relationship of the American healthcare system but there are clearly also disparities in patient's lives pre-hospital such as access to routine healthcare, leniency in the workplace for regular healthcare maintenance, financial freedom for healthcare maintenance, safe working environments, housing opportunities in neighborhoods free of violence, full of healthy foods, and access to clear air/water, and many more that are simply not documented when our patients present with neuro-trauma (3, 8, 38, 42, 44). The health equity framework with which we claim to utilize to progress our medical care demands that we recognize these extraneous but highly influential aspects of our patients' lives. We must make ourselves aware of the macro-social factors which perpetuate this disproportionate suffering among our patients of color and act with the responsibility and privilege we carry in our communities to make these disparities known. We must not only care for our patients when we encounter them within our clinics, emergency departments (EDs), and operating rooms, but in the healthcare disparities that exist outside of the concrete confines of the traditional healthcare system. Thus, we have a responsibility to engage with the upstream factors in our patients' lives that put them at increased risk even prior to entering our facility's doors. The traumas of structural racism do not start the moment of impact from a fall or an MVC; our patients' traumas begin when they are raised in a discriminatory society and robbed of certain medical, social, political, and financial privileges accustomed by our White/non-Hispanic patients.
Our study is but one current research set to analyze the disparities in yet another aspect of medical care in the United States and certainly not the only one to find inequalities in management of trauma. It is imperative that we as a medical community target not only healthcare improvements to properly regulate and treat neurosurgical trauma, but focus our progress toward equitable community environments, living situations, financial and insurance-based payment plans, and trauma prevention efforts in order to better care for our patients of color both pre-hospital and once they arrive into our ED. Now with an ever-growing accumulation of research shining light to these racial and ethnic disparities in every corner of medical research, it is simply insufficient to produce more research, but it is ever more pertinent to call all medical providers to greater action.
In this study, we explored the in-hospital mortality outcomes and characteristics of adult patients who were admitted with traumatic brain injury to one of the two Level I trauma centers in Portland, OR between 2006 to October of 2017. Our data demonstrate a significant disparity in overall in-hospital mortality in minority patients, greater severity of presenting injury, higher incidence of MVC- or work-related injury, and higher operative rate than White/non-Hispanic patients given insignificant differences in insurance, hospital charges, and other accounting factors. Although these are novel findings for the field of neurosurgical trauma related to traumatic brain injury, they are repeated in other specialties and other medically complex patient populations in the American healthcare system. Research has been keen to identify these marked inequalities over the past couple of decades yet still there has not been a clear path to dismantling these disparities within the medical community. Treating patients under our care is our greatest privilege and responsibility as physicians. As such, we have a societal and professional duty to recognize and accept that the effects of structural racism have taken hold of our patients' health long before they arrive in our trauma bays, ICU beds, and operating tables. These disparities permeate our society and contribute to inequitable health outcomes, and we must take action to identify the factors which perpetuate this disproportionate suffering. Simply treating the minority of patients who require surgical intervention or clinical consultation is not enough. Our roles demand that we recognize these larger social factors acting upstream on our patients before they enter our fractioned healthcare system which often fosters the very mistrust that hides them from our otherwise watchful eyes in the first place. The necessary first step in providing an equitable healthcare system for all patients regardless of socioeconomic, racial, or ethnic status, is continued awareness of the pervasiveness and consistency of these medical disparities and emphasized efforts to improve the sociological factors that perpetuate them.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by OHSU Institutional Review Board. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
ER was the primary author on this manuscript and also assisted in methodology, concept design, and coordination. JN was the primary statistician of the project, designed the statistical methodology, and performed all necessary coordination tasks for data analysis. AR was the supervising physician on this project and was responsible for overseeing all aspects of its creation. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2021.690971/full#supplementary-material
1. Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press (US) (2003).
2. Churchwell K, Elkind MSV, Benjamin RM, Carson AP, Chang EK, Lawrence W, et al. Call to action: structural racism as a fundamental driver of health disparities: a presidential advisory from the American Heart Association. Circulation. (2020) 142:e454–68. doi: 10.1161/CIR.0000000000000936
3. Gee GC, Ford CL. Structural racism and health inequities. Du Bois Rev. (2011) 8:115–32. doi: 10.1017/S1742058X11000130
4. Kuzawa CW, Sweet E. Epigenetics and the embodiment of race: developmental origins of US racial disparities in cardiovascular health. Am J Hum Biol. (2009) 21:2–15. doi: 10.1002/ajhb.20822
5. Phelan JC, Link BG, Feldman NM. The genomic revolution and beliefs about essential racial differences. Am Soc Rev. (2013) 78:167–91. doi: 10.1177/0003122413476034
6. Meloni M. Scientific racism. In: Golden BL, Shier DR, editors. The Wiley-Blackwell Encyclopedia of Social Theory. Wiley Online Library (2017). p. 1–3.
7. Geneviève LD, Martani A, Shaw D, Elger BS, Wangmo T. Structural racism in precision medicine: leaving no one behind. BMC Med Ethics. (2020) 21:17. doi: 10.1186/s12910-020-0457-8
8. Smedley A, Smedley BD. Race as biology is fiction, racism as a social problem is real: anthropological and historical perspectives on the social construction of race. Am Psychol. (2005) 60:16. doi: 10.1037/0003-066X.60.1.16
9. Nazroo JY, Bhui KS, Rhodes J. Where next for understanding race/ethnic inequalities in severe mental illness? Structural, interpersonal and institutional racism. Sociol Health Illn. (2020) 42:262–76. doi: 10.1111/1467-9566.13001
10. Gao S, Kumar RG, Wisniewski SR, Fabio A. Disparities in health care utilization of adults with traumatic brain injuries are related to insurance, race, and ethnicity: a systematic review. J Head Trauma Rehabil. (2018) 33:E40–50. doi: 10.1097/HTR.0000000000000338
11. Haider AH, Weygandt PL, Bentley JM, Monn MF, Rehman KA, Zarzaur BL, et al. Disparities in trauma care and outcomes in the United States. J Trauma Acute Care Surg. (2013) 74:1195–205. doi: 10.1097/01586154-201305000-00002
12. Udyavar R, Perez S, Haider A. Equal access is quality: an update on the state of disparities research in trauma. Curr Trauma Rep. (2018) 4:25–38. doi: 10.1007/s40719-018-0114-6
13. Collaborative G. Mortality of emergency abdominal surgery in high-, middle- and low-income countries. Br J Surg. (2016) 103:971–88. doi: 10.1002/bjs.10151
14. Montgomery JR, Cain-Nielsen AH, Jenkins PC, Regenbogen SE, Hemmila MR. Prevalence and payments for traumatic injury compared with common acute diseases by episode of care in medicare beneficiaries, 2008-2014. JAMA. (2019) 321:2129. doi: 10.1001/jama.2019.1146
15. Madsen T, Erlangsen A, Orlovska S, Mofaddy R, Nordentoft M, Benros ME. Association between traumatic brain injury and risk of suicide. JAMA. (2018) 320:580. doi: 10.1001/jama.2018.10211
16. Crane PK, Gibbons LE, Dams-O'Connor K, Trittschuh E, Leverenz JB, Keene CD, et al. Association of traumatic brain injury with late-life neurodegenerative conditions and neuropathologic findings. JAMA Neurol. (2016) 73:1062. doi: 10.1001/jamaneurol.2016.1948
17. Hyder AA, Wunderlich CA, Puvanachandra P, Gururaj G, Kobusingye OC. The impact of traumatic brain injuries: a global perspective. NeuroRehabilitation. (2007) 22:341–53. doi: 10.3233/NRE-2007-22502
18. James SL, Theadom A, Ellenbogen RG, Bannick MS, Montjoy-Venning W, Lucchesi LR, et al. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. (2019) 18:56–87. doi: 10.1016/S1474-4422(18)30415-0
19. Branch CL, Boop F, Haglund MM, Dempsey RJ. Introduction. Neurosurgical opportunities in global health inequities. Neurosurg Focus. (2018) 45:E1. doi: 10.3171/2018.7.FOCUS18367
20. Johnson WD, Griswold DP. Traumatic brain injury: a global challenge. Lancet Neurol. (2017) 16:949–50. doi: 10.1016/S1474-4422(17)30362-9
21. Brenner EK, Grossner EC, Johnson BN, Bernier RA, Soto J, Hillary FG. Race and ethnicity considerations in traumatic brain injury research: incidence, reporting, and outcome. Brain Inj. (2020) 34:801–10. doi: 10.1080/02699052.2020.1741033
22. Chiu RG, Murphy BE, Zhu A, Mehta AI. Racial and ethnic disparities in the inpatient management of primary spinal cord tumors. World Neurosurg. (2020) 140:e175–84. doi: 10.1016/j.wneu.2020.04.231
23. Curry WT, Carter BS, Barker FG. Racial, ethnic, and socioeconomic disparities in patient outcomes after craniotomy for tumor in adult patients in the United States, 1988-2004. Neurosurgery. (2010) 66:427–38. doi: 10.1227/01.NEU.0000365265.10141.8E
24. Homo RL, Grigorian A, Chen J, Figueroa C, Chin T, Kuza CM, et al. Regional, racial, and mortality disparities associated with neurosurgeon staffing at level I trauma centers. Am Surg. (2020) 000313482098318. doi: 10.1177/0003134820983187
25. Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. (2007) 370:1453–7. doi: 10.1016/S0140-6736(07)61602-X
26. Clark DE, Black AW, Skavdahl DH, Hallagan LD. Open-access programs for injury categorization using ICD-9 or ICD-10. Inj Epidemiol. (2018) 5:11 doi: 10.1186/s40621-018-0149-8
27. Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. (1983) 70:41–55. doi: 10.1093/biomet/70.1.41
28. Vanderweele TJ. Principles of confounder selection. Eur J Epidemiol. (2019) 34:211–9. doi: 10.1007/s10654-019-00494-6
29. Ho DE, Imai K, King G, Stuart EA. MatchIt: nonparametric preprocessing for parametric causal inference. J Stat Softw. (2011) 42:1–28. doi: 10.18637/jss.v042.i08
30. Cuthbert JP, Corrigan JD, Harrison-Felix C, Coronado V, Dijkers MP, Heinemann AW, et al. Factors that predict acute hospitalization discharge disposition for adults with moderate to severe traumatic brain injury. Arch Phys Med Rehabil. (2011) 92:721–30.e3. doi: 10.1016/j.apmr.2010.12.023
31. Kowalski RG, Hammond FM, Weintraub AH, Nakase-Richardson R, Zafonte RD, Whyte J, et al. Recovery of consciousness and functional outcome in moderate and severe traumatic brain injury. JAMA Neurol. (2021) 78:548–57. doi: 10.1001/jamaneurol.2021.0084
32. Fuentes A, Schoen C, Kulzer RR, Long C, Bushnik T, Rath JF. Impact of racial-ethnic minority status and systemic vulnerabilities on time to acute TBI rehabilitation admission in an urban public hospital setting. Rehabil Psychol. (2019) 64:229–36. doi: 10.1037/rep0000260
33. Meagher AD, Beadles CA, Doorey J, Charles AG. Racial and ethnic disparities in discharge to rehabilitation following traumatic brain injury. J Neurosurg. (2015) 122:595–601. doi: 10.3171/2014.10.JNS14187
34. Zhu TH, Hollister L, Opoku D, Galvagno SM. Improved survival for rural trauma patients transported by helicopter to a verified trauma center: a propensity score analysis. Acad Emerg Med. (2018) 25:44–53. doi: 10.1111/acem.13307
35. Lucas FL, Stukel TA, Morris AM, Siewers AE, Birkmeyer JD. Race and surgical mortality in the United States. Ann Surg. (2006) 243:281–6. doi: 10.1097/01.sla.0000197560.92456.32
36. Martin MJ, Mccarthy B, Conger RD, Gibbons FX, Simons RL, Cutrona CE, et al. The enduring significance of racism: discrimination and delinquency among black American youth. J Res Adolesc. (2011) 21:662–76. doi: 10.1111/j.1532-7795.2010.00699.x
37. Lane SD, Rubinstein RA, Bergen-Cico D, Jennings-Bey T, Fish LS, Larsen DA, et al. Neighborhood trauma due to violence: a multilevel analysis. J Health Care Poor Underserved. (2017) 28:446–62. doi: 10.1353/hpu.2017.0033
38. Williams DR, Mohammed SA. Racism and health I. Am Behav Sci. (2013) 57:1152–73. doi: 10.1177/0002764213487340
39. Mesic A, Franklin L, Cansever A, Potter F, Sharma A, Knopov A, et al. The relationship between structural racism and black-white disparities in fatal police shootings at the state level. J Natl Med Assoc. (2018) 110:106–16. doi: 10.1016/j.jnma.2017.12.002
40. Krivo JL, Peterson DR, Kuhl CD. Segregation, racial structure, and neighborhood violent crime. Am J Sociol. (2009) 114:1765–802. doi: 10.1086/597285
41. Haider AH, Hashmi ZG, Zafar SN, Hui X, Schneider EB, Efron DT, et al. Minority trauma patients tend to cluster at trauma centers with worse-than-expected mortality. Ann Surg. (2013) 258:572–81. doi: 10.1097/SLA.0b013e3182a50148
42. Bailey ZD, Feldman JM, Bassett MT. How structural racism works—racist policies as a root cause of U.S. racial health inequities. N Engl J Med. (2021) 384:768–73. doi: 10.1056/NEJMms2025396
43. Egede LE. Race, ethnicity, culture, and disparities in health care. J Gen Intern Med. (2006) 21:667–9. doi: 10.1111/j.1525-1497.2006.0512.x
Keywords: mortality, disparities, inequities, TBI, neurotrauma, race
Citation: Richie EA, Nugent JG and Raslan AM (2021) Racial and Ethnic Inequities in Mortality During Hospitalization for Traumatic Brain Injury: A Call to Action. Front. Surg. 8:690971. doi: 10.3389/fsurg.2021.690971
Received: 05 April 2021; Accepted: 06 May 2021;
Published: 02 June 2021.
Edited by:
Claire Karekezi, Rwanda Military Hospital, RwandaReviewed by:
Laura Lippa, Ospedale di Livorno, ItalyCopyright © 2021 Richie, Nugent and Raslan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Emma A. Richie, cmljaGllQG9oc3UuZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.