- Key Laboratory of Oral Biomedical Research of Zhejiang Province, School of Stomatology, The Affiliated Hospital of Stomatology, Zhejiang University School of Medicine, Hangzhou, China
In the past half-century, considerable attention has been paid to oral and maxillofacial skeletal cyst, however, aneurysmal bone cyst (ABC), unlike other common bone diseases, still contours numerous unanswered questions in terms of classification, etiology and pathological mechanism. The purpose of this article was to evaluate the proportion of primary ABC and secondary ABC, and to assess the recurrence of ABC and related factors. A methodical search of Embase, MEDLINE, Cochrane Library, Web of Science was conducted for well-documented jaw aneurysmal bone cyst (JABC) cases. One hundred thirty-one articles were identified after database searching and 31 of them were included in our study for further research with 44 JABC cases. All the articles were analyzed by two separate authors. About 25% of the reported jaw aneurysmal bone cyst was secondary. Both the pathological classification and surgical treatment had a significant influence on recurrence rate (P = 0.0082, P = 0.0022), while patients' age or radiographic features rarely affected prognosis. Jaw aneurysmal bone cysts can present variable clinical and histological presentations. Recurrence may be attributed to omittance of underlying potential blood supply or conservative surgical protocol.
Introduction
Aneurysmal bone cyst (ABC) is a common skeletal bone lesion that usually observed in long bones and vertebra. Only 1.8% of ABCs, however, occur in the jaw bones (JABC). This rare occurrence was firstly recognized by Jaffe and Lichtenstein in 1942 (1). Several misconceptions still stand due to its scarceness and diversity in clinicopathology. In most cases, JABC presents itself as a rapid-growing, painful or painless, swelling defect with or without bony expansion (1). In some cases, it may be misdiagnosed as a malignant disease. Occasionally, however, an asymptomatic, slow-growing lesion can also be found as JABC. More recently, a review has updated the recurrence rate of head and neck ABCs with 94.4% patients free of disease in the average follow-up period of 3.59 years (2). This result was widely different from the old ones, which ranged from 21 to 50%. However, the risking factors of ABC recurrence remains an ongoing challenge due to the diverse clinical features and pathogeny.
For a very long time, ABC had been considered as a pseudocyst of hemodynamic or reaction origin, in other words, “primary ABC” or “secondary” to other diseases. Primary aneurysmal bone cyst could result from any traumatic cause which leads to intramedullary or subperiosteal hemorrhage if followed by an inaccurate repair process, or other hemodynamic states, it can create an enlarging vascular bed and erosion of bone (1, 3). The terminology “secondary aneurysmal bone cyst” is characterized as a haemorrhagic reaction of a pre-existing bone lesion. The initial lesion could be totally replaced by a secondary ABC or remains a part of it (4). This uncertainty increases the difficulty of distinguishing a pure ABC and an affiliated one, although histopathology is essential in the final diagnosis.
This review aims to evaluate the proportion of primary ABC and secondary ABC, and to assess the recurrence of ABC and related factors, which has certain clinical significance for the diagnosis of oral and maxillofacial skeletal cyst.
Materials and Methods
Search Strategy and Selection Criteria
Articles published in English journals from 1958 to October 2019 that reported ABCs in the jaws (maxilla or mandible) were included in the present study. Reported ABCs in animals, in locations other than jaw bones, in languages other than English and cases with disputed description or diagnosis of ABC were excluded.
We searched online databases (Embase, MEDLINE, Cochrane Library, Web of Science), electronic abstract databases and references in published articles.
We used the following keywords:
Jaw aneurysmal bone cyst OR aneurysmal bone cyst.
AND clinical OR radiograph OR pathology OR treatment OR surgery.
AND recurrence OR recurrence rate OR relapse rate.
AND case OR review OR analysis.
Two authors cross-checked the relevant cases and determined a final list of included articles.
Data Synthesis and Analysis
The proportion of different clinical features were calculated in this study, including gender, location, and radiographic behavior. We made estimates of the mean and standard deviation (SD). Chi-square test/Fisher's exact test was applied to evaluate the relation of recurrence and clinicopathology features and P < 0.05 was considered statistically significant. All statistical analyses were performed with GraphPad Prism 8.0 (GraphPad Software Inc., San Diego, CA, USA).
Results
General Description
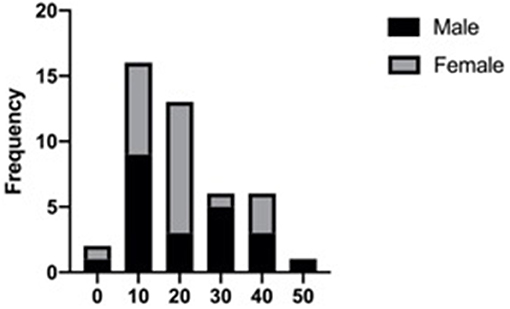
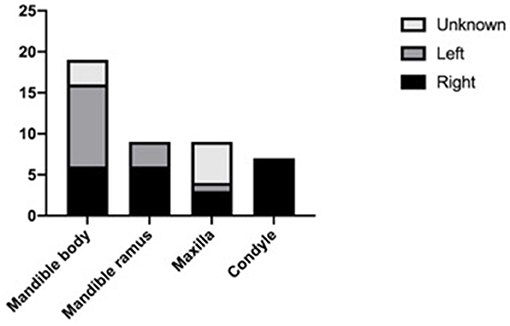
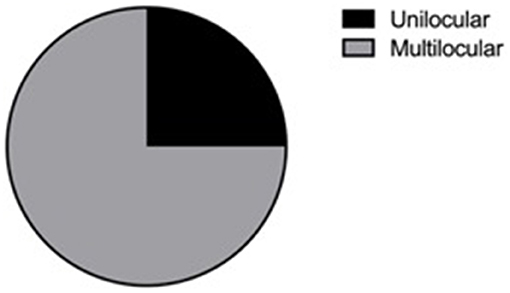
After excluding articles as per criteria, 31 articles with 44 JABC cases were included in the present review, with 22 (50%) males and 22 (50%) females ranging in age from 3 to 48 years (mean age: 19.25 ± 15.46 years). There was no gender predilection. The age distribution, on the other hand, was significant, 63.64% (n = 28) of the lesions had occurred in the first 2 decades of life (P < 0.05). The distribution of cases according to age and gender groups is presented in Figure 1. Distribution of location were presented in Figures 2, 3, with 9 cases in maxilla (20.45%) and 35 cases in mandible (79.54%). Figure 3 showed that 75% of patients had multilocular presentation in radiographic examination and only 25% were presented as unilocular lesions. The majority of patients had shown with rapidly growing swelling as a significant clinical feature, in several cases also with localized pain. Table 1 encompasses data regarding the clinical features and other parameters of JABCs.
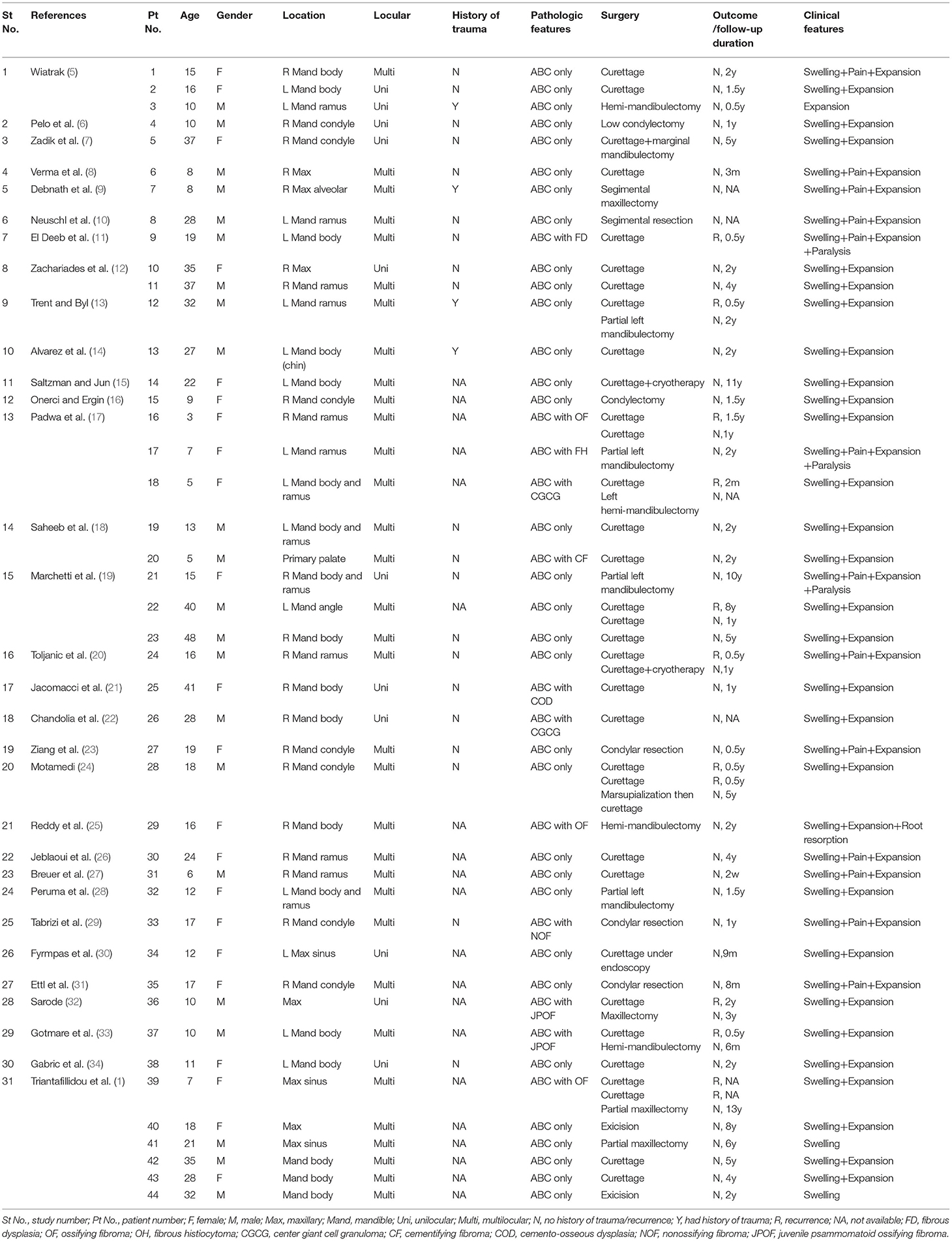
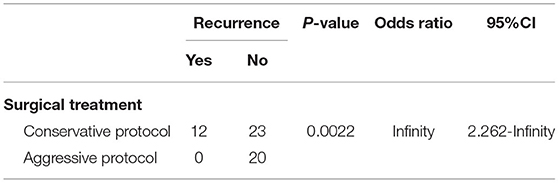
Table 1. Summary OF clinicoradiographic and histopathologic features of 31 studies of jaw aneurysmal bone cyst.
Recurrence Analysis
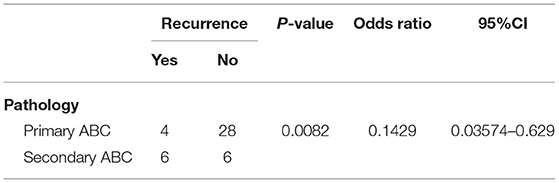
Focusing on the recurrence status, it was surprising to find a distinguishable division between primary ABC and secondary ABC, the latter possesses a higher recurrence rate than the former (P = 0.0082) (Table 2). A similar result was found when surgical procedure was involved (Table 3). Forty-four patients had experienced 55 surgery with 12 cases of recurrence. Patients underwent radical surgery such as Hemi-mandibulectomy and partial mandibulectomy retained a lower recurrence rate than conservative curettage or excision (P = 0.0022). Age and radiographic features (unilocular or multilocular) had no significant influence on the relapse rate.
Discussion
Jaw aneurysmal bone cyst occurs predominately in young individuals under the age of 20 (3, 35). Most studies present a similar balance in gender difference (3, 4, 35). Our review showed similar results that are compatible with previously reported literature. Rutter et al. (36) and Biesecker et al. (37) found a slight bias toward female patients, as they accounted for 66 cases (59%) in a total sample of 105. Posterior of mandible is the most common site for JABC (35, 38). JABC can have variable clinical features, however, most of them would show swelling and bony expansions. In several cases, it also exhibits an asymptomatic lesion occasionally discovered as radiolucency on routine radiography. JABC has variable radiological appearances and should be considered in the differential diagnosis of any unilocular or multilocular radiolucency of the jaws and any mixed radiopaque-radiolucent lesion (35, 39). The current case series showed a tendency toward multilocular defect with soap-bubble or honeycomb appearance. Other complications like pathological fracture, paralyzation, and malocclusion are not very common. El Deeb et al. (11), Laskin et al. (40) and Shafer et al. (41) reported the presence of trauma history in this situation, which theoretically backs the assumption of intramedullary or subperiosteal hemorrhage.
In terms of diagnosing JABC, comprehensive pre-surgical examination is important, particularly the vascular type which accounts for 95% in JABCs. Brisk hemorrhage can be rebellious under this circumstance (5, 6, 8). Clinically, a multilocular, rapid-growing, destructive skeletal lesion is supposed to undertake digital subtraction angiography (DSA) or magnetic resonance angiography (MRA) to clarify the blood supplementary. Although the majority of oral and maxillofacial bone cysts cause no concern, thus hard tissue evaluation like panoramic radiograph and cone beam CT scan is generally sufficient. Highly vascularized lesions such as JABC and central hemangioma would result in unexpectable crisis, especially in the absence of blood preparation. Möller et al. (39) reported a JABC lesion furnished by ipsilateral external carotid artery. At the same time, Padwa et al. (17) found a displacement of internal maxillary superficial temporal arteries in a JABC patient. Wiatrak et al. (5) found an expansion of lingual, facial and internal maxillary arteries surrounding the pathological field. Related to rich blood supply, embolization before surgical procedure can be an effective measure to avoid uncontrollable bleeding.
Precisely because of the diversiform of JABC's clinical and radiographic features, the differential diagnosis ranges from simple bone cyst, central giant cell granuloma, ameloblastoma, odontogenic keratocyte, ossifying fibroma. Histopathology, as usual, is the golden standard for the final diagnosis. Surgical exploration can be an accessory for preliminary judgment.
Due to the absence of an epithelial wall, JABC was considered as a pseudocyst until 2004. It usually consists of a fibrous connective tissue stroma with blood-filled sinusoids, multinucleated giant cells, and irregular osteoid (42, 43). According to different histopathologic features, JABC can be segmented into 3 types. Vascular type is characterized by a loose stroma, numerous engorged blood-filled sinusoids. When occurring as the vascular type, it is very common to observe risky bleeding during surgery and extensive bony destruction with spread in the soft tissues. The solid type is identified by a dense, fibrous stroma, few blood vessels and without severe bleeding during the surgery (6, 44, 45). The third, mixed type lies somewhere in between the previous two variants. Proportion of each type varies between studies. Pelo et al. (6) reported that vascular type is the most common among the three classes. This concurs with Vergel et al. (46) who have reported that the solid variety was least common as opposed to Henriques et al. (47) who proposed that the solid variety is the most common.
When it comes back to the question of whether ABC is a primary or secondary lesion, opinions are controversial and still open to interpretation. Based on the classic etiologic hypothesis, primary ABC can result from any intramedullary or subperiosteal hemorrhage in which trauma may play a role in this process, or other altered hemodynamic state followed by the expansion of vascular bed and erosion of bone. Secondary ABC, on the other hand, is a phenomenon that originates from a previous osseous lesion (1, 3, 48). The exact proportion of primary and secondary ABC remains debatable as well. A 25% incidence of secondary JABCs with other pathological lesions was obtained in our study, similar to the findings of Pedwa et al. (22%) (17). This varies remarkably varies from Triantafillidou et al. research (50%) (1). Arora et al. (49) reported a result of 14.8% secondary ABC. Besides, Sun et al. reported an incidence of secondary JABCs of 76.5% with a detailed presentation of 17 JABC patients, which indicted that most secondary JABCs are lesions where the primary disease has been completely overlapped with aneurysmal change (50, 51). These differences may be a reflection of publication bias or reporting bias (where histopathology may not have been the focus of publication or the secondary lesion may be overlooked).
Another problem with JABC is the perplexing high recurrence. Ectopic anatomy and incomplete surgical procedure may both explain this issue in a specific type, that is, the exitance of communication between the primary bone lesion and surrounding arteries. Curettage is the most common and convenient solution and also holds a recurrence rate ranging from 21 to 50% in JABC patients (3). On this particular occasion, the supplementary artery is the fundamental problem rather than the cyst itself. Simple curettage or excision will not disconnect the blood supply nor correct the displacement of vessels which logically leads to a second expansion. Pedwa et al. (17), Trent et al. (13), Sarode et al. (32) and Gotmare et al. (33) all reported JABCs with initial curettage treatment then followed by recurrence and a second thorough hemi-mandibulectomy or maxillectomy were needed. Reddy et al. (25) also presented a relapse case in which this patient had taken over a second curettage along with cryotherapy. All of the above patients have not suffered any further recurrence, which verified that handling with blood supply and the primary bone lesion could be a meaningful treatment to avoid recurrence. Enlarged resection with ligation of nearby vessels, cryotherapy, embolization and sclerotherapy should be taken into consideration when countered with a recurrent JABC patient.
Conclusion
From the discussion above, the acknowledgment of jaw aneurysmal bone cyst remains an ongoing challenge due to the epidemiology multiformity. The higher recurrence rate in secondary JABC may result from diverse histopathology of primary lesions, yet it requires further research. For clinical practitioners, the manifestation of JABC may be diverse, but in a single case, the biological behavior always matches pathological features, also prompting consistent and appropriate treatment. We here advocate comprehensive clinical and radiographic examination in suspected JABC patients, especially the transmission between the lesion and well-known arteriovenous in head and neck region, to avoid unexpected severe bleeding. Treatment should be cautiously considered in every patient to balance the recurrence and surgical injury.
Author Contributions
YL: acquisition of data, laboratory or literature search. JZ: drafting of article and critical revision. JS: conception and design of review, final approval, and guarantor of manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study has been jointly supported by National Natural Science Foundation of China (81801024) and Department of Health of Zhejiang Province (2017KY449).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2021.678696/full#supplementary-material
References
1. Triantafillidou K, Venetis G, Karakinaris G, Iordanidis F, Lazaridou M. Variable histopathological features of 6 cases of aneurysmal bone cysts developed in the jaws: review of the literature. J Cranio-Maxillofac Surg. (2012) 40:e33–8. doi: 10.1016/j.jcms.2011.03.010
2. Richardson J, Litman E, Stanbouly D, Lee KC, Philipone E. Aneurysmal bone cyst of the head & neck: a review of reported cases in the literature. J Stomatol Oral Maxillofac Surg. (2021) 21:38–40. doi: 10.1016/j.jormas.2021.01.014. [Epub ahead of print].
3. Motamedi MHK, Navi F, Eshkevari PS, Jafari SM, Shams MG, Taheri M, et al. Variable presentations of aneurysmal bone cysts of the jaws: 51 cases treated during a 30-year period. J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg. (2008) 66:2098–103. doi: 10.1016/j.joms.2008.05.364
4. Buraczewski J, Dabska M. Pathogenesis of aneurysmal bone cyst: relationship between the aneurysmal bone cyst and fibrous dysplasia of bone. Cancer. (1971) 28:597–604. doi: 10.1002/1097-0142(197109)28:3<597::AID-CNCR2820280311>3.0.CO;2-I
5. Wiatrak B.J. Alternatives in the management of aneurysmal bone cysts of the mandible. Int J Pediatr Otorhinolaryngol. (1995) 31:247–57. doi: 10.1016/0165-5876(94)01082-9
6. Pelo S, Gasparini G, Boniello R, Moro A, Amoroso PF. Aneurysmal bone cyst located in the mandibular condyle. Head Face Med. (2009) 5:8. doi: 10.1186/1746-160X-5-8
7. Zadik Y, Aktaş A, Drucker S, Nitzan DW. Aneurysmal bone cyst of mandibular condyle: a case report and review of the literature. J Cranio-Maxillofac Surg. (2012) 40:e243–8. doi: 10.1016/j.jcms.2011.10.026
8. Verma RK, Kumar R, Bal A, Panda NK. Aneurysmal bone cyst of maxilla with ectopic molar tooth–A case report. Otolaryngol Pol. (2013) 67:302–7. doi: 10.1016/j.otpol.2013.06.004
9. Debnath SC, Adhyapok AK, Hazarika K, Malik K, Vatsyayan A. Aneurysmal bone cyst of maxillary alveolus: a rare case report. Contemp Clin Dent. (2016) 7:111–3. doi: 10.4103/0976-237X.177098
10. Neuschl M, Reinert S, Guelicher D, Neuschl J, Hoffmann J. Aneurysmal bone cyst of the ascending ramus mandible. A case report. J Cranio-Maxillofac Surg. (2014) 42:E36–8. doi: 10.1016/j.jcms.2013.05.027
11. El Deeb M, Sedano HO, Waite DE. Aneurysmal bone cyst of the jaws: report of a case associated with fibrous dysplasia and review of the literature. Int J Oral Surg. (1980) 9:301–11. doi: 10.1016/S0300-9785(80)80039-1
12. Zachariades N, Vairaktaris E, Mezitis M, Triantafyllou D, Papavassiliou D, Economopoulou P. Aneurysmal bone cyst of the jaws. Review of the literature and report of 2 cases. Int J Oral Maxillofac Surg. (1986) 15:534–40. doi: 10.1016/S0300-9785(86)80055-2
13. Trent C, Byl FM. Aneurysmal bone cyst of the mandible. Ann Otol Rhinol Laryngol. (1993) 102:917–24. doi: 10.1177/000348949310201202
14. Alvarez-Martinez E-DC, Posso-Zapata M-V, Florez-Arango V-A, Lopera-Valle J-S, Ardila C-M. Aneurysmal bone cyst of the mandible with conservative surgical management: a case report. J Clin Exp Dent. (2019) 11:e561–4. doi: 10.4317/jced.55771
15. Saltzman EI, Jun MY. Aneurysmal bone cyst of the mandible: report of a case. J Surg Oncol. (1981) 17:385–94. doi: 10.1002/jso.2930170412
16. Onerci M, Ergin NT. Aneurysmal bone cyst of the mandible. Laryngorhinootologie. (1996) 75:306–8. doi: 10.1055/s-2007-997584
17. Padwa BL, Denhart BC, Kaban LB. Aneurysmal bone cyst-”plus”: a report of three cases. J Oral Maxillofac Surg. (1997) 55:1144–52. doi: 10.1016/S0278-2391(97)90296-2
18. Saheeb BDO, Ojo MA, Obuekwe ON. Aneurysmal bone cyst: a primary or secondary lesion? Niger J Clin Pract. (2007) 10:243–6.
19. Marchetti C, Bacchini P, Tomasetti N, Bertoni F. Aneurysmal bone cyst: a radiolucent lesion of the mandible. Report of 3 cases. J Oral Maxillofac Surg. (2012) 70:1102–8. doi: 10.1016/j.joms.2011.04.018
20. Toljanic JA, Lechewski E, Huvos AG, Strong EW, Schweiger JW. Aneurysmal bone cysts of the jaws: a case study and review of the literature. Oral Surg Oral Med Oral Pathol. (1987) 64:72–77. doi: 10.1016/0030-4220(87)90119-8
21. Jacomacci WP, Veloso Perdigão JP, Veltrini VC, Farah GJ, Tolentino ES, Vessoni Iwaki LC, et al. Associated aneurysmal bone cyst and cemento-osseous dysplasia: a case report and review of the literature. Gen Dent. (2017) 65:28–32.
22. Chandolia B, Bajpai M, Arora M. Central giant cell granuloma with aneurysmal bone cyst in a 28-year male patient: a rare concurrence. Jcpsp J Coll Physicians Surg Pak. (2018) 28:S128–9. doi: 10.29271/jcpsp.2018.06.S128
23. Ziang Z, Chi Y, Minjie C, Yating Q, Xieyi C. Complete resection and immediate reconstruction with costochondral graft for recurrent aneurysmal bone cyst of the mandibular condyle. J Craniofac Surg. (2013) 24:e567–70. doi: 10.1097/SCS.0b013e31829ad227
24. Motamedi MHK. Destructive aneurysmal bone cyst of the mandibular condyle: report of a case and review of the literature. J Oral Maxillofac Surg. (2002) 60:1357–61. doi: 10.1053/joms.2002.35744
25. Reddy AVS, Reddy KRK, Prakash AR, Rajinikanth Vidhyadhari P. Juvenile ossifying fibroma with aneurysamal bone cyst: a case report. J Clin Diagn Res JCDR. (2014) 8:ZD01–2.
26. Jeblaoui Y, Ben Neji N, Haddad S, Zribi A, Neji R, Boussafa H, et al. Mandibular aneurismal bone cyst mimicking a malignant tumor. Rev Stomatol Chir Maxillofac. (2007) 108:238–40. doi: 10.1016/j.stomax.2006.10.006
27. Breuer C, Paul H, Zimmermann A, Braunstein S, Schaper J, Mayatepek E, et al. Mandibular aneurysmal bone cyst in a child misdiagnosed as acute osteomyelitis: a case report and a review of the literature. Eur J Pediatr. (2010) 169:1037–40. doi: 10.1007/s00431-010-1138-2
28. Perumal C, Mohamed A, Singh A. New bone formation after ligation of the external carotid artery and resection of a large aneurysmal bone cyst of the mandible with reconstruction: a case report. Craniomaxillofacial Trauma Reconstr. (2012) 5:59–64. doi: 10.1055/s-0031-1293519
29. Tabrizi R, Nejhad ST, Ozkan BT. Nonossifying fibroma secondary to aneurysmal bone cyst in the mandibular condyle. J Craniofac Surg. (2011) 22:1157–8. doi: 10.1097/SCS.0b013e318210bb71
30. Fyrmpas G, Constantinidis J, Televantou D, Konstantinidis I, Daniilidis J. Primary aneurysmal bone cyst of the maxillary sinus in a child: case report and review of the literature. Eur Arch Otorhinolaryngol. (2006) 263:695–8. doi: 10.1007/s00405-006-0037-7
31. Ettl T, Staender K, Schwarz S, Reichert TE, Driemel O. Recurrent aneurysmal bone cyst of the mandibular condyle with soft tissue extension. Int J Oral Maxillofac Surg. (2009) 38:699–703. doi: 10.1016/j.ijom.2009.01.014
32. Sarode SC, Sarode GS, Ingale Y, Ingale M, Majumdar B, Patil N, et al. Recurrent juvenile psammomatoid ossifying fibroma with secondary aneurysmal bone cyst of the maxilla: a case report and review of literature. Clin Pract. (2018) 8:69–72. doi: 10.4081/cp.2018.1085
33. Gotmare SS, Tamgadge A, Tamgadge S, Kesarkar KS. Recurrent psammomatoid juvenile ossifying fibroma with aneurysmal bone cyst: an unusual case presentation. Iran J Med Sci. (2017) 42:603–6.
34. Gabric D, Manojlovic S, Zadravec D, Boras VV, Virag M. Unusual radiographic presentation of an aneurysmal bone cyst of the mandible. Oral Radiol. (2017) 33:71–75. doi: 10.1007/s11282-016-0239-7
35. Urs AB, Augustine J, Chawla H. Aneurysmal bone cyst of the jaws: clinicopathological study. J Maxillofac Oral Surg. (2014) 13:458–63. doi: 10.1007/s12663-013-0552-1
36. Ruiter DJ, Van Rijssel TG, Van Velde ED. Aneurysmal bone cysts. A clinicopathological study of 105 cases. Cancer. (1977) 39:2231–9. doi: 10.1002/1097-0142(197705)39:5<2231::AID-CNCR2820390541>3.0.CO;2-Q
37. Biesecker JL, Marcove RC, Huvos AG, Mike V. Aneurysmal bone cysts. A clinicopathologic study of 66 cases. Cancer. (1970) 26:615–25. doi: 10.1002/1097-0142(197009)26:3<615::AID-CNCR2820260319>3.0.CO;2-I
38. Motamedi MHK, Yazdi E. Aneurysmal bone cyst of the jaws: analysis of 11 cases. J Oral Maxillofac Surg. (1994) 52:471–5. doi: 10.1016/0278-2391(94)90343-3
39. Möller B, Claviez A, Moritz J-D, Leuschner I, Wiltfang J. Extensive aneurysmal bone cyst of the mandible. J Craniofac Surg. (2011) 22:841–4. doi: 10.1097/SCS.0b013e31820f3703
41. Shafer WG, Hine MK, Levy BM, Rajendran R, Sivapathasundharam B. A Textbook of Oral Pathology. Philadelphia: Saunders (1983).
42. Roychoudhury A, Rustagi A, Bhatt K, Bhutia O, Seith A. Aneurysmal bone cyst of the mandible: report of 3 cases. J Oral Maxillofac Surg. (2009) 67:1996–2004. doi: 10.1016/j.joms.2009.04.021
43. Rapidis AD, Vallianatou D, Apostolidis C, Lagogiannis G. Large lytic lesion of the ascending ramus, the condyle, and the infratemporal region. J Oral Maxillofac Surg. (2004) 62:996–1001. doi: 10.1016/j.joms.2004.04.009
44. Perrotti V, Rubini C, Fioroni M, Piattelli A. Solid aneurysmal bone cyst of the mandible. Int J Pediatr Otorhinolaryngol. (2004) 68:1339–44. doi: 10.1016/j.ijporl.2004.05.001
45. Zak MJ, Spinazze DJ, Obeid G. Mildly symptomatic radiolucency of the mandible. J Oral Maxillofac Surg. (1998) 56:656–61. doi: 10.1016/S0278-2391(98)90468-2
46. Vergel De Dios AM, Bond JR, Shives TC, McLeod RA, Unni KK. Aneurysmal bone cyst. A clinicopathologic study of 238 cases. Cancer. (1992) 69:2921–31. doi: 10.1002/1097-0142(19920615)69:12<2921::AID-CNCR2820691210>3.0.CO;2-E
47. Henriques ACG, de Vasconcelos Carvalho M, da Costa Miguel MC, Queiroz LMG, da Silveira EJD. Clinical pathological analysis of nine cases of aneurysmal bone cyst of the jaws in a Brazilian population. Eur Arch Otorhinolaryngol. (2012) 269:971–6. doi: 10.1007/s00405-011-1705-9
48. Bernier JL, Bhaskar SN. Aneurysmal bone cysts of the mandible. Oral Surg Oral Med Oral Pathol. (1958) 11:1018–28. doi: 10.1016/0030-4220(58)90142-7
49. Arora SS, Paul S, Arora S, Kapoor V. Secondary jaw aneurysmal bone cyst (JABC)–a possible misnomer? A review of literature on secondary JABCs, their pathogenesis and oncogenesis. J Oral Pathol Med. (2014) 43:647–51. doi: 10.1111/jop.12132
50. Kransdorf MJ, Sweet DE. Aneurysmal bone cyst: concept, controversy, clinical presentation, and imaging. AJR Am J Roentgenol. (1995) 164:573–80. doi: 10.2214/ajr.164.3.7863874
Keywords: aneurysmal bone cyst, recurrence, clinicopathology, jaw bone, radiograph
Citation: Liu Y, Zhou J and Shi J (2021) Clinicopathology and Recurrence Analysis of 44 Jaw Aneurysmal Bone Cyst Cases: A Literature Review. Front. Surg. 8:678696. doi: 10.3389/fsurg.2021.678696
Received: 10 March 2021; Accepted: 19 May 2021;
Published: 23 June 2021.
Edited by:
Claudio Roberto Cernea, University of São Paulo, BrazilReviewed by:
AB Zulkiflee, University Malaya Medical Centre, MalaysiaSérgio Gonçalves, University of São Paulo, Brazil
Copyright © 2021 Liu, Zhou and Shi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jue Shi, ZGVudGlzdHNqQHpqdS5lZHUuY24=
 Yu Liu
Yu Liu Jinhan Zhou
Jinhan Zhou Jue Shi
Jue Shi