
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Surg. , 25 May 2021
Sec. Neurosurgery
Volume 8 - 2021 | https://doi.org/10.3389/fsurg.2021.669433
This article is part of the Research Topic Case Reports in Neurosurgery: 2021 View all 12 articles
Background: Anterior inferior cerebellar artery (AICA) aneurysms are relatively rare in clinical practice, accounting for <1% of all intracranial arteries. After the diagnosis and location are confirmed by angiography, magnetic resonance, and other imaging examinations, interventional, or surgical treatment is often used, but some complex aneurysms require reconstructive surgery.
Case Description: An 8-year-old male child was admitted to the hospital due to sudden disturbance of consciousness for 2 weeks. The head CT showed hematocele in the ventricular system with subarachnoid hemorrhage in the basilar cistern and annular cistern. On admission, he was conscious, answered correctly, had a soft neck, limb muscle strength was normal, and had no cranial nerves or nervous system abnormalities. A preoperative examination showed the right side of the anterior distal arteries class under the circular wide neck aneurysm, the distal anterior inferior cerebellar artery supplying a wide range of blood to the cerebellum, the ipsilateral posterior inferior cerebellar artery absent, and the aneurysm close to the VII, VIII nerves. The aneurysm was successfully treated by aneurysm resection and intracranial artery anastomosis in situ of a2 AICA-a2 AICA.
Conclusions: AICA aneurysms are relatively rare; in this case, a complex wide-necked aneurysm was successfully treated by aneurysm resection and anastomosis in situ of a2 AICA-a2 AICA. This case can provide a reference for the surgical treatment of complex anterior cerebellar aneurysms.
- In the treatment of complex aneurysms, bypass reconstruction can effectively ensure the patency of the distal posterior circulation artery and avoid cerebral infarction.
- In situ anastomosis technology has good matching of vascular diameter and wall and high expected patency rate, and its patency can be effectively verified by intraoperative fluorescence contrast and ultrasound Doppler.
- It can provide reference for the surgical treatment of complex anterior cerebellar small aneurysms.
Anterior inferior cerebellar artery (AICA) aneurysms are rare clinically, accounting for <1% of all intracranial artery aneurysm. After the diagnosis and location are confirmed by angiography, magnetic resonance, and other imaging examinations, aneurysms are usually treated with intervention embolization or surgery (1–3). However, under the different anatomical locations and morphology of an AICA aneurysm, what kind of treatment is the most effective? There is still no unified conclusion. We report a case of a complex AICA aneurysm. The patient was admitted due to sudden disturbance of consciousness 2 weeks earlier. Physical examination on admission: clear, accurate answers; soft neck; normal muscle strength of limbs; no abnormality in cranial nerve and nervous system examination. CT showed that the ventricular system had hematocele, accompanied by subarachnoid hemorrhage in the basal cistern and annular cistern. Digital subtraction angiography revealed a circular wide-necked aneurysm of the distal AICA with an aneurysm size of about 5.2*4.8 mm. The aneurysm was isolated and resected; intracranial anastomosis in situ of a2 AICA-a2 AICA was performed. As far as we know, reports of similar cases are rare. Combined with the patient's clinical characteristics, surgical techniques, results, and literature review, the report is as follows:
The patient, an 8-year-old male, was admitted December 4, 2020, due to sudden disturbance of consciousness 2 weeks earlier. The patient had a sudden headache and consciousness disturbance 2 weeks earlier, and the head CT showed that the ventricular system had hematocele, accompanied by subarachnoid hemorrhage in the basal cistern and annular cistern. The patient was conscious after symptomatic treatment and then transferred to our hospital for further diagnosis and treatment. Physical examination on admission: clear, accurate answers, soft neck, normal muscle strength of limbs, no abnormality in cranial nerve, and nervous system examination. Digital subtraction angiography revealed a circular wide-necked aneurysm of the distal AICA with an aneurysm size of about 5.2*4.8 mm. The distal AICA supplied a wide range of blood, and the ipsilateral posterior inferior cerebellar artery was absent as shown in Figures 1A–C. Magnetic resonance imaging (MRI) shows that the aneurysm was located lateral to the internal auditory canal (IAC), near the VII, VIII nerves. The right AICA was diagnosed, Hunt–Hess class I.
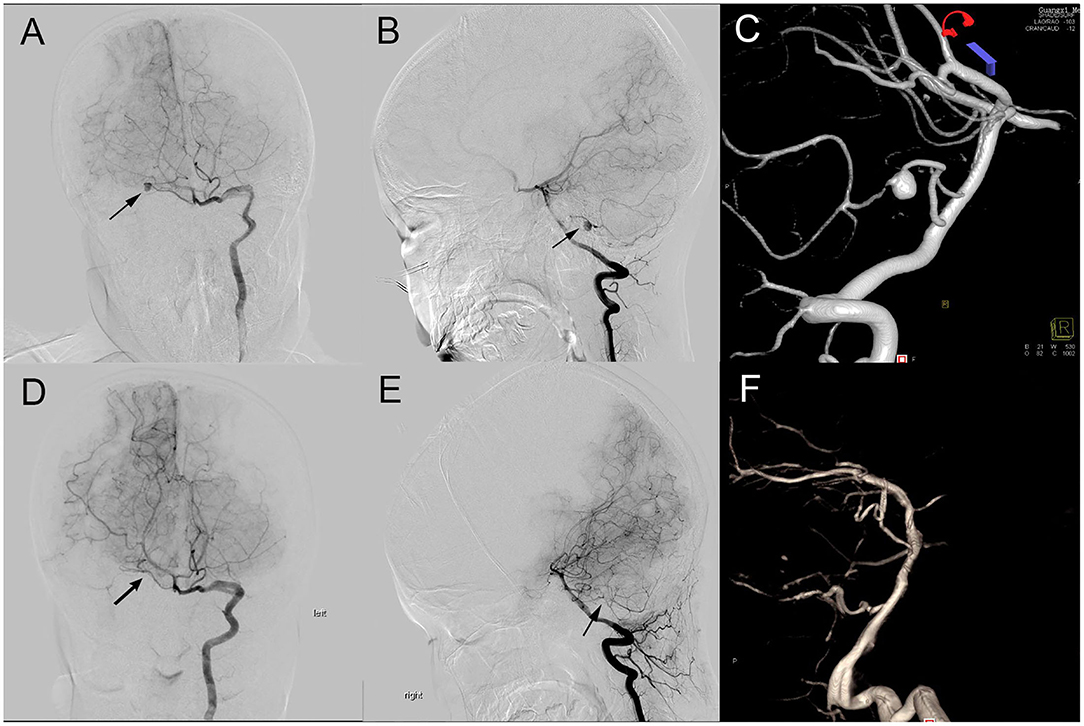
Figure 1. Preoperative and postoperative DSA comparison. (A–C): Preoperative DSA (A, A-P view; B, lateral view) showing an aneurysm (black arrow) located at main trunk of the right AICA; (D–F): Preoperative DSA (D, A-P view; E, lateral view) showing the aneurysm disappeared and the distal AICA patency.
Craniotomy of the aneurysm by retrosigmoid approach and anastomosis of the AICA was performed under general anesthesia. Intraoperatively, the aneurysm was found to be located in the middle segment of the right AICA, between the facial auditory nerve and the posterior cranial nerve. The aneurysm was closely adhered to the surrounding arachnoid with a wide neck and unclear boundary between the neck and the parent artery (Figure 3A). It is estimated that simple clamping is difficult to ensure patency of the parent artery, so we decided to separate the aneurysm from the surrounding adhesion carefully and remove it and part of the parent artery. After dissociating the proximal and distal vessels of the AICA, end-to-end intracranial vascular anastomosis of a2 AICA-a2 AICA was performed in situ (the schematic diagram of the operation is shown in Figure 2), and intraoperative fluorescence angiography was performed to confirm the patency of the anastomotic vessels (Figures 3B,C). The patient recovered well after the operation with no facial paralysis, hoarseness, or dysphagia, and limb muscle strength is normal with no ataxia. Cerebrovascular angiography before discharge indicated that the aneurysm disappeared, the distal and proximal ends of the AICA had patency, and the blood supply range was the same as before operation (Figures 1D–F).
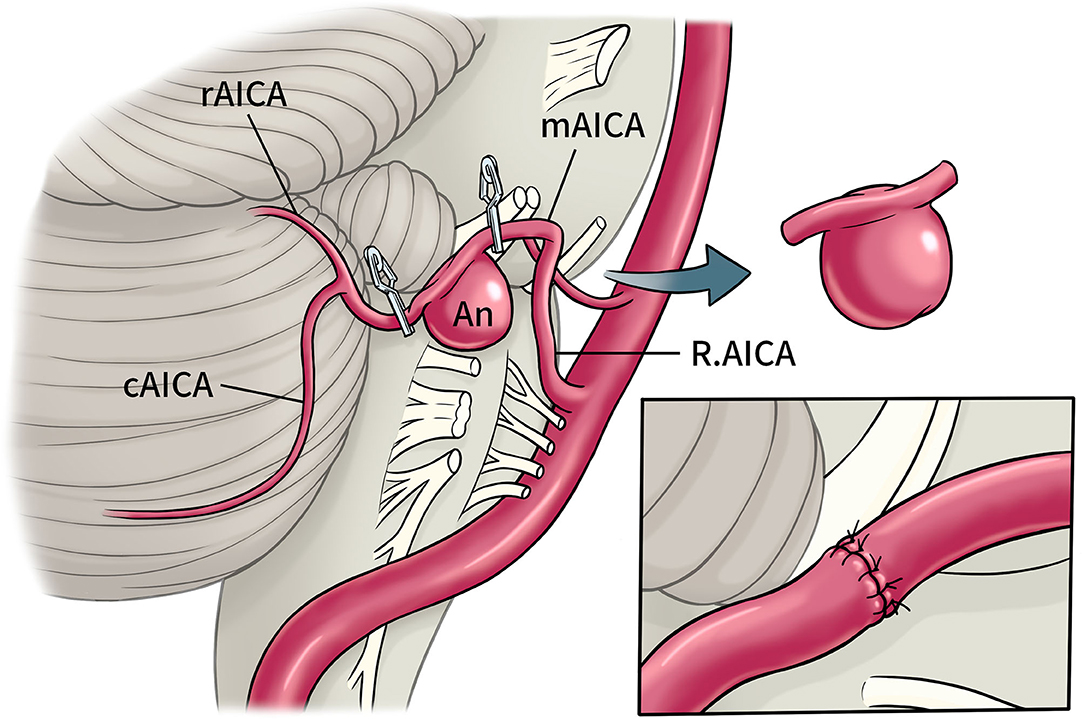
Figure 2. Schematic diagram of operation. Right AICA aneurysm located in a2 segments, intracranial artery anastomosis in situ was perform after trapping and resection. (cAICA, caudal trunk of AICA; mAICA, main trunk of AICA; rAICA, rostral trunk of AICA; a2, lateral pontine segments of AICA).
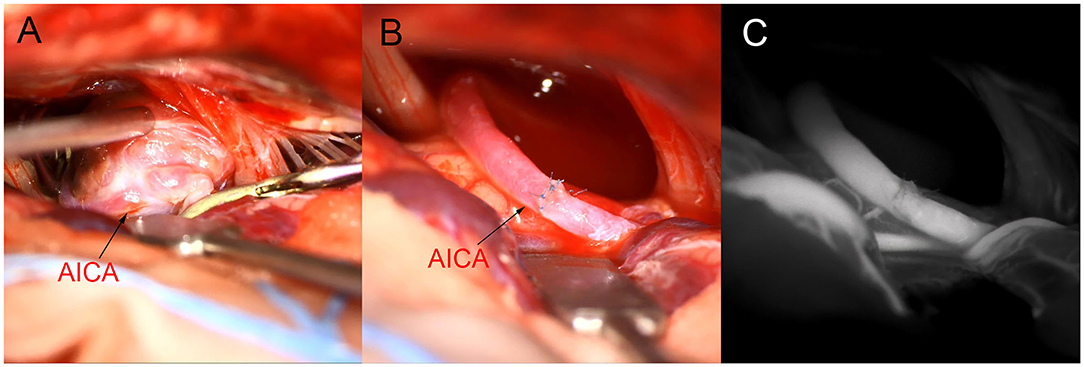
Figure 3. Intraoperative image. (A): Aneurysm neck and parent artery were not clearly defined. (B,C): a2AICA-a2AICA anastomosis in situ after aneurysm resection, intraoperative fluorescence imaging confirmed patency.
AICA aneurysms are relatively rare, and the treatment reports of each center are mainly individual cases and small case series. The total number of aneurysms of the AICA reported by major neurosurgery centers in China accounts for about 0.15–0.3% (1, 2, 4). Symptomatic rupture of the AICA aneurysm is mainly associated with subarachnoid hemorrhage. Some patients show symptoms of mass effect in the cerebellar pontine angle, such as hearing loss, facial paralysis, hoarseness, dysphagia, dizziness, etc., which is related to the location of the aneurysm. Preoperative imaging, the thin layer of magnetic resonance, the bone of the skull base combination CTA reconstruction can effectively locate the aneurysm. AICA aneurysms can be cured by interventional embolization, craniotomy clipping, isolation, and other methods, and the overall effect is satisfied (3, 5–8). A few complex aneurysms require vascular reconstruction (9) and artery anastomosis of the occipital artery. Anterior inferior cerebellar is more common.
According to the relationship between different segments of AICA and the IAC, aneurysm of the AICA can be divided into anterior, internal, and posterior segments of IAC (2). According to the AICA and cerebellar pontine angle region nerve anatomical position relationship, it can be divided into the a1: anterior pontine segments, a2: lateral pontine segments, a3: flocculopeduncular segments, and a4: cortical segments (5, 10). a2 gives rise to the labyrinthine, recurrent perforating, and subarcuate arteries (9). As the a1 segment is deep, and the a4 segment has tiny vessels, a2 and a3 segments can make full use of the space in the CPA region, and the vessels are usually curled and of moderate diameter. They are often used as ideal bypass vessels (9, 11).
When the aneurysm is located in the anterior or internal segment of the IAC, namely segment a1 or a2, interventional embolization is the primary choice of treatment due to the difficulty of anatomical exposure. However, in the case of the tiny AICA, it is difficult to completely ensure the patency of the parent artery during interventional embolization of a complex wide-necked aneurysm, and some patients need to occlude the parent artery (5, 12). Due to the existence of potential perforating arteries, occluding the AICA may lead to facial paralysis, dysphagia, water choking, occipital lobe infarction, binocular hemianopia, etc. (2).
When the aneurysm is located in the posterior segments of IAC, namely segment a3 or a4, application of a retrosigmoid sinus approach can obtain effective surgical anatomy of the exposure; previous literature has reported that the clipping effect is good (1, 4, 13). However, there are also some cases due to the aneurysm shape being broad neck or fusiform, which are difficult to clip. Once the parent artery is narrowed or the aneurysm has a residual neck after clipping, it leads to an increased risk of rebleeding, and these cases can only choose the aneurysm isolation technique. However, when the ipsilateral PICA and SCA is hypoplasia or tiny, when AICA is the mutation of PICA, or when you cannot be sure that variations in the course of the internal auditory artery (IAA) arise from the distal AICA, pure isolated aneurysm or occlusion of the anterior artery can produce a wide range of cerebral infarction and severe neurological dysfunction.
Therefore, for these complex AICAs, the application of the bypass vessel reconstruction technique is an effective strategy to preserve the distal vessel patency and avoid cerebral infarction. This paper reviews and summarizes previous literature reports on vascular reconstruction for complex AICA aneurysms, and most of them achieve good efficacy as shown in Table 1. Pasler et al. (16) and Baranoski et al. (9), respectively, report one case of complex AICA resection by the retrosigmoid sinus approach, followed by end-to-end anastomosis of AICA in situ, which effectively avoided postoperative cerebral infarction. Baranoski et al. (9) and Lee et al. (11) also, respectively, report that the p3 segment of PICA was anastomotic with the a3 segment of AICA to isolate proximal aneurysms of AICA and effectively avoid cerebral infarction. No matter which type of vascular reconstruction, this requires the surgeon to be proficient in deep vascular anastomosis. Comparatively, on the one hand, the distal anastomosis between the OA and AICA is superficial but usually requires the application of an incision flap similar to the distal lateral approach. Besides this, there is a risk that the diameter and wall of bypass vessels will not match very well, which affects the anastomosis effect. On the other hand, the anastomosis of PICA-AICA must first be anatomically similar to the branch vessels, and the additional intraoperative risk of blocking PICA may lead to more extensive cerebral infarction after surgery. Compared with the above two vascular reconstruction techniques, end-to-end anastomosis of AICA in situ for craniotomy using a retrosigmoid sinus approach can achieve good matching of vascular diameter and wall of bypass vessels, recovery of original hemodynamics, closer to natural anatomy, and high expected patency rate.
In this case, preoperative angiography suggested that the right PICA was absent, and the blood supply range of the right AICA was extensive. If aneurysm isolation was performed alone, the risk of postoperative cerebellar and brainstem infarction was high. Therefore, the aneurysm was treated by excision of the aneurysm and anastomosis in situ of AICA. Intraoperative fluorescence angiography and Doppler imaging confirmed that the vessel patency. Postoperative angiography also indicated that anastomosis patency, and the blood supply range of the anterior cerebellar artery was the same as before. There are few reports on the application of vascular reconstruction in the treatment of AICA aneurysms. This case can provide a reference for the surgical treatment of complex AICA aneurysms.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
CH and WH: conceptualization and study design. CH and SQ: data collection, literature research, and manuscript drafting. WH and YY: revision. CH: funding. All authors contributed to the article and approved the submitted version.
This work was supported by Guangxi Medical and Health Key Scientific Research Project (No. Z20190610).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
CT, computed tomography; DSA, digital subtraction angiography; MRI, Magnetic resonance imaging; AICA: Anterior Inferior Cerebellar Artery; IAC: internal auditory canal; PICA: posterior inferior cerebellar artery; SCA: superior cerebellar artery; IAA: internal auditory artery; OA: occipital artery.
1. Li X, Zhang D, Zhao J. Anterior inferior cerebellar artery aneurysms: six cases and a review of the literature. Neurosurg Rev. (2012) 35:111–9. doi: 10.1007/s10143-011-0338-1
2. Kai-ming G, Xiao-guang T. Surgical treatment for ruptured anterior inferior cerebellar artery aneurysms. Chin J Contemp Neurol Neurosurg. (2013) 13:201–10. doi: 10.3969/j.issn.1672-6731.2013.03.009
3. Anil G, Sein L, Nga V, Teo K, Chou N, Yeo TT. Dissecting distal cerebellar artery aneurysms: options beyond a parent vessel sacrifice. Neurosurg Rev. (2019) 43:771–80. doi: 10.1007/s10143-019-01119-y
4. Xin C, Hao W, Peng-Jun J, Yu-Ming J, Yong C, You-Xiang L, et al. Clinical analysis of 11 cases of anterior inferior cerebellar artery aneurysms. Chin J Stroke. (2020) 15:631–6. doi: 10.3969/j.issn.1673-5765.2020.06.011
5. Rodríguez-Hernández A, Zador Z, Rodríguez-Mena R, Lawton MT. Distal aneurysms of intracranial arteries: application of numerical nomenclature, predilection for cerebellar arteries, and results of surgical management. World Neurosurgery. (2013) 80:103–12. doi: 10.1016/j.wneu.2012.09.010
6. Tokimura H, Ishigami T, Yamahata H, Yonezawa H, Yokoyama S, Haruzono A, et al. Clinical presentation and treatment of distal anterior inferior cerebellar artery aneurysms. Neurosurg Rev. (2012) 35:497–503. doi: 10.1007/s10143-012-0390-5
7. Lv X, Ge H, He H, Jiang C, Li Y. Anterior inferior cerebellar artery aneurysms: segments and results of surgical and endovascular managements. Interv Neuroradiol. (2016) 22:643–8. doi: 10.1177/1591019916656474
8. Khayat HA, Alshareef F, Alshamy A, Algain A, Alhejaili E, Alnabihi O, et al. Pure endovascular management of an arteriovenous malformation and an aneurysm both supplied by anterio-inferior cerebellar artery: a case report and a review of literature. Front Neurol. (2017) 8:382. doi: 10.3389/fneur.2017.00382
9. Baranoski JF, Przybylowski CJ, Mascitelli JR, Lang MJ, Lawton MT. anterior inferior cerebellar artery bypasses: the 7-bypass framework applied to ischemia and aneurysms in the cerebellopontine angle. Operat Neurosurg. (2020) 19:165–74. doi: 10.1093/ons/opz347
10. Rodríguez-Hernández A, Rhoton AL Jr, Lawton MT. Segmental anatomy of cerebellar arteries: a proposed nomenclature. laboratory investigation. J Neurosurg. (2011) 115:387–97. doi: 10.3171/2011.3.JNS101413
11. Lee BS, Witek AM, Moore NZ, Bain MD. Treatment of an anterior inferior cerebellar artery aneurysm with microsurgical trapping and in situ posterior inferior cerebellar artery to anterior inferior cerebellar artery bypass: case report. Operat Neurosurg. (2018) 15:418–24. doi: 10.1093/ons/opx275
12. Hou K, Li G, Xu B, Xu K, Yu J. Which patients with aneurysms involving the a1-a2 segment of the anterior inferior cerebellar artery would benefit from parent artery occlusion? World Neurosurgery. (2019) 126:301–9. doi: 10.1016/j.wneu.2019.03.070
13. Bambakidis NC, Manjila S, Dashti S, Tarr R, Megerian CA. Management of anterior inferior cerebellar artery aneurysms: an illustrative case and review of literature. Neurosurg Focus. (2009) 26:E6. doi: 10.3171/2009.1.FOCUS0915
14. Fukushima S, Hirohata M, Okamoto Y, Yamashita S, Ishida S, Shigemori M. Anterior inferior cerebellar artery dissecting aneurysm in a juvenile: case report. Neurol Med Chir. (2009) 49:81–4. doi: 10.2176/nmc.49.81
15. Oyama H, Kito A, Maki H, Hattori K, Tanahashi K. Compression of the medulla oblongata and acute respiratory failure caused by rupture of a thrombosed large aneurysm of the anterior inferior cerebellar artery. Neurol Med Chir. (2010) 50:571–3. doi: 10.2176/nmc.50.571
16. Päsler D, Baldauf J, Runge U, Schroeder HW. Intrameatal thrombosed anterior inferior cerebellar artery aneurysm mimicking a vestibular schwannoma. J Neurosurg. (2011) 114:1057–60. doi: 10.3171/2010.9.JNS10491
17. Fujimura M, Inoue T, Shimizu H, Tominaga T. Occipital artery-anterior inferior cerebellar artery bypass with microsurgical trapping for exclusively intra-meatal anterior inferior cerebellar artery aneurysm manifesting as subarachnoid hemorrhage. case report. Neurol Med Chir. (2012) 52:435–8. doi: 10.2176/nmc.52.435
18. Kanamori F, Kawabata T, Muraoka S, Kojima T, Watanabe T, Hatano N, et al. Ruptured partially thrombosed anterior inferior cerebellar artery aneurysms: two case reports and review of literature. Nagoya J Med Sci. (2016) 78:517–22. doi: 10.18999/nagjms.78.4.517
19. Umekawa M, Hasegawa H, Shin M, Kawashima M, Nomura S, Nakatomi H, et al. Radiosurgery-induced anterior inferior cerebellar artery pseudoaneurysm treated with trapping and bypass. World Neurosurg. (2018) 116:209–13. doi: 10.1016/j.wneu.2018.04.161
Keywords: aneurysms, complex aneurysms, anterior inferior cerebellar aneurysm, aneurysm resection, arterial anastomosis in situ
Citation: Huang C, Qin S, Huang W and Yu Y (2021) Anterior Inferior Cerebellar Aneurysm Treated by Aneurysm Resection and Intracranial Artery Anastomosis in situ: A Case Report and Literature Review. Front. Surg. 8:669433. doi: 10.3389/fsurg.2021.669433
Received: 18 February 2021; Accepted: 13 April 2021;
Published: 25 May 2021.
Edited by:
Michael Sughrue, University of New South Wales, AustraliaReviewed by:
Hiroki Toda, Kitano Hospital, JapanCopyright © 2021 Huang, Qin, Huang and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei Huang, MTM5NzcxNjY2MzZAMTI2LmNvbQ==; Chaojue Huang, MzEwMDQ2NTQyQHFxLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.