- 1Department of Urology, Shanghai General Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China
- 2Department of Urology, Tongren Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
Background: Until recently, most enucleation techniques of the prostate were performed with the application of morcellator. We introduce a modified enucleation technique of thulium laser with non-morcellator approach, which is about incising and vaporizing remaining prostate tissue instead of a morcellator.
Methods: A retrospective evaluation of 223 patients undergoing ThuLEP from January 2014 to December 2015 was performed in our institution. One hundred five of the patients used morcellator while the other 118 used non-morcellator approach. All patients were assessed with the International Prostate Symptom Score (IPSS), quality of life (Qol), ultrasonography, serum prostate-specific antigen (PSA), maximal urine flow rate (Qmax), and postvoid residual urine volume (PVR). We reassessed these parameters at 1-, 3-, 6-, and 12-months after operation. Operative time, perioperative, and postoperative complications were also recorded.
Results: Significant improvement was noted in the IPSS, QoL, Qmax, and PVR in both groups at the 12-month follow-up, and assessment showed no differences in these parameters between the two groups. Comparisons of the total operation time and enucleation time demonstrated no significant differences between the two groups. Our non-morcellator approach needed more time to incise and vaporize the enucleated tissue compared to morcellation when the prostate volume was about 40–80 ml (p < 0.05), while it showed a significant lower rate of superficial bladder injury than using morcellator (p < 0.05). There were no significant differences in other complications between the two groups (p > 0.05).
Conclusions: Our modified technique is a safe and effective procedure for the treatment of BPH avoiding the potential complications caused by morcellator.
Background
Transurethral resection of the prostate (TURP) is considered as the gold standards for the treatment of benign prostatic hyperplasia(BPH). However, TURP is still associated with significant morbidity including severe bleeding, capsular perforation, and transurethral resection syndrome(TURS) (1). Since the renaissance of laser prostatectomy with the advent of the holmium laser in the 1990s (2), various lasers and subsequent procedures have been introduced (3, 4). Among all kinds of laser-associated techniques, holmium laser transurethral enucleation of the prostate(HoLEP), and thulium laser enucleation of the prostate(ThuLEP) are becoming more and more popular and have been proven to be safe and effective (5–7). Morcellator is widely used in most reported enucleation techniques including HoLEP and ThuLEP. Although morcellation of intravesical adenoma is currently the standard procedure following transurethral enucleation procedures, it can be associated with several morbidities, including ureteral orifice, bladder mucosal injuries even bladder perforation (8, 9). In this study, we introduce a modified ThuLEP without the procedure of morcellation for the treatment of BPH, and make a comparison with ThuLEP with morcellation.
Methods
Subjects
From January 2014 to December 2016, a total of 223 symptomatic BPH patients who underwent ThuLEP in our institution were evaluated retrospectively. One hundred five of the patients used morcellator (Group 1) while the other 118 used the new non-morcellator approach (Group 2). Inclusion criteria were as follows: the prostate volume <80 ml, Qmax <15 ml/s, PVR ≥ 50 ml, repeated urinary retention(including patients with indwelling catheterization), medical therapy failure, and lower urinary tract symptoms with IPSS above 7. Patients diagnosed with neurogenic bladder, prostate cancer, or previous prostate surgery were excluded.
All surgeries were performed by two experienced surgeons who had performed over 300 ThuLEP procedures. Perioperative assessment included medical history, digital rectal examination (DRE), IPSS, ultrasonography, PSA, Qmax, QoL, PVR, operative time, catheterization day, resected tissue weight, hemoglobin decrease, hospital stay, and operation-related complications.
Instruments and Surgical Technique
The instruments used were a 120-W continuous-wave Tm:yttrium aluminum garnet laser (Raykeen), a 26 F continuous flow resectoscope (KARL STORZ) and a mechanical morcellator (Hawk). The laser was used at two different energy levels. The cutting setting was 120 W, and the enucleation setting was 50 W. Laser energy was applied through a reusable 550 lm laser fiber. Physiological saline irrigation was applied throughout the entire procedure.
The technique using morcellator for Group 1 has been previously described in detail (5). The surgical steps of our modified technique of ThuLEP for Group 2 are as follows.
• Making the incision line
An inverted-U-shaped incision around the verumontanum is made. The incision is continued until the surgical capsule is identified (Figure 1A). The laser fiber is then drawn back into the channel of the modified working channel.
• Enucleation
After inspection of the urethral sphincter, the enucleation process goes on along the obtained circumferential surgical capsule from 5 o'clock, the left apex of prostate with the beak of the resectoscope for blunt dissection, freeing the left lateral lobe from the surgical capsule. Then moving it from a counterclockwise fashion along the capsule up to 1 o'clock (Figure 1B), and the left lateral adenoma is gradually released from the capsule with long sweeps from the bladder neck to the apex. Haemostasis is achieved using 50 w laser beam throughout the enucleation as each bleeding vessel is encountered. The middle and the right lateral lobes are similarly enucleated along the capsule from 5 to 11 o'clock (Figures 1C,D). During blunt disconnection, visual control of the surgical capsule and laser coagulation of perforating vessels is necessary. Rather than releasing the lobes completely off the prostatic capsule, we keep the lobes attached to remaining tissue from 11 to 1 o'clock. The way to treat the apex of prostate is truncating the urethral muscosa along the surface of the enucleated lobe (Figure 1E).
• Incision and vaporization
Switching laser energy to 120 W for incision and vaporization, the lobes attached to the remaining tissue from 11 to 1 o'clock is resected into small pieces radially centered on urethra and released to the bladder (Figures 1F,G). Small residual fragments in the bladder are washed out with Ellik. At last, a three-way Foley catheter is placed into the bladder for continuous bladder irrigation with normal saline.
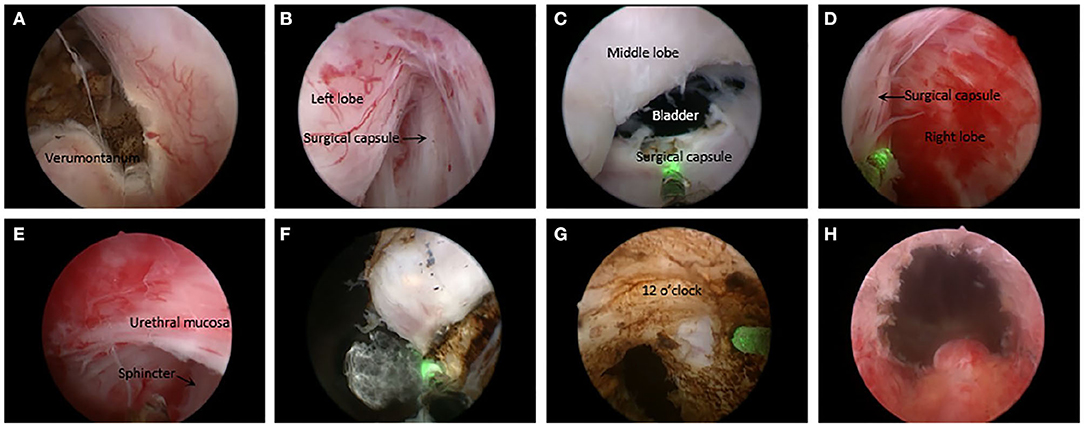
Figure 1. Overview of the non-morcellator technique. (A) Making an inverted-U shaped incision line. (B) Dissecting the left lobe from the obtained surgical capsule up to 1 o'clock with resectoscope. (C) Freeing the middle lobe from the surgical capsule toward the bladder neck. (D) Enucleating the right lobe similarly to 11 o'clock. (E) Truncating the urethral muscosa along the surface of the enucleated lobe at the apex of prostate. (F) Incising and vaporizing the lobes attached to the remaining tissue from 11 to 1 o'clock into small pieces. (G) Resecting the remaining tissue from 11 to 1 o'clock. (H) Postoperative effect.
Statistical Analysis
Normally distributed continuous variables were expressed as the mean ± standard deviation, and they were compared by t-tests. Non-normally distributed continuous variables are presented as the median and interquartile range, and they were analyzed with the Wilcoxon rank-sum test. Categorical data were compared by the χ2 test or Fisher's exact test. SPSS 16 software was used for the statistical analysis. A p < 0.05 was considered statistically significant.
Results
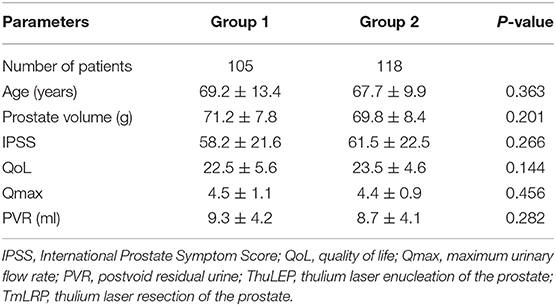
Table 1 compares the baseline parameters and primary perioperative outcomes between the 2 groups. There were no significant differences with regard to patients age, prostate volume, IPSS, QoL, Qmax, or PVR (p > 0.05).
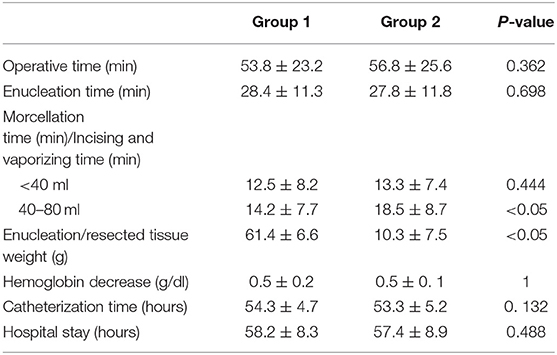
The perioperative data are shown in Table 2. Both procedures required a similar operative time, enucleation time, catheterization time, and length of hospitalization. Our non-morcellator approach needed more time to incise and vaporize the enucleated tissue compared to morcellation when the prostate volume was about 40–80 ml (p < 0.05), while there were no significant differences between the two groups when it comes to small prostates (<40 ml).
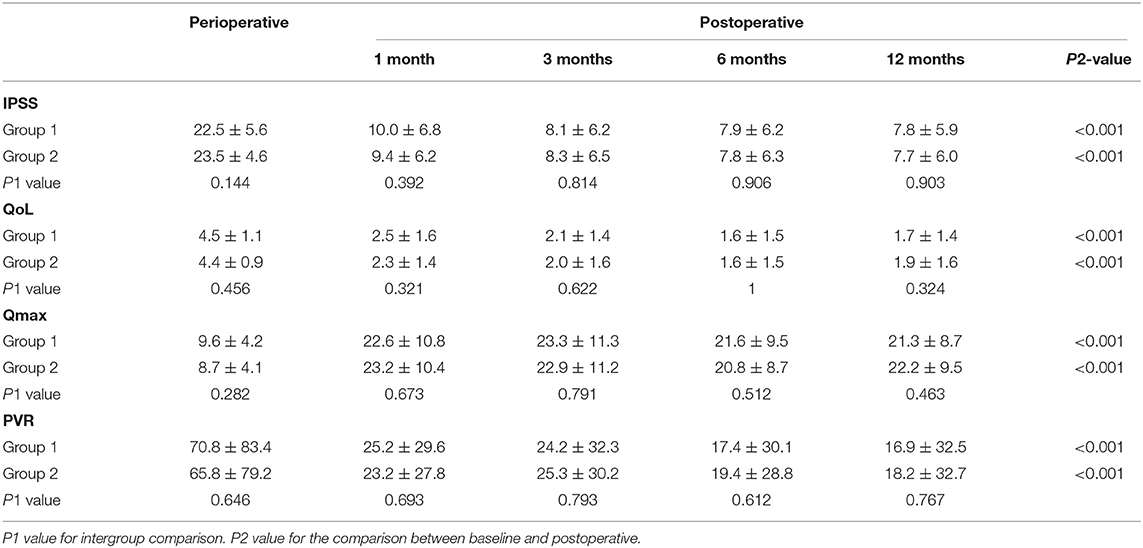
Table 3 lists the changes in IPSS, QoL, Qmax and PVR at 1, 3, 6, and 12 months. Significant improvements in all these parameters compared with the baseline values were observed at the 1-year follow-up. However, the differences between both groups were not significant.
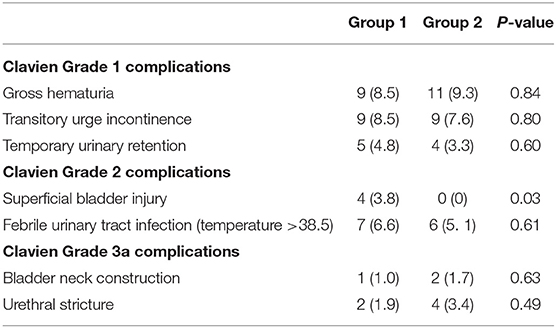
Perioperative complications are listed in Table 4. No cases required second TURP surgery or blood transfusion. There were also no cases of capsular perforation or ureteral orifice injury. Superficial bladder injury occurred in 4 patients in the Group 1, while no patient had this complication in the Group 2. Patients in the Group 1 (4.8%) showed a higher rate than those in the Group 2 (0%), and the difference was significant (p < 0.05). Both two groups had 9 patients with urgency urinary incontinence after operation, respectively, but no patients developed urinary incontinence that was persistent for more than 3 months. The incidences of gross haematuria and febrile UTI were not different between the two groups, and they usually resolved with bladder irrigation and antibiotic therapy. The occurrence of Urethral stricture and bladder neck contracture was similar between the two groups, and they were controlled by outpatient urethral dilation. Figure 2 list the changes in IPSS, QoL scores, Qmax and PVR at 1, 3, 6 and 12 months. Significant improvements in all these parameters compared with the baseline values were observed at the 1-year follow-up.
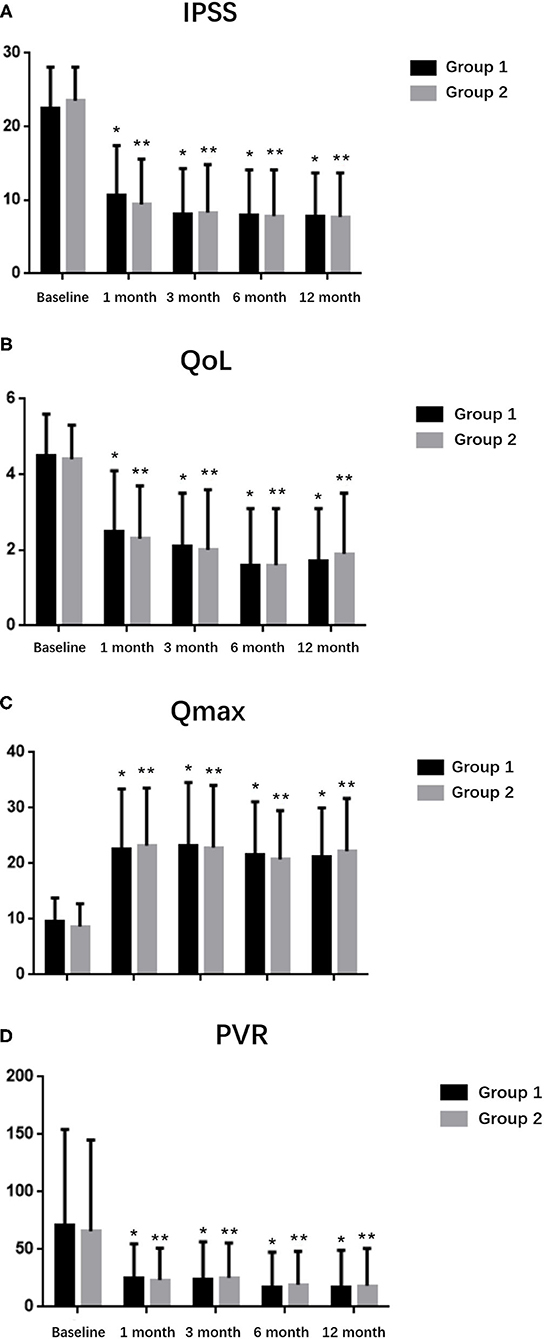
Figure 2. Follow-up data for up to 12 months in the two groups. (A) IPSS, (B) QoL, (C) Qmax, and (D) PVR. *P < 0.05 and **P < 0.05 compared with baseline values.
Discussion
Laser treatment of BPH through enucleation techniques has become increasingly utilized in the field of urology (10). Similar to open prostatectomy, enucleation of the adenoma carry the advantage of doing an anatomical based deobstruction (11), which may ensure excellent and long-term functional results and low recurrence rate. Multiple competing techniques using different energy sources to accomplish the enucleation procedure have been described, and ThuLEP has been proven to be safe, effective and comparable to HoLEP (11, 12). However, most relevant studies were related with the morcellation procedure, which we believed had some limitations.
Surgeons once used the mushroom method to remove glands after enucleation was performed, which need to substitute electrocautery device during the surgery and it was a very time-consuming process (13). Now with the development of the morcellator (14, 15), surgery for patients with large-sized BPH can be possible (16). However, the smooth surface of the gland and the great mobility of the enucleated pieces made it difficult to catch the targeted pieces. The firmness of the tissue and the dull blades sometimes greatly lowered the suctioning efficiency (17). All these reasons can result in several morbidities, including bladder neck false passage as well as ureteral orifice and bladder mucosal injuries (8, 9, 18). Besides, some researches reported that during the morcellation the bladder is distended to greater than maximal bladder capacity and is likely to result in postoperative voiding difficulties (19).
Thulium laser provides smooth incision and excellent hemostasis with minimal mechanical injury to the pericapsular tissue (20). Given these characteristics, we developed a modified enucleation technique with the use of the Thulium laser instead of morcellator. After the initial attempt, we found the technique was feasible and safe. So we collected the 2-year follow-up information to prove it.
Both groups used the enucleation technique, but the treatment of the enucleated tissue was different. We replaced the morcellation procedure with incision and vaporization of thulium laser. Postoperative functional results showed that PVR, QoL, and IPSS dropped immediately while Qmax increased at first month and this trend continued in the 12 months follow-up period, which confirmed effective anatomic desobstruction and significant relief of symptoms (21).
Compared with Group 1, the operative time in Group 2 was relatively longer, especially when the prostate volume is over 40 ml. That was because the incising and vaporizing time will be prolonged with the increase of prostate volume accordingly. But our data showed the incising and vaporizing time can be similar with morcellation time in condition of small prostate volumes(<40 ml). The catheter inside the urinary bladder depends on postoperative bleeding intensity. The hospital stay and catheterization time were similar with each other, which may be relevant with our careful hemostasis during the surgery. The resected tissue in Group 2 was much smaller than actual resected weight because most tissues were vaporized during the incision procedure.
The incidence of superficial bladder injury was the only postoperative complication that was significantly different in the two groups(p < 0.05). For these patients, we need immediate laser hemostasis, prolonged indwelling catheter time, and close observation of urine color and hemoglobin changes. The morcellation procedure has a risk of injury to the bladder mucosa when the bladder is unfilled, sometimes misoperation can also lead to this complication. Relatively, incising and vaporizing the enucleated lobes attached to the remaining tissue from to 1 o'clock is safer than morcellation. Our non-morcellator approach can completely avoid bladder injury.
Our series showed a low incidence of perioperative complications in 223 patients with ThuLEP, which is comparable with other minimally invasive procedures such as HoLEP (6, 22, 23). The mean hemoglobin decrease was 0.5 g/dl and no cases need blood transfusion. No cases of death or secondary surgery also highlight the safety of our methods. Gross hematuria occurs in 9 and 11 cases, respectively, and was resolved spontaneously or with conservative treatment including antibiotic therapy. The incidence of urinary incontinence, including urgency and stress, was up to 8.5 and 7.6%, respectively, when just removing of catheter, which we believed originated from transient urethral dilatation of the apex of the prostate structure. The rate reduced to 2.9 and 2.5% at 1 month and to 0 at 6 month. As reported by Fong et al., avoiding to incising the sphincter base in the anterior area of the prostate during the operation can account for the phenomenon (24).
Several studies indicated a lower incidence of urethral stricture following HoLEP and ThuLEP (25, 26), In our series, the risk of urethral stricture was similar. There were total 6 cases of urethral stricture at first month and 2 cases at third month, we believe it was temporarily associated with urethral edema caused by postoperative inflammation. Only one patient in Group 2 still needed urethra expansion at the twelfth month for urethral stricture that might be related with the patient himself.
Without the morcellation procedure, we avoided the potential occurrence of the superficial bladder mucosal injury and injury to the ureteric orifice.
Some studies reported that plasmakinetic enucleation of the prostate didn't have to use morcellator or change device during the surgery either (27). However, unlike thulium laser incising and vaporizing the tissue accurately by laser fiber, plasmakinetic bipolar resection performed the same procedure with resection loop, which caused smooth wound plane rather than an exact point. When it comes to the apex of prostate, a position needed to be dealt with very carefully in case of urinary incontinence, the thulium laser is supposed to be superior to plasmakinetic bipolar resection, but it need further prospective study.
However, this modified technique had a limitation in that the operation time took longer as the prostate size increased, for the attached tissue is not fixed and may swing to the opposite direction against the fiber. From our experience, if the size of the prostate is too large, the incising and vaporizing procedure can be hard and time-consuming. Thus, it is more suitable for a relatively small prostate. Also, because the data were collected retrospectively, this study could have had a selection bias. However, the results of our study can still be meaningful because of the similar preoperative factors between the groups. Besides, the steep learning curve is a hurdle to overcome for urologists. Finding correct surgical capsule and incising the “half-floating” attached lobes can be difficult and the procedure is better committed to experienced surgeons.
Conclusions
We introduce a modified technique of ThuLEP without using morcellator. Our initial results prove it was feasible and relatively safe and not inferior to other technique. Further follow-up is needed to prove its long-term durability.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by the institutional review board of Shanghai First People's Hospital. The registration number of the trial is ChiCTR1900021072 and the ethical approval number is [2018]61. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
YJ and QS were responsible for project development, data analysis, data management, and manuscript writing/editing. YJ and BH performed the procedures. YZhu, DZ, DC, XW, YR, and YZha conducted the data collection. WG and FZ performed the data analysis. BH and SX designed the study. All authors read and approved the final manuscript.
Funding
This work was supported by grants from the National Nature Science Foundation of China. (No. 81570682). The funding body covered the costs of English proofreading and the statistical analysis. The funders had no role in study design, study completion, data analysis, and writing of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors appreciate all our participants for their gracious contribution in this study.
Abbreviations
IPSS, International Prostate Symptom Score; QoL, Quality of life; PSA, Prostate-specific antigen; Qmax, maximal urine flow rate; PVR, Postvoid residual urine volume; TURP, Transurethral resection of the prostate; BPH, Benign prostatic hyperplasia; TURS, Transurethral resection syndrome; HoLEP, Holmium laser transurethral enucleation of the prostate; ThuLEP, Thulium laser enucleation of the prostate; DRE, Digital rectal examination.
References
1. Rassweiler J, Teber D, Kuntz R, Hofmann R. Complications of transurethral resection of the prostate (TURP)–incidence, management, and prevention. Eur Urol. (2006) 50:969–79. doi: 10.1016/j.eururo.2005.12.042
2. Gilling PJ, Cass CB, Malcolm AR, Fraundorfer MR. Combination holmium and Nd: YAG laser ablation of the prostate: initial clinical experience. J Endourol. (1995) 9:151–3. doi: 10.1089/end.1995.9.151
3. Gravas S, Bachmann A, Reich O, Roehrborn CG, Gilling PJ, De La Rosette J. Critical review of lasers in benign prostatic hyperplasia (BPH). BJU Int. (2011) 107:1030–43. doi: 10.1111/j.1464-410X.2010.09954.x
4. Schroeck FR, Hollingsworth JM, Kaufman SR, Hollenbeck BK, Wei JT. Population based trends in the surgical treatment of benign prostatic hyperplasia. J Urol. (2012) 188:1837–41. doi: 10.1016/j.juro.2012.07.049
5. Gilling PJ, Wilson LC, King CJ, Westenberg AM, Frampton CM, Fraundorfer MR. Long-term results of a randomized trial comparing holmium laser enucleation of the prostate and transurethral resection of the prostate: results at 7 years. BJU Int. (2012) 109:408–11. doi: 10.1111/j.1464-410X.2011.10359.x
6. Zhang F, Shao Q, Herrmann TR, Tian Y, Zhang Y. Thulium laser versus holmium laser transurethral enucleation of the prostate: 18-month follow-up data of a single center. Urology. (2012) 79:869–74. doi: 10.1016/j.urology.2011.12.018
7. Herrmann TR, Liatsikos EN, Nagele U, Traxer O, Merseburger AS. EAU guidelines panel on lasers, technologies. Eur Urol. (2012) 61:783–95. doi: 10.1016/j.eururo.2012.01.010
8. Lee SH, Choi JI, Moon KY, Na W, Lee JB. Holmium laser enucleation of the prostate: modified morcellation technique and results. Korean J Urol. (2012) 53:779–84. doi: 10.4111/kju.2012.53.11.779
9. Elshal AM, Mekkawy R, Laymon M, El-Assmy A, El-Nahas AR. Towards optimizing prostate tissue retrieval following holmium laser enucleation of the prostate (HoLEP): assessment of two morcellators and review of literature. Can Urol Assoc J. (2015) 9:E618–25. doi: 10.5489/cuaj.3035
10. Gilling PJ. Laser enucleation is increasingly becoming the standard of care for treatment of benign prostatic hyperplasia of all sizes. Eur Urol. (2013) 63:868–9; discussion 870-1. doi: 10.1016/j.eururo.2013.01.001
11. Herrmann TR, Bach T, Imkamp F, Georgiou A, Burchardi M, Oelke M, et al. Thulium laser enucleation of the prostate (ThuLEP): transurethral anatomical prostatectomy with laser support. introduction of a novel technique for the treatment of benign prostatic obstruction. World J Urol. (2010) 28:45–51. doi: 10.1007/s00345-009-0503-0
12. Gomez Sancha F, Rivera VC, Georgiev G, Botsevski A, Kotsev J, Herrmann T. Common trend: move to enucleation:Is there a case for GreenLight enucleation? Development and description of the technique. World J Urol. (2015) 33:539–47. doi: 10.1007/s00345-014-1339-9
13. Hochreiter WW, Thalmann GN, Burkhard FC, Studer UE. Holmium laser enucleation of the prostate combined with electrocautery resection: the mushroom technique. J Urol. (2002) 168:1470–4. doi: 10.1097/00005392-200210010-00040
14. Fraundorfer MR, Gilling PJ. Holmium:YAG laser enucleation of the prostate combined with mechanical morcellation: preliminary results. Eur Urol. (1998) 33:69–72. doi: 10.1159/000019535
15. Gilling PJ, Kennett K, Das AK, Thompson D, Fraundorfer MR. Holmium laser enucleation of the prostate (HoLEP) combined with transurethral tissue morcellation: an update on the early clinical experience. J Endourol. (1998) 12:457–9. doi: 10.1089/end.1998.12.457
16. Elmansy H, Baazeem A, Kotb A, Badawy H, Riad E, Emran A, et al. Holmium laser enucleation versus photoselective vaporization for prostatic adenoma greater than 60 ml: preliminary results of a prospective, randomized clinical trial. J Urol. (2012) 188:216–21. doi: 10.1016/j.juro.2012.02.2576
17. Chen Q, Chen Y-B, Wang Z, Peng Y-B, Zheng D-C, Cai Z-K, et al. An improved morcellation procedure for holmium laser enucleation of the prostate. J Endourol. (2012) 26:1625–8. doi: 10.1089/end.2012.0265
18. Kuo RL, Paterson RF, Siqueira TM Jr, Watkins SL, Simmons GR, Steele RE, et al. Holmium laser enucleation of the prostate: morbidity in a series of 206 patients. Urology. (2003) 62:59–63. doi: 10.1016/S0090-4295(03)00124-9
19. Kim SH, Yoo C, Choo M, Paick JS, Oh SJ. Factors affecting de novo urinary retention after holmium laser enucleation of the prostate. PLoS ONE. (2014) 9:e84938. doi: 10.1371/journal.pone.0084938
20. Xia S-J, Zhuo J, Sun X-W, Han B-M, Shao Y, Zhang Y-N. Thulium laser versus standard transurethral resection of the prostate: a randomized prospective trial. Eur Urol. (2008) 53:382–90. doi: 10.1016/j.eururo.2007.05.019
21. Gratzke C, Bachmann A, Descazeaud A, Drake MJ, Madersbacher S, Mamoulakis C, et al. EAU guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. (2015) 67:1099–109. doi: 10.1016/j.eururo.2014.12.038
22. Gross AJ, Netsch C, Knipper S, Hölzel J, Bach T. Complications and early postoperative outcome in 1080 patients after thulium vapoenucleation of the prostate: results at a single institution. Eur Urol. (2013) 63:859–67. doi: 10.1016/j.eururo.2012.11.048
23. Vavassori I, Valenti S, Naspro R, Vismara A, Dell'Acqua V, Manzetti A, et al. Three-year outcome following holmium laser enucleation of the prostate combined with mechanical morcellation in 330 consecutive patients. Eur Urol. (2008) 53:599–604. doi: 10.1016/j.eururo.2007.10.059
24. Fong BC, Elhilali MM. Holmium: YAG laser enucleation of the prostate: multimedia description from a trainee's perspective. J Endourol. (2004) 18:791–4. doi: 10.1089/end.2004.18.791
25. Wilson LC, Gilling PJ, Williams A, Kennett KM, Frampton CM, Westenberg AM, et al. A randomised trial comparing holmium laser enucleation versus transurethral resection in the treatment of prostates larger than 40 grams: results at 2 years. Eur Urol. (2006) 50:569–73 doi: 10.1016/j.eururo.2006.04.002
26. Yeon JK, Yoon HL, Joon BK, Cho SR, Kim JS. A novel one lobe technique of thulium laser enucleation of the prostate: ‘All-in-One' technique. Korean J Urol. (2015) 56:769–74. doi: 10.4111/kju.2015.56.11.769
Keywords: benign prostatic hyperplasia, enucleation, morcellator, thulium laser, modified technique
Citation: Jing Y, Sun Q, Guo W, Zhou D, Zhu Y, Zhao Y, Cui D, Wang X, Ruan Y, Zhao F, Xia S and Han B (2021) A Modified Technique of Thulium Laser Enucleation for Benign Prostatic Hyperplasia With Non-morcellator Approach. Front. Surg. 8:657869. doi: 10.3389/fsurg.2021.657869
Received: 24 January 2021; Accepted: 06 April 2021;
Published: 07 May 2021.
Edited by:
Hai-Hong Jiang, First Affiliated Hospital of Wenzhou Medical University, ChinaReviewed by:
Daniele Castellani, Polytechnic University of Le Marche, ItalyZhangqun Ye, Huazhong University of Science and Technology, China
Copyright © 2021 Jing, Sun, Guo, Zhou, Zhu, Zhao, Cui, Wang, Ruan, Zhao, Xia and Han. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shujie Xia, eHNqdXJvbG9naXN0QDE2My5jb20=; Bangmin Han, aGFuYm1AMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Yifeng Jing
Yifeng Jing Qian Sun2†
Qian Sun2†