
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Surg. , 01 March 2021
Sec. Thoracic Surgery
Volume 8 - 2021 | https://doi.org/10.3389/fsurg.2021.648759
This article is part of the Research Topic Surgery and COVID-19: Which Strategies to Apply in Oncologic Patients View all 6 articles
 Alessandro Baisi1*
Alessandro Baisi1* Alessandra Mazzucco1
Alessandra Mazzucco1 Giovanni Caffarena1
Giovanni Caffarena1 Gerardo Cioffi2
Gerardo Cioffi2 Angelo Guttadauro3*
Angelo Guttadauro3* Ugo Cioffi4
Ugo Cioffi4Background: SARS-CoV-2 is a new disease with some manifestations not yet well-known. Sharing experiences in this topic is crucial for the optimal management of the patients.
Case Presentation: Left upper extremity deep vein thrombosis (UEDVT) due to a mediastinal mass strongly suspected of lymphoproliferative disease in a patient affected by SARS-CoV-2, disappearing at the resolution of the viral infection.
Conclusion: Before proceeding to surgical biopsy, mediastinal mass in SARS-CoV-2 patients must be revaluated after the resolution of the infection.
In order to contribute positively to the development of a precise decision-making process, sharing the experiences and perspectives is crucial. We report the case of a positive SARS-CoV-2 female patient candidate to surgical biopsy of a Positron Emission Tomography (PET-TC) positive mediastinal mass which, following the resolution of the viral infection, underwent a complete regression.
A 50-year-old woman, former smoker with a negative medical history, went to the emergency room in March 2020 for pain in the neck and left arm. No dyspnea or cough were reported. At clinical examination the upper left arm and the neck showed swelling edema and redness. Blood tests showed leukocytosis, C-reactive Protein and D-dimer elevated. SARS-CoV-2 and H1N1 nasal swabs were negative. An eco-color-doppler showed left upper extremity deep vein thrombosis (UEDVT). The anatomical extension of the thrombosis was up to the left axillary vein, left subclavian vein, left jugular vein. The patient was therefore treated with Low Molecular Weight Heparin (Enoxaparin) 8000 IU BID. The UEDVT was due to a mass in the upper anterior mediastinum compressing and displacing the left anonymous vein evident at a contrast medium Chest Computed Tomography (CT) (Figure 1). Pulmonary Embolisms (PE) of the Right Lower Lobe (RLL) and Left Upper Lobe (LUL) were also present. At a PET-CT (Figure 2) an intense uptake of the mediastinal mass was evident suggesting a lymphoproliferative disease or lymph nodes' metastasis. An ultrasound-guided left supraclavicular lymph node biopsy was performed with negative culture and histological results. A surgical mediastinal mass biopsy by VATS was therefore planned, but a new SARS-CoV-2 nasal swab was positive. This, together to the pulmonary embolism, prompted us to delay the procedure. The patient was relocated in a dedicated SARS-CoV-2 department where she was treated with azithromycin and hydroxychloroquine for 10 days and long-term anticoagulation therapy. The patient was discharged in home isolation protocol 24 days after access (11 from positivity). After the execution of 2 negative SARS-CoV-2 control nasal swabs, respectively, 15 and 20 days after discharge, the patient was revaluated for the surgical procedure. Because the previous PET-CT dated back a couple of months before it was repeated. A complete regression of the mediastinal lesion was evident, confirmed also by a contrast medium CT, that showed also a resolution of the UEDVT.
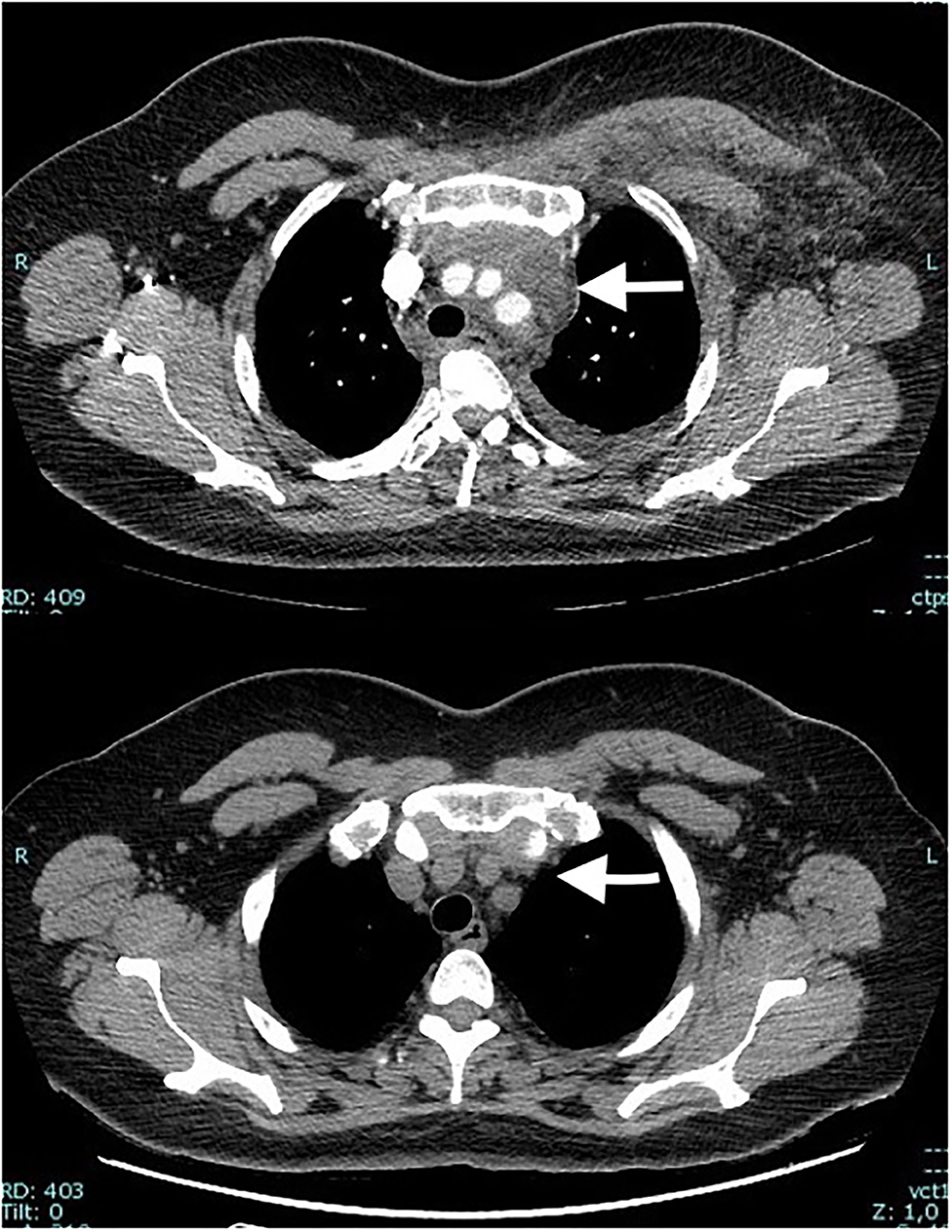
Figure 1. Contrast medium Chest Computed Tomography showing a mass of the upper anterior mediastinum compressing and displacing the left anonymous vein that is occluded (above) (white arrow). After 6 weeks, after the resolution of the SARS-CoV-2 the mass disappeared (white arrow).
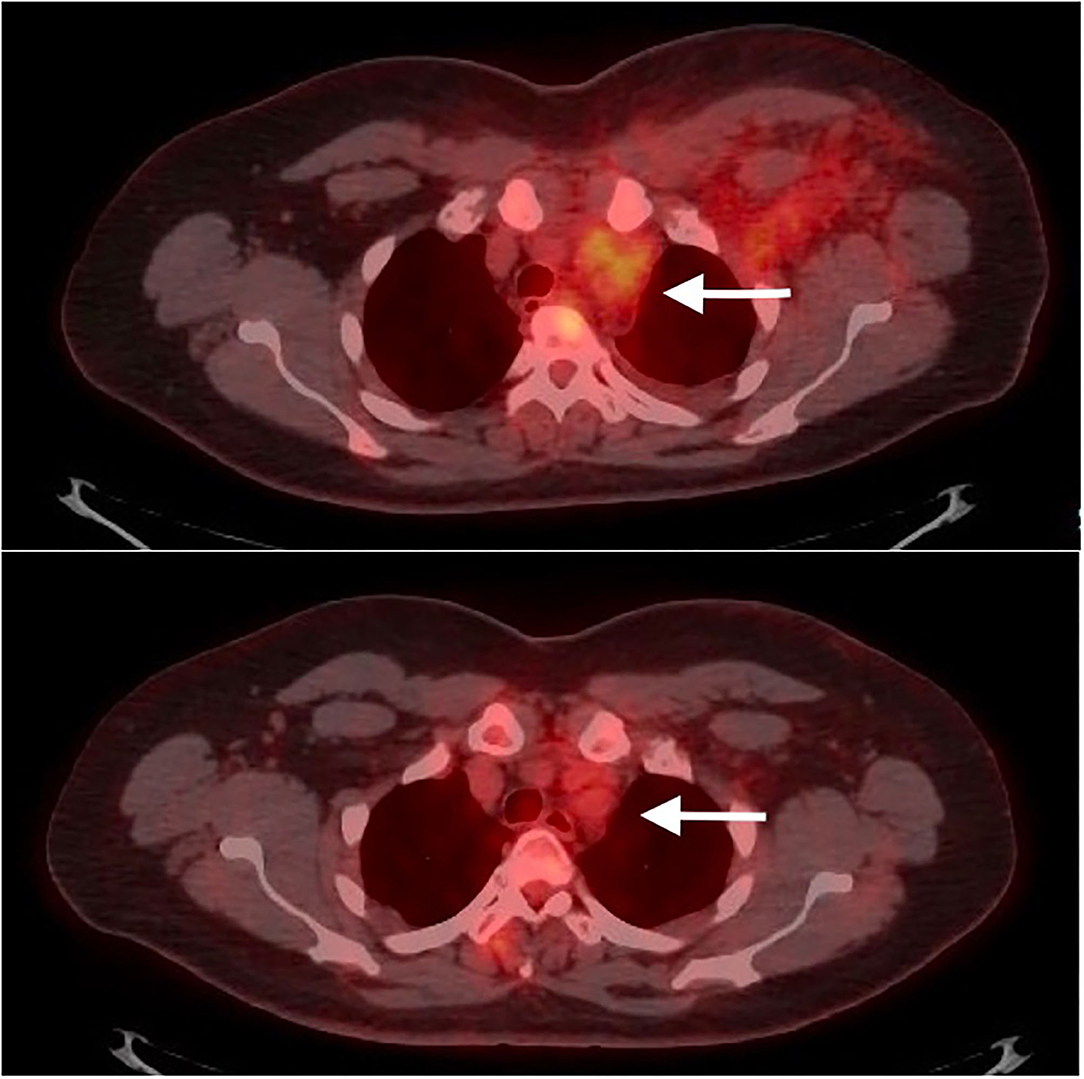
Figure 2. The mediastinal positive PET-CT scan mediastinal mass (above) disappeared after 46 days (below), at the resolution of the SARS-CoV-2.
According to a WHO report on SARS-CoV-2, the disease has no specific manifestation, and the presentation can range from completely asymptomatic to severe pneumonia and death (1). In our patient, the presenting symptom of the SARS-CoV-2 was a UEDVT due to a mass in the anterior mediastinum compressing and displacing the left anonymous vein. There was also some pulmonary embolism due to the well-known thrombotic complication of the disease (2, 3). Interestingly, the mediastinal mass, that was initially strongly suspected of lymphoproliferative disease, disappeared after 2 months with the resolution of the SARS-CoV-2 without any specific therapy. It must therefore be considered as enormous mediastinal confluent lymphadenopathy (4, 5).
Our experience suggests that in SARS-CoV-2 patients affected by mediastinal mass, the evaluation of the mass must be repeated after the resolution of the disease, before proceeding to surgical biopsy.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
All authors participated equally in the case and in the writing of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We thank GC, native speaker, for reviewing the English language.
1. WHO. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). WHO (2020). Available online at: http://who.int/docs/default-source/coronaviruse/who-china-joint-mission-oncovid-19-final-report.pdf
2. Lodigiania C, Iapichinoc G, Carenzo L, Cecconi M, Ferrazzi P, Sebastian T, et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. (2020) 191:9–14. doi: 10.1016/j.thromres.2020.04.024
3. The Lancet Haematology. COVID-19 coagulopathy: an evolving story. Lancet Haematol. (2020) 7:e425. doi: 10.1016/S2352-3026(20)30151-4
4. Valette X, du Cheyron D, Goursaud S. Mediastinal lymphadenopathy in patients with severe COVID-19. Lancet Infec Dis. (2020) 20:1230. doi: 10.1016/S1473-3099(20)30310-8
Keywords: SARS-CoV-2, mediastinal mass, viral infection, lymphoproliferative disease, biopsy
Citation: Baisi A, Mazzucco A, Caffarena G, Cioffi G, Guttadauro A and Cioffi U (2021) Case Report: Mediastinal Mass in SARS-COV-2 Pandemic: A Word of Caution. Front. Surg. 8:648759. doi: 10.3389/fsurg.2021.648759
Received: 01 January 2021; Accepted: 09 February 2021;
Published: 01 March 2021.
Edited by:
Christopher William Seder, Rush University Medical Center, United StatesReviewed by:
Benilde Cosmi, University of Bologna, ItalyCopyright © 2021 Baisi, Mazzucco, Caffarena, Cioffi, Guttadauro and Cioffi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Angelo Guttadauro, YW5nZWxvLmd1dHRhZGF1cm9AdW5pbWliLml0; Alessandro Baisi, YWxlc3NhbmRyby5iYWlzaUB1bmltaS5pdA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.