- 1Shiraz Nephrology-Urology Research Center, Shiraz University of Medical Sciences, Shiraz, Iran
- 2Department of Urology, Shaheed Faghihi Hospital, Shiraz University of Medical Sciences, Shiraz, Iran
- 3Shiraz Geriatric Research Center, Shiraz University of Medical Sciences, Shiraz, Iran
- 4Student Research Committee, Shiraz University of Medical Sciences, Shiraz, Iran
- 5Department of Urology, Urology Research Center, Al-Thora General Hospital, Ibb University of Medical Since, Ibb, Yemen
Purpose: Renal calculi are becoming more common among children. Although, extracorporeal shock wave lithotripsy (ESWL) is the first choice in this age group, minimal invasive surgeries, such as percutaneous nephrolithotomy (PCNL), are indicated for some patients. Recently, PCNL devices have become smaller in size with acceptable efficacy and lower complications. We evaluated the outcomes and complications of mini-PCNL (MPCNL) surgery in our referral training centers.
Materials and Methods: Between September 2012 and January 2020, a total of 112 children under the age of 18, who had shown failure of ESWL, and/or their parents refused to do it, underwent MPCNL (15 Fr). The patients' profiles were reviewed for data collection including preoperative and stone data, operation information, and postoperative complications.
Results: Of 112 patients, 69 were boys, and 43 were girls. Their mean age was 8.6 years (14 months to 18 years). Mean stone size was 20 mm (14–34 mm). Seventy-four cases had renal pelvic stone, 22 had pelvis and lower pole, and 16 had staghorn. The mean operation time was 65 min (35–100 min), and mean radiation time was 0.6 min (0.2–1.4 min). Low-grade fever was detected in 14 patients (12.5%). Four patients needed blood transfusion and two had increased creatinine, which improved with conservative management. One patient developed urosepsis that resolved with antibiotic therapy. None of the patients had kidney perforation or other organ injury or death. Early stone-free rate (SFR) after operation was 90.2% (101 patients). Six patients had residual fragment <5 mm, which passed spontaneously in 2 weeks after operation (total SFR 95.3%). Three patients underwent second-look nephroscopy, and ureteroscopy was done for two patients due to migrated stone fragments to the distal ureter.
Conclusion: MPCNL is recommended as a safe alternative option for treatment of the nephrolithiasis in children with good outcome and acceptable complications.
Introduction
Epidemiologic studies have demonstrated an increasing rate of pediatric urinary stone disease in the past decades (1–3). Although, pediatric urinary stone disease is less common in children than adults, it is more difficult to manage because of their urinary tract size and higher recurrence rate (4). The clinically insignificant stone fragments (<4–5 mm) that may be observed after treatment of adult stones can cause obstructive symptoms for pediatric patients and need for surgical intervention. However, spontaneous passage of a renal stone is more likely in children than in adults (5). Hence, the goals of surgical management of pediatric urinary stone disease include maximum stone clearance rate and less perioperative morbidity. The latest American Urological Association guidelines recommended percutaneous nephrolithotomy (PCNL) or extracorporeal shock wave lithotripsy (ESWL) for treatment of a pediatric renal stone exceeding 2 cm (6). However, ESWL has lost its popularity in treatment of large stones due to poor clearance rate (7, 8). Miniaturization of PCNL in recent years has diminished its perioperative comorbidities through decreasing the size of the access sheath tract (4, 9). Since there are few studies investigating this approach in the pediatric population, the aim of this study was to evaluate the postoperative outcomes of mini-PCNL (MPCNL) in terms of safety and efficacy in a single-referral center in Southern Iran.
Methods
Study Design
This study was approved by the ethics committees of Shiraz University of Medical Sciences (Approval code ofIR.sums.med.rec.1398.459) and performed in accordance with the Declaration of Helsinki. In this retrospective cross-sectional study, the pediatric patients who had undergone MPCNL between September 2012 and January 2020 in our referral centers (Nemazi Teaching Hospital and Ali-Asghar Teaching Hospital, Shiraz, Southern Iran) were considered for this study. During this period, 112 patients under age 18, who had failure of ESWL and/or their parents refused to do it, underwent MPCNL. Almost all patients were referred to our clinic by a pediatric nephrologist. They had preoperative evaluation of the urinary system including ultrasonography and plain abdominal and pelvic X-ray (KUB) or excretory urography for lucent stones and low-dose non-contrast CT scan with reconstruction limited to the kidneys (10). Also, complete blood count (CBC), renal function test (BUN and creatinine), and urine analysis and culture were done. Positive cultures were treated with appropriate antibiotic and admitted with sterile urine for operation. All patients were admitted 6 h before operation and received parenteral hydration and a single dose of prophylactic antibiotic.
Inclusion Criteria
The inclusion criteria were age under 18 years, normal renal function, renal stones more than 10 mm, and history of previous ESWL failure.
Exclusion Criteria
The exclusion criteria were patients with uncorrected coagulopathy, active urinary tract infection (UTI), patients who had undergone transplant or urinary diversion, and congenital abnormalities.
Operation
The procedure was done under general anesthesia. In lithotomy or supine with abducted thigh position, a ureteral catheter 3 Fr or 4 Fr was inserted into the kidney and fixed to the urethral Foley catheter. Then, the patient was switched into prone position. After proper padding of the chest, abdomen, knee, and ankle, the patient was draped with sterile coverage. Then, diluted contrast was injected through a ureteral catheter, and under fluoroscopic guidance (C-arm fluoroscopy image intensifier), the pelvicalyceal system (PCS) was visualized. In patients whose color Doppler US guide with a 3.5-MHz probe (BK Medical) was used for puncture, saline was injected for better visualization of the PCS. A Chiba needle 18G was inserted in the target calyx, and a 0.035-inch J-tip guide wire was passed through the needle into the PCS and ureter, if possible. Tract dilation was performed using Alken telescopic dilators up to 18 Fr and Amplatz sheath 18 Fr (11). Nephroscopy was done with 15 Fr (Wolf) nephroscope. Lithotripsy was done with pneumatic lithoclast, and its particles were removed by forceps. Warm saline solution was used as irrigation for prevention of possible hyponatremia and hypothermia. Stone-free status was checked at the end of operation by fluoroscopy and US. Tubeless MPCNL was used in the patients with single-tract access, no significant residual stones, no significant perforation, minimal bleeding, and no requirement for a secondary procedure (12). Ureteral stent and urethral Foley catheter were removed 12 to 24 h postoperatively. Nephrostomy tubes were removed on the second day after operation. A plain abdominal film (KUB X-ray) or US was done on the day after operation, and residual stones, if presented, were followed for spontaneous passage of <4–5 mm stones and possible second-look nephroscopy (second-look nephroscopy was done 24 h after MPCNL, which was performed percutaneously through the previously established tract in an attempt to render the patient stone free).
Data Collection
The patients' profiles were reviewed for data collection. Demographic data including age and sex were recorded. Preoperative information was previous history of stone or other surgery on the involved kidney, history of ESWL, solitary kidney, radiopacity of stone, hydronephrosis, stone laterality (left, right), stone location, and stone size. The mean stone size was assessed by preoperative low-dose non-enhanced computed tomography (CT) scan and determined by the largest diameter in the coronal view. Laboratory data consisted of blood urea nitrogen, creatinine, and hemoglobin that were measured before the surgery and 6 h after the operation. Operation and postoperative data included results and complications such as operation time, fluoroscopy screening time, stone-free status (KUB X-ray or ultrasound the day after the operation), hospitalization period, DJ insertion, ureteroscopy, redo-nephroscopy, fever, blood transfusion, infection, and other complications. Using the Modified Clavien grading system (13), postoperative complications were classified into fever as grade I, blood transfusion need, urine leakage, and urinary tract infection as grade II, double-J placement for urine leakage, ureteroscopy, and redo-PCNL as grade III, urosepsis and neighboring organ injury as grade IV, and death as grade V.
Statistical Analysis
Continuous variables were presented using mean and standard deviation. Categorical variables were presented using numbers and percentages. All statistical analyses were done using SPSS software (IBM SPSS, version 13).
Results
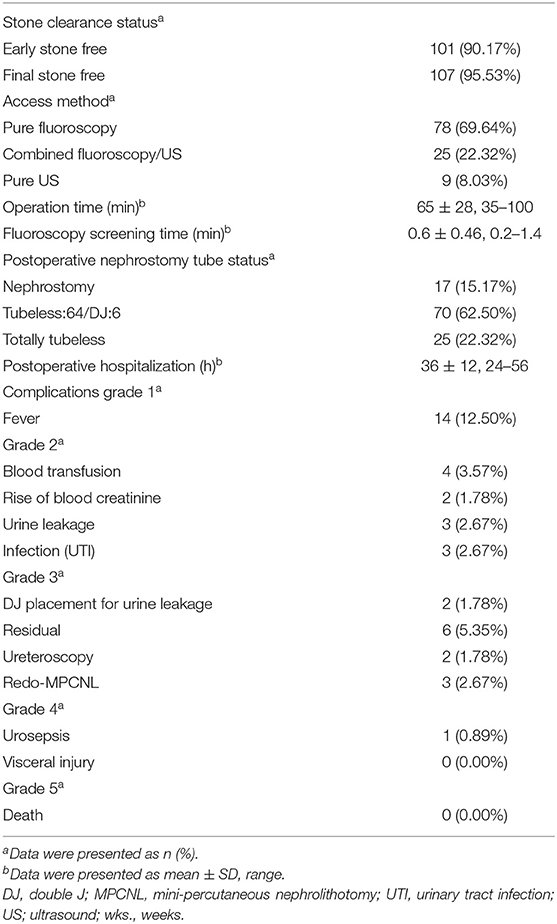
Of 112 patients, 69 were boys and 43 girls. Their mean age was 8.6 years (14 months to 18 years). Mean stone size was 20 mm (14–34 mm); 64 patients had left and 48 had right side stone. Seventy-four cases had renal pelvis stone, 22 had pelvis and lower pole, and 16 had staghorn. Thirty-six patients had a history of previous renal surgery (PCNL or open nephrolithotomy) on the same kidney, and 26 had a history of ESWL on the kidney. Ninety-eight had opaque, and the remaining 14 had lucent stone. Eight patients had solitary kidney. Seventy-seven of them had mild, 26 moderate, and 9 severe degrees of hydronephrosis on preoperative imaging studies (Table 1).
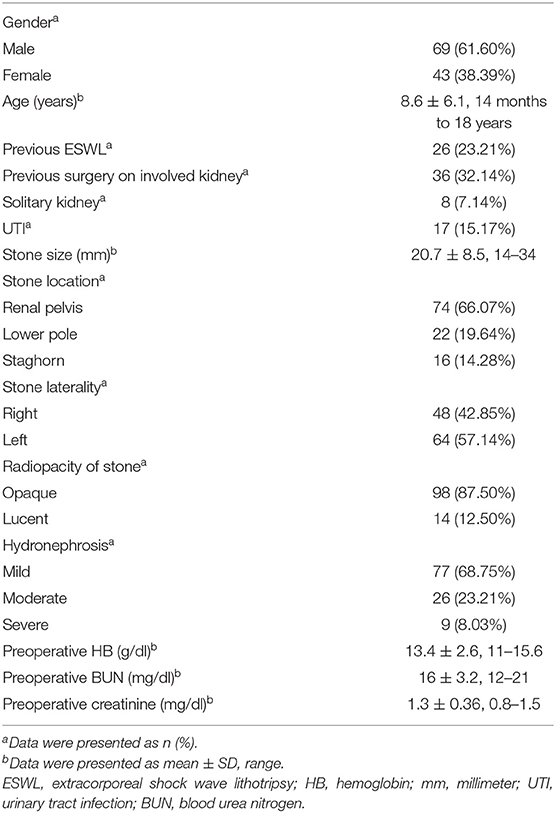
Table 1. Demographic characteristics of 112 pediatric patients who underwent mini-percutaneous nephrolithotomy (MPCNL).
The mean operation time was 65 min (35–100 min), and mean radiation was 0.6 min (0.2–1.4 min). Nephrostomy tube was inserted in 17 (15.17%) patients, tubeless MPCNL (having externalized ureteral catheter) in 70 patients including 6 patients who had double-J stent (62.50%), and totally tubeless in 25 (22.32%) cases.
Low-grade fever was detected in 14 patients (12.5%). Four patients needed packed cell transfusion, and two patients had increased level of creatinine, which improved with conservative management. One patient developed urosepsis that resolved with antibiotic therapy. None of the patients had kidney perforation or other organ injury or death (Table 2).
Early stone-free rate (SFR) after operation was 90.2% (101 patients) on the first day after operation in accordance with KUB X-ray or US (14), but 6 patients had residual fragment <5 mm, which passed spontaneously 2 weeks after the operation (total SFR reached 95.3% without any axillary procedure). Three patients underwent second-look nephroscopy, and ureteroscopy was done for two patients due to migrated stone fragments to the distal ureter.
Discussion
The results of this study demonstrate high clearance rate and acceptable complication rate of MPCNL procedure in patients under 18 years of age. Nephrolithiasis in children is increasing, and treatments have progressed to minimal invasive modalities including ESWL and PCNL, with its advancement to super minimal invasive and laparoscopy, instead of open surgery such as in adults even for nephrectomy (15, 16). PCNL, as one of the minimal invasive ways for treatment of renal stones, has progressed and modified since 1976 (17). Renal access has changed from pure fluoroscopic to combined fluoroscopic/ultrasound and pure ultrasound guided to minimize the surgeon and patient radiation exposure (18, 19). The technology of miniaturization of the access sheath has progressed recently, and the miniaturized PCNL can currently be classified into mini-PCNL (≤22 Fr), Chinese mini-PCNL (14–20 Fr), super-mini-PCNL (10–14 Fr), ultra-mini-PCNL (11–13 Fr), micro-PCNL (4.8 Fr), and mini-micro-PCNL (8 Fr) (20). Jackman was the first to perform MPCNL for adult patients in 1997 (21).
Complications of PCNL include bleeding, infectious complications, rupture of the PCS, urinary system leakage, thoracic complications, other organ injury (colon, bowel, spleen, liver), and postoperative pain (22, 23). It is established that MPCNL has the same effectiveness and less complications compared with standard PCNL (17, 24). SFR does not significantly differ between these two procedures. Bleeding, blood transfusion need, and postoperative hospitalization are less in MPCNL (17). Operation time is slightly more in MPCNL. Fever, postoperative pain, kidney, and another organ injury are less in MPCNL (24).
Wah et al. (25) performed MPCNL on 23 pediatric patients. The median stone burden was 3.44 cm2, 10 on the right and 13 on the left. Their primary SFR was 83.6%, which increased to 90.5% after treating the residual fragments. One of their patients developed postoperative hydrothorax and two of them had urinary tract infection. We had early SFR about 90% and total SFR 95.3%, which was higher than other studies, and 5.3% residual stone fragment. Farouk et al. (26) performed a prospective study on 108 pediatric patients with 1- to 2-cm renal stone and randomized them into two groups to compare MPCNL and ESWL. Those who underwent MPCNL had 88.9% SFR after the first session surgery and reached 92.59% SFR after the second-look PCNL. However, the ESWL group had 55.6% after the first session and reached 88.89% SFR after the third session of ESWL (26). Another study compared the outcomes of super-MPCNL and retrograde intra-renal surgery (RIRS) for children with upper urinary tract calculus. Those who underwent RIRS had a significantly longer operating time (76.3 vs. 53.9 min) and postoperative hospital stay (4.2 vs. 2.9 days), less SFR (60.0 vs. 94.4%), and more re-treatment rate (20.0 vs. 0.0%) (27).
Another retrospective study was done on 163 patients who underwent MPCNL. They reported 95.7% SFR, 37-min mean operation time, 18.4-mm mean stone size, and 14.6% postoperative fever (28). In our study, 12.5% of the patients developed fever after surgery, and one of them had urosepsis. Sofimajidpour et al. (29) reported the outcome of 22 pediatric patients who underwent ultra-mini-PCNL. SFR was 95.5% among their patients, 18.2% had postoperative fever, and none of them developed septicemia. Liu et al. had a study to explore the risk factors of sepsis following MPCNL. Twenty out of 834 studied patients had developed septic shock. Of them, three patients expired due to multiple organ dysfunction syndromes. They found that postoperative septic shock was associated with female sex (OR = 1.055, P < 0.001) and diabetes mellitus (OR = 4.192, P = 0.001) (30). All of our patients were cured with antibiotic therapy and conservative managements. Children may develop hyponatremia and hypothermia; it is recommended to use warm saline for irrigation. Although, some studies showed that distilled water was safe in adult PCNL, saline is the standard solution (31). None of our patients had developed these problems in this study.
The current study had several limitations. First, this is a retrospective observational study, which needs validation with larger sample size, but in prospective studies. Second, the natural history of residual fragments in children is not well-known and is estimated the same as adult urolithiasis, which may not be similar for pediatric cases. Third, our study had a few subjects <5 years of age. Fourth, we did not use the multivariable model (The multivariable models were studied in previous articles. Additionally, it could help avoid crowdedness and make this study easier to read and comprehend since we aimed to evaluate the MPCNL in pediatric patients). Next, there was no access to data on stone composition (The use of infrared spectrophotometry had not been routinely used by the laboratory in our center, and most of the stone analyses were carried out in a private laboratory clinic, and we do not have access to these data); finally, there was no control group for comparison of MPCNL with other treatment modalities.
Conclusion
The results of our study reveal that MPCNL in children is a relative safe procedure with acceptable complication and appropriate surgery outcomes.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the ethics committees of Shiraz University of Medical Sciences (Approval code# IR.sums.med.rec.1398.459). Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
MH: investigation, resources, writing-reviewing and editing, and supervision. DI, AAl, and AE: investigation and resources. AH: methodology, software, and formal analysis. MB: software and data curation. AAd and FA: conceptualization, writing-original draft preparation, software, and data curation. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Vice-Chancellor of Research and Technology, Shiraz University of Medical Sciences. This study was part of a Urology residency thesis by Ala'a Altofeyli (thesis NO#17772).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank Shiraz University of Medical Sciences, Shiraz, Iran, and also the Center for Development of Clinical Research of Nemazee Hospital, and Dr. Nasrin Shokrpour for editorial assistance.
References
1. Novak TE, Lakshmanan Y, Trock BJ, Gearhart JP, Matlaga BR. Sex prevalence of pediatric kidney stone disease in the United States: an epidemiologic investigation. Urology. (2009) 74:104–7. doi: 10.1016/j.urology.2008.12.079
2. Tasian GE, Ross ME, Song L, Sas DJ, Keren R, Denburg MR, et al. Annual incidence of nephrolithiasis among children and adults in South Carolina from 1997 to 2012. Clin J Am Soc Nephrol. (2016) 11:488–96. doi: 10.2215/CJN.07610715
3. Ward JB, Feinstein L, Pierce C, Lim J, Abbott KC, Bavendam T, et al. Pediatric urinary stone disease in the United States: the urologic diseases in america project. Urology. (2019) 129:180–7. doi: 10.1016/j.urology.2019.04.012
4. Mahmood SN, Aziz BO, Tawfeeq HM, Fakhralddin SS. Mini–versus standard percutaneous nephrolithotomy for treatment of pediatric renal stones: is smaller enough? J Pediatr Urol. (2019) 15:664.e1–6. doi: 10.1016/j.jpurol.2019.09.009
5. Baydilli N, Tosun H, Akinsal EC, Gölbaşi A, Yel S, Demirci D. Effectiveness and complications of mini-percutaneous nephrolithotomy in children: one center experience with 232 kidney units. Turk J Urol. (2020) 46:69. doi: 10.5152/tud.2019.19158
6. Assimos D, Krambeck A, Miller NL, Monga M, Murad MH, Nelson CP, et al. Surgical management of stones: American urological association/endourological society guideline, PART I. J Urol. (2016) 196:1153–60. doi: 10.1016/j.juro.2016.05.090
7. Dombrovskiy V, Olweny EO. Percutaneous nephrolithotomy in children: analysis of nationwide hospitalizations and short-term outcomes for the United States, 2001–2014. J Endo urol. (2018) 32:912–8. doi: 10.1089/end.2018.0370
8. Guven S, Frattini A, Onal B, Desai M, Montanari E, Kums J, et al. Percutaneous nephrolithotomy in children in different age groups: data from the Clinical Research Office of the Endourological Society (CROES) percutaneous nephrolithotomy global study. BJU Int. (2013) 111:148–56. doi: 10.1111/j.1464-410X.2012.11239.x
9. Tian Y, Yang X, Luo G, Wang Y, Sun Z. Initial prospective study of ambulatory mPCNL on upper urinary tract calculi. Urol J. (2020) 17:14–8. doi: 10.22037/uj.v0i0.4828
10. Planz VB, Posielski NM, Lubner MG, Li K, Chen GH, Nakada SY, et al. Ultra-low-dose limited renal CT for volumetric stone surveillance: advantages over standard unenhanced CT. Abdom Radiol. (2019) 44:227–33. doi: 10.1007/s00261-018-1719-5
11. Hennessey DB, Kinnear NK, Troy A, Angus D, Bolton DM, Webb DR. Mini PCNL for renal calculi: does size matter? BJU Int. (2017) 119:39–46. doi: 10.1111/bju.13839
12. Agrawal MS, Agrawal M. Tubeless percutaneous nephrolithotomy. Indian J Urol. (2010) 26:16. doi: 10.4103/0970-1591.60438
13. Tefekli A, Karadag MA, Tepeler K, Sari E, Berberoglu Y, Baykal M, et al. Classification of percutaneous nephrolithotomy complications using the modified clavien grading system: looking for a standard. Eur Urol. (2008) 53:184–90. doi: 10.1016/j.eururo.2007.06.049
14. Ahmed F, Askarpour M-R, Eslahi A, Nikbakht H-A, Jafari S-H, Hassanpour A, et al. The role of ultrasonography in detecting urinary tract calculi compared to CT scan. Res Rep Urol. (2018) 10:199. doi: 10.2147/RRU.S178902
15. Aminsharifi A, Hosseini M-M, Khakbaz A. Laparoscopic pyelolithotomy versus percutaneous nephrolithotomy for a solitary renal pelvis stone larger than 3 cm: a prospective cohort study. Urolithiasis. (2013) 41:493–7. doi: 10.1007/s00240-013-0589-0
16. Aminsharifi A, Taddayun A, Niroomand R, Hosseini M-m, Afsar F, Afrasiabi MA. Laparoscopic nephrectomy for non-functioning kidneys is feasible after previous ipsilateral renal surgery: a prospective cohort trial. J Urol. (2011) 185:930–4. doi: 10.1016/j.juro.2010.10.075
17. Thapa BB, Niranjan V. Mini PCNL over standard PCNL: what makes it better? Surg J. (2020) 6:e19–23. doi: 10.1055/s-0040-1701225
18. Hosseini MM, Hassanpour A, Farzan R, Yousefi A, Afrasiabi MA. Ultrasonography-guided percutaneous nephrolithotomy. J Endourol. (2009) 23:603–7. doi: 10.1089/end.2007.0213
19. Hosseini MM, Yousefi A, Rastegari M. Pure ultrasonography-guided radiation-free percutaneous nephrolithotomy: report of 357 cases. Springerplus. (2015) 4:1–5. doi: 10.1186/s40064-015-1078-4
20. Zeng G, Zhu W, Lam W. Miniaturised percutaneous nephrolithotomy: its role in the treatment of urolithiasis and our experience. Asian J Urol. (2018) 5:295–302. doi: 10.1016/j.ajur.2018.05.001
21. Jackman SV, Docimo SG, Cadeddu JA, Bishoff JT, Kavoussi LR, Jarrett TW. The “mini-perc” technique: a less invasive alternative to percutaneous nephrolithotomy. World J Urol. (1998) 16:371–4. doi: 10.1007/s003450050083
22. Kallidonis P, Panagopoulos V, Kyriazis I, Liatsikos E. Complications of percutaneous nephrolithotomy: classification, management, and prevention. Curr Opin Urol. (2016) 26:88–94. doi: 10.1097/MOU.0000000000000232
23. Kyriazis I, Panagopoulos V, Kallidonis P, Özsoy M, Vasilas M, Liatsikos E. Complications in percutaneous nephrolithotomy. World J Urol. (2015) 33:1069–77. doi: 10.1007/s00345-014-1400-8
24. Zhu W, Liu Y, Liu L, Lei M, Yuan J, Wan SP, et al. Minimally invasive versus standard percutaneous nephrolithotomy: a meta-analysis. Urolithiasis. (2015) 43:563–70. doi: 10.1007/s00240-015-0808-y
25. Wah TM, Kidger L, Kennish S, Irving H, Najmaldin A. MINI PCNL in a pediatric population. Cardiovasc Intervent Radiol. (2013) 36:249–54. doi: 10.1007/s00270-012-0460-7
26. Farouk A, Tawfick A, Shoeb M, Mahmoud MA, Mostafa DE, Hasan M, et al. Is mini-percutaneous nephrolithotomy a safe alternative to extracorporeal shockwave lithotripsy in pediatric age group in borderline stones? A randomized prospective study. World J Urol. (2018) 36:1139–47. doi: 10.1007/s00345-018-2231-9
27. Jia H, Li J, Liu B, Zhang P, Yusufu A, Nan Y, et al. Comparison of super-mini-PCNL and flexible ureteroscopy for the management of upper urinary tract calculus (1–2 cm) in children. World J Urol. (2020) 39:195–200. doi: 10.1007/s00345-020-03150-x
28. Long Q, Guo J, Xu Z, Yang Y, Wang H, Zhu Y, et al. Experience of mini-percutaneous nephrolithotomy in the treatment of large impacted proximal ureteral stones. Urol Int. (2013) 90:384–8. doi: 10.1159/000343668
29. Sofimajidpour H, Rasouli MA, Zarei B, Hosseini M. Ultra-mini-percutaneous nephrolithotomy for the treatment of upper urinary tract stones sized between 10-20 mm in children younger than 8 years old. J Urol. (2020) 17:139–42. doi: 10.22037/uj.v0i0.5903
30. Liu C, Zhang X, Liu Y, Wang P. Prevention and treatment of septic shock following mini-percutaneous nephrolithotomy: a single-center retrospective study of 834 cases. World J Urol. (2013) 31:1593–7. doi: 10.1007/s00345-012-1002-2
Keywords: minimal invasive, nephrolithiasis, nephrolithotomy, pediatrics, mini-percutaneous
Citation: Hosseini MM, Irani D, Altofeyli A, Eslahi A, Basiratnia M, Haghpanah A, Adib A and Ahmed F (2021) Outcome of Mini-Percutaneous Nephrolithotomy in Patients Under the Age of 18: An Experience With 112 Cases. Front. Surg. 8:613812. doi: 10.3389/fsurg.2021.613812
Received: 03 October 2020; Accepted: 10 May 2021;
Published: 15 June 2021.
Edited by:
Khurshid Ghani, University of Michigan, United StatesReviewed by:
Katharina Boehm, Johannes Gutenberg University Mainz, GermanyJohn Michael DiBianco, University of Michigan, United States
Copyright © 2021 Hosseini, Irani, Altofeyli, Eslahi, Basiratnia, Haghpanah, Adib and Ahmed. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ali Eslahi, YWxpZXNsYWhpQHlhaG9vLmNvbQ==
 Mohammad Mehdi Hosseini1
Mohammad Mehdi Hosseini1 Dariush Irani
Dariush Irani Ala'a Altofeyli
Ala'a Altofeyli Ali Eslahi
Ali Eslahi Mitra Basiratnia
Mitra Basiratnia Abdolreza Haghpanah
Abdolreza Haghpanah Ali Adib
Ali Adib Faisal Ahmed
Faisal Ahmed