
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Surg. , 28 September 2018
Sec. Visceral Surgery
Volume 5 - 2018 | https://doi.org/10.3389/fsurg.2018.00057
Introduction: In hernia surgery, too, the influence of the surgeon on the outcome can be demonstrated. Therefore the role of the learning curve, supervised procedures by surgeons in training, simulation-based training courses and surgeon volume on patient outcome must be identified.
Materials and Methods: A systematic search of the available literature was carried out in June 2018 using Medline, PubMed, and the Cochrane Library. For the present analysis 81 publications were identified as relevant.
Results: Well-structured simulation-based training courses was found to be associated with a reduced perioperative complication rate for patients operated on by trainees. Open as well as, in particular, laparo-endoscopic hernia surgery procedures have a long learning curve. Its negative impact on the patient can be virtually eliminated through consistent supervision by experienced hernia surgeons. However, this presupposes availability of an adequate trainee caseload and of well-trained hernia surgeons and calls for a certain degree of centralization in hernia surgery.
Conclusion: Training courses, learning curve, supervision, and surgeon volume are important aspects in training and outcomes in hernia surgery.
Using multivariable analyses and propensity score-matched comparisons it is possible to identify the influence factors impacting the outcome in hernia surgery (1, 2). In hernia surgery, too, the influence of the individual surgeon on the outcome can be demonstrated (3). There is one prominent example of that in the literature. A Swedish surgeon not only impacted comparison of totally extraperitoneal patch plasty (TEP) vs. the Lichtenstein operation in primary inguinal hernia repair due to a high recurrence rate in a prospective randomized trial to the disadvantage of TEP but also impacted a meta-analysis, likewise to the disadvantage of TEP (4–6). A further aspect is that hernia surgery has become increasingly more complex due to the introduction of new techniques and technologies (7). That gives rise to a debate about appropriate training in hernia surgery (7). “Many studies have indicated that surgical trainees are not receiving sufficient experience, and are failing to reach nationally identified targets” (8). Therefore well-structured training opportunities and training concepts that take account of the learning curve, simulation-based training, supervision, surgeon, and hospital caseload are needed. The following analysis of the available literature investigates these aspects and their impact on outcomes in hernia surgery.
A systematic search of the available literature was performed in June 2018 using Medline, PubMed, and the Cochrane Library. Furthermore, surgical journals and the reference lists of published articles were searched for relevant studies.
The following search terms were used: “Hernia and learning curve,” “Hernia and training,” “Hernia and supervision,” “Hernia and training course,” “Hernia and caseload,” “Hernia and volume,” “Hernia and experience,” “Hernia and education,” “Hernia and simulation-based training courses.”
The abstracts of 742 publications were consulted and a decision was taken on their inclusion in this literature review. For the present analysis 81 publications were identified as relevant (Figure 1). The quality of evidence according to Grade is moderate.
“Surgical training has traditionally been an apprenticeship, where the surgical trainee learns to perform surgery under the supervision of a trained surgeon” (9). Based on the published guidelines, the techniques currently recommended for inguinal hernia repair are the laparo-endoscopic TEP (totally extraperitoneal patch plasty) and TAPP (transabdominal preperitoneal patch plasty) as well as the Lichtenstein technique, and for ventral and incisional hernia repair the laparoscopic IPOM (intraperitoneal only mesh), sublay and posterior component separation technique (6, 10–20). The learning curve in laparo-endoscopic techniques in hernia surgery is longer due to the greater complexity (11, 12). Hence, there is a growing call for the introduction of preclinical courses to help master the learning curve, especially in laparo-endoscopic hernia surgery (6, 11).
In the International guidelines for groin hernia management the recommendation for a goal-directed curriculum including anatomy, procedure steps, intraoperative decision-making and proficiency-based, simulation-enhanced technical skills training has been strongly upgraded (11).
In a systematic review about the state of evidence on simulation-based training for laparoscopic surgery significant effects were identified for simulation-based training courses for knowledge, skills time, skills process, skills product, behavior time, behavior process, and patient effects (21). And in an extended review of patient outcomes in simulation-based medical education an association was found between simulation-based education and small to moderate patient benefits (22). Here, too little attention has been paid to date to the cost aspect, whereby simulation-based medical education could have potential savings' effects (23). That applies to the costs incurred for training young surgeons as well as to the operative times and hospital stay (9).
In a prospective randomized trial (RCT) it was found that for inguinal hernia surgery in TEP technique a simulation-based mastery learning course led to a reduction in the operative time, improved trainee performance, a reduced intra- and postoperative complication rate and a lower hospital admission rate (24). Evaluation of simulation-based training courses for laparo-endoscopic hernia surgery showed that they received a very positive assessment from young surgeons in training (25).
Consensus recommendations from the Association of Surgeons in Training for improving the future of surgical training include a recommendation whereby trainees have an obligation to ensure they play a proactive role in utilizing all training opportunities available, including surgical simulation facilities (26).
These simulation-based training courses could also be part of a standardized curriculum concept for continuing training in hernia surgery along the lines of a “Hernia School” (7). In any case the goal should be, through the formulation of a definitive curriculum for acquisition of surgical skills outside the operating room, to prepare young surgeons for clinical surgical practice (27).
The corresponding concepts and models are available for hernia surgery (7, 24, 25, 28–31). Surgeons in training should be urgently required to intensively engage with these training concepts and training models before carrying out their initial procedures on hernia patients, in their own interest and that of the patient. The available state of evidence supports that demand but it should be further improved in future studies. However, that demand has already now been accordingly upgraded in the new International Guidelines for Groin Hernia Management, even in the absence of strong evidence so far, because of its implications for patient treatment (11).
“Increasing performance through learning and repeating is well known” (32). “The repetition of a special task over a period of time leads to improvement of the results and shortens the time used to complete the task” (32). “In surgery the term ‘learning curve' is often used to describe the phenomenon of acquiring the surgical skills to perform a specific operation safely, sufficiently and effectively” (32). Since the learning curve in laparo-endoscopic hernia surgery is longer compared with in open procedures because of the greater complexity of the procedures (12), in the literature there are essentially more studies reporting on the learning curve in laparo-endoscopic compared with open hernia surgery. Likewise, since there seems to be also a difference between the learning curves in the endoscopic TEP and the laparoscopic TAPP in inguinal hernia repair, far more studies have been carried out on TEP (33–49) than on TAPP (50–52) (Tables 1, 2).
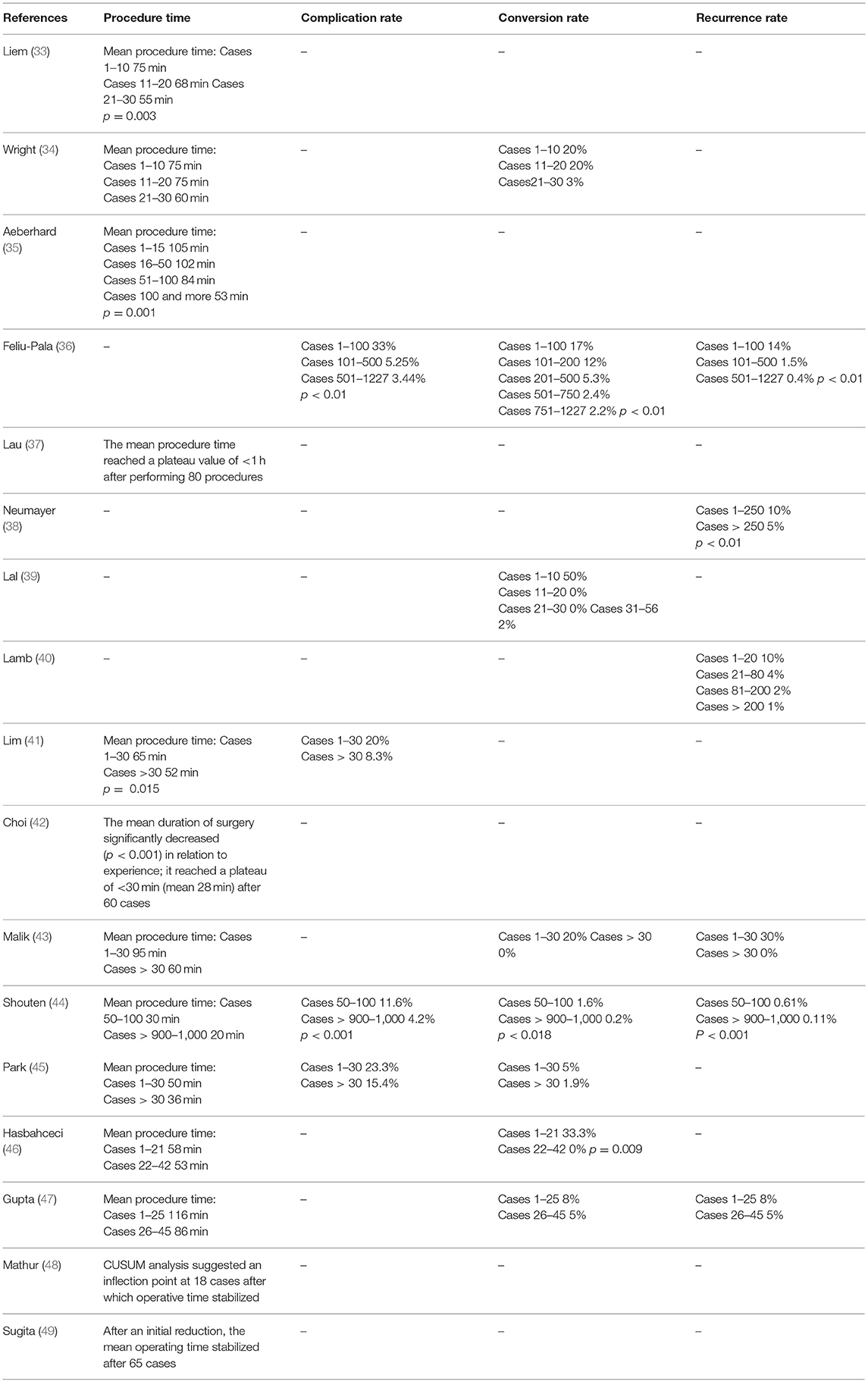
Table 1. Learning curve of inguinal hernia repair in totally extraperitoneal patch plasty (TEP) technique.
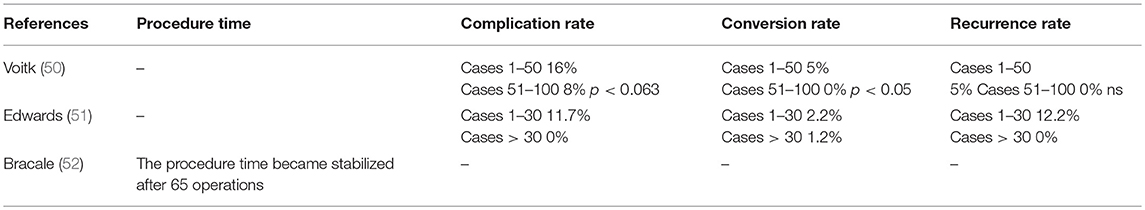
Table 2. Learning curve of inguinal hernia repair in transabdominal preperitoneal patch plasty (TAPP) technique.
The operative time for TEP is < 1 h once the surgeon has performed 30–100 operations (33, 37, 41–46). The postoperative complication rate can still be significantly reduced after more than 100 TEP operations compared with up to 100 operations (36, 44). That is also true for the conversion rate. Likewise, the recurrence rate can be significantly reduced after more than 250 TEP operations compared with up to 250 TEP operations (38).
Accordingly, the learning curve in the TEP technique for inguinal hernia repair, when taking into account all outcome criteria, spans a surgical volume of up to 250 operations. Hence, the TEP technique seems to be associated with a longer learning curve for inguinal hernia repair (Tables 1, 2), although some studies report about a much shorter learning curve (34, 39, 43, 45, 46).
For TAPP the learning curve is reported to be around 50–100 procedures (Table 2). As such, the learning curve in TAPP seems to be associated with a lower caseload compared with TEP. This might be explained by better comparability of TAPP with other laparoscopic operations and the much narrower spatial conditions in TEP. In a Consensus Development Conference of the European Association of Endoscopic Surgery a statement is given, that studies showed significant reduction of operating time, conversion rates, and complication rates after 30–100 TEP procedures and 50–75 TAPP procedures (12). In the new international guidelines for groin hernia management (11) no difference in the learning curve between TEP and TAPP was found.
Nevertheless, training in TEP and TAPP requires a corresponding caseload in the training hospital and longer supervision of trainees by an experienced laparo-endoscopic surgeon. This of courses means that higher costs are incurred for training in laparo-endoscopic surgery (23).
The longer learning curve in laparo-endoscopic surgery could possibly be reduced through more the provision of more intensive preclinical training courses with simulation models. Therefore further models must be developed for learning the laparo-endoscopic techniques and shortening the learning curve, and these should be made available in intensive preclinical training courses.
In open mesh repair of inguinal hernias unsupervised junior trainees had unacceptably high recurrence rates (53). On average, the trainees in a UK study achieved proficiency for independent inguinal hernia repair after they had performed 64 repairs (range 12–73) which usually was reached in their fourth year of training (11, 54).
Accordingly, open inguinal hernia repair with mesh also has a relevant learning curve. Therefore the benefits of structured, simulation-based training courses should also be exploited for open mesh repair of inguinal hernia.
The learning curve in laparoscopic ventral hernia repair is associated with a significantly higher intestinal injury rate on comparing the first 32 operations with the subsequent 32 operations (12 vs. 0%; p = 0.02) (55). Likewise, there were clear, but not significant, differences in the conversion rate (12 vs. 0%; p = 0.11) (55).
A further study of the learning curve in laparoscopic ventral hernia repair that identified a conversion rate of 13.8% and intestinal injury rate of 6.9% attests to a high complication rate during the learning curve (56).
An investigation of the learning curve in laparoscopic ventral hernia repair found that three experienced laparoscopic surgeons reached a plateau operative time after 12 operations each (57).
Here too, as pointed out above, the learning curve can be reduced though structured simulation-based training courses (55).
But mentoring and supervision by a surgeon experienced in this technique is crucial during the learning curve. Therefore the learning curve under the supervision of an experienced hernia surgeon is now analyzed in the following.
Training in complex laparoscopic procedures under the supervision of an experienced surgeon can be performed safely without jeopardizing the patient's outcome (58). Only very rarely does a surgeon in training perform operations without the supervision of an experienced surgeon (59). The degree of supervision needed by a surgeon in training can apparently be well estimated by experienced surgeons (59). Appropriate supervision of surgeons in training does not lead to poorer patient outcomes (59).
In hernia surgery, too, there are a number of studies that investigated the role of supervision of surgeons in training or during the learning curve on these outcomes (32, 53, 60–66) (Table 3). Follow-up from 3.5 to 6.1 years of TEP operations carried out by trainees under the supervision of experienced consultants identified recurrence rates of 1% and 2.6%, respectively (60, 61). The chronic pain rate following TEP repair was 1.5% after 6.1 years (61).
A comparative study of TAPP did not find any significantly higher postoperative complication rates or recurrence rates for patients operated on by supervised trainees compared with those operated on by experienced surgeons (62).
Likewise, a comparable recurrence rate was identified for open and laparoscopic inguinal hernia surgery performed by trainees under supervision of consultants (53).
Only in the operative time was a difference found in a further study of the Lichtenstein operation to the disadvantage of trainees (63). But not even a longer operative time was found for trainees compared with consultants in all studies (64, 65).
For more complex procedures, such as hiatoplasty and fundoplication for reflux disease, high demands are made on the trainees in preparation for such operations as well as on the supervisor in order to assure comparable outcomes (66).
The available studies clearly demonstrate that consistent supervision by experienced consultants of trainees play a pivotal role in mastering the learning curve. This virtually eliminates the negative implications of the trainee learning curve for the patient.
Somewhat longer trainee operative times are not a problem for the patient but rather are just a matter of higher costs (67). But what is essentially more important is the aspect of patient safety. Each trainee should be supervised by an experienced consultant until they have mastered the learning curve for the respective procedure. The fact that, as stated above, the learning curve in hernia surgery procedures can be very long (TEP) means a considerable investment in training young surgeons. Furthermore, a sufficiently large caseload must be available for training. This also calls for the formation of a certain number of centers in hernia surgery with specified caseloads (68).
Annual caseload specifications for individual hospitals and each surgeon have important implications for the patient outcome. This is now discussed below on the basis of the available literature.
An overview of systematic reviews has shown strong evidence of an association between higher volumes and better outcomes in surgery (69).
An analysis of inpatient Hospital Episode Statistics in 125,342 patients with inguinal hernia repair showed for surgeons with a low laparoscopic hernia repair caseload an increased reoperation rate (70).
In a registry-based analysis of 16,240 laparo-endoscopic (TEP, TAPP) primary inguinal hernia repairs low-volume surgeons (< 25 procedures per year) have significantly higher recurrence and pain on exertion rates than high-volume surgeons (≥25 procedures per year) (71).
Another study also confirmed the link between a high surgical volume and improved outcome for TEP repair of inguinal hernia (72).
In a study comparing the results of surgeons with an annual volume of > 30 vs. 15–30 vs. < 15 TEP repairs the perioperative complication and recurrence rates were lowest in the high volume group (73).
An analysis from the New York Statewide Planning and Research Cooperative System with 18,047 patients found a strong association between individual surgeon incisional hernia repair volume (< 36 vs. ≥36 repairs/year) and reoperation rates, operative efficiency, and charges (74). The authors concluded that preferential referral to high-volume surgeons may lead to improved outcomes and lower costs (74).
In a study of the National Impatient Sample patients treated at high—volume hospitals with >60 ventral hernia repairs per year were less likely to experience a major complication (OR 0.88; 95% CI 0.82–0.96; p = 0.002) or wound-based complication (OR 0.84; 95% CI 0.76–0.92; p < 0.001) (75). The authors concluded, that hospitals performing larger numbers of ventral hernia repairs, despite caring for a more complex patient population, may be associated with better patient outcomes than lower volume hospitals (75).
In addition to the well-known influence factors that impact the outcome in hernia surgery, the influence of the surgeon under different aspects can be demonstrated. That gives rise to a debate about appropriate training in hernia surgery (7). Studies have indicated that surgical trainees are not receiving sufficient experience (8). Traditionally, surgery has been taught and learned through a structured training program and proctorship (76). The orthodox apprenticeship approach of surgical training where trainees learn from their supervisors is no longer sustainable (76). This longstanding training approach is being increasingly challenged by legal and ethical concerns for patient safety, working time regulations, the cost, and surgical complications (77). As direct consequence of these challenges the interest in simulation-based training concepts has increased dramatically (78). In systematic reviews simulation-based training courses contribute to a shortening of the learning curve and improvement of trainee's surgical skills (21, 22, 78). This reduces the perioperative complication rate during the learning curve (24). Despite the advantages simulation-based training courses have not been fully incorporated into surgical training curriculum (78). But experts expect that this will become reality over the next decade (78). The Association of Surgeons in Training recommends for training units the introduction and funding of local hospital-based skills labs with appropriate training and simulation equipment (26). In a pilot project for improving surgical training the Royal College of Surgeons of England has integrated simulation-based training courses for developing surgical skills earlier, so that time is not wasted, particularly in the early years of surgical training (79). Since laparo-endoscopic and advanced open hernia operations are complex procedures, trainees should definitely participate in well-structured, 2 days training courses with theoretical and practical training on simulations (7, 25) and anatomic specimens before they perform their first procedures on a patient.
Supervision by experienced surgeons is another important aspect for prevention of perioperative complications and avoidance of the negative impact of the learning curve of the surgeon in training when performing hernia surgery procedures. Consistent supervision of trainees in the learning curve can achieve perioperative complication rates and long-term outcomes on a par with those of an experienced consultant, thus completely eliminating the negative effects of the trainee learning curve on the patients. However, this presupposes the availability of an adequate number of experienced consultants to engage in supervision. This also demonstrates that training in surgery is associated with considerable costs but that investment is crucial to patient safety. However, each surgery-teaching/training hospital should allocate funds in its budget to cover these costs.
Qualification of the training consultants is another important aspect. The studies presented above demonstrate the clear link between the annual caseload per consultant and the outcome. Accordingly, the consultants supervising trainees when performing surgical procedures should themselves conduct a minimum number of the most important hernia surgery procedures each year. That calls for a certain degree of specialization in hernia surgery.
The aspects comprising the learning curve, supervision, and surgeon volume are relevant arguments that support specialization and formation of centers in hernia surgery for optimal implementation of the aforementioned requirements (80). This presupposes the availability of a corresponding caseload and specialization of consultants in hernia surgery. Developments to that effect should be based within departments of general surgery and cover the entire range of hernia surgery because the infrastructure of a large hospital is needed for complex hernia surgery.
FK literature search, literature analyses, publication concept, publication draft.
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Köckerling F, Stechemesser B, Hukauf M. TEP versus lichtenstein: which technique is better for the repair of primary unilateral inguinal hernias in men? Surg Endosc. (2016) 30:3304–13. doi: 10.1007/s00464-015-4603-1
2. Köckerling F, Bittner R, Kofler M, Mayer F, Adolf D, Kuthe A, et al. Lichtenstein versus total extraperitoneal patch plasty versus transabdominal patch plasty technique for primary unilateral inguinal hernia repair: a registry-based, propensity score-matched comparison of 57.906 patients. Ann Surg. (2017) doi: 10.1097/SLA0000000000002541. [Epub ahead of print].
3. Aquina CT, Fleming FJ, Becerra AZ, Xu Z, Hensley BJ, Noyes K, et al. Explaining variation in ventral and inguinal hernia repair outcomes: a population-based analysis. Hernia (2017) 162:628–39. doi: 10.1016/j.surg.2017.03.013
4. Eklund AS, Montgomery AK, Rasmussen IC, Sandbue RP, Bergkvist LA, Rudberg CR. Low recurrence rate after laparoscopic (TEP) and open (Lichtenstein) inguinal hernia repair: a randomized multicenter trial with 5-year follow-up. Ann Surg. (2009) 249:33–8. doi: 10.1097/SLA.Ob013e31819255d0
5. O'Reilly EA, Burke JP, O'Connell PR. A meta-analysis of surgical morbidity and recurrence after laparoscopic and open repair of primary unilateral inguinal hernia. Ann Surg. (2012) 255:846–53. doi: 10.1097/SLA.0b013e31824e96cf
6. Miserez M, Peeters E, Aufenacker T, Bouillot JL, Campanelli G, Conze J, et al. Update with level 1 studies of the European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia (2014) 18:151–63. doi: 10.1007/s10029-014-1236-6
7. Lorenz R, Stechemesser B, Reinpold W, Fortelny R, Mayer F, Schröder W, et al. Development of a standardized curriculum concept for continuing training in hernia surgery: German Hernia School. Hernia (2017) 21:153–62. doi: 10.1007/s10029-016-1566-7
8. Radford PD, Derbyshire LF, Shalzhoub J, Fitzgerald JEF. Publication of surgeon specific outcome data: a review of implementation, controversies and the potential impact on surgical training. Int J Surg. (2015) 13:211–6. doi: 10.1016/j.ijsu.2014.11.049
9. Gurusamy KS, Nagendran M, Toon CD, Davidson BR. Laparoscopic surgical box model training for surgical trainees with limited prior laparoscopic experience (Review). Cochrane Database Syst Rev. (2014) 1:CD010478. doi: 10.1002/14651858.CD010478.pub2
10. Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J. et al European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia (2009) 13:343–403. doi: 10.1007/s10029-009-0529-7
11. HerniaSurge Group. International guidelines for groin hernia management. Hernia (2018) 22:1–165. doi: 10.1007/s10029-017-1668-x
12. Poelman MM, van den Heuvel B, Deelder JD, Abis GSA, Beudecker N, Bittner RR, et al. EAES Consensus Development Conference on endoscopic repair of groin hernias. Surg Endosc. (2013) 27:3505–19. doi: 10.1007/s00464-013-3001-9
13. Bittner R, Arregui ME, Bisgaard T, Dudai M, Ferzli GS, Fitzgibbons RJ, et al. Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment on inguinal Hernia [International Endohernia Society (IEHS)]. Surg Endosc. (2011) 25:2773–843. doi: 10.1007/s00464-011-1799-6
14. Bittner R, Montgomery MA, Arregui ME, Bansal V, Bingener J, Bisgaard T, et al. Update of guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment on inguinal Hernia [International Endohernia Society (IEHS)] Surg Endosc. (2015) 29:289–321. doi: 10.1007/s00464-014-3917-8
15. Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli GS, Fortelny RH et al. Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias [International Endohernia Society (IEHS)] – Part 1. Surg Endosc. (2014) 28:2–29 doi: 10.1007/s00464-013-3170-6
16. Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli GS, Fortelny RH, et al. Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias [International Endohernia Society (IEHS)] – Part 2. Surg Endosc. (2014) 28:353–79. doi: 10.1007/s00464-013-3171-5
17. Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli GS, Fortelny RH, et al. Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias [International Endohernia Society (IEHS)] – Part III. Surg Endosc. (2014) 28:380–404. doi: 10.1007/s00464-013-3172-4
18. Earle D, Scott Roth J, Saber A, Haggerty S, Bradley JF, Fanelli R, et al. SAGES guidelines for laparoscopic ventral hernia repair Surg Endosc. (2016) 30:3163–83. doi: 10.1007/s00464-016-5072-x
19. Silecchia G, Campanile F, Sanchez CL, Ceccarelli L, Antinori G, Ansaloni A, et al. Laparoscopic ventral/incisional hernia repair: updated guidelines from the EAES and EHS endorsed Consensus Development Conference. Surg Endosc. (2015) 29:2463–84. doi: 10.1007/s00464-015-4293-8
20. Liang MK, Holihan JL, Itani K, Alawadi ZM, Gonzalez JR, Askenasy EP, et al. Ventral hernia management – expert consensus guided by systematic review. Ann Surg. (2017) 265:80–9. doi: 10.1097/SLA.0000000000001701
21. Zendejas B, Brydges R, Hamstra SJ, Cook DA. State of the evidence on simulation-based training for laparoscopic surgery: a systematic review. Ann Surg. (2013) 257:586–93. doi: 10.1097/SLA.Ob013e318288c40b
22. Zendejas B, Brydges R, Wang AT, Cook DA. Patient outcomes in simulation-based medical education: a systematic review. JGIM (2013) 28:1078–89. doi: 10.1007/s11606-012-2264-5
23. Zendejas B, Wang AT, Brydges R, Hamstras SJ, Cook DA, et al. Cost: the missing outcome in simulation-based medical education research: a systematic review. Surgery (2013) 153:160–76. doi: 10.1016/j.surg.2012.06.025
24. Zendejas B, Cook DA, Bingener J, Huebner M, Dunn WF, Sarr MG, et al. Simulation-based mastery learning improves patient outcomes in laparoscopic inguinal hernia repair – a randomized controlled trial. Ann Surg. (2011) 254:3. doi: 10.1097/SLA.0b013e31822c6994
25. Köckerling F, Pass M, Brunner P, Hafermalz M, Grund S, Sauer J, et al. Simulation-based training – evaluation of the course concept “laparoscopic surgery curriculum” by the participants. Front Surg. (2016) 3:47. doi: 10.3389/fsurg.2016.00047
26. Fitzgerald JEF, Giddings CEB, Khera G, Marron CD. Improving the future of surgical training and education: consensus recommendations from the Association of Surgeons in Training. Int J Surg. (2012) 10:389–92. doi: 10.1016/j.ijsu2012.03.012
27. Paydar S, Ghahramani Z, Bolandparvaz S, Hosseinali K, Abbas HR. Learning operational strategies in surgery training. J Adv Med Educ Prof. (2014) 2:92–4.
28. Light D, Bawa S, Gallagher P. Outcomes of an innovative training course in laparoscopic hernia repair. Ann R Coll Surg Engl. (2017) 99:614–6. doi: 10.1308/rcsann.2017.0094
29. Consalvo V, Salsano V. Surgical skills improvement using a low-cost laparoscopic simulator for ventral incisional hernia. Surg Technol Int. (2017) 31:25–30
30. Jain M, Tantia O, Khanna S, Sen B, Sasmal PK. Hernia endotrainer: results of training on self-designed hernia trainer box. J Laparoendosc Adv Surg Tech A. (2009) 19:535–40. doi: 10.1089/lap.2008.0384
31. Slater GH, Jourdan I, Fölscher A, Snook AL, Cooper M, D'Allessandro C, et al. The Guildford MATTU TEP hernia model. Surg Endosc. (2001) 15:493–96. doi: 10.1007/s004640000361
32. Wiese M, Kaufmann T, Metzger J, Schüpfer G, Honimann P. Learning curve for Lichtensstein hernioplasty. Open Access Surg. (2010) 3:43–6.
33. Liem MSL, van Steensel CJ, Boelhouwer RU, Weidema WF, Clevers GJ, Meijer WS, et al. The learning curve for totally extraperitoneal laparoscopic inguinal hernia repair. Am J Surg. (1996) 171:281–5.
34. Wright D, O'Dwyer PJ. The learning curve for laparoscopic hernia repair. Surg Innov. (1998) 5:227 doi: 10.1177/155335069800500405
35. Aeberhard P, Klaiber C, Meyenberg A, Osterwalder A, Tschudi J. Prospective audit of laparoscopic totally extraperitoneal inguinal hernia repair A multicenter study of the Swiss Association for Laparoscopic and Thoracoscopic Surgery (SALTC). Surg Endosc. (1999) 13:1115–20.
36. Feliu-Palà X, Martin-Gomez M, Morales-Conde S, Fernandez-Sallent E. The impact of the surgeon's experience of the results of laparoscopic hernia repair. Surg Endosc. (2001) 15:1467–70. doi: 10.1007/s00464-001-9017-6
37. Lau H, Patil NG, Yuen WK, Lee F. Learning curve for unilateral endoscopic totally extraperitoneal (TEP) inguinal hernioplasty. Surg Endosc. (2002) 16:1724–8. doi: 10.1007/s00464-001-8298-0
38. Neumayer L, Biobbie-Hurder MS, Jonasson O, Fitzgibbons R, Dunlop D, Gibbs J, et al. Open Mesh versus Laparoscopic mesh Repair of Inguinal Hernia. N Engl J Med. (2004) 350:1819–27. doi: 10.1056/NEJMoa040093
39. Lal P, Kajla RK, Chander J, Ramteke VK. Laparoscopic total extraperitoneal (TEP) inguinal hernia repair Overcoming the learning curve. Surg Endosc. (2004) 18:642–5. doi: 10.1007/s00464-002-8649-5
40. Lamb ADG, Robson AJ, Nixon SJ. Recurrence after totally extra-peritoneal laparoscopic repair: Implications for operative technique and surgical training. Surgeon (2006) 4:299–307.
41. Lim JW, Lee JY, Lee SE, Moon JI, Ra YM, Choi IS, et al. The learning curve in laparoscopic totally extraperitoneal herniorrhaphy by moving average. J Korean Surg Soc. (2012) 83:92–6. doi: 10.4174/jkss.2012.83.2.92
42. Choi YY, Kim Z, Hur KY. Learning curve for laparoscopic totally extraperitoneal repair of inguinal hernia. Can J Surg. (2012) 55:1. doi: 10.1503/cjs.019610
43. Malik AM, Talpur AH, Soomro AG, Qureshi JN. A walk along the learning curve of totally extra-peritoneal (TEP) repair of inguinal hernia surgery. Curr Res. (2012) 2:3. doi: 10.4172/2161-1076.10000116
44. Schouten N, Simmermacher RKJ, van Dalen T, Smakman N, Clevers GJ, Davids PHP, et al. Is there an end of the “learning curve” of endoscopic totally extraperitoneal (TEP) hernia repair? Surg Endsosc. (2013) 27:789–94. doi: 10.1007/s00464-012-2512-0
45. Park BS, Ryu DY, Son GM, Cho YH. Factors influencing of difficulty with laparoscopic total extraperitoneal repair according to learning period. Ann Surg Treat Res. (2014) 87:203–8. doi: 10.4174/astr.2014.87.4.203
46. Hasbahceci M, Basak F, Acar A, Alimoglu O. A new proposal for learning curve of TEP inguinal hernia repair: ability to complete operation endoscopically as a first phase of learning curve. Minim Invas Surg. (2014) 2014:528517. doi: 10.1155/2014/528517
47. Gupta A, Bhandari V, Kumar L, Garg P, Gaind SK. A run oft he path of learning curve of laparoscopic hernia repair (TEP). Sch J App Med Sci. (2015) 3:1821–5.
48. Mathur S, Fracs Suei Lin S-Y. The learning curve in laparoscopic inguinal hernia repair: a newly qualified surgeon perspective. J Surg Res. (2016): 246–51. doi: 10.1016/j.jss2016.06.041
49. Suguita FY, Essu FF, Torres Oliveira L, Iuanoto KRM, Kato JM, Torsani MB, et al. Learning curve takes 65 repetitions of totally extraperitoneal laparoscopy on inguinal hernias for reduction of operating time and complications. Surg Endosc. (2017) 31:3939–45. doi: 10.1007/s00464-017-5426-z
50. Voitk AJ. The Learning Curve in Laparoscopic Inguinal Hernia Repair for the Community General Surgeon. JCC (1998) 41:446–50.
51. Edwards CC, Bailey RW. Laparoscopic hernia repair: the learning curve. Surg Laparosc Endosc Percutan Tech. (2000) 10:149–53.
52. Bracale U, Merola G, Sciuto A, Cavallaro G, Andreuccetti J, Pignata G. Achieving the learning curve in laparoscopic inguinal hernia repair by Tapp: a quality improvement study. J Invest Surg. (2018) 14:1–8. doi: 10.1080/08941939.2018.1468944
53. Robson AJ, Wallace CG, Sharma AK, Nixon SJ, Paterson-Brown S. Effects of training and supervision on recurrence rate after inguinal hernia repair. Br J Surg. (2004) 91:774–7. doi: 10.1002/bjs.4540
54. Abderahman T, Long J, Egan R, Lewis WG. Operative experience vs. competence: a curriculum concordance and learning curve analysis. J Surg Educ. (2016) 73:694–8. doi: 10.1016/j.jsurg.2016.01.011
55. Bencini L, Sanchez LJ. Learning curve for laparoscopic ventral hernia repair. Am J Surg. (2004) 187:378–82. doi: 10.1016/j.amjsurg.2003.12.005
56. Salameh JR, Sweeney JF, Graviss EA, Essien FA, Williams MD, Awad S, et al. Laparoscopic ventral repair during the learning curve. Hernia (2002) 6:182–7. doi: 10.1007/s10029-002-0083-z
57. Al-Harazi A, Goel R, Tan CTK, Cheah WK, Lamanto D. Laparoscopic ventral hernia repair: defining the learning curve. Surg Laparosc Endosc Percutan Tech. (2013) 24:475–7. doi: 10.1097/SLE.0000000000000020
58. Akiyoshi T, Kuroyanagi H, Ueno M, Oya M, Fujimoto Y, Konishi T, et al. Learning curve for standardized laparoscopic surgery for colorectal cancer under supervision: a single-center experience. Surg Endosc. (2011) 25:1409–14. doi: 10.1007/s00464-010-1404-4
59. Kazaure HS, Roman SA, Sosa JA. The resident as surgeon: an analysis of ACS-NSQIP. J Surg Res. (2012)178:126–32. doi: 10.1016/j.jss.2011.12.033
60. Haidenberg J, Kendrick ML, Meile T, Farley DR. Totally extraperitoneal (TEP) approach for inguinal hernia: the favorable learning curve in trainees. Curr Surg. (2003) 60:65–8. doi: 10.1016/S0149-7944(02)00657-8
61. Zendejas B, Onkendi EO, Brahmbhatt RD, Lohse CM, Greenlee SM, Farley DR. Long-term outcomes of laparoscopic totally extraperitoneal inguinal hernia repairs performed by supervised surgical trainees. Am J Surg. (2011) 201:379–84. doi: 10.1016/j.amjsurg.2010.08.019
62. Bökeler U, Schwarz J, Bittner R, Zacheja S, Smaxwil C. Teaching and training in laparoscopic inguinal hernia repair (TAPP): impact of the learning curve on patient outcome. Surg Endosc. (2013) 27:2886–93. doi: 10.1007/s00464-013-2849-z
63. Koizumi M, Sata N, Taguchi M, Kasahara N, Morishima K, Kaneda Y, et al. Participation of surgical residents does not adversely affect the outcome of inguinal hernia repair in an integrated teaching program. J Surg Educ. (2012) 69:605–10. doi: 10.1016/j.jsurg.2012.05.015
64. El-Sharkawy AM, Morris DLJ, Grewal BS, Quarmby JW, Rowlands TE. Daycase hernia surgery: a missed training opportunity. Int J Surg. (2013) 11:338–43. doi: 10.1016/j.ijsu.2013.02.0156
65. Khan OA, Balaji S, Lahiri O, Monsell N, Agunloye V, Davies NA, et al. Impact of training on outcomes following incisional hernia repair. Acta Chir Belg. (2012) 112:432–5.
66. Brown CN, Smith LT, Watson DI, Devitt PG, Thompson SK, Jamieson GG. Outcomes for trainees vs. experienced surgeons undertaking laparoscopic antireflux surgery – is equipoise achieved? J Gastrointest Surg. (2013) 17:1173–80. doi: 10.1007/s11605-013-2211-8
67. Koperna T. How long do we need teaching in the operating room? The true costs of achieving surgical routine. Langenbecks Arch Surg. (2004) 389:204–8. doi: 10.1007/s00423-003-0421-3
68. Köckerling F, Berger D, Jost JO. What is a certified hernia center? The example of the German Hernia society and German Society of General and Visceral Surgery. Front Surg. (2014) 1:26. doi: 10.3389/fsurg.2014.00026
69. Amato L, Fusco D, Acampora A, Bontempi K, Rosa AC, Colais P, et al. Volume and health outcomes: evidence from systematic reviews and from evaluation of Italian hospital data. Epidemiol Prev. (2017) 41(5–6 (Suppl. 2)):1–128. doi: 10.19191/EP17.5-6S2.Poo1.100
70. El-Dhuwaib Y, Corless D, Emmett C, Deakin M, Slavin J. Laparoscopic versus open repair of inguinal hernia: a longitudinal cohort study. Surg Endosc. (2013) 27:936–45. doi: 10.1007/s00464-012-2538-3
71. Köckerling F, Bittner R, Kraft B, Hukauf M, Kuthe A, Schug-Pass C. Does surgeon volume matter in the outcome of endoscopic inguinal hernia repair? Surg Endosc. (2016) 31:573–85. doi: 10.1007/s00464-016-5001-z
72. Aikoye A, Harilingam M, Khushal A. The impact of high surgical volume on outcomes fram laparoscopic (Totally Extra Peritoneal) inguinal hernia repair. J Clin Diagn Res. (2015) 9:PC15–6. doi: 10.7860/JCDR/2015/14094.6057
73. AlJamal YN, Zendejas B, Gas BL, Shahzad MA, Heller SF, Kendrick ML, et al. Annual surgeon volume and patient outcomes following laparoscopic totally extraperitoneal inguinal hernia repairs. J Laparoendosc Adv Surg Tech. (2016) 26:92–8. doi: 10.1089/lap.2015.0368
74. Aquina CT, Kelly KN, Probst CP, Iannuzzi JC, Noyes K, Langstein HN, et al. Surgeon volume plays a significant role in outcomes and cost following open incisional hernia repair. J Gastrointest Surg. (2015) 19:100–10. doi: 10.1007/s11605-014-2627-9
75. Chattha A, Muste J, Patel A. The impact of hospital volume on clinical and economic outcomes in ventral hernia repair: an analysis with national policy implications. Hernia (2018) doi: 10.1007/s10029-018-1803-3. [Epub ahead of print].
76. Guraya SY. The changing landscape of surgical education training. J Musculoskelet Surg Res. (2018) 2:1–3. doi: 10.1007/s11605-2627-9
77. Roberts KE, Bell RL, Duffy AJ. Evolution of surgical skills training. World J Gastroenterol. (2006) 12:3219–24. doi: 10.3748/wjg.v12.i20.3219
78. Shaharan S, Neary P. Evaluation of surgical training in the era of simulation. World J Gastrointest Endosc. (2014) 6:436–47. doi: 10.4253/wjge.v6.i9.436
79. Royal College of Surgeons Improving Surgical Training (IST). (2018). Available online at: https://www.rcseng.ac.uk/careers-in-surgery/trainees/ist/
Keywords: hernia, training course, learning curve, case load, supervision
Citation: Köckerling F (2018) What Is the Influence of Simulation-Based Training Courses, the Learning Curve, Supervision, and Surgeon Volume on the Outcome in Hernia Repair?—A Systematic Review. Front. Surg. 5:57. doi: 10.3389/fsurg.2018.00057
Received: 23 July 2018; Accepted: 28 August 2018;
Published: 28 September 2018.
Edited by:
Hakan Kulacoglu, Recep Tayyip Erdogan University, TurkeyReviewed by:
Gabriel Sandblom, Karolinska Institutet (KI), SwedenCopyright © 2018 Köckerling. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ferdinand Köckerling, ZmVyZGluYW5kLmtvZWNrZXJsaW5nQHZpdmFudGVzLmRl
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.