- 1Department of Neurology, University of Kansas Medical Center, Kansas City, KS, United States
- 2University of Kansas Alzheimer's Disease Research Center, Fairway, KS, United States
- 3Department of Physical Medicine and Rehabilitation, University of Kansas Medical Center, Kansas City, KS, United States
- 4Department of Cell Biology and Physiology, University of Kansas Medical Center, Kansas City, KS, United States
- 5MedStar National Rehabilitation Network, Department of Rehabilitation Medicine, Georgetown University School of Medicine, Washington, DC, United States
1 Introduction
In 2017, there were over 7.6 million new ischemic strokes and 3.4 million new intracerebral hemorrhages globally. Stroke was the third-leading cause of death and disability combined (as expressed by DALYs [adjusted life-years lost]) in the world. The estimated global cost of stroke was approximately US$861 billion, or 1.12% of the global GDP (Feigin et al., 2022). Thus, because of the high burden of care associated with stroke, it is incumbent on rehabilitation providers to provide the best possible interventions to facilitate recovery in order to reduce the direct and indirect costs of post-stroke care.
When prescribing any stroke rehabilitation intervention, one of the key principles that contributes to neuroplastic changes in the brain is intensity (Kleim and Jones, 2008). Researchers have proposed variable definitions of intensity, including numbers of minutes, repetitions, sessions, or exercise intensity. While the American College of Sports Medicine uses a standard definition of exercise intensity (Table 1; Feito and Fountaine, 2022), the parameters used for moderate and vigorous intensity in stroke rehabilitation may vary across studies.
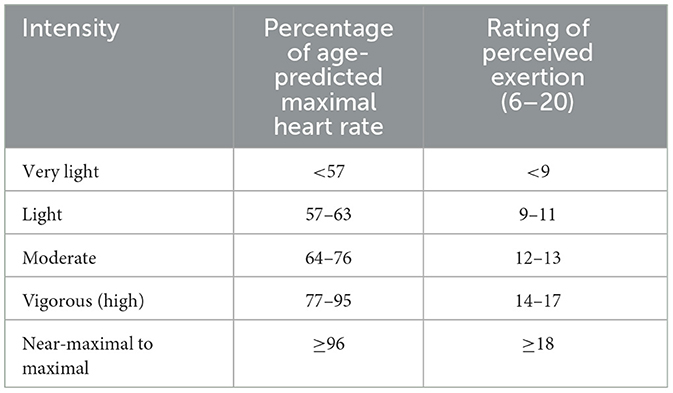
Table 1. Adapted from the american college of sports medicine's (ACSM) guidelines for exercise testing and prescription, 11th edition (Feito and Fountaine, 2022).
Aerobic exercise should be prescribed to stroke survivors as it may reduce modifiable vascular and metabolic risk factors of recurrent stroke, such as systolic blood pressure, fasting glucose, and LDL cholesterol (Billinger et al., 2014; Brouwer et al., 2021). The ACSM recommendations for healthy individuals are the same as those for stroke survivors: a minimum of 30 min of moderate-intensity exercise 5 days per week, or a minimum of 20 min of high-intensity exercise 3 days per week (Feito and Fountaine, 2022). To prescribe aerobic exercise, one can calculate the percentage of maximal heart rate (% HRmax) and rating of perceived exertion, or complete a submaximal exercise stress test using a treadmill or total body recumbent stepper to determine predicted peak oxygen consumption (VO2) (Mackay-Lyons et al., 2020). Many gaps in the literature exist to guide clinical practice for employing the FITT (frequency, intensity, time, and type) principles in stroke survivors across the continuum of recovery. A useful publication, “Aerobic Exercise Recommendations to Optimize Best Practices in Care after Stroke” is a user-friendly set of recommendations to guide screening and prescription and was developed by stroke rehabilitation professionals (Mackay-Lyons et al., 2020).
2 High-intensity training
To improve walking for individuals with chronic stroke (>6 months post-stroke), high-intensity gait training has been recommended as best practice (Hornby et al., 2020). High-intensity gait training is defined as variable context stepping activities, such as walking overground, treadmill walking, walking on uneven/compliant surfaces, and stair climbing, with a cardiovascular response of 75%−85% of age-predicted maximal heart rate (Henderson et al., 2022). High-intensity gait training can be performed either continuously or through intervals. High-intensity interval exercise focuses on repetitive switching between high-intensity bouts and active or passive recovery bouts (Boyne et al., 2013). Superiority between high-intensity continuous and high-intensity interval training has not yet been established in the stroke population. However, high-intensity interval gait training has been found to result in greater improvements in walking endurance and speed compared to that from moderate-intensity continuous gait training (Boyne et al., 2023), as well as improve blood pressure (Batacan et al., 2016; Costa et al., 2018), vascular function (Ramos et al., 2015), and aerobic fitness (Foster et al., 2015; Hwang et al., 2016). The benefits of high-intensity gait training for subacute stroke survivors (1 week to <6 months post-stroke) are less established compared to that of chronic stroke survivors, but multiple studies have demonstrated its efficacy (Holleran et al., 2014; Hornby et al., 2016; Henderson et al., 2022). For stroke survivors with and without significant cardiovascular co-morbidities, high-intensity gait training should be considered as the primary intervention if improving walking is a functional goal. The incidence of serious adverse events in both subacute and chronic stroke survivors have been limited with high-intensity gait training as compared to that of usual care (Boyne et al., 2013; Hornby et al., 2015; Henderson et al., 2022). To advance the field of stroke rehabilitation and recovery, we challenge researchers to develop, validate, and implement evidence-based interventions that maximize the functional recovery of the stroke survivors we serve (Scheets et al., 2021).
3 Opportunities
Current opportunities in the rehabilitation and recovery research field are to:
• Establish a standard definition of high-intensity aerobic exercise for stroke survivors.
• Determine the optimal timing to implement high-intensity aerobic exercise in stroke survivors: acute, subacute, chronic stroke?
• Determine if and how different modes of high-intensity exercise affect stroke survivors.
• Establish optimal exercise prescription parameters using FITT principles.
∘ Likely variable for each individual and may need to consider precision medicine.
Author contributions
SB: Conceptualization, Project administration, Writing – original draft, Writing – review & editing. RZ: Conceptualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We thank Amanda Britton-Carpenter for her assistance with the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Batacan, R. B., Duncan, M. J., Dalbo, V. J., Tucker, P. S., and Fenning, A. S. (2016). Effects of high-intensity interval training on cardiometabolic health: a systematic review and meta-analysis of intervention studies. Br. J. Sports Med. 51, 494–503. doi: 10.1136/bjsports-2015-095841
Billinger, S. A., Arena, R., Bernhardt, J., Eng, J. J., Franklin, B. A., Johnson, C. M., et al. (2014). Physical activity and exercise recommendations for stroke survivors: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 45, 2532–2553. doi: 10.1161/STR.0000000000000022
Boyne, P., Billinger, S. A., Reisman, D. S., Awosika, O. O., Buckley, S., Burson, J., et al. (2023). Optimal intensity and duration of walking rehabilitation in patients with chronic stroke: a randomized clinical trial. JAMA Neurol. 80, 342–351. doi: 10.1001/jamaneurol.2023.0033
Boyne, P., Dunning, K., Carl, D., Gerson, M., Khoury, J., and Kissela, B. (2013). High-intensity interval training in stroke rehabilitation. Topics Stroke Rehabilit. 20, 317–330. doi: 10.1310/tsr2004-317
Brouwer, R., Wondergem, R., Otten, C., and And Pisters, M. F. (2021). Effect of aerobic training on vascular and metabolic risk factors for recurrent stroke: a meta-analysis. Disab. Rehabilit. 43, 2084–2091. doi: 10.1080/09638288.2019.1692251
Costa, E. C., Hay, J. L., Kehler, D. S., Boreskie, K. F., Arora, R. C., Umpierre, D., et al. (2018). Effects of high-intensity interval training versus moderate-intensity continuous training on blood pressure in adults with pre-to established hypertension: a systematic review and meta-analysis of randomized trials. Sports Med. 48, 2127–2142. doi: 10.1007/s40279-018-0944-y
Feigin, V. L., Brainin, M., Norrving, B., Martins, S., Sacco, R. L., Hacke, W., et al. (2022). World Stroke Organization (WSO): global stroke fact sheet 2022. Int. J. Stroke 17, 18–29. doi: 10.1177/17474930211065917
Feito, Y., and Fountaine, C. (2022). “General Principles of Exercise Prescription,” in ACSM's Guidelines for Exercise Testing and Prescription, ed. G. Liguori (Alphen aan den Rijn: Wolters Kluwer).
Foster, C., Farland, C. V., Guidotti, F., Harbin, M., Roberts, B., Schuette, J., et al. (2015). The effects of high intensity interval training vs steady state training on aerobic and anaerobic capacity. J. Sports Sci. Med. 14:747. doi: 10.1249/01.mss.0000476771.63318.52
Henderson, C. E., Plawecki, A., Lucas, E., Lotter, J. K., Scofield, M., Carbone, A., et al. (2022). Increasing the amount and intensity of stepping training during inpatient stroke rehabilitation improves locomotor and non-locomotor outcomes. Neurorehabilit. Neural Repair 36, 621–632. doi: 10.1177/15459683221119759
Holleran, C. L., Straube, D. D., Kinnaird, C. R., Leddy, A. L., and Hornby, T. G. (2014). Feasibility and potential efficacy of high-intensity stepping training in variable contexts in subacute and chronic stroke. Neurorehab. Neural Repair 28, 643–651. doi: 10.1177/1545968314521001
Hornby, T. G., Holleran, C. L., Hennessy, P. W., Leddy, A. L., Connolly, M., Camardo, J., et al. (2016). Variable intensive early walking poststroke (VIEWS) a randomized controlled trial. Neurorehab. Neural Repair 30, 440–450. doi: 10.1177/1545968315604396
Hornby, T. G., Holleran, C. L., Leddy, A. L., Hennessy, P., Leech, K. A., Connolly, M., et al. (2015). Feasibility of focused stepping practice during inpatient rehabilitation poststroke and potential contributions to mobility outcomes. Neurorehab. Neural Repair 29, 923–932. doi: 10.1177/1545968315572390
Hornby, T. G., Reisman, D. S., Ward, I. G., Scheets, P. L., Miller, A., Haddad, D., et al. (2020). Clinical practice guideline to improve locomotor function following chronic stroke, incomplete spinal cord injury, and brain injury. J. Neurol. Phys. Ther. 44, 49–100. doi: 10.1097/NPT.0000000000000303
Hwang, C.-L., Yoo, J.-K., Kim, H.-K., Hwang, M.-H., Handberg, E. M., Petersen, J. W., et al. (2016). Novel all-extremity high-intensity interval training improves aerobic fitness, cardiac function and insulin resistance in healthy older adults. Exper. Gerontol. 82, 112–119. doi: 10.1016/j.exger.2016.06.009
Kleim, J. A., and Jones, T. A. (2008). Principles of experience-dependent neural plasticity: implications for rehabilitation after brain damage. J. Speech, Lang. Hear. Res. 51, S225–S239. doi: 10.1044/1092-4388(2008/018)
Mackay-Lyons, M., Billinger, S. A., Eng, J. J., Dromerick, A., Giacomantonio, N., Hafer-Macko, C., et al. (2020). Aerobic exercise recommendations to optimize best practices in care after stroke: AEROBICS 2019 update. Phys. Ther. 100, 149–156. doi: 10.1093/ptj/pzz153
Ramos, J. S., Dalleck, L. C., Tjonna, A. E., Beetham, K. S., and Coombes, J. S. (2015). The impact of high-intensity interval training versus moderate-intensity continuous training on vascular function: a systematic review and meta-analysis. Sports Med. 45, 679–692. doi: 10.1007/s40279-015-0321-z
Keywords: stroke, recovery, rehabilitation, intensity, exercise, walking, physical activity
Citation: Billinger SA and Zorowitz R (2024) Specialty grand challenge: intensive training. Front. Stroke 3:1412447. doi: 10.3389/fstro.2024.1412447
Received: 04 April 2024; Accepted: 08 April 2024;
Published: 26 April 2024.
Edited and reviewed by: Sean Isaac Savitz, University of Texas Health Science Center at Houston, United States
Copyright © 2024 Billinger and Zorowitz. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sandra A. Billinger, c2JpbGxpbmdlckBrdW1jLmVkdQ==; Richard Zorowitz, cmljaGFyZC56b3Jvd2l0ekBtZWRzdGFyLm5ldA==
 Sandra A. Billinger
Sandra A. Billinger Richard Zorowitz
Richard Zorowitz