- 1Department of Exercise Science and Recreation, CUNY Lehman College, New York, NY, United States
- 2The Human Performance Mechanic, New York, NY, United States
- 3The BFR PROS, New York, NY, United States
Introduction
Early training studies used single-chambered bladder tourniquets with arbitrary pressures (e.g., 100 mmHg) to study the impact of temporary blood flow restriction on muscle strength and hypertrophy (1, 2). Research since then has applied knowledge from medical tourniquet literature on factors that impact complete arterial occlusion including limb circumference, blood pressure, cuff shape and width, body positioning, and more (3, 4). Current practice recommendations indicate that personalizing the applied pressure (known as limb occlusion pressure, LOP) allows for a similar stimulus between participants in the same study and a better ability to compare different studies (5). Importantly, prescribing the pressure relative to the individual removes common methodological shortcomings and enhances safety (6). Literature indicates that the applied pressure used is an important methodological consideration given there appears to be a minimum amount of pressure (∼50% LOP) required to meaningfully accelerate muscular fatigue (7), a primary way BFR exerts its effect in practice. Therefore, it is crucial for BFR researchers and clinicians to point out BFR cuff features that may preclude LOP determination and the impact of such features on acute- and longitudinal outcomes of BFR.
In this manuscript, I discuss the challenges of a multi-chambered bladder design to the study of BFR exercise, focusing on the applied pressure prescriptions.
The multi-chambered cuff: missteps in the literature
The growing interest in BFR exercise has led to new features that clinicians and researchers can use to modulate limb blood flow. Altering the design of the air bladder that applies circumferential pressure to the underlying limb is a potentially important device feature. Traditional BFR cuff bladders are single-chambered, meaning when air is pumped into the cuff it exerts a largely equal circumferential pressure around the limb, permitting a measurement of relativized pressure (8).
Recently, manufacturers (e.g., BStrong, B3 Bands) introduced a multi-chambered cuff designed to avoid arterial occlusion for participant safety (9). The design largely prevents arterial occlusion (and, consequently, the ability to determine a personalized pressure) due to the gaps between the sequential bladders, which do not compress the underlying limb (8). Reducing arterial inflow during resting conditions with multi-chambered cuffs occurs only at very high set pressures (e.g., the pressure set by the BFR user) (> 350 mmHg) (10). Thus, when researchers overlook this important cuff design, it can lead to conclusions not supported by single-chambered cuffs applied at the same pressure. As this body of evidence grows (11–19), it is important to highlight methodological oversights to reduce the likelihood of these occurring in future studies and in practice.
Comparison of BFR cuff designs: impact on acute physiological and perceptual responses
Stray-Gunderson et al. (15) employed a short interval walking program (5 × 2 min at 3 mph) with bilateral Hokanson (single-chambered) or BStrong cuffs (multi-chambered) applied to the thighs. They determined that using a wide rigid Hokanson cuff (18 cm wide inflated to 160 mmHg) exacerbates the intra-exercise systolic blood pressure and double product (marker of myocardial demand) compared to the narrow elastic BStrong cuffs (5 cm wide) inflated to 300 mmHg. Additionally, the rating of perceived exertion and lactate release was significantly higher in the Hokanson condition whereas it was unchanged in the BStrong cuff condition. The authors concluded that the safety profile of BFR might be compromised with the Hokanson cuff and should be prescribed carefully.
However, it is perplexing that the authors did not attempt to relativize the pressure of the single-chambered cuff, especially considering the high usage of personalized pressures in practice (20) and the recommendations against arbitrary pressure use in research design (6). Although blood flow was not measured, the wide design of the Hokanson cuff and the inflation pressure would likely be near or exceed 100% LOP in most participants. For example, Hughes et al. (21) reported that a 13 cm-wide Hokanson [5 cm narrower than the cuff used in (15)] and reported that 163 mmHg was 100% LOP in their participant cohort (21). The use of such a wide cuff without determining a relativized pressure appears to have maximized the physiological stress of the exercise bout in the single-chambered cuff and elicit differences between cuffs. The BStrong cuffs behaved similarly to the low-intensity control exercise in most outcomes, except for a slightly greater increase in systolic blood pressure (15). This suggests the study may have been designed to favor the BStrong cuffs, as the widest cuffs recommended for practice (18 cm) (5) were applied with a higher-than-normal applied pressure in the Hokanson single-chambered cuff. Increased physiological demands are likely why low-intensity aerobic exercise with BFR is effective (22). As no longitudinal trials have investigated the impact of multi-chambered bladder cuffs on aerobic training outcomes, caution is warranted when extrapolating the effectiveness of aerobic exercise using cuffs with this feature, particularly given the limited acute physiological perturbations observed in the discussed study.
Bordessa et al. (11) compared muscle excitation and perceptual responses using the Delfi Personalized Tourniquet device (11.5 cm wide), applied at 80% LOP (∼152 mmHg), and the BStrong cuffs (5 cm wide), applied at ∼274 mmHg, during 30% 1RM leg extensions. These were compared against high-load control exercise at 80% 1RM. Across four fixed repetition sets (30-15-15-15), muscle excitation was similar between the BFR conditions, though both showed less excitation than high-load exercise. Additionally, the BStrong cuffs were perceived as less demanding than the Delfi Personalized Tourniquet, leading the authors to suggest that BStrong cuffs may be preferable in practice. However, it is well established that load, rather than applied pressure, is the primary driver of muscle excitation (23), so conditions exercising at a similar percentage of the one-rep max should produce comparable muscular excitation. Moreover, muscle excitation is not a reliable surrogate for hypertrophic potential during low-load exercise performed to high levels of voluntary effort as any low-intensity condition nearing failure is likely to produce similar long-term benefits, regardless of the BFR application (24). It is possible that participants using the BStrong cuffs were further from muscular failure compared to those using the Delfi cuffs, which may have led to lower perceived exertion despite the differing cuff pressures. This aligns with evidence that closer proximity to failure increases perceptual demands (25).
It is highly likely that the interface pressure (e.g., the pressure applied to the limb from the cuff) of the BStrong cuffs was significantly lower than that of the Delfi Personalized Tourniquet, despite differences in set pressures. This may also explain the higher perceptual demands, as pressure can modulate perceptual response (23). While both cuffs facilitate BFR exercise, the multi-chambered system modulates blood flow during resting conditions at pressures exceeding 350 mmHg, whereas the single-chambered cuff may require as little as 83 mmHg to achieve comparable effects (10).
It's important to note that the pressure applied with a multi-chambered cuff is not the same as the pressure applied to the underlying limb, as seen in traditional single-chambered cuffs (9, 26). This is a result of the multi-chambered design, where the set pressure does not directly correlate with the interface pressure (26). In fact, the multi-chambered system ensures that the device is unable to provide arterial occlusion even at pressures as high as 500 mmHg (9). Since no longitudinal studies exist using a multi-chambered cuff with fixed repetition schemes, it remains unclear whether the lower interface pressures would elicit meaningful hypertrophy compared to low-load exercise alone or BFR applied with a single-chambered cuff. This represents a critical area for future research, especially given the manufacturer's emphasis on safety, which may come at the cost of reduced effectiveness in BFR exercise due to the cuff's inability to sufficiently modulate blood flow compared to single-chambered cuffs.
Misapplying algorithms meant for single-chambered cuffs while using multi-chambered cuffs
In 2014, Loenneke et al. introduced an algorithm based on thigh circumference using 5 cm wide elastic and nylon BFR cuffs to determine a ballpark estimate percentage of LOP without a doppler ultrasound or other automatic computer-based tourniquets (27). This algorithm is supposed to be applied when using cuffs of similar widths and bladder design to enhance the validity of application and ensure a sub occlusive BFR stimulus.
However, as BFR research has grown, researchers have begun to apply this algorithm inappropriately by not considering the impact of the bladder design on arterial occlusive capabilities (16, 19, 28). This is important from a methodological perspective because the interface pressure will be significantly less in the multi-chamber BFR cuff due to the bladder design despite a similar set pressure, potentially leading to conclusions or effects that differ when the same applied pressure is implemented with a single-chambered BFR cuff.
Wang et al. (16) and Zhang et al. (19) used Loenneke's limb circumference algorithm to determine restrictive pressure application, reporting average pressures between 180 and 260 mmHg using the BStrong cuffs (16, 19). Both studies demonstrated that adding BFR to high-load exercise and vibration training improved sports performance. However, the application of pressures in the range of 180-260 mmHg, particularly with multi-chambered systems like BStrong cuffs, may not produce the same level of blood flow restriction as single-chambered cuffs. The multi-chambered design likely results in lower interface pressures, potentially creating a compression-like effect rather than inducing true blood flow restriction (10, 29). It is important to note that blood flow modulation was not measured in these studies, limiting the ability to fully understand the exercise-induced effects of the applied pressure. While this compression may still enhance performance, it may not provide the same physiological stimulus as BFR using single-chambered cuffs, particularly regarding metabolic stress and occlusion-induced adaptations. If similar pressures were applied with a single-chambered cuff, it is likely that the response would differ, potentially reaching supra-occlusive levels. Future research should consider the impact of cuff design when determining applied pressure and prioritize the use of single-chambered cuffs when employing limb circumference algorithms to ensure a more consistent and effective BFR stimulus.
Not considering pressure-dependent relationships when using multi-chambered cuffs
Research investigating pressure-dependent relationships in blood flow restriction has yielded mixed findings. Some studies suggest that arterial inflow is reduced in a non-linear fashion between 30 and 80% LOP in the brachial and superficial femoral arteries (30, 31), while others have found a more linear relationship in the posterior tibial artery (32). Despite these mixed results, it remains crucial to examine how pressure impacts the acute responses to BFR exercise. Single-chambered cuffs allow for a personalized, relativized pressure that can be tailored to everyone based on their LOP, ensuring a more consistent and effective BFR stimulus. The ability to adjust pressure to individual needs enhances the translation of research findings into practical applications. In contrast, multi-chambered cuffs such as BStrong cannot determine personalized pressure, as they do not significantly modulate blood flow from resting conditions unless very high pressures (>350 mmHg) are applied (10). This limitation reduces the ability to establish clear pressure-dependent relationships with this cuff design. Therefore, when studying pressure-dependent responses, single-chambered cuffs should be prioritized for their precision and the improved safety and efficacy they offer in BFR practice.
While single-chambered cuffs provide more precise pressure modulation and a clearer understanding of pressure-dependent responses, studies using multi-chambered cuffs like BStrong have begun to explore these relationships despite their inherent limitations. One such study by Jia et al. (13) investigated the pressure-dependent relationship of cerebral oxygenation levels following bilateral BFR squatting exercise using BStrong cuffs applied at pressures of 150, 200, 250, 300, and 350 mmHg. The authors found that cerebral oxygenation levels dropped sharply only at 350 mmHg. Based on this, they concluded that moderate applied pressures (150-250 mmHg) induced the most favorable acute responses in the cerebral cortex and should be used in BFR exercise. This recommendation was based on their observation that optimal cerebral activation and functional connectivity occurred at pressures between 150 and 250 mmHg, whereas 350 mmHg caused a significant decrease in oxygenated hemoglobin levels, indicating reduced cerebral blood flow. These results suggest that higher pressures, such as 350 mmHg, may lead to excessive restriction, reducing oxygenation and potentially diminishing the benefits of cerebral activation, which is crucial for neural adaptation during training.
However, it should be noted that in a separate study, 350 mmHg was the first pressure shown to modulate blood flow from resting conditions in the lower extremities with a multi-chambered cuff, achieving a similar effect to 40% LOP in a single-chambered cuff—the minimum recommended relativized pressure for BFR exercise (5, 10). While it might be tempting to equate 350 mmHg with 40% LOP due to their similar effects on blood flow reduction from resting conditions, without standardizing pressure relative to the individual, such comparisons remain speculative.
Additionally, given the existing knowledge on multi-chambered cuffs, the results of this study cannot be extrapolated to single-chambered cuffs. Applying the level of “moderate pressure” recommended by Jia et al. (13) in a single-chambered cuff would most certainly result in supra-occlusive pressure in most participants. Moreover, the multi-chambered bladder cuff is a poor choice to study pressure-dependent relationships in BFR exercise as it is designed to reduce the likelihood of arterial occlusion, not to function as a tourniquet (9). Thus, the results of Jia et al. (13) do not inform clinicians about how pressure impacts cerebral oxygenation responses when using more commonly applied single-chambered bladder BFR cuffs inflated to recommended 40%–80% LOP—especially as the only applied pressure that significantly impacted cerebral oxygenation was the minimum pressure that altered arterial blood flow from resting conditions (40% LOP) (10). Future research in this area should strongly consider how bladder design impacts restrictive capabilities, particularly if the desired response is a reduction in arterial blood flow.
Conclusions and future directions
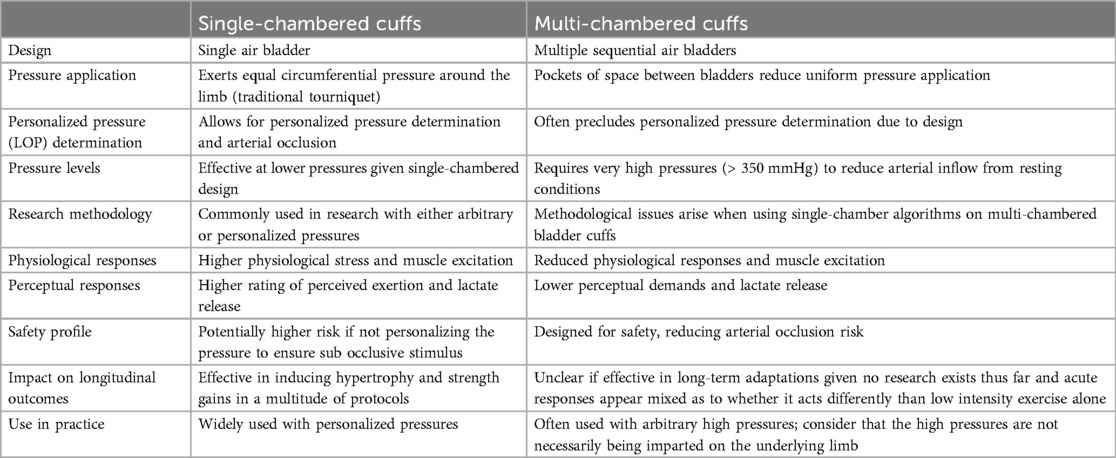
The current body of literature on multi-chambered BFR cuffs has several methodological oversights that can be addressed in future studies by taking the multi-chambered bladder design into account (Table 1). Given multi-chambered bladder cuffs are unlikely to fully occlude arterial blood flow, they are inherently unable to determine a personalized pressure, which significantly limits their ability to offer the same precision as single-chambered cuffs. As of mid-2024, no longitudinal studies have compared the chronic adaptive responses to fixed repetition schemes using multi-chambered cuffs, which would typically outperform low-intensity exercise when based upon the findings from single-chambered BFR cuffs. Therefore, while acute responses appear significantly diminished with multi-chambered BFR cuffs compared to single-chambered BFR cuffs, it remains unknown whether the long-term adaptations would differ. Understanding the impact of BFR cuff features, especially the limitations of multi-chambered cuffs in personalizing pressure, will be critical for advancing research and improving study designs. This will also better inform populations implementing multi-chambered BFR cuffs in their exercise routines.
Author contributions
NR: Writing – original draft, Writing – review & editing.
Funding
The author declares that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
NR is the founder of THE BFR PROS, a BFR education company that provides BFR training workshops to fitness and rehabilitation professionals across the world using a variety of BFR devices.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Shinohara M, Kouzaki M, Yoshihisa T, Fukunaga T. Efficacy of tourniquet ischemia for strength training with low resistance. Eur J Appl Physiol Occup Physiol. (1998) 77(1–2):189–91. doi: 10.1007/s004210050319
2. Takarada Y, Takazawa H, Sato Y, Takebayashi S, Tanaka Y, Ishii N. Effects of resistance exercise combined with moderate vascular occlusion on muscular function in humans. J Appl Physiol. (2000) 88(6):2097–106. doi: 10.1152/jappl.2000.88.6.2097
3. Graham B, Breault MJ, McEwen JA, McGraw RW. Occlusion of arterial flow in the extremities at subsystolic pressures through the use of wide tourniquet cuffs. Clin Orthop Relat Res. (1993) 286(286):257–61.
4. Hughes L, Jeffries O, Waldron M, Rosenblatt B, Gissane C, Paton B, et al. Influence and reliability of lower-limb arterial occlusion pressure at different body positions. PeerJ. (2018) 2018:5. doi: 10.7717/peerj.4697
5. Patterson SD, Hughes L, Warmington S, Burr J, Scott BR, Owens J, et al. Blood flow restriction exercise position stand: considerations of methodology, application, and safety. Front Physiol. (2019) 10(MAY):533. doi: 10.3389/fphys.2019.00533
6. Jessee MB, Buckner SL, Mouser JG, Mattocks KT, Loenneke JP. Letter to the editor: applying the blood flow restriction pressure: the elephant in the room. Am J Physiol Heart Circ Physiol. (2016) 310(1):H132–3. doi: 10.1152/ajpheart.00820.2015
7. Cerqueira MS, Lira M, Mendonça Barboza JA, Burr JF, Wanderley E, Lima TB, et al. Repetition failure occurs earlier during low-load resistance exercise with high but not low blood flow restriction pressures: a systematic review and meta-analysis. J Strength Cond Res. (2021). Publish Ahead of Print. doi: 10.1519/JSC.0000000000004093
8. Rolnick N, Kimbrell K, de Queiros V. Beneath the cuff: often overlooked and under-reported blood flow restriction device features and their potential impact on practice. Front Physiol. (2023) 14:1089065. doi: 10.3389/fphys.2023.1089065
9. Safety. (n.d.). BStrong. Available online at: https://bstrong.training/pages/safety (Accessed September 23, 2024).
10. Citherlet T, Willis SJ, Chaperon A, Millet GP. Differences in the limb blood flow between two types of blood flow restriction cuffs: a pilot study. Front Physiol. (2022) 13:931270. doi: 10.3389/fphys.2022.931270
11. Bordessa J. M., Hearn M. C., Reinfeldt A. E., Smith T. A., Baweja H. S., Levy S. S., Rosenthal M. D. (2021). Comparison of blood flow restriction devices and their effect on quadriceps muscle activation. Phys Ther Sport, 49(MAY), 90–7. doi: 10.1016/j.ptsp.2021.02.005
12. Dancy ME, Alexander AS, Abbas MJ, Rolnick N, Alder KD, Lu Y, et al. No differences in exercise performance, perceptual response, or safety were observed among 3 blood flow restriction devices. Arthrosc Sports Med Rehabil. (2023) 5(6):100822. doi: 10.1016/j.asmr.2023.100822
13. Jia B, Lv C, Li D, Lv W. Cerebral cortex activation and functional connectivity during low-load resistance training with blood flow restriction: an fNIRS study. PLoS One. (2024) 19(5):e0303983. doi: 10.1371/journal.pone.0303983
14. Machek SB, Harris DR, Zawieja EE, Heileson JL, Wilburn DT, Radziejewska A, et al. The impacts of combined blood flow restriction training and betaine supplementation on one-leg press muscular endurance, exercise-associated lactate concentrations, serum metabolic biomarkers, and hypoxia-inducible factor-1α gene expression. Nutrients. (2022) 14(23):5040. doi: 10.3390/nu14235040
15. Stray-Gundersen S, Wooten S, Tanaka H. Walking with leg blood flow restriction: wide-rigid cuffs vs. Narrow-elastic bands. Front Physiol. (2020) 11:568. doi: 10.3389/fphys.2020.00568
16. Wang J, Fu H, Zhang Q, Zhang M, Fan Y. Effect of leg half-squat training with blood flow restriction under different external loads on strength and vertical jumping performance in well-trained volleyball players. Dose-Response: A Publication of International Hormesis Society. (2022) 20(3):15593258221123672. doi: 10.1177/15593258221123673
17. Wooten SV, Stray-Gundersen S, Tanaka H. Hemodynamic and pressor responses to combination of yoga and blood flow restriction. Int J Sports Med. (2020) 41(11):759–65. doi: 10.1055/a-1171-1620
18. Wooten SV, Wolf JS Jr, Mendoza D, Bartholomew JB, Stanforth PR, Stanforth D, et al. The impact of a multimodal sport science-based prehabilitation program on clinical outcomes in abdominal cancer patients: a cohort study. Am Surg. (2022) 88(9):2302–08. doi: 10.1177/00031348221103657
19. Zhang J, Zhou R, Zhao N, Li Y, Liu H, Zhang W, et al. Acute effects of blood flow restriction with whole-body vibration on sprint, muscle activation and metabolic accumulation in male sprinters. Front Physiol. (2023) 14:1149400. doi: 10.3389/fphys.2023.1149400
20. Scott BR, Marston KJ, Owens J, Rolnick N, Patterson SD. Current implementation and barriers to using blood flow restriction training: insights from a survey of allied health practitioners. J Strength Cond Res. (2023) 38(3):481–90. doi: 10.1519/JSC.0000000000004656
21. Hughes L, Rosenblatt B, Gissane C, Paton B, Patterson SD. Interface pressure, perceptual, and mean arterial pressure responses to different blood flow restriction systems. Scand J Med Sci Sports. (2018a) 28(7):1757–65. doi: 10.1111/sms.13092
22. Formiga MF, Fay R, Hutchinson S, Locandro N, Ceballos A, Lesh A, et al. Effect of aerobic exercise training with and without blood flow restriction on aerobic capacity in healthy young adults: a systematic review with meta-analysis. Int J Sports Phys Ther. (2020) 15(2):175–87. doi: 10.26603/ijspt20200175
23. Loenneke JP, Kim D, Fahs CA, Thiebaud RS, Abe T, Larson RD, et al. The effects of resistance exercise with and without different degrees of blood-flow restriction on perceptual responses. J Sports Sci. (2015) 33(14):1472–9. doi: 10.1080/02640414.2014.992036
24. Morton RW, Sonne MW, Farias Zuniga A, Mohammad IYZ, Jones A, McGlory C, et al. Muscle fibre activation is unaffected by load and repetition duration when resistance exercise is performed to task failure. J Physiol (Lond). (2019) 597(17):4601–13. doi: 10.1113/JP278056
25. Refalo MC, Helms ER, Hamilton DL, Fyfe JJ. Influence of resistance training proximity-to-failure, determined by repetitions-in-reserve, on neuromuscular fatigue in resistance-trained males and females. Sports Med Open. (2023) 9(1):10. doi: 10.1186/s40798-023-00554-y
26. Hughes L, Swain PM, Lai T, McEwen JA. It's time to regulate – the importance of accurate surgical-grade tourniquet autoregulation in blood flow restriction exercise applications. Phys Ther Sport. (2024) 67:41–46. doi: 10.1016/j.ptsp.2024.02.001
27. Loenneke J, Thiebaud RS, Fahs CA, Rossow LM, Abe T, Bemben MG. Blood flow restriction: effects of cuff type on fatigue and perceptual responses to resistance exercise. Acta Physiol Hung. (2014) 101(2):158–66. doi: 10.1556/APhysiol.101.2014.2.4
28. Zhang J, Ye J, Liu H. Acute effects of low-intensity resistance combined with blood flow restriction and high-intensity resistance exercise on lower extremity explosive strength, pennation angle and muscle-tendon stiffness in male sprinters. In Research Square. [Preprint] (2024). Available online at: https://assets-eu.researchsquare.com/files/rs-3952436/v1/e4b954e7-b984-4cf7-812c-90f66bad331a.pdf?c=1718895858 (Accessed September 01, 2024).
29. Rolnick N, Kamis O. Important methodological concern regarding the article “effect of leg half-squat training with blood flow restriction under different external loads on strength and vertical jumping performance in well-trained volleyball players”: a letter to the editor. Dose Response. (2023) 21(2):155932582311734. doi: 10.1177/15593258231173494
30. Crossley KW, Porter DA, Ellsworth J, Caldwell T, Feland JB, Mitchell U, et al. Effect of cuff pressure on blood flow during blood flow-restricted rest and exercise. Med Sci Sports Exercise. (2020) 52(3):746–53. doi: 10.1249/MSS.0000000000002156
31. Mouser JG, Ade CJ, Black CD, Bemben DA, Bemben MG. Brachial blood flow under relative levels of blood flow restriction is decreased in a nonlinear fashion. Clin Physiol Funct Imaging. (2018) 38(3):425–30. doi: 10.1111/cpf.12432
Keywords: Delfi, multi-chambered, resistance training, limb occlusion pressure, BStrong, B3 Bands
Citation: Rolnick N (2024) Unpacking the blood flow restriction device features literature: multi-chambered bladder design. Front. Sports Act. Living 6:1457539. doi: 10.3389/fspor.2024.1457539
Received: 15 July 2024; Accepted: 27 September 2024;
Published: 10 October 2024.
Edited by:
Francis Degache, Université de Lausanne, SwitzerlandReviewed by:
Stuart Warmington, Deakin University, AustraliaCopyright: © 2024 Rolnick. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nicholas Rolnick, bnJvbG5pY2tAZ21haWwuY29t
†ORCID:
Nicholas Rolnick
orcid.org/0000-0003-0430-5015
 Nicholas Rolnick
Nicholas Rolnick