- 1Department of Kinesiology and Public Health, Biola University, La Mirada, CA, United States
- 2Department of Biological Sciences, Biola University, La Mirada, CA, United States
- 3Department of Chemistry, Physics, and Engineering, Biola University, La Mirada, CA, United States
- 4Department of Mathematics and Computer Science, Biola University, La Mirada, CA, United States
Since the outset of the COVID-19 pandemic, the global healthcare community has faced the challenge of understanding and addressing the ongoing and multi-faceted SARS-CoV-2 infection outcomes. As millions of individuals worldwide continue to navigate the complexities of post-hospitalization recovery, reinfection rates, and the increasing prevalence of Long-COVID symptoms, comprehensive COVID-19 rehabilitation strategies are greatly needed. Previous studies have highlighted the potential synergy between exercise and nutrition, suggesting that their integration into patient rehabilitation programs may yield improved clinical outcomes for survivors of COVID-19. Our group aimed to consolidate existing knowledge following the implementation of patient, intervention, comparison, and outcome (PICO) search strategies on the distinct and combined impacts of exercise and nutrition interventions in facilitating the recovery of COVID-19 patients following hospitalization, with a specific focus on their implications for both public health and clinical practice. The incorporation of targeted nutritional strategies alongside exercise-based programs may expedite patient recovery, ultimately promoting independence in performing activities of daily living (ADLs). Nonetheless, an imperative for expanded scientific inquiry remains, particularly in the realm of combined interventions. This mini-review underscores the compelling prospects offered by an amalgamated approach, advocating for the seamless integration of exercise and nutrition as integral components of post-hospitalization COVID-19 rehabilitation. The pursuit of a comprehensive understanding of the synergistic effects and effectiveness of exercise and nutrition stands as a crucial objective in advancing patient care and refining recovery strategies in the wake of this enduring global health crisis.
1. Introduction
Since initial cases were identified in November 2019, the global healthcare community has contended with the relentless challenge posed by the coronavirus disease (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (1). By some reports, COVID-19 has become endemic (2), however, recent statistics paint a sobering picture. Approximately 4.5 million new cases and 32,000 deaths occurred between February 6th and March 5th, 2023 (3). As of March 5th, 2023, a staggering 759 million confirmed cases and 6.8 million deaths have been reported worldwide, emphasizing the enduring need for public health and medical interventions (3). As COVID-19 transitions into an endemic disease, the inevitable consequence of a growing survivor population has become apparent.
An increasing number of adults, regardless of vaccination status, have been contending with an array of lingering symptoms and post-acute conditions collectively known as post-COVID conditions, long-haul COVID, or more commonly noted as long-term COVID (4); more so in older adults, ages 65 and older (5). While symptom severity varies, most patients encounter the triad of coughing, fever, and fatigue, often accompanied by anosmia, headaches, myalgia, congestion, rhinorrhea, dyspnea, vomiting, or diarrhea, which may worsen a week or more after onset (6). Persistent symptoms lasting longer than four weeks following diagnosis, and some suffering effects for greater than two years have been reported (7). While some COVID-based physical rehabilitation studies exist to address these issues, to our knowledge, no studies have examined the implementation of exercise and nutritional interventions in a COVID rehabilitation model. Thus, the purposes of this mini-review were: (1) to evaluate and synthesize existing knowledge regarding the pivotal role of exercise or nutritional interventions for COVID patients, and (2) to propose COVID rehabilitation modeling which includes a combination of exercise and nutritional interventions aimed at optimal recovery, physical well-being, and improved quality of life (QOL). Search strategies employed by our group followed the patient, intervention, comparison, and outcome (PICO) model (Supplementary Table S1) (8).
2. Impact of COVID-19 on patients’ health and significance of rehabilitation
Hospitalized or recovering patients may experience substantial mental health challenges directly from the disease, which often overlap with physical challenges, and then contribute to the overall complexity of psychological well-being (9, 10). Hospitalization, isolation, and uncertainty in severe illness can precipitate mental health challenges or post-traumatic stress disorder (PTSD)-like symptoms (11–13), cognitive disorders, memory lapses, and difficulties in concentrating (14). Immunological dysregulation (15), ongoing inflammatory conditions (16, 17), and organ system dysfunction have been linked to symptom persistence (18). Persistent anxiety and depression may result from the uncertainties surrounding the illness, isolation, and exposure to illness and mortality (19). Cognitive challenges, described as brain fog, may further complicate recovery (20). Rehabilitation for patients who continue to experience lingering symptoms is paramount as it may vitally impact the recovery process by improving outcomes, reducing complications, and enhancing overall QOL (21). Muscle weakness, decreased mobility, and reduced functional capacity have been highlighted as a consequence of prolonged bed rest and the catabolic effects of the virus (22). Persistent fatigue further exacerbates the challenges faced by patients, hampering their ability to engage in daily activities and threatening overall QOL (23, 24). Additionally, the virus's potential to influence the development of novel health conditions, such as metabolic and cardiovascular issues, adds another layer of complexity to the rehabilitation process (25). The Stanford-Hall consensus statement for post-COVID rehabilitation, while initially targeting active individuals, has provided a valuable rehabilitative framework for addressing the major health challenges faced by COVID-19 patients (25). However, nutritional interventions were notably absent from this consensus, leaving an important aspect of recovery unaddressed.
3. Exercise in COVID-19 rehabilitation
Human movement, whether by physical activity or exercise, has been long established in the literature for the wide array of health benefits and for the reduction of risks of developing chronic health disorders or disease states. Ruegsegger and Booth (2018), in a review of the literature, reported that lifelong exercise is associated with the delayed onset of approximately 40 different diseases in addition to the extenuation of lifespan (26). Numerous studies have demonstrated improvements in cardiovascular and cardiorespiratory function (27–29), improvements in mental health and QOL (30–34), and improvements in blood parameters, mitochondrial function, and metabolic conditions (35–38).
Contemporary rehabilitation strategies have been developed and implemented for large-scale health conditions such as cancer and cardiovascular disease according to phase-based standard-of-care models (39, 40). Both follow progressively similar trajectories often initiating in the in-patient setting to address medical or surgical issues with goals of referring patients toward prescriptive out-patient rehabilitation programs. Assessment and screening procedures guide patient allocation toward addressing specific needs of symptom reduction and improvements in functional capacity. Then, as patient progress and physiological improvement occurs, exercise interventions advance through additional phase increases resulting in an individual maintaining healthy active living and independence at the completion of the final phase (41). Comparitively, phase-based cancer rehabilitation modeling may be more appropriate because of the greater expectance of a wide array of known cancer treatment-related side effects such as chemotherapy-related cognitive impairment, balance and coordination disorders, fatigue, muscle and joint pain, depression, reductions in QOL, urinary or gastrointestinal disorders, thrombocytoppenia, integumentary system disorders, neuropathic conditions, cardiorespiratory conditions, fertility issues, and edema (42, 43).
4. Nutrition in COVID-19 rehabilitation
Infection susceptibility and advanced disease severity have been linked to a number of risk factors including male gender, advanced age, obesity, type-II diabetes diagnoses, poor diet, under-represented population groups, and pro-inflammatory conditions (44, 45). Butler and Barrientos (2020) suggested that highly processed diets composed of high fat and carbohydrate content, low fiber foods may play a significant role in not only association with risk factors but also with negative impacts on innate and adaptive immunological function (46). Excessive dietary sodium and alcohol in addition to deficiencies in vitamin D may also negatively predispose an individual to be at greater risk for infection and greater severity of the disease (47). Yet, Downer, Berkowitz, Harlan, Olstad, and Mozaffarian, et al. (2020) suggest that targeted nutritional interventions have a significant role in the treatment, prevention, management, and reversal of some diseases (48). As it relates directly to COVID-19, Tsagari, Risvas, Papathanasiou, and Dionyssiotis (2022) specifically noted that patients are more prone to sarcopenia and malnutrition due to multiple nutritional and metabolic factors that may result in decreases in immune function, decreases in respiratory and swallowing function, and reductions in resilience to metabolic stress. Yet, a consensus would indicate that obtaining macro- and micronutrients in proper concentrations is conducive to overall health and well-being (49).
5. The synergy of exercise and nutrition
Adequate nutrition necessary for healthy human function has been demonstrated to support immunological function, organ health, and functioning, prolong lifespans, and decrease risks for diseases such as diabetes and some cancers (50). In addition to the benefits of exercise during patient rehabilitation, adequate nutrition complements positive outcomes and provides potential synergistic strength when they are utilized in combination (Table 1). Given the abundance of evidence supporting the positive impacts of exercise or nutrition alone, the combined exercise and nutrition theoretical construct synergizes both for potentially additive effects. Yet, research is often convoluted and challenging to conduct because of the many different factors presented herein. Thus, our group strongly advocates for increased research in this area with the hopes that ultimately, these investigative efforts may lead to wide-scale development and implementation of standardized exercise and nutrition programs that are targeted toward the individual needs of patients recovering from COVID-19.
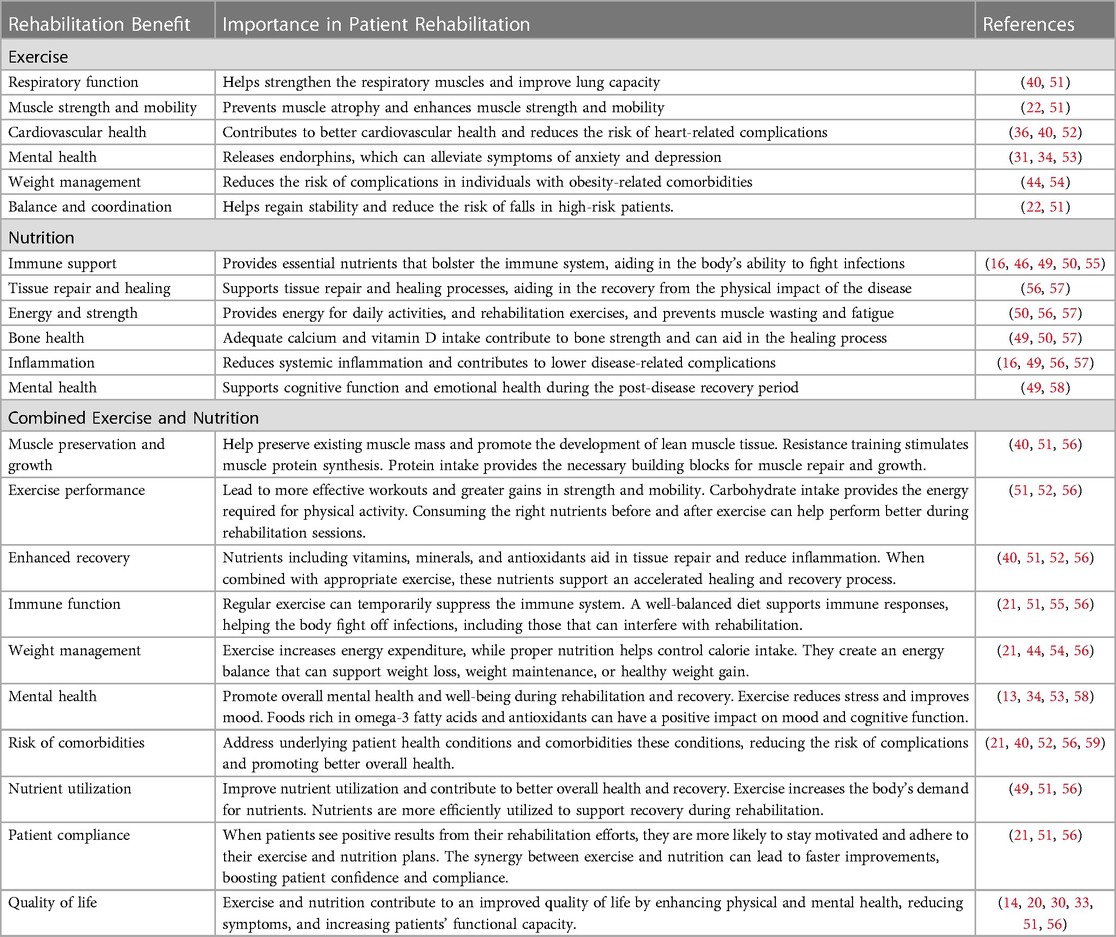
Table 1. Benefits of exercise, nutrition, and their synergistic effects during patient rehabilitation and recovery.
Patient education on diet and exercise may also substantially impact COVID-19 rehabilitation by accelerating the return to functional capacity by empowering individuals to take an active role in their recovery. A combined holistic approach that integrates targeted exercise regimens with nutritional guidance may provide additional effectiveness. Nutritional interventions support the healing process, enhance energy levels, and aid in muscle recovery, complementing the benefits of physical rehabilitation (60). Emphasizing the importance of exercise and nutrition in rehabilitation, may reduce the long-term burdens of COVID-19 and help patients regain their independence and overall well-being.
6. Discussion
The implementation of combined exercise and nutritional interventions in a hospitalized setting for patients with COVID-19 presents with several challenges (Figure 1). COVID-19 not only affects the respiratory system but also leads to muscle weakness, deconditioning, and nutritional deficiencies due to prolonged illness and reduced food intake. Integrating exercise and nutrition therapies is crucial for addressing both the respiratory and musculoskeletal aspects of recovery. Such an approach not only enhances physical function but also supports mental and emotional well-being during the long recovery process. One significant obstacle is ensuring patient compliance, particularly in cases of severe illness or limited mobility. Patients may experience discomfort or fatigue, making it difficult to engage in exercise routines. Additionally, resource limitations in healthcare facilities, such as a shortage of qualified personnel, equipment, or dedicated spaces for exercise, can hinder program implementation. Overcoming these challenges requires a multifaceted approach with a multidisciplinary team who are trained and equipped to address this disease from the acute phase throughout active recovery and return to apparently healthy functional status. Clinical exercise physiologists, physiotherapists, dietitians, occupational therapists, and statisticians working alongside physicians, nurses, and specialists play essential roles in the assessment, development, monitoring, and in-depth analytical evaluations of programmatic implementation specifically targeting patient-specific needs and conditions throughout the continuum of care. Personalized expert guidance may increase the likelihood of intervention adherence.
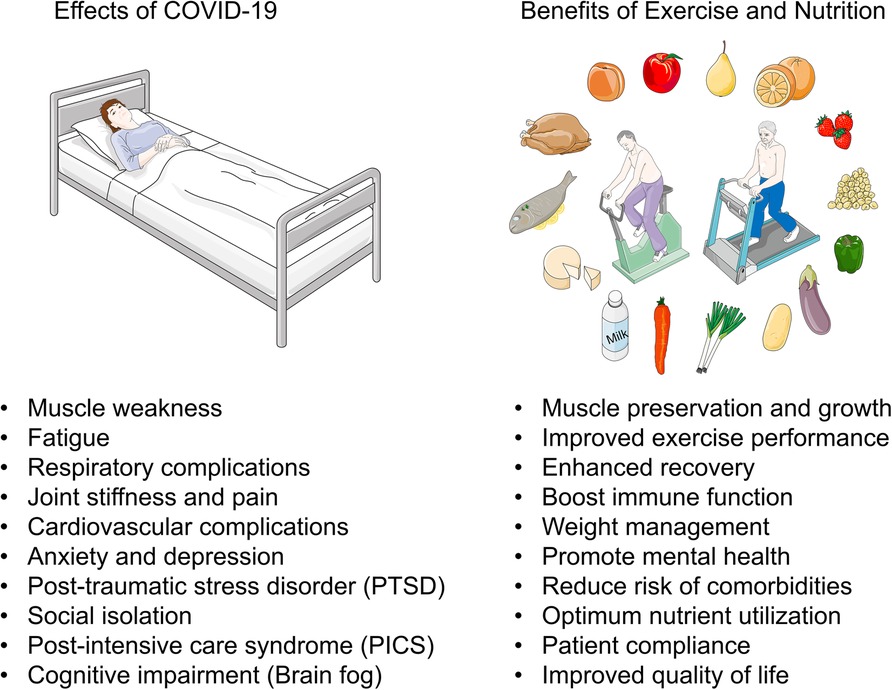
Figure 1. Benefits of exercise and nutritional interventions for patients hospitalized with COVID-19. Patients hospitalized with COVID-19 may experience symptoms including, muscle weakness, fatigue, respiratory complications, joint stiffness and pain, cardiovascular complications, anxiety and depression, post-traumatic stress disorder (PTSD), social isolation, post-intensive care syndrome (PICS), and cognitive impairment (brain fog). Incorporating exercise and nutritional interventions during patient rehabilitation could elicit synergistic benefits including, muscle preservation and growth, improved exercise performance, enhanced recovery, boost immune function, weight management, promote mental health, reduce risk of comorbidities, optimum nutrient utilization, patient compliance, and improved quality of life. This figure utilizes images available at Servier Medical Art, licensed under a Creative Commons Attribution 3.0 Unported License.
As we continue to navigate the complex landscape of rehabilitation for hospitalized patients, especially those with COVID-19, there are promising avenues for future health education, research, and innovative methodologies to address disease risk, infection, hospitalization, recovery, and rehabilitation. Investigating the optimal timing and intensity of exercise interventions, along with personalized nutrition plans, can further improve patient outcomes. The integration of technology, such as telehealth platforms and wearable telemetric devices, may facilitate remote monitoring and enhance patient engagement. Moreover, research should explore the long-term effects of combined exercise and nutrition therapy on reducing the risk of readmission, improving overall quality of life, and addressing potential comorbidities associated with sarcopenia and malnutrition.
The successful implementation of exercise and nutrition programs in a hospital setting, particularly for patients recovering from severe illnesses like COVID-19, necessitates a comprehensive strategy. Overcoming patient compliance issues, and resource constraints, and ensuring a multidisciplinary approach are critical steps. Future research endeavors and innovative approaches should aim to refine these interventions, ultimately leading to better patient outcomes and improved healthcare delivery.
Author contributions
BP: Conceptualization, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. IU: Formal Analysis, Investigation, Resources, Writing – review & editing. SS: Conceptualization, Data curation, Investigation, Methodology, Resources, Writing – review & editing. J-YP: Investigation, Methodology, Project administration, Writing – review & editing. JK: Conceptualization, Methodology, Project administration, Writing – review & editing. RG: Conceptualization, Methodology, Project administration, Supervision, Writing – review & editing. JW: Formal Analysis, Methodology, Supervision, Writing – review & editing. TG: Conceptualization, Data curation, Investigation, Methodology, Supervision, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fspor.2023.1305175/full#supplementary-material
References
1. WHO. Coronavirus disease (COVID-19). (2023). Available at: https://www.who.int/health-topics/coronavirus#tab=tab_1
2. Biancolella M, Colona VL, Mehrian-Shai R, Watt JL, Luzzatto L, Novelli G, et al. COVID-19 2022 update: transition of the pandemic to the endemic phase. Hum Genomics. (2022) 16(1):19. doi: 10.1186/s40246-022-00392-1
3. WHO. Weekly epidemiological update on COVID-19. (2023). Available at: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---8-march-2023
4. Soriano JB, Murthy S, Marshall JC, Relan P, Diaz JV. A clinical case definition of post-COVID-19 condition by a delphi consensus. Lancet Infect Dis. (2022) 22(4):e102–e7. doi: 10.1016/S1473-3099(21)00703-9
5. Mayo_Clinic. COVID-19: long-term effects. (2022). Available at: https://www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/coronavirus-long-term-effects/art-20490351
6. Sharma A, Ahmad Farouk I, Lal SK. COVID-19: a review on the novel coronavirus disease evolution, transmission, detection, control and prevention. Viruses. (2021) 13(2):202. doi: 10.3390/v13020202
7. Zarei M, Bose D, Nouri-Vaskeh M, Tajiknia V, Zand R, Ghasemi M. Long-term side effects and lingering symptoms post COVID-19 recovery. Rev Med Virol. (2022) 32(3):e2289. doi: 10.1002/rmv.2289
8. Schardt C, Adams MB, Owens T, Keitz S, Fontelo P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med Inform Decis Mak. (2007) 7(1):16. doi: 10.1186/1472-6947-7-16
9. Penninx B, Benros ME, Klein RS, Vinkers CH. How COVID-19 shaped mental health: from infection to pandemic effects. Nat Med. (2022) 28(10):2027–37. doi: 10.1038/s41591-022-02028-2
10. Galbadage T, Peterson BM, Wang DC, Wang JS, Gunasekera RS. Biopsychosocial and spiritual implications of patients with COVID-19 dying in isolation. Front Psychol. (2020) 11:588623. doi: 10.3389/fpsyg.2020.588623
11. Cortés Zamora EB, Mas Romero M, Tabernero Sahuquillo MT, Avendaño Céspedes A, Andrés-Petrel F, Gómez Ballesteros C, et al. Psychological and functional impact of COVID-19 in long-term care facilities: the COVID-A study. Am J Geriatr Psychiatry. (2022) 30(4):431–43. doi: 10.1016/j.jagp.2022.01.007
12. Walecka I, Ciechanowicz P, Dopytalska K, Mikucka-Wituszyńska A, Szymańska E, Bogucki J, et al. Psychological consequences of hospital isolation during the COVID-19 pandemic—research on the sample of Polish firefighting academy students. Curr Psychol. (2023) 42(8):6856–65. doi: 10.1007/s12144-021-01982-3
13. Serra R, Borrazzo C, Vassalini P, Di Nicolantonio C, Koukopoulos AE, Tosato C, et al. Post-traumatic stress disorder trajectories the year after COVID-19 hospitalization. Int J Environ Res Public Health. (2022) 19(14):8452. doi: 10.3390/ijerph19148452
14. Ceban F, Ling S, Lui LMW, Lee Y, Gill H, Teopiz KM, et al. Fatigue and cognitive impairment in post-COVID-19 syndrome: a systematic review and meta-analysis. Brain Behav Immun. (2022) 101:93–135. doi: 10.1016/j.bbi.2021.12.020
15. Davitt E, Davitt C, Mazer MB, Areti SS, Hotchkiss RS, Remy KE. COVID-19 disease and immune dysregulation. Best Pract Res Clin Haematol. (2022) 35(3):101401. doi: 10.1016/j.beha.2022.101401
16. Vollbracht C, Kraft K. Oxidative stress and hyper-inflammation as major drivers of severe COVID-19 and long COVID: implications for the benefit of high-dose intravenous vitamin C. Front Pharmacol. (2022) 13:899198. doi: 10.3389/fphar.2022.899198
17. Pierce JD, Shen Q, Cintron SA, Hiebert JB. Post-COVID-19 syndrome. Nurs Res. (2022) 71(2):164–74. doi: 10.1097/NNR.0000000000000565
18. Dennis A, Cuthbertson DJ, Wootton D, Crooks M, Gabbay M, Eichert N, et al. Multi-organ impairment and long COVID: a 1-year prospective, longitudinal cohort study. J R Soc Med. (2023) 116(3):97–112. doi: 10.1177/01410768231154703
19. Shah SMA, Mohammad D, Qureshi MFH, Abbas MZ, Aleem S. Prevalence, psychological responses and associated correlates of depression, anxiety and stress in a global population, during the coronavirus disease (COVID-19) pandemic. Community Ment Health J. (2021) 57(1):101–10. doi: 10.1007/s10597-020-00728-y
20. Becker JH, Lin JJ, Doernberg M, Stone K, Navis A, Festa JR, et al. Assessment of cognitive function in patients after COVID-19 infection. JAMA Network Open. (2021) 4(10):e2130645. doi: 10.1001/jamanetworkopen.2021.30645
21. Yu C, Helwig EJ. Role of rehabilitation amidst the COVID-19 pandemic: a review. J Transl Med. (2021) 19(1):376. doi: 10.1186/s12967-021-03048-1
22. Sagarra-Romero L, Viñas-Barros A. COVID-19: short and long-term effects of hospitalization on muscular weakness in the elderly. Int J Environ Res Public Health. (2020) 17(23):8715. doi: 10.3390/ijerph17238715
23. Ayres JS. A metabolic handbook for the COVID-19 pandemic. Nat Metab. (2020) 2(7):572–85. doi: 10.1038/s42255-020-0237-2
24. Guzik TJ, Mohiddin SA, Dimarco A, Patel V, Savvatis K, Marelli-Berg FM, et al. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res. (2020) 116(10):1666–87. doi: 10.1093/cvr/cvaa106
25. Barker-Davies RM, O’Sullivan O, Senaratne KPP, Baker P, Cranley M, Dharm-Datta S, et al. The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br J Sports Med. (2020) 54(16):949–59. doi: 10.1136/bjsports-2020-102596
26. Ruegsegger GN, Booth FW. Health benefits of exercise. Cold Spring Harb Perspect Med. (2018) 8(7):a029694. doi: 10.1101/cshperspect.a029694
27. Fiuza-Luces C, Garatachea N, Berger NA, Lucia A. Exercise is the real polypill. Physiology. (2013) 28(5):330–58. doi: 10.1152/physiol.00019.2013
28. Nystoriak MA, Bhatnagar A. Cardiovascular effects and benefits of exercise. Front Cardiovasc Med. (2018) 5:135. doi: 10.3389/fcvm.2018.00135
29. Tanasescu M, Leitzmann MF, Rimm EB, Willett WC, Stampfer MJ, Hu FB. Exercise type and intensity in relation to coronary heart disease in men. JAMA. (2002) 288(16):1994–2000. doi: 10.1001/jama.288.16.1994
30. Dauwan M, Begemann MJH, Slot MIE, Lee EHM, Scheltens P, Sommer IEC. Physical exercise improves quality of life, depressive symptoms, and cognition across chronic brain disorders: a transdiagnostic systematic review and meta-analysis of randomized controlled trials. J Neurol. (2021) 268(4):1222–46. doi: 10.1007/s00415-019-09493-9
31. Fossati C, Torre G, Vasta S, Giombini A, Quaranta F, Papalia R, et al. Physical exercise and mental health: the routes of a reciprocal relation. Int J Environ Res Public Health. (2021) 18(23):12364. doi: 10.3390/ijerph182312364
32. Gill DL, Hammond CC, Reifsteck EJ, Jehu CM, Williams RA, Adams MM, et al. Physical activity and quality of life. J Prev Med Public Health. (2013) 46(Suppl 1):S28–34. doi: 10.3961/jpmph.2013.46.S.S28
33. Marquez DX, Aguiñaga S, Vásquez PM, Conroy DE, Erickson KI, Hillman C, et al. A systematic review of physical activity and quality of life and well-being. Transl Behav Med. (2020) 10(5):1098–109. doi: 10.1093/tbm/ibz198
34. Pearce M, Garcia L, Abbas A, Strain T, Schuch FB, Golubic R, et al. Association between physical activity and risk of depression: a systematic review and meta-analysis. JAMA Psychiatry. (2022) 79(6):550–9. doi: 10.1001/jamapsychiatry.2022.0609
35. Mairbäurl H. Red blood cells in sports: effects of exercise and training on oxygen supply by red blood cells. Front Physiol. (2013) 4:332. doi: 10.3389/fphys.2013.00332
36. Myers J, Kokkinos P, Nyelin E. Physical activity, cardiorespiratory fitness, and the metabolic syndrome. Nutrients. (2019) 11(7):1652. doi: 10.3390/nu11071652
37. Sorriento D, Di Vaia E, Iaccarino G. Physical exercise: a novel tool to protect mitochondrial health. Front Physiol. (2021) 12:660068. doi: 10.3389/fphys.2021.660068
38. Wardyn GG, Rennard SI, Brusnahan SK, McGuire TR, Carlson ML, Smith LM, et al. Effects of exercise on hematological parameters, circulating side population cells, and cytokines. Exp Hematol. (2008) 36(2):216–23. doi: 10.1016/j.exphem.2007.10.003
39. Brown JM, Shackelford DYK, Hipp ML, Hayward R. Evaluation of an exercise-based phase program as part of a standard care model for cancer survivors. Transl J Am Coll Sports Med. (2019) 4(7):45–54. doi: 10.1249/TJX.0000000000000082
40. Tessler J, Bordoni B. Cardiac rehabilitation. Statpearls. Treasure Island, FL: StatPearls Publishing LLC (2023).
41. CDC. Long COVID or post-COVID Conditions: centers for disease control and prevention. (2023). Available at: https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html
42. NCI. Side effects of cancer treatment: National Cancer Institute at the National Institutes of Health. (2023). Available at: https://www.cancer.gov/about-cancer/treatment/side-effects
43. ACS. Managing cancer-related side effects: American Cancer Society. (2023). Available at: https://www.cancer.org/cancer/managing-cancer/side-effects.html
44. Sawadogo W, Tsegaye M, Gizaw A, Adera T. Overweight and obesity as risk factors for COVID-19-associated hospitalisations and death: systematic review and meta-analysis. BMJ Nutr Prev Health. (2022) 5(1):10–18. doi: 10.1136/bmjnph-2021-000375
45. Zhang J-J, Dong X, Liu G-H, Gao Y-D. Risk and protective factors for COVID-19 morbidity, severity, and mortality. Clin Rev Allergy Immunol. (2023) 64(1):90–107. doi: 10.1007/s12016-022-08921-5
46. Butler MJ, Barrientos RM. The impact of nutrition on COVID-19 susceptibility and long-term consequences. Brain Behav Immun. (2020) 87:53–4. doi: 10.1016/j.bbi.2020.04.040
47. Iaccarino Idelson P, Rendina D, Strazzullo P. Nutrition and the COVID-19 pandemic: three factors with high impact on community health. Nutr Metab Cardiovasc Dis. (2021) 31(3):756–61. doi: 10.1016/j.numecd.2020.12.001
48. Downer S, Berkowitz SA, Harlan TS, Olstad DL, Mozaffarian D. Food is medicine: actions to integrate food and nutrition into healthcare. Br Med J. (2020) 369:m2482. doi: 10.1136/bmj.m2482
49. Tsagari A, Risvas G, Papathanasiou JV, Dionyssiotis Y. Nutritional management of individuals with SARS-CoV-2 infection during rehabilitation. J Frailty Sarcopenia Falls. (2022) 7(2):88–94. doi: 10.22540/JFSF-07-088
50. CDC. Benefits of healthy eating. (2023). Available at: https://www.cdc.gov/nutrition/resources-publications/benefits-of-healthy-eating.html
51. Hockele LF, Sachet Affonso JV, Rossi D, Eibel B. Pulmonary and functional rehabilitation improves functional capacity, pulmonary function and respiratory muscle strength in post COVID-19 patients: pilot clinical trial. Int J Environ Res Public Health. (2022) 19(22):14899. doi: 10.3390/ijerph192214899
52. Calabrese M, Garofano M, Palumbo R, Di Pietro P, Izzo C, Damato A, et al. Exercise training and cardiac rehabilitation in COVID-19 patients with cardiovascular complications: state of art. Life (Basel). (2021) 11(3):259. doi: 10.3390/life11030259
53. Piva T, Masotti S, Raisi A, Zerbini V, Grazzi G, Mazzoni G, et al. Exercise program for the management of anxiety and depression in adults and elderly subjects: is it applicable to patients with post-COVID-19 condition? A systematic review and meta-analysis. J Affect Disord. (2023) 325:273–81. doi: 10.1016/j.jad.2022.12.155
54. De Amicis R, Cancello R, Capodaglio P, Gobbi M, Brunani A, Gilardini L, et al. Patients with severe obesity during the COVID-19 pandemic: how to maintain an adequate multidisciplinary nutritional rehabilitation program? Obes Facts. (2021) 14(2):205–13. doi: 10.1159/000513283
55. Aman F, Masood S. How nutrition can help to fight against COVID-19 pandemic. Pak J Med Sci. (2020) 36(Covid19-s4):S121–S3. doi: 10.12669/pjms.36.COVID19-S4.2776
56. Shirado K, Furuno Y, Kanamaru K, Kawabata N, Okuno S, Yamashita T. Effect of rehabilitation nutrition on a post-acute severe COVID-19 patient: a case report. Healthcare (Basel). (2021) 9(8):1034. doi: 10.3390/healthcare9081034
57. Moscatelli F, Sessa F, Valenzano A, Polito R, Monda V, Cibelli G, et al. COVID-19: role of nutrition and supplementation. Nutrients. (2021) 13(3):976. doi: 10.3390/nu13030976
58. Barrea L, Grant WB, Frias-Toral E, Vetrani C, Verde L, de Alteriis G, et al. Dietary recommendations for post-COVID-19 syndrome. Nutrients. (2022) 14(6):1305. doi: 10.3390/nu14061305
59. Jimeno-Almazán A, Pallarés JG, Buendía-Romero Á, Martínez-Cava A, Franco-López F, Sánchez-Alcaraz Martínez BJ, et al. Post-COVID-19 syndrome and the potential benefits of exercise. Int J Environ Res Public Health. (2021) 18(10):5329. doi: 10.3390/ijerph18105329
Keywords: COVID-19, exercise, nutrition, rehabilitation, intervention, Long-COVID, muscle strength, mental health
Citation: Peterson BM, Unger I, Sun S, Park J-Y, Kim J, Gunasekera RS, Wilson J and Galbadage T (2023) The vital role of exercise and nutrition in COVID-19 rehabilitation: synergizing strength. Front. Sports Act. Living 5:1305175. doi: 10.3389/fspor.2023.1305175
Received: 30 September 2023; Accepted: 21 November 2023;
Published: 8 December 2023.
Edited by:
Tácio Santos, University Center of Brasilia, BrazilReviewed by:
Karl James New, University of South Wales, United Kingdom© 2023 Peterson, Unger, Sun, Park, Kim, Gunasekera, Wilson and Galbadage. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Brent M. Peterson YnJlbnQucGV0ZXJzb25AYmlvbGEuZWR1 Thushara Galbadage ZG9uLmdhbGJhZGFnZUBiaW9sYS5lZHU=
 Brent M. Peterson
Brent M. Peterson Isabelle Unger
Isabelle Unger Sunny Sun
Sunny Sun Ji-Yeun Park
Ji-Yeun Park Jinsil Kim
Jinsil Kim Richard S. Gunasekera
Richard S. Gunasekera Jason Wilson
Jason Wilson Thushara Galbadage
Thushara Galbadage