- Section of Anatomy and Histology, Department of Experimental and Clinical Medicine, University of Florence, Florence, Italy
Visual disability negatively impacts balance, everyday self-efficacy, and mobility and often leads affected subjects to perceive physical exercise as a burdensome challenge thus discouraging them from practicing. Despite the well-proven benefits of regular physical activity in visually impaired people, especially addressing postural control, there are no specific guidelines and most of the available literature seems to be flawed by critical issues. Given the wide heterogeneity and the multidimensional needs of this population, a more realistic and target-specific perspective is needed in order to properly investigate and promote exercise practice and adherence for balance improvement. On this basis, through a critical overview of the recent literature, the present article aimed to enrich the current knowledge about this topic by providing innovative suggestions, both practical and methodological, and specifically deepening the disability-related deficits and peculiarities of different age ranges. Moreover, since a multidisciplinary approach is advisable when designing and leading exercise protocols tailored to visually impaired individuals, such innovative hints also highlighted the central role of the adapted physical activity specialist, hence contributing to foster its official professional recognition and involvement in this field.
Introduction
Global health is currently jeopardized by three main trends, precisely, ageing population, globalization, and technological advance all of which promoting unhealthy behaviors and frames. Inevitably, the growing prevalence of chronic diseases and their risk factors is rapidly becoming a concerning global issue (1, 2). Physical inactivity, currently identified as the fourth leading risk factor for global mortality, is rising worldwide thus negatively affecting general health of all ages population (3–7). Sedentary lifestyle is associated with decreased quality of life and physical functioning, both causing socio-economic and psychophysical burdens on public health and individual daily life (8, 9). In an aging society, visual impairment is an increasingly prevalent condition especially in developed countries because of the uprising incidence of age-related eye diseases and diabetic retinopathy (10–13). Age regardless, vision impairment has been found to be strongly linked with lower everyday self-efficacy/functioning, both psychologically and physically (14–17) when compared with sighted peers (18–20). In particular, given the disability-related balance and postural control deficit (21–24), visually impaired (VI) individuals show higher risk of falls and accidental injuries (19, 25, 26), therefore perceiving exercise as an overwhelming challenge. Such conditions deeply impact autonomy, social interaction, overall wellbeing, and leisure/sport activity participation (27–32). Despite the well-known benefits of regular physical activity in disabled subjects (33–35), no VI-specific directives are available, and a large proportion of VI individuals does not meet the daily movement guidelines established for the general population (15, 36–39). Fear of falling and postural/proprioceptive control deficiencies play a crucial role in such lack of exercise, frequently leading those individuals to avoid any recreative or sportive physical engagement opportunity (12, 16, 20, 22, 28).
Balance control is the result of an orchestrated integration of visual, vestibular, and proprioceptive input, and deeply affects static and dynamic posture, both in daily life activities and in the recreative/sportive ones (40–43). When alterations occur in even one of those balance-related systems, psychophysical disorders, disabilities, loss of autonomy and functionality inevitably onset (14, 44). It has been widely demonstrated, in all age groups, that regular physical activity improves balance by stimulating proprioceptive postural control, general and segmental coordination, strength, and reaction time (41, 45). Despite the extensive scientific evidence, most studies focused on elderly fall prevention or post-injury and pathological frames rehabilitation, while just a few investigated balance training protocols specifically addressed to VI subjects (10, 46–52). Actually, regarding this target group, many studies deepened the topic more in a social inclusion than in a functional and performative perspective (53–56). Moreover, in case of visual disability, given the high percentage of aging-related onset, the wide range of visual deficit, and the safety purposed need of working out in small class, research often struggled to provide an exhaustive overview of the more effective methodological approaches for this variegated population (57). Visual impairment term includes a broad spectrum of etiology, time of onset and severity level which significantly affect subjective peculiarities and needs (58, 59). In order to provide a global and safe management of such heterogeneity, a multidimensional methodological approach might be preferred. Specifically regarding the training field, protocols should involve both collective and individual sessions, which should be designed, leaded and monitored by an adapted exercise specialist (60, 61).
Given the proved weight of postural control on health and quality of life, especially in case of visual disability (27), an updated review of the current knowledge, enriched with an evidence-based overview of the most innovative tools and technologies, might help designing easily applicable and age-tailored protocols for the VI population.
Specific aims and methods
On the aforementioned basis, the present narrative review aimed to offer not only a comprehensive summary of the recent literature investigating balance training for VI subjects but also innovative cues for future applications in that field. In detail, current balance training methodologies tailored to this target population were deepened in an age range-perspective aiming to provide a specific focus without losing the overall view. Indeed, presenting and discussing, side by side, the current research findings for each age group may ease to identify specific needs and balance sensitive/critical periods, thus guiding and optimizing field-specific investments. Hopefully, such perspective might also provide methodological tools to boost protocol adherence and effectiveness, together with a growing awareness of the central role of the adapted physical activity specialist. Concerning the applied criteria to source the investigated literature, a multiple database search (Pubmed, Web of Science and Scopus) was performed. Specifically, English language papers published from 2000 to 2023 have been found using keywords and sentences such as “visual disability”, “physical activity intervention for visually impaired”, “visually impaired balance”, “balance training and visual impairment”, “postural control in blind subjects”, “adapted sport and visual disability”, and subjectively prioritizing recent investigations and innovative methodological approaches/tools. Moreover, drawn from the identified articles bibliography and using the “similar articles” suggestions provided by scientific database, further literature fulfilling the abovementioned subjective criteria was selected.
Visual impairment implications on postural control
Congenital or acquired visual disability leads to psychophysical development delays and motor pattern alterations that consequently affect postural control (62–64). Posture, strongly linked to stability, balance and functionality, is a multidimensional concept able to impact daily life activities, social interaction, autonomy, and quality of life (65, 66). Motor behaviors, either purposeful or involuntary, are characterized by a bidirectional interplay between the body and the surrounding environment (19, 67). Such inevitable interaction is primarily influenced and driven by visual input, thus giving to this sensory system a crucial role in postural control and adjustments (68–72). Vision is indispensable to provide instant information regarding body-space interaction, movement precision/orientation and motor action timing. Visual impairment often isolates subjects from the external environment thus depriving them of the sensorimotor feedback needed for functional body mechanics acquisition and effective development of postural reflexes (64). The loss of the aforementioned feedback results in postural deviations chiefly characterized by backward leaning trunk, increased dorsal kyphosis, dropped shoulders, head forward compensating position, and valgus flat feet (63, 73, 74). All these anatomo-functional abnormalities, added to uncoordinated limb movements, decreased gait speed, spatial orientation difficulties and body image alteration, lead to faulty motor patterns and dynamic balance control issues (75–78).
Since posture turned out to be a psychosomatic affair, visual impairment can negatively impact not only motricity but also educational and social growth, thus feeding a dangerous vicious cycle (79). Blind children, due to disability-related development delays, exhibit poor body language, and ineffective facial expressions, gestures, and communication (31, 80). Though knowing sport and leisure activities benefits, overprotective parents often prevent them to experience those formative occasions (81–83). Unfortunately, postural control, both in terms of perception and execution, cannot be learnt and mastered without a constant interaction with others in a real environmental context. This lack of learning and peer-interacting opportunities, in addition to boosting fear and frustration, deeply affects postural behaviors (68, 84, 85).
Postural stability is referred to the body skill of maintaining balance and it is often assessed through postural sway analysis and quantification (86, 87). According to research findings, visual disability-affected individuals generally show increased postural sways hence experiencing higher fear of falling (88, 89). Such evaluation tool can help outlining a postural profile in semi-static and study setting, but it is fundamental to remind that human postural control is predominantly motion and reality connected (90). Therefore, balance control of VI individuals should be investigated not only in a fall prevention perspective, but through a comprehensive analysis of the main motor pattern performance in daily life frames, taking into account the disability-related alterations and compensative strategies (91, 92).
Adapted physical activity benefits on balance control in visually impaired individuals
Fundamental motor skills play a key role in learning/development of complex gestures required to effectively perform daily life activities and participate in specific physical activity and sport contexts. Among them, balance and stability skills, both static and dynamic, have the power to influence the correct structuring of motor competence as well as physical fitness level and psychophysical health (93–95).
It has been recently demonstrated that children motor competence perception is more impacting than actual motor abilities on their overall fitness level (96–99). During childhood, physical activity promotes motor skill development and, before self-awareness acquisition, children practice it despite their real competence and results, thus unintentionally increasing motor learning opportunities. After that stage, detectable at about the age of eight, a vicious spiral of physical activity disengagement onsets in children showing low motor competence (100–103). Literature has frequently reported that VI children and adolescents, when compared to sighted peers, tend to conduct a more sedentary life and to exhibit lower physical fitness (20, 31, 62, 104–108). This latter, along with a coherent motor skills impairment, seems to arise mostly from low participation in physical and after-school sport activities (37, 94, 109–111). Similarly, concerns regarding instructor methodological competence, environmental safety, lack of support, convenience and mobility often lead VI adults to not engage in physical/sport activities (112–115). Several studies reported that lower postural stability of VI individuals, compared to sighted ones, is due to the absence of natural compensatory mechanisms based on enhanced non-visual input use for balance control (91, 116–118).
Considering the elderly population, research mainly investigated balance control and fall prevention in healthy subjects affected by age-related visual dysfunctions. Conversely, only a few studies addressed visually disabled individuals highlighting that multimodal exercises can improve their postural control (119, 120). Accordingly, it has been suggested that balance control improvement in sight impaired people requires a conscious behavioral compensation achievable through a targeted training involving balance and navigation skills (121, 122). Based on this evidence, recent research highlighted a positive link between habitual physical activity levels and balance performance in those subjects, as briefly summarized in Table 1. In fact, blind individuals regularly practicing physical exercise show more functional gait pattern and perform better in balance and navigation tasks than sedentary peers (111, 122, 148). Precisely, it has been shown that a 12-week specific training protocol can significantly increase blind adults balance performance, thus confirming the effectiveness of adapted physical activity on their postural control and everyday mobility enhancement (149). Regarding VI children and adolescents, a further study detected that higher amount of physical exercise was deeply related to a postural sway decrease and an improvement in single-leg stance time, orientation abilities, and dynamic gait stability (123, 128). Since balance skills and spatial cognitive functions are development-dependent, the interrelation between motor activity and postural control should be especially promoted during childhood and adolescence (132, 133). Exploiting such learning-sensitive phase, the onset of disability-related balance deficit, postural alterations, mobility issues and fall fear could be effectively prevented or counteracted through a ludic, active, and challenging approach. Despite that, there is an evident lack of literature concerning the most effective exercise types, duration and methodologies in the visually disabled population (129). Since these individuals mostly rely on proprioceptive and vestibular input for postural control, to date, it seems that training protocols promoting such vicariant sense recruitment may be more effective (27, 71, 127, 137, 150, 151).
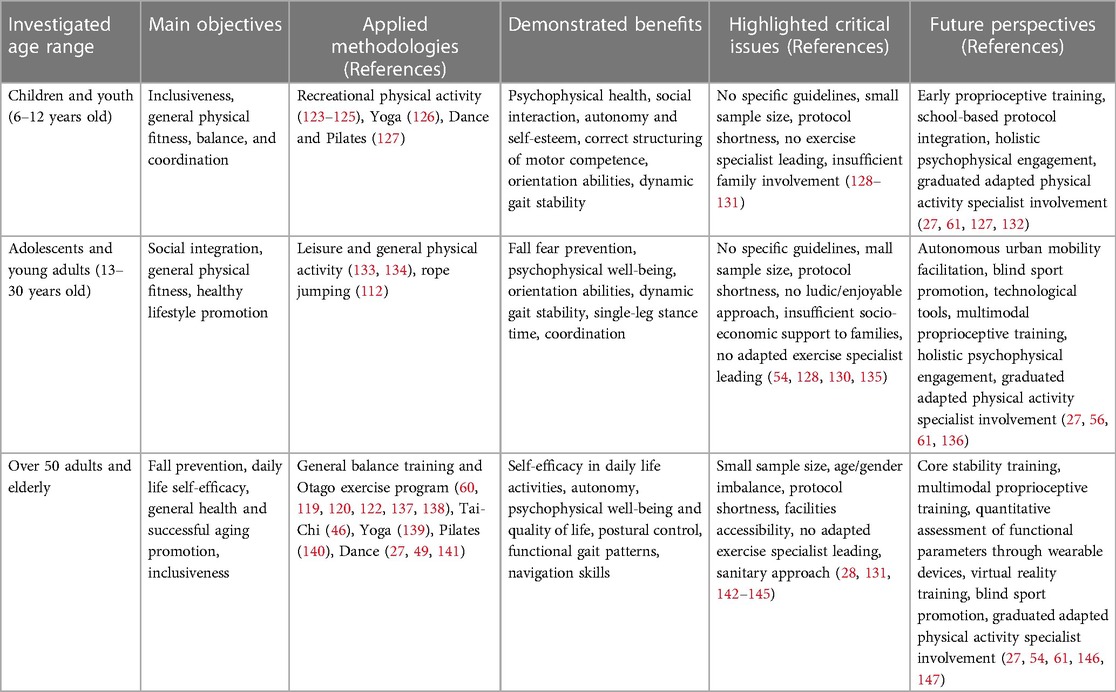
Table 1. Summary of current knowledge (2000–2023) and future perspectives of balance training for visually impaired individuals.
Evidence-based training methodologies and sport activities
Literature specifically addressing balance training for VI people is scarce and presents critical issues often attributed to research design weaknesses or errors, as reported in recent reviews (130, 142, 152). The main intrinsic issues concern the small sample size investigated and the consequent statistical reliability, as well as gender and age imbalance showing a clear predominance of female and elderly participation. In addition, there are almost none quantitative evaluation tools validated for this target population (57), and most of the studies last 8–12 weeks or less, thus being supposed to limit exercise psychophysical benefits and their maintenance over time (131) (Figure 1). Actually, if analyzed in a target-specific perspective, those potential limitations frequently reflect the peculiar multidimensional and safety needs of this heterogeneous population. In particular, adapted physical activity protocols tailored to VI subjects should be conceived, leaded and carried on in small groups thus granting collective and individual support, assistance, and safety (61). Regarding overrepresentation of female and elderly participants it must be considered that such proportion simply reflects the real socio-demographic characteristics of the worldwide population affected by visual impairment (58, 153). Finally, concerning protocols duration, it has been demonstrated that balance improvement is more affected by the frequency and peculiarities of the proprioceptive input applied than the intervention length (154, 155). Honestly, targeted physical exercise benefits maintenance, especially in disabled subjects, strongly relies on constant practice over time (156, 157). However, this criticality should not be imputed to study design weakness but more to the scarcity of field-specific investments in term of research funds, blind sports promotion, facilities accessibility, and involvement of adapted physical activity graduated specialists (28, 143–145) (Figure 1). Considering this necessary premise, current evidence emerged from interventions aimed to balance improvement in VI individuals are hereafter reported and concisely summarized in Table 1. Several studies were fall prevention aimed and, hence, they frequently addressed elderly and over fifty subject sample. As far as the applied methodology is concerned, some interventions used general balance training protocols while others opted for a validated exercise program such as Otago (60, 119, 120, 122, 138, 151). Additionally, recent evidence about Tai-Chi, yoga, Pilates and dance benefits on VI adults and elderly balance highlighted the relevance of a holistic involvement of this target population (27, 46, 49, 139–141). Focusing on research addressing balance improvement of young subjects affected by visual impairment, there is no univocal evidence about preferable or more effective methodologies and activities to apply (128). Therefore, current literature ranges from general physical activity protocols, even school integrated, to coordinative exercise such as rope jumping and holistic disciplines like yoga, dance, and Pilates (112, 124–127, 134). Since balance skills are development sensitive and the perception of motor competences, as well as family support, can deeply impact exercise engagement, adapted sports for VI children and adolescents should become a socio-economic and educational investment priority (56, 136, 158, 159). Finally, there is a variegated body of literature investigating athletes affected by visual impairment, both amateur or competitive, which considered and managed balance control as a crucial sport performance prerequisite (77, 160–169). Given the essential link between dynamic balance, anatomo-functional prerequisites and their on-field/in-game adaptation, it is widely believed that these targeted interventions should be conducted respecting and recalling the real sport specific frame (61).
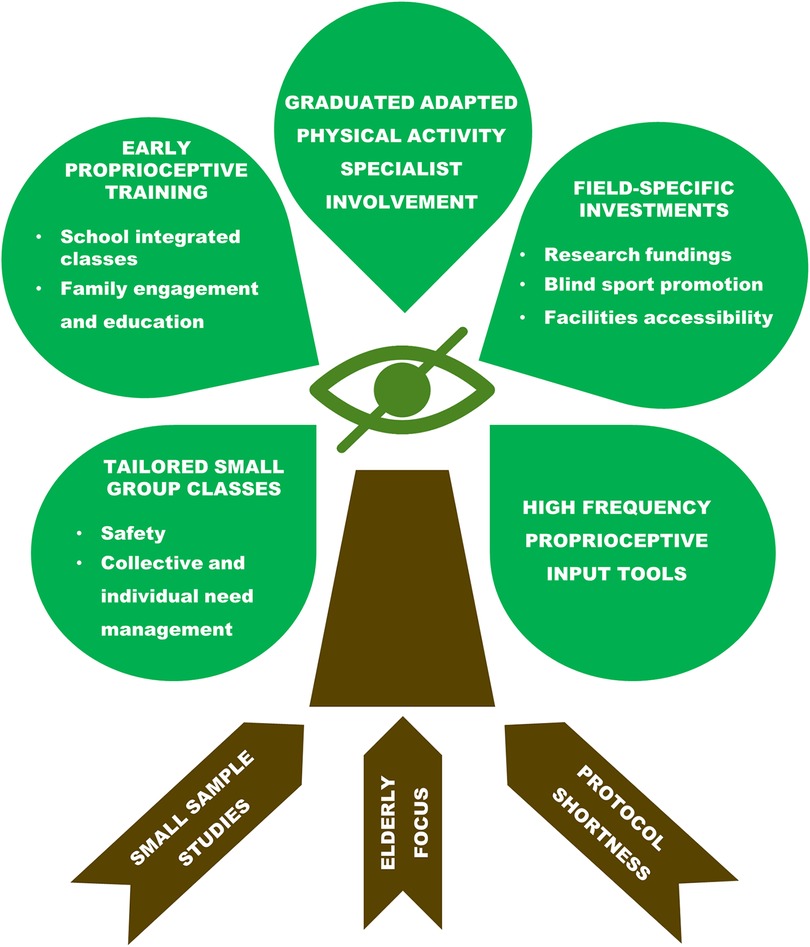
Figure 1. Tree diagram of the evidence-based critical issues (brown labels on tree roots) and the related applicable suggestions (green labels on tree crown) to improve balance control of visually impaired individuals through physical activity and sport practice.
Future perspectives and innovations
Although the well documented cause-effect relationship between physical inactivity and overall health parameters maintenance, balance control included, little is still known about visual impairment tailored exercise (170). Recent innovative approaches focused on core stability training, unstable surface utilization and multimodal proprioceptive input have reported findings worthy to be deepened (49, 171–174). At the same time, it is available in literature a rising application of virtual reality and technological tools, like wearable devices, able to monitor physical/functional parameters or to provide haptic and vibration feedback aimed to balance training of VI individuals (146, 147, 175, 176). Despite those few pioneering interventions, the main critical issues are related to the lack of guideline and literature investigating exercise effectiveness in a dose-response perspective on this target population. Indeed, almost all research applied low-intensity physical activities thus frequently overlooking the crucial link between fitness, motor competence perception and anatomo-functional parameters such as postural control (142). In future investigations, though focusing on balance and stability, it should be recommended to integrate such aimed protocols with moderate and vigorous intensity physical activities, hence globally affecting overall fitness and functionality (177). Moreover, there is scarcity of literature investigating the involvement and enjoyment of VI population approaching and consistently carrying on exercise practice (135). Indeed, the complex needs of these subjects require a global management able to consider not only protocols application and effectiveness, but also disability-specific communication and workout leading strategies to make them enjoyable and attractive, ultimately promoting exercise adherence (61, 131, 178). Unfortunately, balance improvement interventions addressing those who are visual impairment affected are often fall prevention oriented or based exclusively on basic daily life activities and mobility training (4, 5, 12, 14, 15, 41, 48, 179, 180). Despite the undeniable importance of the aforementioned aims, such a mostly sanitary/rehabilitative approach risks to discourage visually disabled individuals, especially youth, to perceive physical exercise as pleasant and worthy of engagement. On the basis of the rising recognition of health-related disparities experienced and reported by disabled people, it becomes crucial to grant them inclusiveness without losing sight both of their integration with healthy population and their peculiar needs (54). Therefore, given the well-known holistic involvement of disabled subjects during exercise practice and the acquired multidisciplinary competences of the graduated adapted physical activity specialists, it is advisable that they become the official professionals operating in such a sensitive field.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
GC: Conceptualization, Writing – original draft, Writing – review & editing. MM: Conceptualization, Writing – original draft, Writing – review & editing. MM: Conceptualization, Writing – original draft, Writing – review & editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Global recommendations on physical activity for health. Available at: https://www.who.int/publications-detail-redirect/9789241599979 (Accessed February 27, 2023).
2. Lavie CJ, Ozemek C, Carbone S, Katzmarzyk PT, Blair SN. Sedentary behavior, exercise, and cardiovascular health. Circ Res. (2019) 124:799–815. doi: 10.1161/CIRCRESAHA.118.312669
3. Kohl HW, Craig CL, Lambert EV, Inoue S, Alkandari JR, Leetongin G, et al. The pandemic of physical inactivity: global action for public health. Lancet Lond Engl. (2012) 380:294–305. doi: 10.1016/S0140-6736(12)60898-8
4. Katzmarzyk PT, Friedenreich C, Shiroma EJ, Lee I-M. Physical inactivity and non-communicable disease burden in low-income, middle-income and high-income countries. Br J Sports Med. (2022) 56:101–6. doi: 10.1136/bjsports-2020-103640
5. Stamatakis E, Gale J, Bauman A, Ekelund U, Hamer M, Ding D. Sitting time, physical activity, and risk of mortality in adults. J Am Coll Cardiol. (2019) 73:2062–72. doi: 10.1016/j.jacc.2019.02.031
6. Andersson C, Vasan RS. Epidemiology of cardiovascular disease in young individuals. Nat Rev Cardiol. (2018) 15:230–40. doi: 10.1038/nrcardio.2017.154
7. Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 19 million participants. Lancet Glob Health. (2018) 6:e1077–86. doi: 10.1016/S2214-109X(18)30357-7
8. Izquierdo M, Merchant RA, Morley JE, Anker SD, Aprahamian I, Arai H, et al. International exercise recommendations in older adults (ICFSR): expert consensus guidelines. J Nutr Health Aging. (2021) 25:824–53. doi: 10.1007/s12603-021-1665-8
9. Bermejo-Cantarero A, Álvarez-Bueno C, Martinez-Vizcaino V, García-Hermoso A, Torres-Costoso AI, Sánchez-López M. Association between physical activity, sedentary behavior, and fitness with health related quality of life in healthy children and adolescents: a protocol for a systematic review and meta-analysis. Medicine (Baltimore). (2017) 96:e6407. doi: 10.1097/MD.0000000000006407
10. Swenor BK, Lee MJ, Varadaraj V, Whitson HE, Ramulu PY. Aging with vision loss: a framework for assessing the impact of visual impairment on older adults. Gerontologist. (2020) 60:989–95. doi: 10.1093/geront/gnz117
11. Varma R, Vajaranant TS, Burkemper B, Wu S, Torres M, Hsu C, et al. Visual impairment and blindness in adults in the United States: demographic and geographic variations from 2015 to 2050. JAMA Ophthalmol. (2016) 134:802–9. doi: 10.1001/jamaophthalmol.2016.1284
12. Inoue S, Kawashima M, Hiratsuka Y, Nakano T, Tamura H, Ono K, et al. Assessment of physical inactivity and locomotor dysfunction in adults with visual impairment. Sci Rep. (2018) 8:12032. doi: 10.1038/s41598-018-30599-z
13. Mihailovic A, De Luna RM, West SK, Friedman DS, Gitlin LN, Ramulu PY. Gait and balance as predictors and/or mediators of falls in glaucoma. Invest Ophthalmol Vis Sci. (2020) 61:30. doi: 10.1167/iovs.61.3.30
14. Wahl H-W, Heyl V, Drapaniotis PM, Hörmann K, Jonas JB, Plinkert PK, et al. Severe vision and hearing impairment and successful aging: a multidimensional view. Gerontologist. (2013) 53:950–62. doi: 10.1093/geront/gnt013
15. Haegele JA, Zhu X. Movement behaviors, comorbidities, and health-related quality of life among adults with visual impairments. Disabil Rehabil. (2022) 44:4361–7. doi: 10.1080/09638288.2021.1906333
16. Seemungal BM, Glasauer S, Gresty MA, Bronstein AM. Vestibular perception and navigation in the congenitally blind. J Neurophysiol. (2007) 97:4341–56. doi: 10.1152/jn.01321.2006
17. van Landingham SW, Willis JR, Vitale S, Ramulu PY. Visual field loss and accelerometer-measured physical activity in the United States. Ophthalmology. (2012) 119:2486–92. doi: 10.1016/j.ophtha.2012.06.034
18. Bednarczuk G, Wiszomirska I, Rutkowska I, Skowroński W. Role of vision in static balance in persons with and without visual impairments. Eur J Phys Rehabil Med. (2021) 57:593–9. doi: 10.23736/S1973-9087.21.06425-X
19. Alghadir AH, Alotaibi AZ, Iqbal ZA. Postural stability in people with visual impairment. Brain Behav. (2019) 9:e01436. doi: 10.1002/brb3.1436
20. Wagner MO, Haibach PS, Lieberman LJ. Gross motor skill performance in children with and without visual impairments–research to practice. Res Dev Disabil. (2013) 34:3246–52. doi: 10.1016/j.ridd.2013.06.030
21. Gaerlan M. The role of visual, vestibular, and somatosensory systems in postural balance. UNLV theses, dissertations, professional papers, and capstones. (2010) 357. doi: 10.34917/1598677
22. Parreira RB, Grecco LAC, Oliveira CS. Postural control in blind individuals: a systematic review. Gait Posture. (2017) 57:161–7. doi: 10.1016/j.gaitpost.2017.06.008
23. Iosa M, Fusco A, Morone G, Paolucci S. Effects of visual deprivation on gait dynamic stability. Sci World J. (2012) 2012:974560. doi: 10.1100/2012/974560
24. Wood JM, Killingly C, Elliott DB, Anstey KJ, Black AA. Visual predictors of postural sway in older adults. Transl Vis Sci Technol. (2022) 11:24. doi: 10.1167/tvst.11.8.24
25. Graham V, Napier-Dovorany K. Multifactoral measures of fall risk in the visually impaired population: a pilot study. J Bodyw Mov Ther. (2016) 20:104–9. doi: 10.1016/j.jbmt.2015.06.012
26. Shuyi O, Zheng C, Lin Z, Zhang X, Li H, Fang Y, et al. Risk factors of falls in elderly patients with visual impairment. Front Public Health. (2022) 10:984199. doi: 10.3389/fpubh.2022.984199
27. Carretti G, Mirandola D, Sgambati E, Manetti M, Marini M. Survey on psychological well-being and quality of life in visually impaired individuals: dancesport vs. other sound input-based sports. Int J Environ Res Public Health. (2022) 19:4438. doi: 10.3390/ijerph19084438
28. Heinze N, Davies F, Jones L, Castle CL, Gomes RSM. Conceptualizations of well-being in adults with visual impairment: a scoping review. Front Psychol. (2022) 13:964537. doi: 10.3389/fpsyg.2022.964537
29. Maaswinkel IM, van der Aa HPA, van Rens GHMB, Beekman ATF, Twisk JWR, van Nispen RMA. Mastery and self-esteem mediate the association between visual acuity and mental health: a population-based longitudinal cohort study. BMC Psychiatry. (2020) 20:461. doi: 10.1186/s12888-020-02853-0
30. Lamoureux EL, Hassell JB, Keeffe JE. The determinants of participation in activities of daily living in people with impaired vision. Am J Ophthalmol. (2004) 137:265–70. doi: 10.1016/j.ajo.2003.08.003
31. Li QD, Kuang XM, Qi J. Correlates of physical activity of children and adolescents with visual impairments: a systematic review. Curr Pharm Des. (2020) 26:5002–11. doi: 10.2174/1381612826666200518110241
32. Nguyen AM, Arora KS, Swenor BK, Friedman DS, Ramulu PY. Physical activity restriction in age-related eye disease: a cross-sectional study exploring fear of falling as a potential mediator. BMC Geriatr. (2015) 15:64. doi: 10.1186/s12877-015-0062-8
33. Martin JJ. Benefits and barriers to physical activity for individuals with disabilities: a social-relational model of disability perspective. Disabil Rehabil. (2013) 35:2030–7. doi: 10.3109/09638288.2013.802377
34. McGuire LC, Strine TW, Okoro CA, Ahluwalia IB, Ford ES. Healthy lifestyle behaviors among older U.S. adults with and without disabilities, behavioral risk factor surveillance system, 2003. Prev Chronic Dis. (2007) 4:A09.17173717
35. Rimmer JH, Marques AC. Physical activity for people with disabilities. Lancet Lond Engl. (2012) 380:193–5. doi: 10.1016/S0140-6736(12)61028-9
36. Carty C, van der Ploeg HP, Biddle SJH, Bull F, Willumsen J, Lee L, et al. The first global physical activity and sedentary behavior guidelines for people living with disability. J Phys Act Health. (2021) 18:86–93. doi: 10.1123/jpah.2020-0629
37. Ginis KA M, van der Ploeg HP, Foster C, Lai B, McBride CB, Ng K, et al. Participation of people living with disabilities in physical activity: a global perspective. Lancet Lond Engl. (2021) 398:443–55. doi: 10.1016/S0140-6736(21)01164-8
38. Ross SM, Haegele JA, Abrahamson K, Schram BM, Healy S. US adults with visual impairments meeting 24-h movement guidelines: updated national prevalence estimates. Disabil Health J. (2022) 15:101320. doi: 10.1016/j.dhjo.2022.101320
39. López-Sánchez GF, Grabovac I, Pizzol D, Yang L, Smith L. The association between difficulty seeing and physical activity among 17,777 adults residing in Spain. Int J Environ Res Public Health. (2019) 16:4267. doi: 10.3390/ijerph16214267
40. Reynard F, Christe D, Terrier P. Postural control in healthy adults: determinants of trunk sway assessed with a chest-worn accelerometer in 12 quiet standing tasks. PLoS ONE. (2019) 14:e0211051. doi: 10.1371/journal.pone.0211051
41. Lipworth WL, Hooker C, Carter SM. Balance, balancing, and health. Qual Health Res. (2011) 21:714–25. doi: 10.1177/1049732311399781
42. Forbes PA, Chen A, Blouin J-S. Sensorimotor control of standing balance. Handb Clin Neurol. (2018) 159:61–83. doi: 10.1016/B978-0-444-63916-5.00004-5
43. Caderby T, Cavallari P, Descarreaux M, Yiou E. Editorial: the contribution of postural adjustments to body balance and motor performance: volume II. Front Hum Neurosci. (2022) 16:910540. doi: 10.3389/fnhum.2022.910540
44. West SK, Munoz B, Rubin GS, Bandeen-Roche K, Broman AT, Turano KA. Compensatory strategy use identifies risk of incident disability for the visually impaired. Arch Ophthalmol Chic Ill 1960. (2005) 123:1242–7. doi: 10.1001/archopht.123.9.1242
45. Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee I-M, et al. American college of sports medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. (2011) 43:1334–59. doi: 10.1249/MSS.0b013e318213fefb
46. Chen EW, Fu ASN, Chan KM, Tsang WWN. The effects of tai chi on the balance control of elderly persons with visual impairment: a randomised clinical trial. Age Ageing. (2012) 41:254–9. doi: 10.1093/ageing/afr146
47. de Jong LD, Coe D, Bailey C, Adams N, Skelton DA. Views and experiences of visually impaired older people and exercise instructors about the falls management exercise programme: a qualitative study. Disabil Rehabil. (2021) 43:2561–7. doi: 10.1080/09638288.2019.1704894
48. Lundälv J, Thodelius C. Risk of injury events in patients with visual impairments: a Swedish survey study among hospital social workers. J Vis Impair Blind. (2021) 115:426–35. doi: 10.1177/0145482X211046666
49. Hackney ME, Hall CD, Echt KV, Wolf SL. Multimodal exercise benefits mobility in older adults with visual impairment: a preliminary study. J Aging Phys Act. (2015) 23:630–9. doi: 10.1123/japa.2014-0008
50. Student J, Engel D, Timmermann L, Bremmer F, Waldthaler J. Visual perturbation suggests increased effort to maintain balance in early stages of Parkinson’s to be an effect of age rather than disease. Front Hum Neurosci. (2022) 16:762380. doi: 10.3389/fnhum.2022.762380
51. Liu W-Y, Tung T-H, Zhang C, Shi L. Systematic review for the prevention and management of falls and fear of falling in patients with Parkinson’s disease. Brain Behav. (2022) 12:e2690. doi: 10.1002/brb3.2690
52. Mollà-Casanova S, Inglés M, Serra-Añó P. Effects of balance training on functionality, ankle instability, and dynamic balance outcomes in people with chronic ankle instability: systematic review and meta-analysis. Clin Rehabil. (2021) 35:1694–709. doi: 10.1177/02692155211022009
53. Papadopoulos K, Montgomery AJ, Chronopoulou E. The impact of visual impairments in self-esteem and locus of control. Res Dev Disabil. (2013) 34:4565–70. doi: 10.1016/j.ridd.2013.09.036
54. Alcaraz-Rodríguez V, Medina-Rebollo D, Muñoz-Llerena A, Fernández-Gavira J. Influence of physical activity and sport on the inclusion of people with visual impairment: a systematic review. Int J Environ Res Public Health. (2021) 19:443. doi: 10.3390/ijerph19010443
55. Columna L, Streete DA, Rocco-Dillon S, Hodge SR, Prieto L, Myers B, et al. Parents’ intentions toward including their children with visual impairments in physical activities. Disabil Rehabil. (2020) 42:667–78. doi: 10.1080/09638288.2018.1505969
56. Blauwet C, Willick SE. The paralympic movement: using sports to promote health, disability rights, and social integration for athletes with disabilities. PM R. (2012) 4:851–6. doi: 10.1016/j.pmrj.2012.08.015
57. Ong SR, Crowston JG, Loprinzi PD, Ramulu PY. Physical activity, visual impairment, and eye disease. Eye. (2018) 32:1296–303. doi: 10.1038/s41433-018-0081-8
58. Abdulhussein D, Abdul Hussein M. WHO vision 2020: have we done it? Ophthalmic Epidemiol (2023) 30:331–9. doi: 10.1080/09286586.2022.2127784
59. Assi L, Rosman L, Chamseddine F, Ibrahim P, Sabbagh H, Congdon N, et al. Eye health and quality of life: an umbrella review protocol. BMJ Open. (2020) 10:e037648. doi: 10.1136/bmjopen-2020-037648
60. Esatbeyoğlu F, Karaçoban L, Akın Ş, Dönmez G. Exercise programming for individuals with vision loss. Spor Hekim Derg. (2022) 57:213–9. doi: 10.47447/tjsm.0690
61. Carretti G, Bianco R, Sgambati E, Manetti M, Marini M. Reactive agility and pitching performance improvement in visually impaired competitive Italian baseball players: an innovative training and evaluation proposal. Int J Environ Res Public Health. (2023) 20:6166. doi: 10.3390/ijerph20126166
62. Bakke HA, Cavalcante WA, de Oliveira IS, Sarinho SW, Cattuzzo MT. Assessment of motor skills in children with visual impairment: a systematic and integrative review. Clin Med Insights Pediatr. (2019) 13:1179556519838287. doi: 10.1177/1179556519838287
63. Pereira RCM, Vigário PS, Mainenti MRM, Silva DTR, Lima TRL, Lemos T. Computerized photogrammetric assessment of postural alignment in visually impaired athletes. J Bodyw Mov Ther. (2019) 23:142–7. doi: 10.1016/j.jbmt.2018.06.010
64. Alotaibi AZ, Alghadir A, Iqbal ZA, Anwer S. Effect of absence of vision on posture. J Phys Ther Sci. (2016) 28:1374–7. doi: 10.1589/jpts.28.1374
65. Soares AV, de Oliveira CSR, Knabben RJ, Domenech SC, Borges Junior NG. Postural control in blind subjects. Einstein São Paulo. (2011) 9:470–6. doi: 10.1590/S1679-45082011AO2046
66. Wong H-B, Machin D, Tan S-B, Wong T-Y, Saw S-M. Visual impairment and its impact on health-related quality of life in adolescents. Am J Ophthalmol. (2009) 147:505–11.e1. doi: 10.1016/j.ajo.2008.09.025
67. Takakusaki K. Functional neuroanatomy for posture and gait control. J Mov Disord. (2017) 10:1–17. doi: 10.14802/jmd.16062
68. Pasqualotto A, Proulx MJ. The role of visual experience for the neural basis of spatial cognition. Neurosci Biobehav Rev. (2012) 36:1179–87. doi: 10.1016/j.neubiorev.2012.01.008
69. Cullen KE, Taube JS. Our sense of direction: progress, controversies and challenges. Nat Neurosci. (2017) 20:1465–73. doi: 10.1038/nn.4658
70. Gori M, Amadeo MB, Campus C. Spatial metric in blindness: behavioural and cortical processing. Neurosci Biobehav Rev. (2020) 109:54–62. doi: 10.1016/j.neubiorev.2019.12.031
71. Jiang T-Y, Shi B, Wu D-M, Zhang L, Weng C-S, Zhang L-H. Effect of vision loss on plasticity of the head and neck proprioception. Int J Ophthalmol. (2021) 14:1059–65. doi: 10.18240/ijo.2021.07.15
72. Hallemans A, Beccu S, Van Loock K, Ortibus E, Truijen S, Aerts P. Visual deprivation leads to gait adaptations that are age- and context-specific: II. Kinematic parameters. Gait Posture. (2009) 30:307–11. doi: 10.1016/j.gaitpost.2009.05.017
73. Foisy A, Kapoula Z. Plantar exteroceptive inefficiency causes an asynergic use of plantar and visual afferents for postural control: best means of remediation. Brain Behav. (2017) 7:e00658. doi: 10.1002/brb3.658
74. Serin-Brackman V, Pezet Poux J, Quintyn J-C. Postural changes in patients with visual deficits. J Fr Ophtalmol. (2019) 42:1078–84. doi: 10.1016/j.jfo.2019.05.034
75. Jeon B-J, Cha T-H. The effects of balance of low vision patients on activities of daily living. J Phys Ther Sci. (2013) 25:693–6. doi: 10.1589/jpts.25.693
76. Bell L, Wagels L, Neuschaefer-Rube C, Fels J, Gur RE, Konrad K. The cross-modal effects of sensory deprivation on spatial and temporal processes in vision and audition: a systematic review on behavioral and neuroimaging research since 2000. Neural Plast. (2019) 2019:9603469. doi: 10.1155/2019/9603469
77. Campayo-Piernas M, Caballero C, Barbado D, Reina R. Role of vision in sighted and blind soccer players in adapting to an unstable balance task. Exp Brain Res. (2017) 235:1269–79. doi: 10.1007/s00221-017-4885-8
78. Pigeon C, Li T, Moreau F, Pradel G, Marin-Lamellet C. Cognitive load of walking in people who are blind: subjective and objective measures for assessment. Gait Posture. (2019) 67:43–9. doi: 10.1016/j.gaitpost.2018.09.018
79. De Araújo PP, De Moura Filho OF, Valenti VE, Gallo SM, Camargo MR, Say KG, et al. Stabilometric parameters analysis in children with visual disorder. Int Arch Med. (2014) 7:1. doi: 10.1186/1755-7682-7-1
80. Ramos de Toledo Negrão JV, de Andrade Freire L, de Araújo BMF, Venâncio TS, Kasahara N. Assessment of everyday functioning in visually impaired children from a developing country. J Pediatr Rehabil Med. (2022) 15:341–8. doi: 10.3233/PRM-200787
81. Greguol M, Gobbi E, Carraro A. Physical activity practice among children and adolescents with visual impairment–influence of parental support and perceived barriers. Disabil Rehabil. (2015) 37:327–30. doi: 10.3109/09638288.2014.918194
82. Hallemans A, Ortibus E, Truijen S, Meire F. Development of independent locomotion in children with a severe visual impairment. Res Dev Disabil. (2011) 32:2069–74. doi: 10.1016/j.ridd.2011.08.017
83. Haegele JA, Zhu X, Kirk TN. Physical activity among children with visual impairments, siblings, and parents: exploring familial factors. Matern Child Health J. (2021) 25:471–8. doi: 10.1007/s10995-020-03080-5
84. Rutkowska I, Lieberman LJ, Bednarczuk G, Molik B, Kazimierska-Kowalewska K, Marszałek J, et al. Bilateral coordination of children who are blind. Percept Mot Skills. (2016) 122:595–609. doi: 10.1177/0031512516636527
85. Schott N, Haibach-Beach P, Knöpfle I, Neuberger V. The effects of visual impairment on motor imagery in children and adolescents. Res Dev Disabil. (2021) 109:103835. doi: 10.1016/j.ridd.2020.103835
86. Whitney SL, Roche JL, Marchetti GF, Lin C-C, Steed DP, Furman GR, et al. A comparison of accelerometry and center of pressure measures during computerized dynamic posturography: a measure of balance. Gait Posture. (2011) 33:594–9. doi: 10.1016/j.gaitpost.2011.01.015
87. Urbaniak-Olejnik M, Loba W, Stieler O, Komar D, Majewska A, Marcinkowska-Gapińska A, et al. Body balance analysis in the visually impaired individuals aged 18–24 years. Int J Environ Res Public Health. (2022) 19:14383. doi: 10.3390/ijerph192114383
88. Sobry V, Badin P, Cernaianu S, Agnani O, Toussaint M. Do visually impaired people have a static balance as effective as sighted people? NeuroRehabilitation. (2014) 35:851–61. doi: 10.3233/NRE-141181
89. Tomomitsu MSV, Alonso AC, Morimoto E, Bobbio TG, Greve JMD. Static and dynamic postural control in low-vision and normal-vision adults. Clin Sao Paulo Braz. (2013) 68:517–21. doi: 10.6061/clinics/2013(04)13
90. Cohen RG, Vasavada AN, Wiest MM, Schmitter-Edgecombe M. Mobility and upright posture are associated with different aspects of cognition in older adults. Front Aging Neurosci. (2016) 8:257. doi: 10.3389/fnagi.2016.00257
91. Schmid M, Nardone A, De Nunzio AM, Schmid M, Schieppati M. Equilibrium during static and dynamic tasks in blind subjects: no evidence of cross-modal plasticity. Brain J Neurol. (2007) 130:2097–107. doi: 10.1093/brain/awm157
92. Russo MM, Lemos T, Imbiriba LA, Ribeiro NL, Vargas CD. Beyond deficit or compensation: new insights on postural control after long-term total visual loss. Exp Brain Res. (2017) 235:437–46. doi: 10.1007/s00221-016-4799-x
93. Gallahue DL, Ozmun JC, Goodway J. Understanding motor development: Infants, children, adolescents, adults. 7th ed. New York: McGraw-Hill (2012). 461 p.
94. den Uil AR, Janssen M, Busch V, Kat IT, Scholte RHJ. The relationships between children’s motor competence, physical activity, perceived motor competence, physical fitness and weight status in relation to age. PLoS One. (2023) 18:e0278438. doi: 10.1371/journal.pone.0278438
95. Smith PF. Is hippocampal neurogenesis modulated by the sensation of self-motion encoded by the vestibular system? Neurosci Biobehav Rev. (2017) 83:489–95. doi: 10.1016/j.neubiorev.2017.09.013
96. De Meester A, Maes J, Stodden D, Cardon G, Goodway J, Lenoir M, et al. Identifying profiles of actual and perceived motor competence among adolescents: associations with motivation, physical activity, and sports participation. J Sports Sci. (2016) 34:2027–37. doi: 10.1080/02640414.2016.1149608
97. Morrison KM, Cairney J, Eisenmann J, Pfeiffer K, Gould D. Associations of body mass Index, motor performance, and perceived athletic competence with physical activity in normal weight and overweight children. J Obes. (2018) 2018:e3598321. doi: 10.1155/2018/3598321
98. Brian A, Starrett A, Haibach-Beach P, De Meester A, Taunton Miedema S, Pennell A, et al. Perceived motor competence mediates the relationship between gross motor skills and physical activity in youth with visual impairments. Res Q Exerc Sport. (2022) 93:310–7. doi: 10.1080/02701367.2020.1831688
99. Haegele JA, Zhu X, Healy S, Patterson F. Proportions of youth with visual impairments meeting 24-hr movement guidelines. Child Care Health Dev. (2020) 46:345–51. doi: 10.1111/cch.12747
100. Stodden D, Goodway J, Langendorfer S, Roberton MA, Rudisill M, Garcia C, et al. A developmental perspective on the role of motor skill competence in physical activity: an emergent relationship. Quest. (2008) 60:290–306. doi: 10.1080/00336297.2008.10483582
101. Babic MJ, Morgan PJ, Plotnikoff RC, Lonsdale C, White RL, Lubans DR. Physical activity and physical self-concept in youth: systematic review and meta-analysis. Sports Med. (2014) 44:1589–601. doi: 10.1007/s40279-014-0229-z
102. Crane JR, Naylor PJ, Cook R, Temple VA. Do perceptions of competence mediate the relationship between fundamental motor skill proficiency and physical activity levels of children in kindergarten? J Phys Act Health. (2015) 12:954–61. doi: 10.1123/jpah.2013-0398
103. Sparto PJ, Redfern MS, Jasko JG, Casselbrant ML, Mandel EM, Furman JM. The influence of dynamic visual cues for postural control in children aged 7–12 years. Exp Brain Res. (2006) 168:505–16. doi: 10.1007/s00221-005-0109-8
104. Giese M, Teigland C, Giessing J. Physical activity, body composition, and well-being of school children and youths with visual impairments in Germany. Br J Vis Impair. (2017) 35:120–9. doi: 10.1177/0264619617689905
105. Haibach PS, Wagner MO, Lieberman LJ. Determinants of gross motor skill performance in children with visual impairments. Res Dev Disabil. (2014) 35:2577–84. doi: 10.1016/j.ridd.2014.05.030
106. Szmodis M, Kälbli K, Kaj M, Király A, Almási G, Csányi T. Bone characteristics and physical fitness in children and adolescents with visual impairment. J Sports Med Phys Fitness. (2022) 62:81–9. doi: 10.23736/S0022-4707.21.12078-X
107. Sit CHP, Huang WY, Yu JJ, McKenzie TL. Accelerometer-assessed physical activity and sedentary time at school for children with disabilities: seasonal variation. Int J Environ Res Public Health. (2019) 16:3163. doi: 10.3390/ijerph16173163
108. Qi J, Xu JW, Shao WD. Physical activity of children with visual impairments during different segments of the school day. Int J Environ Res Public Health. (2020) 17:6897. doi: 10.3390/ijerph17186897
109. Barnett LM, Webster EK, Hulteen RM, De Meester A, Valentini NC, Lenoir M, et al. Through the looking glass: a systematic review of longitudinal evidence, providing new insight for motor competence and health. Sports Med. (2022) 52:875–920. doi: 10.1007/s40279-021-01516-8
110. Houwen S, Visscher C, Lemmink KAPM, Hartman E. Motor skill performance of school-age children with visual impairments. Dev Med Child Neurol. (2008) 50:139–45. doi: 10.1111/j.1469-8749.2007.02016.x
111. Müürsepp I, Arjokesse R, Ereline J, Pääsuke M, Gapeyeva H. Impact of visual impairment on static and dynamic postural control and habitual physical activity in children aged 10–16 years. Br J Vis Impair. (2018) 36:227–37. doi: 10.1177/0264619618780918
112. Chen C-C, Lin S-Y. The impact of rope jumping exercise on physical fitness of visually impaired students. Res Dev Disabil. (2011) 32:25–9. doi: 10.1016/j.ridd.2010.08.010
113. Capella-McDonnall M. The need for health promotion for adults who are visually impaired. J Vis Impair Blind. (2007) 101:133–45. doi: 10.1177/0145482X0710100302
114. Shields N, Synnot AJ, Barr M. Perceived barriers and facilitators to physical activity for children with disability: a systematic review. Br J Sports Med. (2012) 46:989–97. doi: 10.1136/bjsports-2011-090236
115. Kirchner CE, Gerber EG, Smith BC. Designed to deter. Community barriers to physical activity for people with visual or motor impairments. Am J Prev Med. (2008) 34:349–52. doi: 10.1016/j.amepre.2008.01.005
116. Zipori AB, Colpa L, Wong AMF, Cushing SL, Gordon KA. Postural stability and visual impairment: assessing balance in children with strabismus and amblyopia. PLOS ONE. (2018) 13:e0205857. doi: 10.1371/journal.pone.0205857
117. Ozdemir RA, Pourmoghaddam A, Paloski WH. Sensorimotor posture control in the blind: superior ankle proprioceptive acuity does not compensate for vision loss. Gait Posture. (2013) 38:603–8. doi: 10.1016/j.gaitpost.2013.02.003
118. Schwesig R, Goldich Y, Hahn A, Müller A, Kohen-Raz R, Kluttig A, et al. Postural control in subjects with visual impairment. Eur J Ophthalmol. (2011) 21:303–9. doi: 10.5301/EJO.2010.5504
119. Kovács E, Tóth K, Dénes L, Valasek T, Hazafi K, Molnár G, et al. Effects of exercise programs on balance in older women with age-related visual problems: a pilot study. Arch Gerontol Geriatr. (2012) 55:446–52. doi: 10.1016/j.archger.2012.01.009
120. Campbell AJ, Robertson MC, La Grow SJ, Kerse NM, Sanderson GF, Jacobs RJ, et al. Randomised controlled trial of prevention of falls in people aged > or =75 with severe visual impairment: the VIP trial. Br Med J. (2005) 331:817. doi: 10.1136/bmj.38601.447731.55
121. Kupers R, Ptito M. Compensatory plasticity and cross-modal reorganization following early visual deprivation. Neurosci Biobehav Rev. (2014) 41:36–52. doi: 10.1016/j.neubiorev.2013.08.001
122. da Silva ES, Fischer G, da Rosa RG, Schons P, Teixeira LBT, Hoogkamer W, et al. Gait and functionality of individuals with visual impairment who participate in sports. Gait Posture. (2018) 62:355–8. doi: 10.1016/j.gaitpost.2018.03.049
123. Rogge A-K, Hamacher D, Cappagli G, Kuhne L, Hötting K, Zech A, et al. Balance, gait, and navigation performance are related to physical exercise in blind and visually impaired children and adolescents. Exp Brain Res. (2021) 239:1111–23. doi: 10.1007/s00221-021-06038-3
124. Columna L, Fernández-Vivó M, Lieberman L, Arndt K. Recreational physical activity experiences among Guatemalan families with children with visual impairments. J Phys Act Health. (2015) 12:1119–27. doi: 10.1123/jpah.2014-0257
125. Furtado OL, Allums-Featherston K, Lieberman LJ, Gutierrez GL. Physical activity interventions for children and youth with visual impairments. Adapt Phys Act Q APAQ. (2015) 32:156–76. doi: 10.1123/APAQ.2014-0164
126. Mohanty S, Venkata Ramana Murty P, Pradhan B, Hankey A. Yoga practice increases minimum muscular fitness in children with visual impairment. J Caring Sci. (2015) 4:253–63. doi: 10.15171/jcs.2015.026
127. Mavrovouniotis F, Papaioannou CS, Argiriadou E, Mountakis C, Konstantinakos P, Pikoula IT, et al. The effect of a combined training program with Greek dances and pilates on the balance of blind children. J Phys Educ Sport. (2013) 13:91–100. doi: 10.7752/jpes.2013.01016
128. Zarei H, Norasteh AA. Effects of exercise training programs on balance of blind children and adolescents: a systematic review and meta-analysis. J Bodyw Mov Ther. (2022) 30:187–95. doi: 10.1016/j.jbmt.2022.02.017
129. Daneshmandi H, Norasteh AA, Zarei H. Balance in the blind: a systematic review. Phys Treat Specif Phys Ther J. (2021) 11:1–12. doi: 10.32598/ptj.11.1.430.2
130. Augestad LB, Jiang L. Physical activity, physical fitness, and body composition among children and young adults with visual impairments: a systematic review. Br J Vis Impair. (2015) 33:167–82. doi: 10.1177/0264619615599813
131. Surakka A, Kivelä T. The effect of a physical training programme on flexibility of upper body and trunk in visually impaired and deaf-blind persons. Eur J Adapt Phys Act. (2011) 4:7–21. doi: 10.5507/euj.2011.001
132. Bouchard D, Tétreault S. The motor development of sighted children and children with moderate low vision aged 8–13. J Vis Impair Blind. (2000) 94:564–73. doi: 10.1177/0145482X0009400903
133. Kim J, Park S-H. Leisure and health benefits among Korean adolescents with visual impairments. Int J Qual Stud Health Well-Being. (2018) 13:1435097. doi: 10.1080/17482631.2018.1435097
134. Demirturk F, Kaya M. Physical education lessons and activity status of visually impaired and sighted adolescents. Med Sci Monit Int Med J Exp Clin Res. (2015) 21:3521–7. doi: 10.12659/msm.895038
135. Orr K, Evans MB, Tamminen KA, Arbour-Nicitopoulos KP. A scoping review of recreational sport programs for disabled emerging adults. Res Q Exerc Sport. (2020) 91:142–57. doi: 10.1080/02701367.2019.1653432
136. Diaz R, Miller EK, Kraus E, Fredericson M. Impact of adaptive sports participation on quality of life. Sports Med Arthrosc Rev. (2019) 27:73–82. doi: 10.1097/JSA.0000000000000242
137. Rogge A-K, Röder B, Zech A, Hötting K. Exercise-induced neuroplasticity: balance training increases cortical thickness in visual and vestibular cortical regions. NeuroImage. (2018) 179:471–9. doi: 10.1016/j.neuroimage.2018.06.065
138. Waterman H, Ballinger C, Brundle C, Chastin S, Gage H, Harper R, et al. A feasibility study to prevent falls in older people who are sight impaired: the VIP2UK randomised controlled trial. Trials. (2016) 17:464. doi: 10.1186/s13063-016-1565-0
139. Jeter PE, Haaz Moonaz S, Bittner AK, Dagnelie G. Ashtanga-based yoga therapy increases the sensory contribution to postural stability in visually-impaired persons at risk for falls as measured by the wii balance board: a pilot randomized controlled trial. PLoS One. (2015) 10:e0129646. doi: 10.1371/journal.pone.0129646
140. Patti A, Zangla D, Sahin FN, Cataldi S, Lavanco G, Palma A, et al. Physical exercise and prevention of falls. Effects of a pilates training method compared with a general physical activity program: a randomized controlled trial. Medicine (Baltimore). (2021) 100:e25289. doi: 10.1097/MD.0000000000025289
141. Larsson L, Frändin K. Body awareness and dance-based training for persons with acquired blindness—effects on balance and gait speed. Vis Impair Res. (2009) 8:25–40. doi: 10.1080/13882350600964667
142. Sweeting J, Merom D, Astuti PAS, Antoun M, Edwards K, Ding D. Physical activity interventions for adults who are visually impaired: a systematic review and meta-analysis. BMJ Open. (2020) 10:e034036. doi: 10.1136/bmjopen-2019-034036
143. Ilhan B, Idil A, Ilhan I. Sports participation and quality of life in individuals with visual impairment. Ir J Med Sci. (2021) 190:429–36. doi: 10.1007/s11845-020-02285-5
144. Talmachev RA. [Present-day sports activities among the blind and persons with poor vision in different countries of the world]. Vestn Oftalmol. (2003) 119:43–6.12608047
145. Jaarsma EA, Dekker R, Koopmans SA, Dijkstra PU, Geertzen JHB. Barriers to and facilitators of sports participation in people with visual impairments. Adapt Phys Act Q APAQ. (2014) 31:240–64. doi: 10.1123/2013-0119
146. Jiménez MF, Mello RC, Bastos T, Frizera A. Assistive locomotion device with haptic feedback for guiding visually impaired people. Med Eng Phys. (2020) 80:18–25. doi: 10.1016/j.medengphy.2020.04.002
147. Phu S, Vogrin S, Al Saedi A, Duque G. Balance training using virtual reality improves balance and physical performance in older adults at high risk of falls. Clin Interv Aging. (2019) 14:1567–77. doi: 10.2147/CIA.S220890
148. Aydoğ E, Aydoğ ST, Çakci A, Doral MN. Dynamic postural stability in blind athletes using the biodex stability system. Int J Sports Med. (2006) 27:415–8. doi: 10.1055/s-2005-865777
149. Rogge A-K, Hötting K, Nagel V, Zech A, Hölig C, Röder B. Improved balance performance accompanied by structural plasticity in blind adults after training. Neuropsychologia. (2019) 129:318–30. doi: 10.1016/j.neuropsychologia.2019.04.005
150. Salari A, Sahebozamani M, Daneshjoo A, Karimi Afshar F. Assessment of balance recovery strategies during manipulation of somatosensory, vision, and vestibular system in healthy and blind women. J Rehabil Sci Res. (2019) 6:123–9. doi: 10.30476/jrsr.2019.81543.1001
151. Maćkowiak Z, Osiński W, Salamon A. The effect of sensorimotor training on the postural stability of visually impaired women over 50 years of age. J Women Aging. (2015) 27:68–80. doi: 10.1080/08952841.2014.928140
152. Lindsay RK, Di Gennaro F, Allen PM, Tully MA, Marotta C, Pizzol D, et al. Correlates of physical activity among adults with sight loss in high-income-countries: a systematic review. Int J Environ Res Public Health. (2021) 18:11763. doi: 10.3390/ijerph182211763
153. Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. (2012) 96:614–8. doi: 10.1136/bjophthalmol-2011-300539
154. Riva D, Fani M, Benedetti MG, Scarsini A, Rocca F, Mamo C. Effects of high-frequency proprioceptive training on single stance stability in older adults: implications for fall prevention. BioMed Res Int. (2019) 2019:2382747. doi: 10.1155/2019/2382747
155. Rivera MJ, Winkelmann ZK, Powden CJ, Games KE. Proprioceptive training for the prevention of ankle sprains: an evidence-based review. J Athl Train. (2017) 52:1065–7. doi: 10.4085/1062-6050-52.11.16
156. Aitchison B, Rushton AB, Martin P, Barr M, Soundy A, Heneghan NR. The experiences and perceived health benefits of individuals with a disability participating in sport: a systematic review and narrative synthesis. Disabil Health J. (2022) 15:101164. doi: 10.1016/j.dhjo.2021.101164
157. Carroll DD, Courtney-Long EA, Stevens AC, Sloan ML, Lullo C, Visser SN, et al. Vital signs: disability and physical activity — united States, 2009–2012. Morb Mortal Wkly Rep. (2014) 63:407–13.
158. Prieto LA, Meera B, Katz H, Hernandez MI, Haegele JA, Columna L. Physical activity of children with visual impairments: intentions and behaviors of parents post intervention. Disabil Rehabil. (2023). doi: 10.1080/09638288.2023.2228193 [Epub ahead of print].37353939
159. Williams G, Aggio D, Stubbs B, Pardhan S, Gardner B, Smith L. Physical activity levels in children with sensory problems: cross-sectional analyses from the millennium cohort study. Disabil Health J. (2018) 11:58–61. doi: 10.1016/j.dhjo.2017.07.002
160. Bataller-Cervero AV, Bascuas PJ, Rabal-Pelay J, Gutiérrez H, Piedrafita E, Berzosa C. Attack and defense performance in goalball: a proposal for throwing, balance and acoustic reaction evaluation. Biology (Basel). (2022) 11:1234. doi: 10.3390/biology11081234
161. Molik B, Morgulec-Adamowicz N, Kosmol A, Perkowski K, Bednarczuk G, Skowroński W, et al. Game performance evaluation in male goalball players. J Hum Kinet. (2015) 48:43–51. doi: 10.1515/hukin-2015-0090
162. Conn AF. Basketball for the blindA key step in developing navigational skills. J Rehabil Res Dev. (2006) 43:xi. doi: 10.1682/JRRD.2005.11.0161
163. Fortin-Guichard D, Ravensbergen HJC, Krabben K, Allen PM, Mann DL. The relationship between visual function and performance in para swimming. Sports Med Open. (2022) 8:20. doi: 10.1186/s40798-022-00412-3
164. Kons RL, Sakugawa RL, Rossato M, Diefenthaeler F, Detanico D. Neuromuscular and postural control in visually and nonvisually impaired judo athletes: case study. J Exerc Rehabil. (2019) 15:60–6. doi: 10.12965/jer.1836566.283
165. Krabben K, Ravensbergen RHJC, Orth D, Fortin-Guichard D, Savelsbergh GJP, Mann DL. Assessment of visual function and performance in paralympic judo for athletes with vision impairment. Optom Vis Sci Off Publ Am Acad Optom. (2021) 98:854–63. doi: 10.1097/OPX.0000000000001735
166. Kurz A, Lauber B, Franke S, Leukel C. Balance training reduces postural sway and improves sport-specific performance in visually impaired cross-country skiers. J Strength Cond Res. (2021) 35:247. doi: 10.1519/JSC.0000000000002597
167. Marini M, Sarchielli E, Portas MF, Ranieri V, Meli A, Piazza M, et al. Can baseball improve balance in blind subjects? J Sports Med Phys Fitness. (2011) 51:227–32.21681156
168. Myint J, Latham K, Mann D, Gomersall P, Wilkins AJ, Allen PM. The relationship between visual function and performance in rifle shooting for athletes with vision impairment. BMJ Open Sport Exerc Med. (2016) 2:e000080. doi: 10.1136/bmjsem-2015-000080
169. Torralba MA, Padullés JM, Losada JL, López JL. Spatiotemporal characteristics of motor actions by blind long jump athletes. BMJ Open Sport Exerc Med. (2017) 3:e000252. doi: 10.1136/bmjsem-2017-000252
170. Ackley-Holbrook E, Kang M, Morgan DW. Development and evaluation of the walk for health program: a physical activity intervention for adults with visual impairments. J Vis Impair Blind. (2016) 110:103–14. doi: 10.1177/0145482X1611000204
171. Anderson K, Behm DG. The impact of instability resistance training on balance and stability. Sports Med Auckl NZ. (2005) 35:43–53. doi: 10.2165/00007256-200535010-00004
172. Willson JD, Dougherty CP, Ireland ML, Davis IM. Core stability and its relationship to lower extremity function and injury. J Am Acad Orthop Surg. (2005) 13:316–25. doi: 10.5435/00124635-200509000-00005
173. Tchórzewski D, Jaworski J, Bujas P. Influence of long-lasting balancing on unstable surface on changes in balance. Hum Mov. (2010) 11:144–52. doi: 10.2478/v10038-010-0022-2
174. Karimizadeh Ardakani M, Shalamzari MH, Mansori MH. Effect of core stability training on postural control, risk of falling, and function of the blind: a randomized controlled trial. Balt J Health Phys Act. (2020) 12:11–22. doi: 10.29359/BJHPA.12.3.02
175. Bowman T, Gervasoni E, Arienti C, Lazzarini SG, Negrini S, Crea S, et al. Wearable devices for biofeedback rehabilitation: a systematic review and meta-analysis to design application rules and estimate the effectiveness on balance and gait outcomes in neurological diseases. Sensors. (2021) 21:3444. doi: 10.3390/s21103444
176. di Cagno A, Giombini A, Iuliano E, Moffa S, Caliandro T, Parisi A, et al. Acute effect of whole body vibration on postural control in congenitally blind subjects: a preliminary evidence. Disabil Rehabil. (2018) 40:2632–6. doi: 10.1080/09638288.2017.1353650
177. Barbosa DG, Andrade RD, Pelegrini A, Felden ÉP. Rating of perceived capacity: a proposal to predict adequate levels of physical activity in visually impaired individuals. J Sports Med Phys Fitness. (2019) 59:274–82. doi: 10.23736/S0022-4707.17.08070-7
178. Arem H, Moore SC, Patel A, Hartge P, Berrington de Gonzalez A, Visvanathan K, et al. Leisure time physical activity and mortality: a detailed pooled analysis of the dose-response relationship. JAMA Intern Med. (2015) 175:959–67. doi: 10.1001/jamainternmed.2015.0533
179. Haegele JA, Zhu X. Physical activity, self-efficacy and health-related quality of life among adults with visual impairments. Disabil Rehabil. (2021) 43:530–6. doi: 10.1080/09638288.2019.1631397
Keywords: visual disability, adapted physical activity, sport practice, balance training, postural control, exercise specialist
Citation: Carretti G, Manetti M and Marini M (2023) Physical activity and sport practice to improve balance control of visually impaired individuals: a narrative review with future perspectives. Front. Sports Act. Living 5:1260942. doi: 10.3389/fspor.2023.1260942
Received: 18 July 2023; Accepted: 31 August 2023;
Published: 13 September 2023.
Edited by:
Miguel-Angel Gomez-Ruano, Universidad Politécnica de Madrid, SpainReviewed by:
Lorenzo Rum, University of Sassari, Italy© 2023 Carretti, Manetti and Marini. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mirca Marini bWlyY2EubWFyaW5pQHVuaWZpLml0
 Giuditta Carretti
Giuditta Carretti Mirko Manetti
Mirko Manetti Mirca Marini
Mirca Marini