
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Sports Act. Living, 01 November 2023
Sec. Physical Activity in the Prevention and Management of Disease
Volume 5 - 2023 | https://doi.org/10.3389/fspor.2023.1236143
This article is part of the Research TopicPhysical Fitness via Advanced Technology - ICT Solutions for Healthier AgeingView all 5 articles
Purpose: Accelerometers can be used to objectively measure physical activity. They could be offered to people with chronic low back pain (CLBP) who are encouraged to maintain an active lifestyle. The aim of this study was to examine the use of accelerometers in studies of people with CLBP and to synthesize the main results regarding the measurement of objective physical activity.
Methods: A scoping review was conducted following Arksey and O'Malley's framework. Relevant studies were collected from 4 electronic databases (PubMed, Embase, CINHAL, Web of Science) between January 2000 and July 2023. Two reviewers independently screened all studies and extracted data.
Results: 40 publications out of 810 citations were included for analysis. The use of accelerometers in people with CLBP differed across studies; the duration of measurement, physical activity outcomes and models varied, and several limitations of accelerometry were reported. The main results of objective physical activity measures varied and were sometimes contradictory. Thus, they question the validity of measurement methods and provide the opportunity to discuss the objective physical activity of people with CLBP.
Conclusions: Accelerometers have the potential to monitor physical performance in people with CLBP; however, important technical limitations must be overcome.
Chronic low back pain (CLBP) has been defined as pain in the lumbar region persisting for more than 3 months (1). It is a major public health problem because of its high prevalence and its significant impact on the physical performance, psychological resources, and quality of life of affected individuals. It is a common cause of activity limitations, work disability and sick leave worldwide (2).
People with CLBP report high levels of disability and low levels of daily physical activity (3). They have difficulty maintaining their usual lifestyle habits, and their ability to perform work and leisure activities (4, 5). They describe their physical activity levels as reduced (6) and appear to have a high level of sedentary behavior. Sedentary behavior is defined as behavior adopted during low energy expenditure activities performed in a resting position like sitting or lying (6). Reducing sedentary behavior is a common treatment goal for people with CLBP (7). Several reasons for the reduction in physical activity levels have already been identified. One of these is the fear of experiencing pain (8). According to the fear-avoidance model, people with CLBP may interpret their pain as threatening and avoid exercise because of fear of reinjury (9). This can lead to physical deconditioning, disuse, depression, and disability (8). Other causes of activity limitation may include physical barriers such as pain intensity and comorbidities; psychological barriers such as lack of motivation, false beliefs, lack of perceived benefits, and misinterpretation; and socio-environmental barriers such as lack of time, work occupation, incorrect advice from health professionals and the family environment (10).
Nowadays, promoting physical activity and reducing sedentary behavior is widely recommended for people with CLBP. The management of this condition has progressed over the last 50 years from a biomedical to a biopsychosocial approach. Physical rest used to be systematically prescribed, whereas now the importance of physical activity and therapeutic education sessions is recognized (11). The World Health Organization defines physical activity as “any bodily movement produced by skeletal muscles that requires energy expenditure” (12). Daily physical activity, also known as free-living physical activity, refers to all movements regularly performed during leisure, employment, chores, sports and mobility activities (12). It is described according to several characteristics: intensity, duration, frequency, context and purpose (13). It can be measured using subjective or objective methods.
Assessments of physical activity are generally based on self-report measurements collected using personal records, activity diaries or questionnaires (14). The Baecke Physical Activity Questionnaire and the International Physical Activity Questionnaire are 2 examples of self-report measurements (14). These tools are inexpensive, easy to implement, and they measure individuals' perceptions of their own physical activity level (15). However, responses may be subject to recall and social desirability biases (15). For example, respondents may evaluate their level of physical activity differently from one session to another, or they may overestimate it.
The objective assessment of physical activity using motion sensors has progressed greatly over the last 2 decades. These sensors measure the biomechanical characteristics and/or physiological effects of physical activity (16). Initially developed in research laboratories, their use in the natural environment has been made possible by important technical advances related to the miniaturization of the tools (and consequently, the reduction of their weight and production costs), the optimization of battery autonomy, improvements in connectivity, and the optimization of data processing methods (17). Currently, accelerometers and inertial measurement systems (composed of an accelerometer, a gyroscope and possibly a magnetometer) are the gold standard for the measurement of activity in people with chronic diseases (18–21). They can be integrated into treatment methods and/or used to assess treatments effects.
However, little information is available about the use of motion sensors in people with CLBP. There are few studies in this population. Systematic reviews on the topic are outdated and include different methods of physical activity assessment (14, 22). Furthermore, data on the objective physical activity of people with CLBP are scarce and rarely compared to the objective physical activity of healthy people. Beyond the interest of producing objective research data, exploration of the different uses of accelerometers would allow for a more informed discussion of their potential benefits specifically within CLBP. Given the heterogeneity of studies in this specific population, a scope of the literature is required to inform researchers and clinicians about their use.
Thus, the main aims of this study were to examine the use of accelerometers in studies of people with CLBP and to synthesize the main results regarding the measurement of objective physical activity. More precisely, the first specific aim of this study was to map the use of accelerometers in studies of people with CLBP according to the models and number of sensors used, their position on the body, the duration of measurement, outcomes measured, and limitations. The second specific aim of this study was to synthesize the main findings for objective physical activity measured by accelerometers.
A scoping review was undertaken in accordance with the 5-stage methodological frameworks described by Arksey and O'Malley (23) and Levac et al. (24) as well as the PRISMA-ScR guidelines (Supplementary Table 1) (25).
We defined 2 research questions. (1) How is objective physical activity measured using accelerometers in research involving people with CLBP? (2) What are the results of accelerometry studies of objective physical activity in people with CLBP?
Relevant articles were sought in 4 electronic databases (PubMed, Embase, CINHAL, Web of Science), and the reference lists of selected articles and conference proceedings were also searched. A complementary search was conducted in Google and Google Scholar to identify other scientific sources. Four categories of keywords (chronic low back pain, activity, accelerometer, evaluation) were defined by the 4 co-authors. Boolean search terms were used to combine subject keywords and synonyms. The search was performed in all fields of the databases screened and is described in Table 1. The search was limited to articles published between January 1, 2000 and July 1, 2023, due to the timeframe of clinical use of these instruments in healthcare and the rapid evolution of sensor technology.
Inclusion criteria were defined prior to article selection. Exclusion criteria were specified during article selection. They were applied to all articles identified by the search.
Inclusion criteria:
• Study focusing on the assessment of people with CLBP (lumbar pain persisting beyond 3 months).
• Study focusing on the use of accelerometers as instruments to measure objective physical activity.
• Study focusing on daily physical activity data collection, or free-living data collection, over a period of several consecutive days.
• Article written in English or French.
Exclusion criteria:
• Study focusing on the evaluation of surgical techniques.
• Study focusing on the quantification of sleep duration and quality.
• Study focusing on specific populations (e.g., children, people over 75 years old or pregnant women).
• Study focusing on movement analysis or specifically analyzing muscle function.
First, 2 reviewers independently selected the articles according to titles, keywords and abstracts. Then, further selection was performed by the same 2 reviewers, based on the full-text review. Discrepancies were discussed and resolved with the help of 2 other reviewers with different backgrounds (research engineer and movement specialist).
Data were extracted using a specifically created form. In addition to the usual information (authors, title, year of publication, and source) and study characteristics (objectives, study design, sample size and population), the following data were extracted: accelerometer models used, number of accelerometers used per person, position of accelerometers on the body, measurement duration, objective physical activity outcomes measured using the accelerometers, limitations of accelerometer use, main outcomes for objective physical activity.
First, a table was drawn to present the characteristics of the studies selected. The data were then examined and organized into the characteristics of use of accelerometers and objective physical activity outcomes. The characteristics of use were further analyzed and classified according to 6 themes defined by the 4 authors during the development of the reporting chart: accelerometer models, number of accelerometers used per person, placement of accelerometers, duration of measurement, outcomes, and limitations relating to accelerometer use. The occurrence and frequency of each characteristic identified were calculated.
The results of the studies were analyzed and classed into 6 subcategories consistent with the purpose of this review:
• Comparing the objective physical activity of participants with CLBP and asymptomatic participants.
• Comparing subjective physical activity (as estimated by self-questionnaires) and objective physical activity in both participants with CLBP and control participants.
• Comparing the objective physical activity of participants with CLBP with usual expert recommendations.
• Assessing factors associated with objective physical activity.
• Assessing the measurement properties of physical activity assessment scales or objective physical activity assessment techniques.
• Assessing changes in objective physical activity in participants with CLBP after a rehabilitation intervention.
Any disagreement in the categorization was discussed between the co-authors until agreement was reached.
A total of 810 articles were identified. The selection process is described in the PRISMA flow chart (Figure 1) (26). In total, 40 articles were selected for analysis (27–66). An overview of the articles included can be found in the supplementary data (Supplementary Table 2).
The use of accelerometers in people with CLBP is described in Table 2. A variety of accelerometer models were used to measure objective physical activity in people with CLBP. The triaxial Actigraph was the most often used in the included studies (n = 14, 36.9%). Two other models were also used many times: the ActivPAL (uniaxial or triaxial accelerometer) (n = 6, 15.4%) and the Fitbit (n = 3, 7.7%) (triaxial accelerometer, also known as an activity tracker).
Accelerometers were positioned on many different parts of the body to measure activity in people with CLBP. The most common position was the hip (n = 15, 38.5%), particularly the right hip (n = 13, 33.3%); however, they could be positioned on the lower back (n = 8, 20.5%), wrist (n = 7, 17.9%) or thigh (n = 6, 15.4%), and were occasionally positioned on the sternum (n = 5, 5.1%). In more than half of the studies included, the duration of physical activity measurement was 7 days (n = 22, 56.4%).
The objective physical activity outcomes measured in people with CLBP differed between studies. The average activity per minute, called “counts” (n = 25, 64.1%) and the number of steps (n = 15, 38.4%) were often reported. Around 30% of the studies reported time spent at different intensities of activity (sedentary, light, moderate, vigorous) (n = 12, 30.8%) whereas more than 15% focused on the postural components of physical activity (time spent sitting, standing, walking, lying, and number of transfers) (n = 6, 15.4%).
The use of accelerometers was limited by a lack of compliance with wearing the instrument for several days (n = 12, 30.8%), and technical failures (n = 9, 23.1%). More than half of the selected studies excluded participants because of a lack of usable data (n = 22, 56.4%).
The results of the studies are presented in Tables 3–8. Tables 3–5 synthesize the results of studies that reported the objective physical activity of people with CLBP measured with accelerometers. Specifically, Table 3 synthesizes the results of studies that reported the objective physical activity of people with CLBP compared to asymptomatic participants. The objective physical activity of people with CLBP appeared to differ from that of asymptomatic people. These differences were related to specific objective measures of physical activity. For example, people with CLBP spent more time in sedentary activities and less time in light-intensity activities during the day (59). Their level of objective physical activity differed from that of asymptomatic participants based on different times of the day (58, 61). They spent more time lying down and sitting in the evening (61). However, the total amount of objective physical activity of people with CLBP over a week did not seem to differ from that of asymptomatic people (60, 61).
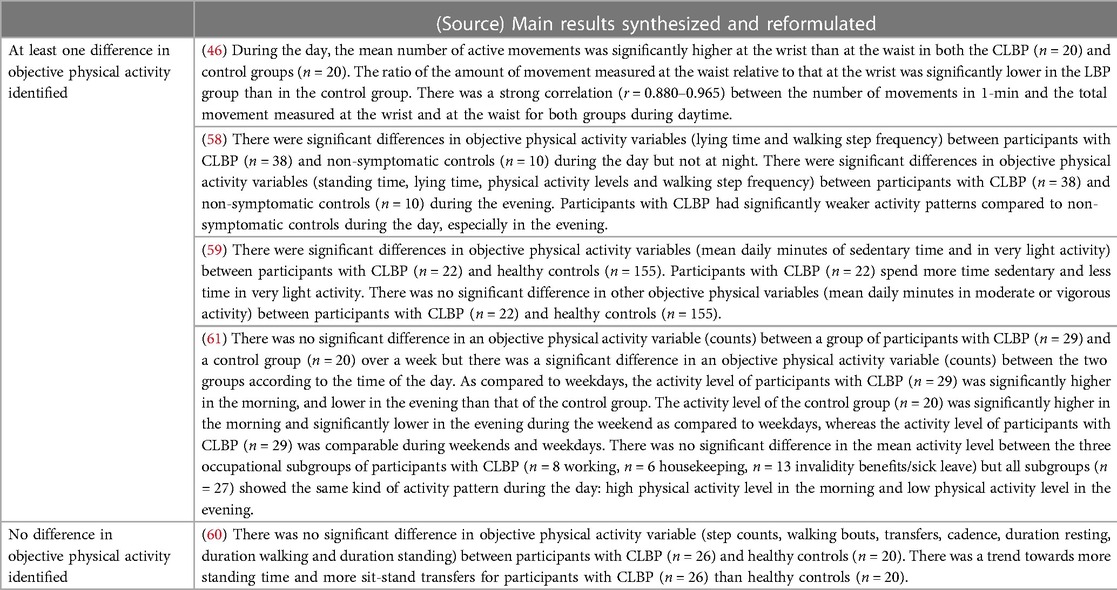
Table 3. Main results comparing the objective physical activity of participants with CLBP and asymptomatic participants.
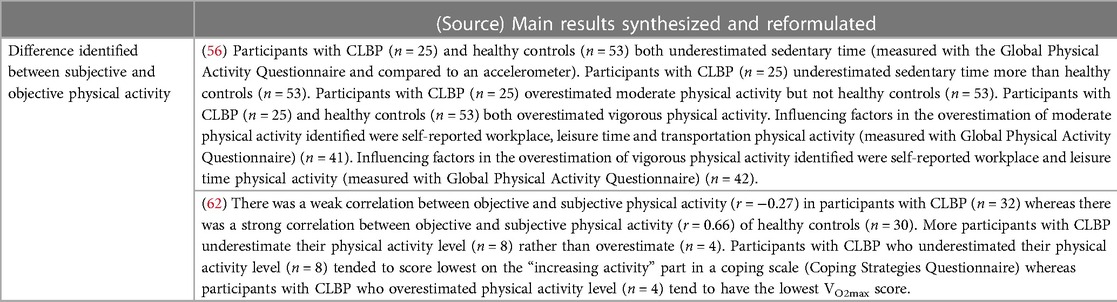
Table 4. Main results comparing the subjective physical activity and objective physical activity in both participants with CLBP and asymptomatic.
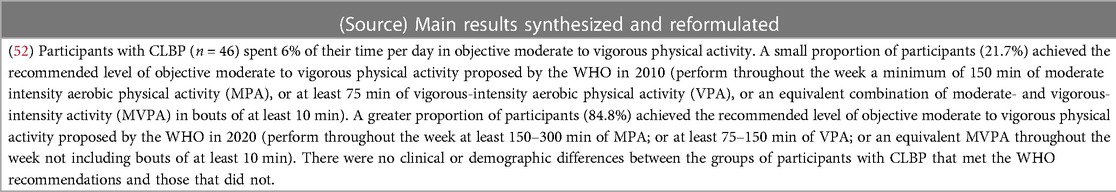
Table 5. Main results comparing the objective physical activity of participants with CLBP with usual expert recommendations.
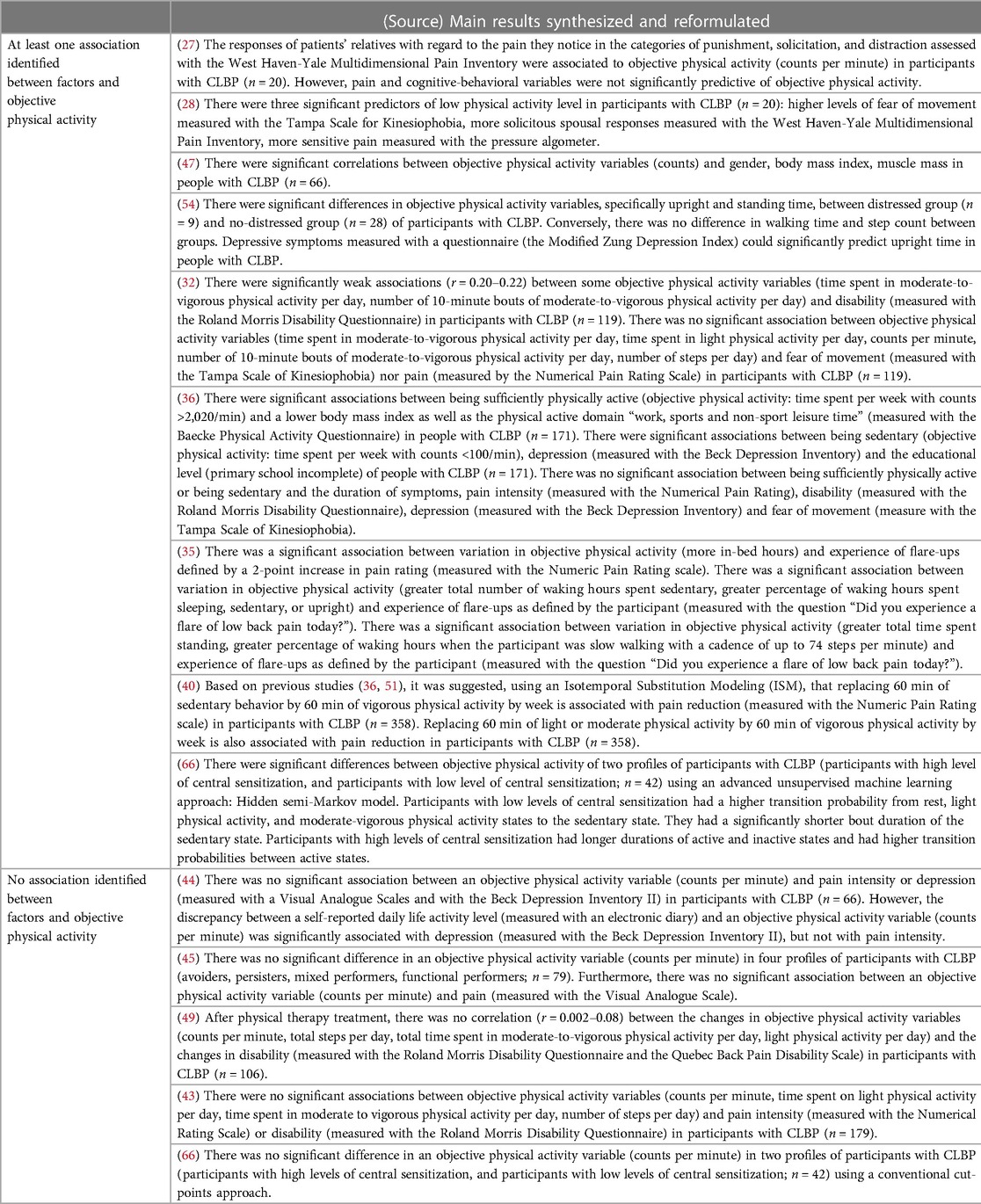
Table 6. Main results of the evaluation of factors associated with objective physical activity in participants with CLBP.
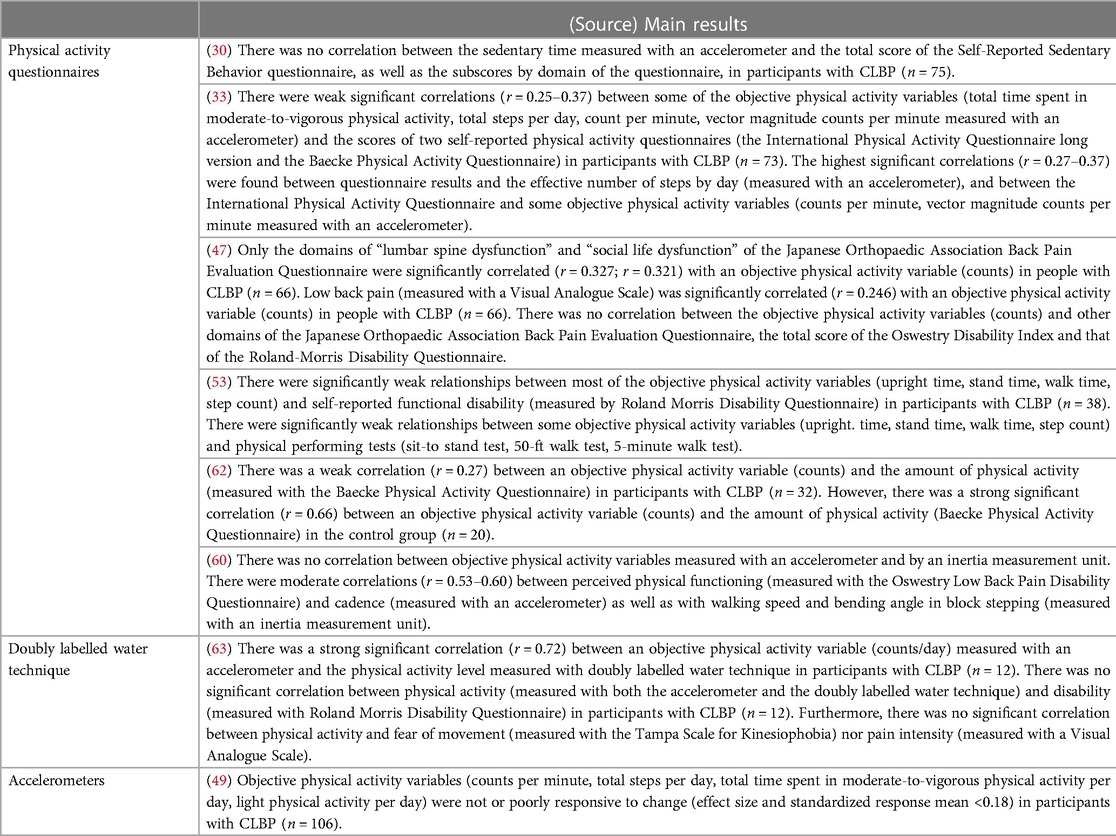
Table 7. Main results of the evaluation of measurement properties of physical assessment scales or other objective physical activity assessment techniques.
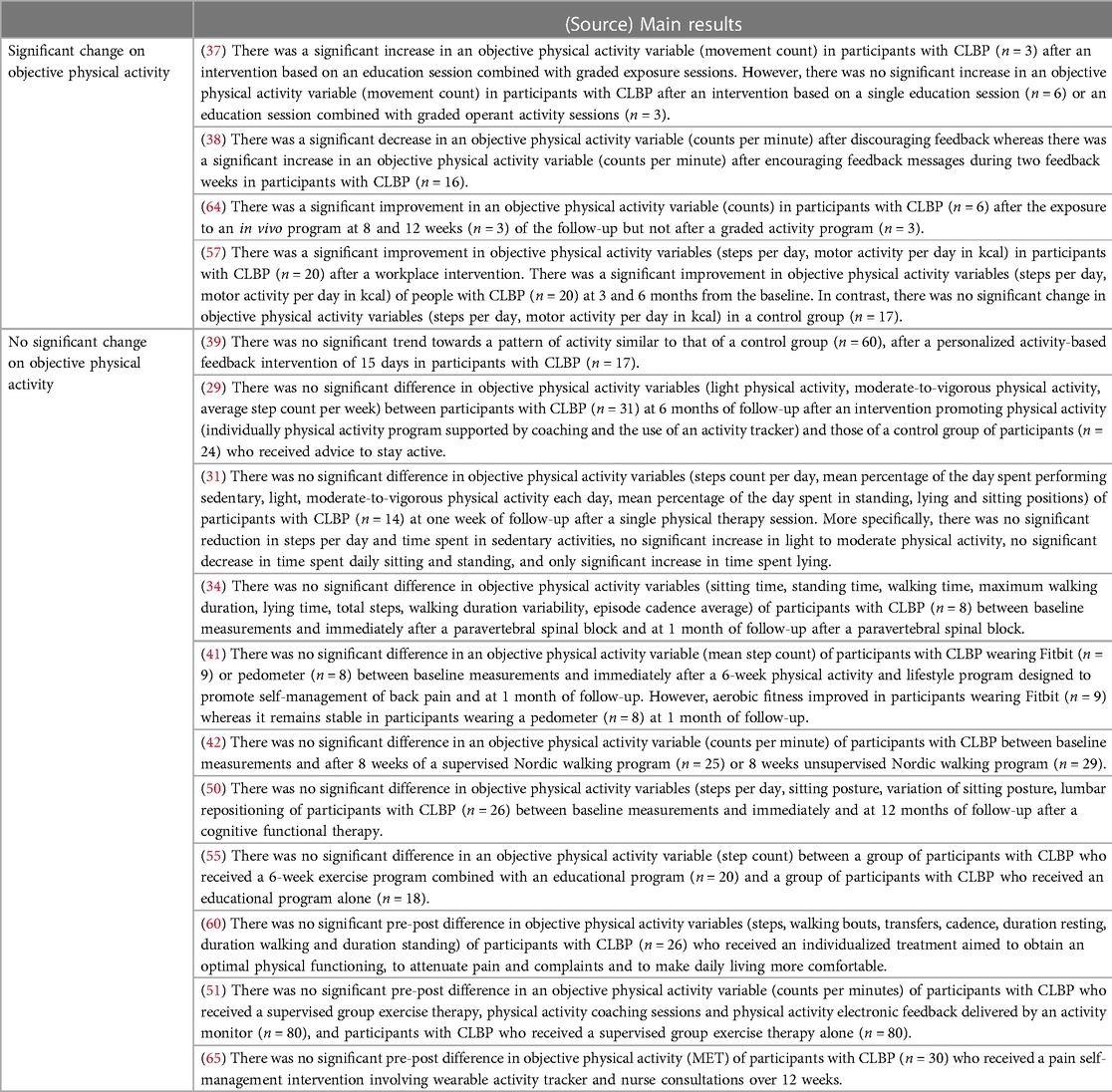
Table 8. Main results of the evaluation of the change in objective physical activity in people with CLBP following rehabilitation interventions.
Table 4 synthesizes the results of studies that reported the subjective physical activity and objective physical activity in both people with CLBP and asymptomatic people. Both people with CLBP and asymptomatic people underestimated their sedentary time and overestimated their time spent in vigorous activity (56). However, people with CLBP underestimated their sedentary time more than healthy controls (56). The correlation between objective and subjective physical activity in people with CLBP appeared to be weak (62).
Table 5 synthesizes the results of the only study that reported the objective physical activity of people with CLBP compared to usual expert recommendations. The results suggested that a significant proportion (84.8%) of people with CLBP met the current WHO recommendations for moderate to vigorous physical activity (52).
Table 6 presents the results of studies that reported factors associated with objective physical activity in participants with CLBP. The results indicated that the amount of physical activity performed by people with CLBP was associated with specific psychosocial factors (27, 28), distress (54), gender, body mass index and muscle mass (36, 47). But it did not appear to be associated with a specific level of pain (32, 36, 44, 45, 67), kinesiophobia, disability (32, 36, 49), or depression (36, 44).
Table 7 synthesizes the results of studies that evaluated the measurement properties of physical assessment scales (such as questionnaires) or other objective physical activity assessment techniques (such as the doubly labelled water technique). Many of the included studies showed that the results of physical activity questionnaires were not, or were only weakly, correlated with the objective physical activity variables obtained using accelerometers in people with CLBP. This was the case for many questionnaires: the Self-Reported Sedentary Behavior (30), the International Physical Activity Questionnaire (33), the Baecke Physical Activity Questionnaire (33, 62), the Japanese Orthopaedic Association Back Pain Evaluation Questionnaire (47), the Roland Morris Disability Questionnaire (47, 53). However, there was a strong significant correlation between objective physical activity measured with accelerometers and objective physical activity measured with the doubly labelled water technique (63). Only one study has evaluated the psychometric properties of accelerometers for measuring the objective physical activity in people with CLBP (49). This study demonstrated an absence or poor responsiveness to change of an accelerometer (Actigraph GT3X-BT) to measure the variables of objective physical activity intensity and step per day (49).
Finally, more than a third of the studies included in this scoping review (15 out of 40 studies) used accelerometers to assess changes in objective physical activity in people with CLBP following a rehabilitation intervention. Table 8 synthesizes the main results of changes in objective physical activity after various interventions. Few significant changes were found despite the diversity of rehabilitation treatments proposed. In fact, only 4 of 15 interventions had significant effects on objective physical activity variables. This was the case for an education session combined with graded exposure sessions (37, 64), a workplace intervention based on physical activity (57) and messages encouraging or discouraging activity sent on a phone application over 2 weeks (38). Interventions that did not show significant effects on objective physical activity variables included a physical activity program supported by coaching and the use of an activity tracker (27, 51, 65), a physical therapy session (31), a paravertebral spinal block (34), a program based on self-management of low back pain (41), a Nordic walking program (42), a cognitive functional therapy program (50), a 6-week exercise program combined with an education program (54), and an individualized program based on quality of life improvement (60).
The main aim of this scoping review was to examine the use of accelerometers in studies of people with CLBP and to synthesize the main results regarding the measurement of objective physical activity. The main research findings obtained with accelerometers were contradictory because they sometimes identified differences, associations, and significant effects of interventions on objective physical activity, but not always. These disparate results could be related to differences in the ways the accelerometers were used as well as differences in data processing methods.
Several models of accelerometers used in the studies were identified. The outcomes measured using these different accelerometers were not directly comparable (16) since the conversion of acceleration signals depends on the instrument models (68) and on the software used to process the data. The Actigraph model was the most prevalent in the included studies and it is also the most widely used in the medical and research communities at large (69).
The position of the accelerometers on the body was variable. Most earlier studies of physical activity attached the instruments around the waist and hips. These positions were chosen because of their proximity to the body center of gravity (70); however, the inability of the instrument to detect upper limb and upper body movements in this position can lead to underestimation of physical activity (71). In addition, the possible interference with clothing and potential discomfort led to the exploration of other positions on the body (72). More recent studies favored wrist-worn accelerometers because they are easier for users to accept. Strong correlations were identified between wrist and waist measurements in people with CLBP (46). However, identifying basic aspects of physical behavior, such as postures and types of activities performed, is difficult using wrist-worn accelerometers. They are more susceptible to random noise compared to sensor data from other positions (e.g., the hip) because of variations in movement and posture of the upper limb (73). Placement of the accelerometer on the thigh has several advantages. The accelerometer can easily be worn under clothing, and it can be used to measure specific activities such as sitting, standing, lying down, walking, running, climbing, and pedaling (70). Results from a recent narrative review indicate that accelerometers placed on the wrist, waist, thigh, ankle and foot are considered more comfortable and acceptable by users than those placed on the neck, chest, trunk, elbow, and fingers (74). Thus, the most commonly suggested positions for people with CLBP (hip, lower back, waist and wrist) appear to be relevant and should be recommended for future research.
The most common duration of physical activity measurement in the included studies was 7 days. This duration allows the influence of specific physical activities that might be a one-off to be filtered out (75). However, this duration appears to be too short to account for the influence of seasons, weather, or holidays on the measurement of objective physical activity. The measurement period and weather conditions were not discussed in the results of the selected studies. In some cases, the measurement could exceed several weeks, especially when the aim of the study was to evaluate the effects of monitoring physical activity with an accelerometer-based treatment (41, 76).
Several limitations in the use of accelerometers were identified in the studies included. In addition to forgetting to put on the instrument (77), technical failures, such as battery malfunction (72) or failure of the accelerometer to recharge (78), contributed to later abandonment at home. To improve compliance with wearing the instrument for several days, a daily telephone call (72), an activity diary to complete, or a list of activities to be checked off daily were suggested (48). A small number of studies included in this review used these strategies. For example, Xu et al. proposed regular follow-up by nurses (65). An activity diary was suggested by several teams to provide information on missing accelerometric data (27, 37, 52).
Overall, the relationship between physical activity and chronic low back pain is not yet well understood. Studies using objective measures of physical activity do not support the widespread belief that people with CLBP are less active than people without CLBP (22, 60, 61, 79). Although the amount of physical activity performed by people with CLBP is often considered to be reduced (14), the findings of this review show that, rather than being reduced overall, the level of physical activity varies depending on the specific physical activity outcomes measured. People with CLBP have a lower step frequency and spend more time lying down than controls (58). They are more active in the morning and less active in the evening than controls. They spend more time being sedentary and less time performing very light activity than controls (59). Therefore, as suggested by Griffin et al. it seems that it is mainly the distribution of activities performed during the day by people with CLBP that differs from that of people without CLBP (22). In fact, objective physical activity measurements show that people with CLBP are significantly less active in the evening and significantly more active in the morning compared to asymptomatic people (22). All these results confirm the need to consider perceived physical activity and objective physical activity as independent and complementary outcomes (60, 80).
Few studies evaluating change in physical activity following rehabilitation interventions in people with CLBP found significant differences on objective physical activity. These results are analogous to those published in 2018 in a systematic review of people with different musculoskeletal disorders that found no effect of physical activity interventions on objective physical activity (81).
These findings raise questions about the content of interventions intended to modify participants' behavior toward a more active lifestyle (82). They also question the validity of physical activity measurement techniques (27, 33, 46, 53, 60, 62), their sensitivity and responsiveness for this population (49). Furthermore, the methods used to analyze accelerometry data may not be appropriate for people with CLBP. Classical analysis methods stratify activity into several levels (sedentary, light, moderate and vigorous), based on the activity count. These levels were initially developed for the field of cardiovascular research, in which moderate to vigorous activity was primarily considered to reflect a person's physical condition (68). The levels do not include light intensity activity that reflects the impact of disorders on daily physical performance. They do not specifically address light physical activity, which is particularly impacted in CLBP (59, 68, 83). Moreover, the reliability and validity of the activity variables measured using accelerometers have mostly been examined in healthy individuals (17). Studies of the psychometric properties of accelerometry to measure activity variables are still scarce in chronic pain, particularly CLBP (22, 53, 75).
Our results question the common assumption that people with CLBP are less physically active than people without CLBP. High levels of pain and fear avoidance beliefs do not appear to be associated with objective physical activity levels (84). These findings provide an opportunity to question the fear-avoidance model proposed by Vlayen and Layton that suggests that the fear of pain generates disuse or a decreased level of physical activity (8). The results are in line with the avoidance-endurance model that suggests that a subgroup of people with CLBP ignore their pain and persist with activity (85). This latter model could help to understand the diversity of the results found by this scoping review as well as the clinical implications of these findings and the need to adapt rehabilitation programs to the different profiles of people with CLBP (85).
An increasing number of studies are attempting to identify different subgroups of people with CLBP using a multifactorial approach partly based on usual physical activity levels (86, 87). Such objective assessments of physical activity using accelerometers could help clinicians to understand the different subgroups of individuals with CLBP and to develop and provide individualized rehabilitation programs. However, only 2 of the included studies considered subgroups and provided separate results for the objective physical activity profiles of the people assessed (45, 66). Huijnen et al., showed that there was no significant difference in an objective physical activity variable (counts per minute) in 4 profiles of participants with CLBP (avoiders, persisters, mixed performers and functional performers) (45). Zheng et al., showed that there was no significant difference in an objective physical activity variable (counts per minute) in 2 profiles of participants with CLBP (participants with high levels of central sensitization, and participants with low levels of central sensitization) using a conventional cut-points approach, but there were significant differences between the objective physical activity levels of 2 profiles of participants with CLBP (participants with high levels of central sensitization and participants with low levels of central sensitization) using the Hidden semi-Markov model (66). The difference in results between these studies was probably related to the data processing techniques used; 2 used the cut-points approach (45, 66) and the other used an unsupervised machine learning approach (66). Thus, future treatment perspectives should be considered according to technical advances in accelerometry, data processing strategies, the validity of physical activity measurement techniques, and the feasibility of use of these tools with people with CLBP.
The opportunities offered by accelerometers seem promising for monitoring daily physical activity in people with CLBP. Accelerometers could provide measures of individual physical performance, i.e., what a person does in his or her real environment (69), and provide objective data regarding the intensity and extent of physical activity (60, 88). They could be used to define personalized activity goals to enrich educational sessions and self-management approaches (3). Furthermore, combining accelerometry with digital applications displaying physical activity data in a graphic format would allow people to visualize their own progress (14, 89, 90). Such applications could also contribute to the development of an individualized treatment plan (91). They could promote adherence to physical activity, reduce sedentary lifestyles (92–94) and, in addition, could help healthcare professionals to provide more sustainable support to their patients (93, 94). These instruments have already been used with people with other chronic illnesses such as type 2 diabetes or chronic obstructive pulmonary disease with promising results in terms of the quality of the follow-up (20, 95).
However, further research is obviously needed to address the methodological and technical limitations of accelerometers identified in this review. Objective physical activity data collected using accelerometers should be considered as independent of physical activity data collected by self-report measures. Regarding the use of accelerometers, clinicians and researchers need to be attentive to the choices made for use with people with CLBP, particularly in free-living conditions. The model of accelerometer, the position on the body, and the duration of measurement should be determined with caution because of the many biases that can arise (related to the diversity of occupations and environments of the wearers). Several strategies need to be implemented to address issues of non-compliance and potential technical incidents (such as regular reminders, the use of a dairy, and a support service available every day). The processing of accelerometer data should be more transparent to facilitate data sharing between different research teams. This would allow better understanding of the explanatory models of the disease so that more specific treatments could be proposed.
To our knowledge, this is the first scoping review to map the use of accelerometers in people with CLBP. The results should help clinicians and researchers interested in the use of these instruments in the development of future projects. For example, to better define the physical activity of people with CLBP or to assess the effects of interventions more accurately in this group. Furthermore, the results provide an opportunity to increase our understanding of the objective physical activity of people with CLBP. However, this study has some limitations. Only 4 electronic databases were searched. All included articles were in English. The optional step proposed by Arksey and O'Malley's method of presenting the results to users was not performed. Discussion of the results with healthcare professionals and people with CLBP who have used accelerometers would have enriched our thinking. Furthermore, the objective physical activity data measured by accelerometers were impossible to compare due to the diversity of device models used. Although the results of physical activities were expressed in “counts” in over 60% of the studies, the detailed on the post-processing used to obtain these counts was device-dependent and rarely specified.
The design of the current study did not allow rigorous assessment of the methodological quality of the selected articles. The included studies about the objective physical activity of people with CLBP measured with accelerometers after rehabilitation interventions were mainly different types of quasi-experimental studies whose results should be confirmed with more rigorous methodological designs. As such, the results provided an overview of how accelerometers are used in studies of people with CLBP, but analysis of the potential effect of their use on physical activity in people with CLBP was not possible. The results mainly suggest hypotheses and perspectives for further studies.
To conclude, this scoping review mapped the use of accelerometers to objectively measure physical activity in people with CLBP. Although accelerometers have been used in several studies to this purpose, there is no consensus on their use within this specific population. The main results related to objective physical activity are sometimes contradictory. Although accelerometers may indeed prove to be particularly useful for monitoring physical activity in people with CLBP, further research is needed to resolve the identified technical and methodological limitations to confirm this potential.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Conception and design of the study: MB and AB. Data collection: MB, AB. Data analysis and interpretation: MB, AB, TR, and LC. Drafting the manuscript: MB, AB, and LC. Critical revision of the manuscript: MB, AB, TR, and LC. Final approval of the version to be published: MB, AB, TR, and LC. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fspor.2023.1236143/full#supplementary-material
1. Haute Autorité de Santé. Prise en charge du patient présentant une lombalgie commune (2019). p. 178.
2. Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, et al. What low back pain is and why we need to pay attention. Lancet. (2018) 391(10137):2356–67. doi: 10.1016/S0140-6736(18)30480-X
3. Oliveira CB, Franco MR, Maher CG, Christine Lin CW, Morelhão PK, Araújo AC, et al. Physical activity interventions for increasing objectively measured physical activity levels in patients with chronic musculoskeletal pain: a systematic review. Arthritis Care Res. (2016) 68(12):1832–42. doi: 10.1002/acr.22919
4. Heneweer H, Staes F, Aufdemkampe G, van Rijn M, Vanhees L. Physical activity and low back pain: a systematic review of recent literature. Eur Spine J. (2011) 20(6):826–45. doi: 10.1007/s00586-010-1680-7
5. Grabovac I, Dorner TE. Association between low back pain and various everyday performances. Wien Klin Wochenschr. (2019) 131(21):541–9. doi: 10.1007/s00508-019-01542-7
6. Baradaran Mahdavi S, Riahi R, Vahdatpour B, Kelishadi R. Association between sedentary behavior and low back pain; a systematic review and meta-analysis. Health Promot Perspect. (2021) 11(4):393–410. doi: 10.34172/hpp.2021.50
7. Lansing JE, Ellingson LD, DeShaw KJ, Cruz-Maldonado G, Hurt TR, Meyer JD. A qualitative analysis of barriers and facilitators to reducing sedentary time in adults with chronic low back pain. BMC Public Health. (2021) 21(1):1–11. doi: 10.1186/s12889-021-10238-5
8. Vlaeyen JWS, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. (2000) 85(3):317–32. doi: 10.1016/S0304-3959(99)00242-0
9. Vlaeyen JWS, Kole-Snijders AMJ, Boeren RGB, van Eek H. Fear of movement/(re)injury in chronic low back pain and its relation to behavioral performance. Pain. (1995) 62(3):363. doi: 10.1016/0304-3959(94)00279-N
10. Boutevillain L, Dupeyron A, Rouch C, Richard E, Coudeyre E. Facilitators and barriers to physical activity in people with chronic low back pain: a qualitative study. Plos One. (2017) 12(7):e0179826. doi: 10.1371/journal.pone.0179826
11. Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet. (2018) 391(10137):2368–83. doi: 10.1016/S0140-6736(18)30489-6
12. OMS. Activité physique (2020). Available at: https://www.who.int/fr/news-room/fact-sheets/detail/physical-activity
13. Boiche J, Fervers B, Freyssenet D, Gremy I, Guiraud T, Moro C, et al. Activité physique: prévention et traitement des maladies chroniques [Doctoral dissertation]. Paris: Institut national de la santé et de la recherche médicale (INSERM) (2019).
14. Lin CWC, McAuley JH, Macedo L, Barnett DC, Smeets RJ, Verbunt JA. Relationship between physical activity and disability in low back pain: a systematic review and meta-analysis. Pain. (2011) 152(3):607–13. doi: 10.1016/j.pain.2010.11.034
15. Naranjo-Hernandez D, Reina-Tosina J, Roa LM. Sensor technologies to manage the physiological traits of chronic pain: a review. Sensors. (2020) 20(2):365. doi: 10.3390/s20020365
16. Trost SG, O’Neil M. Clinical use of objective measures of physical activity. Br J Sports Med. (2014) 48(3):178–81. doi: 10.1136/bjsports-2013-093173
17. Van Remoortel H, Giavedoni S, Raste Y, Burtin C, Louvaris Z, Gimeno-Santos E, et al. Validity of activity monitors in health and chronic disease: a systematic review. Int J Behav Nutr Phys Act. (2012) 9:1–23. doi: 10.1186/1479-5868-9-84
18. Barker J, Smith Byrne K, Doherty A, Foster C, Rahimi K, Ramakrishnan R, et al. Physical activity of UK adults with chronic disease: cross-sectional analysis of accelerometer-measured physical activity in 96 706 UK biobank participants. Int J Epidemiol. (2019) 48(4):1167–74. doi: 10.1093/ije/dyy294
19. Perruchoud C, Buchser E, Johanek LM, Aminian K, Paraschiv-Ionescu A, Taylor RS. Assessment of physical activity of patients with chronic pain. Neuromodulation. (2014) 17:42–7. doi: 10.1111/ner.12036
20. Vaes AW, Cheung A, Atakhorrami M, Groenen MTJ, Amft O, Franssen FME, et al. Effect of ‘activity monitor-based’ counseling on physical activity and health-related outcomes in patients with chronic diseases: a systematic review and meta-analysis. Ann Med. (2013) 45(5-6):397–412. doi: 10.3109/07853890.2013.810891
21. Smuck M, Kao MC, Goldin M, Patel A. The association of accelerometer-based activity monitoring with chronic low back pain. Spine J. (2011) 11(10):89S. doi: 10.1016/j.spinee.2011.08.223
22. Griffin DW, Harmon DC, Kennedy NM. Do patients with chronic low back pain have an altered level and/or pattern of physical activity compared to healthy individuals? A systematic review of the literature. Physiotherapy. (2012) 98(1):13–23. doi: 10.1016/j.physio.2011.04.350
23. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8(1):19–32. doi: 10.1080/1364557032000119616
24. Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. (2010) 5(1):69. doi: 10.1186/1748-5908-5-69
25. Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169(7):467–73. doi: 10.7326/M18-0850
26. Moher D, Liberati A, Tetzlaff J, Altman DG, Group PRISMA. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6(7):e1000097. doi: 10.1371/journal.pmed.1000097
27. Alschuler KN, Hoodin F, Murphy SL, Geisser ME. Ambulatory monitoring as a measure of disability in chronic low back pain populations. Clin J Pain. (2011) 27(8):707–15. doi: 10.1097/AJP.0b013e318217b7d0
28. Alschuler KN, Hoodin F, Murphy SL, Rice J, Geisser ME. Factors contributing to physical activity in a chronic low back pain clinical sample: a comprehensive analysis using continuous ambulatory monitoring. Pain. (2011) 152(11):2521–7. doi: 10.1016/j.pain.2011.07.017
29. Amorim AB, Pappas E, Simic M, Ferreira ML, Jennings M, Tiedemann A, et al. Integrating mobile-health, health coaching, and physical activity to reduce the burden of chronic low back pain trial (IMPACT): a pilot randomised controlled trial. BMC Musculoskelet Disord. (2019) 20(1):71. doi: 10.1186/s12891-019-2454-y
30. Araujo GMD, Pinto RZ, Azevedo BR, Silva FG, Damato TM, Grande GD, et al. Measurement properties of the sedentary behavior questionnaire in patients with chronic nonspecific low back pain. PM R. (2021) 13(3):250–7. doi: 10.1002/pmrj.12490
31. Brewer W, Swanson BT, Roddey TS, Adewale H, Ashmore C, Frerich J, et al. A pilot study to determine the effect of one physical therapy session on physical activity levels for individuals with chronic low back pain. BMC Res Notes. (2017) 10(1):691. doi: 10.1186/s13104-017-3006-x
32. Carvalho FA, Maher CG, Franco MR, Morelhão PK, Oliveira CB, Silva FG, et al. Fear of movement is not associated with objective and subjective physical activity levels in chronic nonspecific low back pain. Arch Phys Med Rehabil. (2017) 98(1):96–104. doi: 10.1016/j.apmr.2016.09.115
33. Carvalho FA, Morelhão PK, Franco MR, Maher CG, Smeets RJEM, Oliveira CB, et al. Reliability and validity of two multidimensional self-reported physical activity questionnaires in people with chronic low back pain. Musculoskelet Sci Pract. (2017) 27:65–70. doi: 10.1016/j.msksp.2016.12.014
34. Chuan Yen T, Mohler J, Dohm M, Laksari K, Najafi B, Toosizadeh N. The effect of pain relief on daily physical activity: in-home objective physical activity assessment in chronic low back pain patients after paravertebral spinal block. Sensors. (2018) 18(9):1–10. doi: 10.3390/s18093048
35. Costa N, Smits EJ, Kasza J, Salomoni S, Rodriguez-Romero B, Ferreira ML, et al. Are objective measures of sleep and sedentary behaviours related to low back pain flares? Pain. (2022) 163(9):1829–37. doi: 10.1097/j.pain.0000000000002585
36. Damato TM, Oliveira CB, Franco MR, Silva FG, Gobbi C, Morelhão PK, et al. Characteristics associated with people with chronic low back pain meeting physical activity guidelines and recommendations for sedentary behavior: a cross-sectional study. J Manipulative Physiol Ther. (2021) 44(5):378–88. doi: 10.1016/j.jmpt.2021.03.005
37. de Jong JR, Vlaeyen JWS, Onghena P, Goossens MEJB, Geilen M, Mulder H. Fear of movement/(re)injury in chronic low back pain: education or exposure in vivo as mediator to fear reduction? Clin J Pain. (2005) 21(1):9–17. doi: 10.1097/00002508-200501000-00002
38. Dekker-van Weering MGH, Vollenbroek-Hutten MMR, Hermens HJ. Do personalized feedback messages about activity patterns stimulate patients with chronic low back pain to change their activity behavior on a short term notice? Appl Psychophysiol Biofeedback. (2012) 37(2):81–9. doi: 10.1007/s10484-012-9181-6
39. Dekker-van Weering MGH, Vollenbroek-Hutten MMR, Hermens HJ. A pilot study – the potential value of an activity-based feedback system for treatment of individuals with chronic lower back pain. Disabil Rehabil. (2015) 37(24):2250–6. doi: 10.3109/09638288.2015.1019009
40. Freire APCF, de Oliveira CBS, Christofaro DGD, Shumate S, Marques LBF, Pinto RZ. Isotemporal substitution of sedentary behavior by different physical activity intensities on pain and disability of patients with chronic low back pain: a cross-sectional study. Arch Phys Med Rehabil. (2022) 103(10):1944–50. doi: 10.1016/j.apmr.2022.03.017
41. Gordon R, Bloxham S. Influence of the fitbit charge hr on physical activity, aerobic fitness and disability in non-specific back pain participants. J Sports Med Phys Fitness. (2017) 57(12):1669–75. doi: 10.23736/S0022-4707.17.06688-9
42. Hartvigsen J, Morsø L, Bendix T, Manniche C. Supervised and non-supervised nordic walking in the treatment of chronic low back pain: a single blind randomized clinical trial. BMC Musculoskelet Disord. (2010) 11:30. doi: 10.1186/1471-2474-11-30
43. Hisamatsu TM, Oliveira CB, Lira FS, Morelhão PK, Azevedo BR, Lemes ÍR, et al. Occupational physical activity was associated with disability levels at 6-month follow-up of patients with chronic nonspecific low back pain: a prospective cohort study. J Phys Act Health. (2022) 19(6):409–16. doi: 10.1123/jpah.2021-0798
44. Huijnen IPJ, Verbunt JA, Peters ML, Delespaul P, Kindermans HPJ, Roelofs J, et al. Do depression and pain intensity interfere with physical activity in daily life in patients with chronic low back pain? Pain. (2010) 150(1):161–6. doi: 10.1016/j.pain.2010.04.021
45. Huijnen IPJ, Verbunt JA, Peters ML, Smeets RJEM, Kindermans HPJ, Roelofs J, et al. Differences in activity-related behaviour among patients with chronic low back pain. Eur J Pain. (2011) 15(7):748–55. doi: 10.1016/j.ejpain.2010.11.015
46. Inoue M, Orita S, Inage K, Suzuki M, Fujimoto K, Shiga Y, et al. Comparison of the activity level of the upper limbs and trunk in patients with low back pain evaluated using a wearable accelerometer: a validation study. Spine Surg Relat Res. (2019) 3(4):354–60. doi: 10.22603/ssrr.2018-0100
47. Inoue M, Orita S, Inage K, Suzuki M, Fujimoto K, Shiga Y, et al. Relationship between patient-based scoring systems and the activity level of patients measured by wearable activity trackers in lumbar spine disease. Eur Spine J. (2019) 28(8):1804–10. doi: 10.1007/s00586-019-06023-z
48. McDonough SM, Tully MA, Boyd A, O’Connor SR, Kerr DP, O’Neill SM, et al. Pedometer-driven walking for chronic low back pain: a feasibility randomized controlled trial. Clin J Pain. (2013) 29(11):972–81. doi: 10.1097/AJP.0b013e31827f9d81
49. Morelhão PK, Franco MR, Oliveira CB, Hisamatsu TM, Ferreira PH, Costa LO, et al. Physical activity and disability measures in chronic non-specific low back pain: a study of responsiveness. Clin Rehabil. (2018) 32(12):1684–95. doi: 10.1177/0269215518787015
50. O’Sullivan K, Dankaerts W, O’Sullivan L, O’Sullivan PB. Cognitive functional therapy for disabling nonspecific chronic low back pain: multiple case-cohort study. Phys Ther. (2015) 95(11):1478–88. doi: 10.2522/ptj.20140406
51. Oliveira CB, Chirstofaro DGD, Maher CG, Franco MR, Tiedemann A, Silva FG, et al. Adding physical activity coaching and an activity monitor was no more effective than adding an attention control intervention to group exercise for patients with chronic nonspecific low back pain (PAyBACK trial): a randomized trial. J Orthop Sports Phys Ther. (2022) 52(5):287–99. doi: 10.2519/jospt.2022.10874
52. Reneman MF, Ansuategui Echeita J, van Kammen K, Schiphorst Preuper HR, Dekker R, Lamoth CJC. Do rehabilitation patients with chronic low back pain meet World Health Organisation’s recommended physical activity levels? Musculoskelet Sci Pract. (2022) 62:102618. doi: 10.1016/j.msksp.2022.102618
53. Ryan CG, Gray H, Newton M, Granat MH. The convergent validity of free-living physical activity monitoring as an outcome measure of functional ability in people with chronic low back pain. J Back Musculoskelet Rehabil. (2008) 21(2):137–42. doi: 10.3233/BMR-2008-21210
54. Ryan CG, Gray HG, Newton M, Granat MH. The relationship between psychological distress and free-living physical activity in individuals with chronic low back pain. Man Ther. (2010) 15(2):185–9. doi: 10.1016/j.math.2009.10.007
55. Ryan CG, Gray HG, Newton M, Granat MH. Pain biology education and exercise classes compared to pain biology education alone for individuals with chronic low back pain: a pilot randomised controlled trial. Man Ther. (2010) 15(4):382–7. doi: 10.1016/j.math.2010.03.003
56. Schaller A, Rudolf K, Dejonghe L, Grieben C, Froboese I. Influencing factors on the overestimation of self-reported physical activity: a cross-sectional analysis of low back pain patients and healthy controls. BioMed Res Int. (2016):1–11. doi: 10.1155/2016/1497213
57. Shimo K, Hasegawa M, Mizutani S, Hasegawa T, Ushida T. Effects of a 12-week workplace counseling program on physical activity and low back pain: a pilot randomized controlled study. J Back Musculoskelet Rehabil. (2021) 34(5):845–52. doi: 10.3233/BMR-200178
58. Spenkelink CD, Hutten MMR, Hermens HJ, Greitemann BOL. Assessment of activities of daily living with an ambulatory monitoring system: a comparative study in patients with chronic low back pain and nonsymptomatic controls. Clin Rehabil. (2002) 16(1):16–26. doi: 10.1191/0269215502cr463oa
59. Tomkins-Lane C, Sun R, Muaremi A, Zheng P, Mohan M, Ith MA, et al. Objective features of sedentary time and light activity differentiate people with low back pain from healthy controls: a pilot study. Spine J. (2022) 22(4):629–34. doi: 10.1016/j.spinee.2021.11.005
60. van Rooij WMJ, Senden R, Heyligers IC, Cuppen PMAH, van Hemert WLW, Grimm B. Physical functioning of low back pain patients: perceived physical functioning and functional capacity, but not physical activity is affected. Disabil Rehabil. (2015) 37(24):2257–63. doi: 10.3109/09638288.2015.1019010
61. van Weering M, Vollenbroek-Hutten M, Tönis T, Hermens H. Daily physical activities in chronic lower back pain patients assessed with accelerometry. Eur J Pain. (2009) 13(6):649–54. doi: 10.1016/j.ejpain.2008.07.005
62. van Weering M, Vollenbroek-Hutten M, Hermens H. The relationship between objectively and subjectively measured activity levels in people with chronic low back pain. Clin Rehabil. (2011) 25(3):256–63. doi: 10.1177/0269215510380828
63. Verbunt JA, Westerterp KR, van der Heijden GJ, Seelen HA, Vlaeyen JW, Knottnerus JA. Physical activity in daily life in patients with chronic low back pain. Arch Phys Med Rehabil. (2001) 82(6):726–30. doi: 10.1053/apmr.2001.23182
64. Vlaeyen JWS, de Jong J, Geilen M, Heuts PHTG, van Breukelen G. The treatment of fear of movement/(re)injury in chronic low back pain: further evidence on the effectiveness of exposure in vivo. Clin J Pain. (2002) 18(4):251–61. doi: 10.1097/00002508-200207000-00006
65. Xu W, Zhang Y, Wang Z, Dorsey SG, Starkweather A, Kim K. Pain self-management plus activity tracking and nurse-led support in adults with chronic low back pain: feasibility and acceptability of the problem-solving pain to enhance living well (PROPEL) intervention. BMC Nurs. (2023) 22(1):1–13. doi: 10.1186/s12912-022-01080-0
66. Zheng X, Reneman MF, Preuper RHS, Otten E, Lamoth CJ. Relationship between physical activity and central sensitization in chronic low back pain: insights from machine learning. Comput Methods Programs Biomed. (2023) 232:107432. doi: 10.1016/j.cmpb.2023.107432
67. van den Berg-Emons RJ, Schasfoort FC, de Vos LA, Bussmann JB, Stam HJ. Impact of chronic pain on everyday physical activity. Eur J Pain. (2007) 11(5):587–93. doi: 10.1016/j.ejpain.2006.09.003
68. Smuck M, Tomkins-Lane C, Ith MA, Jarosz R, Kao MCJ. Physical performance analysis: a new approach to assessing free-living physical activity in musculoskeletal pain and mobility-limited populations. Plos One. (2017) 12(2):e0172804. doi: 10.1371/journal.pone.0172804
69. Vanhelst J. Quantification de l’activité physique par l’accélérométrie. Rev Epidemiol Sante Publique. (2019) 67(2):126–34. doi: 10.1016/j.respe.2018.10.010
70. Stevens ML, Gupta N, Eroglu EI, Crowley PJ, Eroglu B, Bauman A, et al. Thigh-worn accelerometry for measuring movement and posture across the 24-hour cycle: a scoping review and expert statement. BMJ Open Sport Exerc. Med. (2020) 6(1):e000874. doi: 10.1136/bmjsem-2020-000874
71. Schall MC, Fethke NB, Chen H. Working postures and physical activity among registered nurses. Appl Ergon. (2016) 54:243–50. doi: 10.1016/j.apergo.2016.01.008
72. Perry MA, Hendrick PA, Hale L, Baxter GD, Milosavljevic S, Dean SG, et al. Utility of the RT3 triaxial accelerometer in free living: an investigation of adherence and data loss. Appl Ergon. (2010) 41(3):469–76. doi: 10.1016/j.apergo.2009.10.001
73. Sani S, Massie S, Wiratunga N, Cooper K. Learning deep and shallow features for human activity recognition. In: Li G, Ge Y, Zhang Z, Jin Z, éditeurs. Blumenstein M, knowledge science, engineering and management (KSEM 2017): 10th international conference, KSEM 2017; August 19-20, 2017. Melbourne, Vic, Australia (2017). p. 469–82
74. Lim S, D’Souza C. A narrative review on contemporary and emerging uses of inertial sensing in occupational ergonomics. Int J Ind Ergon. (2020) 76:102937. doi: 10.1016/j.ergon.2020.102937
75. Verbunt JA, Huijnen IPJ, Köke A. Assessment of physical activity in daily life in patients with musculoskeletal pain. Eur J Pain. (2009) 13(3):231–42. doi: 10.1016/j.ejpain.2008.04.006
76. Kim K, Ramesh D, Perry M, Bernier KM, Young EE, Walsh S, et al. Effects of physical activity on neurophysiological and gene expression profiles in chronic back pain: study protocol. Nurs Res. (2020) 69(1):74–81. doi: 10.1097/NNR.0000000000000400
77. Hurley DA, Tully MA, Lonsdale C, Boreham CAG, van Mechelen W, Daly L, et al. Supervised walking in comparison with fitness training for chronic back pain in physiotherapy: results of the SWIFT single-blinded randomized controlled trial. Pain. (2015) 156(1):131–47. doi: 10.1016/j.pain.0000000000000013
78. Patel MS, Asch DA, Volpp KG. Wearable devices as facilitators, not drivers, of health behavior change. J Am Med Assoc. (2015) 313(5):459–60. doi: 10.1001/jama.2014.14781
79. van Weering M, Vollenbroek-Hutten MMR, Kotte EM, Hermens HJ. Daily physical activities of patients with chronic pain or fatigue versus asymptomatic controls. A systematic review. Clin Rehabil. (2007) 21(11):1007–23. doi: 10.1177/0269215507078331
80. Ryan CG, Grant PMM, Dall PM, Gray H, Newton M, Granat MH. Individuals with chronic low back pain have a lower level, and an altered pattern, of physical activity compared with matched controls: an observational study. Aust J Physiother. (2009) 55(1):53–8. doi: 10.1016/S0004-9514(09)70061-3
81. Taylor AM, Phillips K, Patel KV, Turk DC, Dworkin RH, Beaton D, et al. Assessment of physical function and participation in chronic pain clinical trials: IMMPACT/OMERACT recommendations. Pain. (2016) 157(9):1836–50. doi: 10.1097/j.pain.0000000000000577
82. Oliveira CB, Franco MR, Maher CG, Ferreira PH, Morelhão PK, Damato TM, et al. Physical activity–based interventions using electronic feedback may be ineffective in reducing pain and disability in patients with chronic musculoskeletal pain: a systematic review with meta-analysis. Arch Phys Med Rehabil. (2018) 99(9):1900–12. doi: 10.1016/j.apmr.2017.10.013
83. Oliveira CB, Franco MR, Maher CG, Tiedemann A, Silva FG, Damato TM, et al. The efficacy of a multimodal physical activity intervention with supervised exercises, health coaching and an activity monitor on physical activity levels of patients with chronic, nonspecific low back pain (physical activity for back pain (PAyBACK) trial): study protocol for a randomised controlled trial. Trials. (2018) 19(1):40. doi: 10.1186/s13063-017-2436-z
84. Alzahrani H, Mackey M, Stamatakis E, Zadro JR, Shirley D. The association between physical activity and low back pain: a systematic review and meta-analysis of observational studies. Sci Rep. (2019) 9(1):8244. doi: 10.1038/s41598-019-44664-8
85. Hasenbring MI, Verbunt JA. Fear-avoidance and endurance-related responses to pain: new models of behavior and their consequences for clinical practice. Clin J Pain. (2010) 26(9):747–53. doi: 10.1097/AJP.0b013e3181e104f2
86. Debackere F, Clavel C, Roren A, Tran V, Snoubra G, Messai Y, et al. Profiling of low back pain patients for the design of a tailored coaching application. 2022 10th international conference on affective computing and intelligent interaction (ACII) (2022). p. 1–8
87. Rose-Dulcina K, Vuillerme N, Tabard-Fougère A, Dayer R, Dominguez DE, Armand S, et al. Identifying subgroups of patients with chronic nonspecific low back pain based on a multifactorial approach: protocol for a prospective study. JMIR Res Protoc. (2018) 7(4):e104. doi: 10.2196/resprot.9224
88. Pryce R, Johnson M, Goytan M, Passmore S, Berrington N, Kriellaars D. Relationship between ambulatory performance and self-rated disability in patients with lumbar spinal stenosis. Spine. (2012) 37(15):1316–23. doi: 10.1097/BRS.0b013e31824a8314
89. Mercer K, Li M, Giangregorio L, Burns C, Grindrod K. Behavior change techniques present in wearable activity trackers: a critical analysis. JMIR Mhealth Uhealth. (2016) 4(2):e4461. doi: 10.2196/mhealth.4461
90. Arefyev A, Lechauve JB, Gay C, Gerbaud L, Chérillat MS, Figueiredo IT, et al. Activité physique et objets connectés: comment favoriser l’adhésion des patients? La Revue de L’infirmière. (2018) 67(237):38. doi: 10.1016/j.revinf.2017.11.018
91. Patel KV, Dansie EJ, Turk DC. Impact of chronic musculoskeletal pain on objectively measured daily physical activity: a review of current findings. Pain Manage. (2013) 3(6):467–74. doi: 10.2217/pmt.13.46
92. Cavanagh R, Bhargava A, Gleason A, Micheel L, Ciulla R, Hoyt T. Use of health technologies for low back pain in the military health system. J Technol Behav sci. (2019) 4(4):360–71. doi: 10.1007/s41347-019-00107-9
93. Brickwood KJ, Watson G, O’Brien J, Williams AD. Consumer-based wearable activity trackers increase physical activity participation: systematic review and meta-analysis. JMIR Mhealth Uhealth. (2019) 7(4):e11819. doi: 10.2196/11819
94. Davergne T, Rakotozafiarison A, Servy H, Gossec L. Wearable activity trackers in the management of rheumatic diseases: where are we in 2020? Sensors. (2020) 20(17):4797. doi: 10.3390/s20174797
Keywords: physical activity, chronic low back pain, accelerometer, inertial measurement unit, scoping review
Citation: Berger M, Bertrand AM, Robert T and Chèze L (2023) Measuring objective physical activity in people with chronic low back pain using accelerometers: a scoping review. Front. Sports Act. Living 5:1236143. doi: 10.3389/fspor.2023.1236143
Received: 14 June 2023; Accepted: 6 October 2023;
Published: 1 November 2023.
Edited by:
Charlotte Edwardson, University of Leicester, United KingdomReviewed by:
Julie Soulard, Université Grenoble Alpes, France© 2023 Berger, Bertrand, Robert and Chèze. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mathilde Berger bWF0aGlsZGUuYmVyZ2VyQGhldHNsLmNo
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.