- 1Department of Exercise, Sport and Lifestyle Medicine, Faculty of Medicine and Health Sciences, Institute of Sport and Exercise Medicine, Stellenbosch University, Stellenbosch, South Africa
- 2Division of Physiotherapy, Department of Health and Rehabilitation Sciences, Faculty of Medicine and Health Sciences, Stellenbosch University, Stellenbosch, South Africa
Understanding the challenges football (soccer) players face during adolescence is fundamental to avoid disruptions in their development due to injury. This mini review will describe basic concepts of somatic growth and biological maturity, examine data from 53 prospective epidemiological studies on high-level youth football players and discuss how age, growth and maturity may affect the injury patterns observed. Based on the existing evidence, at least every third player sustains an injury during a football season. The thigh (median for studies of boys: 25%, median for girls: 21%), ankle (b: 18%, g: 30%), knee (b: 17%, g: 18%) and hip/groin (b: 14%, g: 10%) are the body parts injured most often, while muscle strains (b: 31%, g: 25%), sprains (b: 20%, g: 27%) and contusions (b: 17%, g: 16%) are the most common injury types. Injury trends are, however, not consistent throughout adolescence, and players' age, maturity status and position relative to peak height velocity (PHV) have shown to influence the number, type and location of injuries sustained. Despite a high volume of observational injury studies published on high-level youth players, girls (7 studies) and settings outside of Europe (included in 23% of studies) are underrepresented and should receive extra attention in the future. Based on the available epidemiological data, tailored injury reduction programmes can be considered in youth football, alongside application of general training principles such as progression, variation and individualization which may be especially important during vulnerable phases such as the adolescent growth spurt.
Introduction
If you have been involved in youth football (soccer) in any capacity – that be as a player, coach, parent, physiotherapist or team coordinator – you probably have at least one story about “that player who grew 10 cm over the summer,” “seemingly fully-grown adults playing alongside children” or “the player who could have reached the top if it wasn't for that injury.” Stories like these make youth football both interesting and challenging, with some unique obstacles not seen at the senior level.
A general understanding of the changes adolescents experience when transitioning from children to adults [see Malina et al. (1)] is essential for anyone working in youth sports, and awareness around issues relating to injury risk may allow more talents to stay in their sport and develop to their full potential. Injuries keep players out of sessions and disrupt their development, which again may lead to them being dropped from a development programme (2). In some instances, they can have long-term health consequences (3). Although preventing all injuries is near impossible, it is in everyone's interest to limit the frequency and severity of injury. In this mini review, we will explore typical injury patterns in youth football and examine how growth and biological maturation may affect the chances of sustaining one.
Understanding concepts of growth and maturity
Phrases like “the growth spurt,” “maturity timing” or “maturity status” can be confusing if used without a clear indication of what they refer to. In research, inconsistent terminology complicates aggregation of findings and in practice it may be a barrier for clear communication within a coaching team or to players and parents. The aim of this first section is therefore to define and clarify some key concepts. Although this review focuses on somatic (bodily) growth and biological maturation, it should be acknowledged that other aspects not covered, such as cognitive, behavioral and social development, or development of motor and psychological skills, also may affect the risk of sustaining injuries (4), which are considered both multifactorial, dynamic and complex (5–7).
Somatic growth and the adolescent spurt
Growth can be defined as a change in the size of the whole body or a body part (1). A player's growth can therefore be assessed by measuring changes in physical dimensions (e.g., height, weight or leg length) over time. Growth in height follows a distinct non-linear pattern from birth to adulthood, with rapid changes observed right after birth, relatively steady growth throughout childhood, a new period of high acceleration during puberty, followed by a deceleration until adult height is reached (8).
The changes around puberty are especially interesting in the context of youth football, as the “adolescent growth spurt” takes off around the age of 8–10 years in girls and 10–12 years in boys (9, 10). The point of maximal acceleration (peak height velocity; PHV), where typical height velocities are around 7–9 cm/year (girls) and 8–10 cm/year (boys), occurs at a younger age in girls (around 11–13 years) compared to boys (around 13–15 years) (9, 10). There is, however, large variation in timing and magnitude between individuals, where age at PHV (timing) can range from 9 to 15 (girls) and 12 to 17 (boys) years, and maximal growth velocities (magnitude) can range from 5 to 10 (girls) and 5–12 (boys) cm/year (9, 10). Variation can also be seen between body parts in the same individual, where distal bones typically reach their peak velocity at a younger age compared to bones located higher up (1).
Adolescents also experience a period of accelerated weight gain: peak weight velocity (PWV). Maximal gains around 7–9 kg/year in girls and 9–11 kg/year in boys are common, around the ages of 12–14 years in girls (range: 11–15) and 13–15 years in boys (range: 13–16) (11). It is worth noting that girls, in general, gain proportionally more fat mass while boys add more lean mass (e.g., muscle and bone) (1). These relatively fast changes in height, weight and body composition at varying ages are important to consider, as they can result in large height and weight differences within age groups (12) and may impact both neuromotor coordination and injury risk negatively (13, 14).
Making sense of biological maturity
The concept of growth can be conceptually easy to grasp; maturation on the other hand, is more complex and refers to the progress toward a mature (adult) state (1). In essence, this implies that a specific biological system has a certain end point (i.e., the mature state), and maturation is the journey to reach this endpoint. The end point depends on the system we are looking at; for example, the skeleton starts off as cartilage and matures to ossified bone (skeletal maturity), while sexual maturity is reached with full reproductive function (1, 15).
Adolescence is a phase associated with particularly large changes in different biological systems relating to the onset of puberty (16). The sequence of puberty often follows a typical pattern; however, there will be variation between girls and boys, and between individuals (16). The age at reaching certain maturational landmarks (e.g., PHV or the onset of menstrual cycles) is what we refer to as maturity timing. When comparing similar indicators, these are typically reached at a younger age in girls than in boys (1). The rate of change or time between maturational events (maturity tempo) also varies, meaning that some will be more advanced than others, even if their chronological age is the same. How far an individual has come at a given time point is what we mean by maturity status. In youth football, differences in maturity status are particularly relevant since players most often compete in chronological, not maturity-based, age groups.
Injury patterns in high-level youth football
As mentioned in the introduction, one purpose of reducing the impact of injuries is to maximize developmental opportunities and performance. Understanding injury patterns is therefore fundamental, as we need to know which problems to focus on in order to best mitigate risk (17). The focus in this section will be on high-level adolescent players (e.g., elite, academy, professional club), including data from 53 prospective studies (per March 2022) which reported overall injury outcomes for minimum one season. Although methodological differences (e.g., injury definitions, recorders, classification systems) make comparisons and data aggregation difficult, and relatively few studies have been published on high-level female players, some trends are apparent.
How common and severe are football injuries?
One approach to determining the extent of injuries is to count how many players sustain at least one injury over a season. In boys, this has ranged from 38 to 85% (18–25), with 0.4–2.2 injuries per player per season (19–42). Only one study reported seasonal injury proportion for girls (37%) (43), with another finding an average of 4.3 injuries per player per season (44). The latter also revealed that every second female player experienced an injury problem affecting performance, participation or pain during a given week (44). This suggests that injuries are indeed common in youth football, with a conservative estimate suggesting that at least every third high-level player will be injured once or more during a season.
Counting injuries or calculating the proportion of injured players does not take the time they play football into consideration. This is important, as a team training eight times per week inevitably will see more injuries than a team training once a week; this does not mean that the risk of playing an hour of football is different. Expressing injuries relative to training and match hours is therefore recommended. Using the median of point estimates for reported injury rates (this does not consider the size of each study, nor the uncertainty in their estimates) and keeping methodological differences in mind, the number of injuries per 1,000 h appears similar between genders (Figure 1): around 6.3 (range: 1.3–12.1) for boys (18–20, 24, 26, 27, 29, 31–33, 36, 37, 41, 42, 46–57) and 6.4 (2.1–9.1) for girls (44, 55, 58–60). Matches are consistently associated with greater risk compared to training sessions in both boys (match: 13.4, training: 4.0) and girls (match: 22.4, training: 4.6) (18–20, 24–26, 29, 31–33, 36, 42, 46–50, 53–55, 58, 60–63).
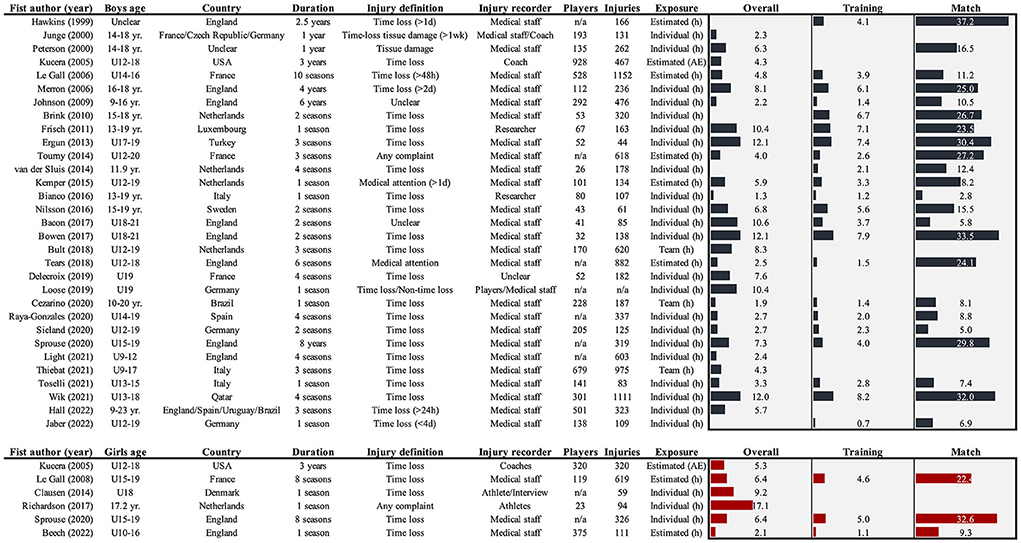
Figure 1. Overview of studies reporting overall, training and/or match injury rates (per 1,000 h or athletic exposures: AE) in high-level youth football players. Where estimates were only provided for subgroups, the average was used to give an idea of the extent, and where rates were presented using multiple definitions, only the narrowest was included (e.g., time loss > medical attention) as these are more comparable between contexts (45). If datasets were overlapping or used in multiple studies, only the main epidemiological study was included.
Injury severity is commonly calculated as the number of days elapsed from the day of injury until the day the player returns to full training and/or is available for match selection (64), often presented as the proportion of injuries falling within defined bins (e.g., percentage of all injuries lasting 7–28 days). Although cut-offs vary slightly between studies and the choice of injury definition affects distributions, the combined findings suggest that 38% (7–74%) of injuries in boys last less than a week, another 38% (16–67%) last between a week and a month, while every fifth injury (21%, 2–37%) lasts more than a month (18, 20, 21, 23, 25, 28, 29, 31–37, 39, 41, 46, 48, 49, 53–56, 61). For girls, a larger proportion of “mild” injuries is observed, with around a half (51%, 38–52%) lasting a week or less, a third (36%, 32–41%) between a week and a month, and the remaining 16% (12–20%) more than a month (55, 58, 60).
What are the most common injury locations and types?
Understanding the injury problem in general is an important first step; however, we need to know which injuries are the most troublesome to design impactful injury reduction programmes that target specific mechanisms and risk factors. Given the high running demands and frequent kicking and tackling actions observed in youth football (65, 66), it is perhaps not surprising that the lower extremities are the most affected – accounting for approximately four out of five injuries in boys and girls (Figure 2). Breaking it down to specific body parts, thigh injuries are the most common among boys (median of percentages reported in studies: 25% of all injuries, range: 11–39%), with the ankle (18%; 9–31%), knee (17%; 7–23%) and hip/groin (14%; 2–33%) also common. In girls, ankle injuries are the most common (30%; 18–39%), followed by injuries to the thigh (21%; 11–35%), knee (18%; 16–25%) and hip/groin (10%; 10–14%). Three main injury types can be identified, with strains (31%; 14–87%), sprains (20%; 9–40%) and contusions (17%; 3–31%) together accounting for two out of three injuries in boys. Sprains appear more common among girls (27%; 27–61%), although they together with strains (25%; 17–33%) and contusions (16%; 8–17%) also account for roughly two thirds of all injuries reported. Taken together, these patterns are similar to senior players (67, 68), and it could be argued that football players – for the most part – sustain “typical football injuries” regardless of age and gender when proportions are used.
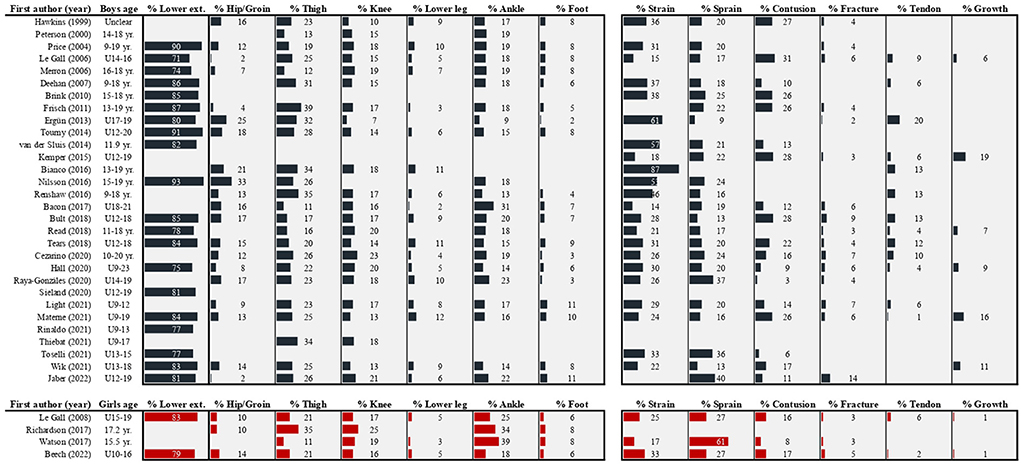
Figure 2. Reported injury proportions within location and type categories in high-level youth football players. Not all studies used the same classifications, and a best effort was made to place injuries in the most applicable category. In studies reporting subgroup proportions without values for the full sample, the average was entered to give an idea of the overall pattern. Where multiple studies were published with the same or overlapping dataset, only the main epidemiological paper was included.
Isolated proportions for body parts and types are of limited value since they do not consider injury severity, nor do they tell us which injury types to focus on within each location or where different types are located. Reporting injury burden (i.e., days lost relative to hours of football exposure) for combinations of body parts and injury types (or specific diagnoses) would therefore represent an advancement in our understanding (69). Few studies provide this, but there is evidence to show that it changes our interpretation of surveillance data. As an example, a study of academy boys (24) highlighted that thigh muscle injuries were the most common (16% of all injuries, accounting for 11% of total days lost), but joint sprains to the knee had the greatest impact on player participation (only 3% of injuries, but 18% of days lost). Similarly, contusions, which ranked high in terms of proportions, were of low severity and consequently had a relatively low impact (17% of injuries, but only 5% of days lost). Of particular interest to youth populations, injuries to the skeleton were the most burdensome tissue type in this study (23% of injuries, 34% of days lost), although muscle/tendon injuries were the most common (27% of injuries, 16% of days lost). These insights would be lost if severity was not accounted for.
Do injuries depend on age, growth and maturity?
A wide span in age groups combined with individual differences in timing and tempo of growth and maturation make “youth football players” a heterogeneous population. Some studies will include players closer to childhood, others closer to the senior level, and within age groups there will be variation at the individual level. This section will examine the potential influence age, growth and maturation can have on injury patterns.
Age-related injury patterns
In general, injury rates are not the same across age groups; however, the age-related pattern is not unified based on the available research. Several studies indicate that rates increase with age (24, 25, 28, 31, 34, 35, 41, 54), although others report less clear patterns or bell-shaped relationships peaking around the U15-16 groups (20, 23, 26, 27, 29, 30, 37, 39, 48, 53). Injury severity and burden also appears to be influenced by age, often peaking in the U14-16 age groups (21, 24, 35, 37, 53). While mainly examined in boys, increasing injury incidence and burden with age was also observed in a recent study of girls (60), although contrasted by another showing a lower incidence in U19 players compared to U15 (58). An increased risk with age could potentially be explained by players being stronger, faster and heavier as they grow, mature and accumulate training experience. Furthermore, training sessions and matches may be more intense and carry more significance as competition intensifies. Having sustained a previous injury is also more likely with age, which is a strong risk factor for new injuries (70). Changes associated with the growth spurt (e.g., more fragile growth plates, differences in tissue adaptation, decreased bone-mineral density) (71–74) are often used to explain the higher rate of severe injuries and higher burden observed around the years of expected PHV and PWV. Finally, injury trends differ depending on injury type, with more growth-related injuries observed in younger players and more muscle injuries and joint/ligament sprains in older players (21, 24, 28, 29, 35, 39, 56) – likely influenced by players' absolute maturity status.
Absolute maturity and injury risk
Some tissues may be more prone to injuries prior to reaching their mature state, such as an underdeveloped brain that appears more prone to concussions, thicker and more fragile cartilage, and a growing skeleton (4). Especially the latter has received attention in youth sports, as skeletal conditions (e.g., Osgood-Schlatter disease) are common and can cause problems for years (75). Some injuries (e.g., fractures through, or extreme load on, the growth plate) have the potential to disrupt normal growth patterns if not managed adequately (76).
Absolute maturity (i.e., how close a player is to the mature state) is an interesting concept in terms of injuries. Several studies have demonstrated a pattern where injuries that involve growth areas are less common in players closer to skeletal maturity or adult height (77–79), for whom muscle, joint and ligament injuries are more prominent (78, 79). This likely reflects which tissues and structures represent the “weak link” in the muscle-tendon-skeletal chain; the skeletal attachment site (apophysis) is relatively weaker in immature players, while muscles, ligaments and tendons yield sooner in players with a mature skeleton (80). As consequence, the same mechanisms may lead to different pathologies depending on maturity. For example, a gradual overload may cause apophysitis in an immature athlete but tendinopathy in a mature athlete, and a sudden force may lead to an avulsion in the immature player but a muscle strain in the mature player (80). This theory also aligns with observations that growth-related injuries appear in a bottom-to-top pattern depending on maturity status and age (79, 81), matching the typical distal-to-proximal skeletal maturation process (1, 82).
Relative maturity and injury risk
Relative maturity (i.e., players maturing earlier or later than others; early, average or late maturer) is perhaps the most obvious concern when discussing maturation and injuries, as this comes back to the issue of early and late maturing players training and competing within the same age groups. Intuitively, the later maturing player would seem more injury prone; however, this is not clear in the literature. Early football studies measuring skeletal age found no differences in overall injury risk between relative maturity categories (i.e., early, on time, late) (47, 78), while two recent studies found that early maturing players actually had a greater risk of injury (77, 83). Studies using anthropometric equations also provide conflicting results, with a Dutch study reporting increased overuse injury risk in later maturing players (but only before and during the year around PHV) (84), an English study reporting no difference in non-contact injury risk between early, normal or late maturing players when PHV-period (pre-, circa-, post-PHV) was accounted for (85), and a Spanish study finding a greater burden of overall and growth-related injuries in late vs. normal maturing players (but not compared to early maturing) before PHV, and no differences between relative maturity categories during or after PHV (40).
Rapid growth and injury risk
Although it is difficult to differentiate effects of growth and maturity, higher growth rates (e.g., changes in height, leg length or body mass index) (19, 38, 86, 87) and the circa-PHV period (the months or years around the estimated or observed PHV) (37, 40, 63, 85) have been associated with increased injury risk in high-level youth football. Most studies use relatively broad injury outcomes (e.g., all injuries combined or all overuse injuries), but there is some evidence suggesting that effects of rapid growth are type-dependent, with injury rates for skeletal growth areas particularly elevated during PHV (40). This fits well with the proposed underlying mechanisms for a growth-injury relationship. First, growth plates tend to be thicker and more fragile when growth is at its fastest, making them more susceptible to injuries (71). Second, slower adaptation of tendons and apophyses to a lengthening skeleton compared to muscles may cause increased tension on weaker structures (72). Changes in limb length and mass also increase the force required to move them, which theoretically leads to greater strain on the apophyses (72). Third, delayed bone mineralisation has been observed during rapid growth, coinciding with increased fracture rates; this suggests a period of relative bone fragility (73, 74). Finally, changes in body proportions have been associated with temporarily decreased neuromuscular control (“adolescent awkwardness”), which again may be an injury risk factor (13, 88). While these theories are plausible explanations for players being particularly vulnerable during the adolescent growth spurt, they are rarely included in injury studies and the actual importance of each factor remains unclear.
Summary
It is clear that injuries are common in high-level male and female youth football players, with strains and sprains to the lower limb dominating among both genders. Injury patterns and the type of injuries recorded do, however, depend on the age group observed, players' absolute maturity status and where a player is in relation to the adolescent growth spurt. This warrants age- and maturity-specific prevention programmes, and one can neither assume that all youth players are the same, nor that interventions that work in senior players automatically transfer to age group football.
What are the research gaps?
While our understanding of youth injuries is constantly improving, some areas are still lacking. First, our knowledge originates from a relatively narrow sample. Nine out of ten publications at this playing level report injury data only for boys, and there is little to no data on growth or maturation as risk factors in high-level girls' football. Additionally, epidemiology studies are mainly conducted in European settings (85%). Consequently, there is a demographic and geographic imbalance in the literature, mainly considering data from European boys. Second, there is a need for studies with a larger number of injuries to better understand where injury reduction efforts should be focused. There is now sufficient data to confidently say something about injury proportions for separate body parts and injury types (especially in boys), and future studies should attempt to report these in combination, preferably using burden metrics and differentiating match and training injuries. Third, many studies do not record exposure at the individual level. This is essential for accurate estimates of injury incidence and burden, and a requirement to address risk factors such as growth and maturation.
How can this be used in practice?
Given the pattern of diverse injury locations and types, general prevention programmes (e.g., FIFA 11+ which has been shown to reduce injury risk in young footballers by a third) (89) targeting a large range of potential injuries can be considered appropriate. Keeping the main concepts intact, these can be tailored to suit your specific context (e.g., available time and resources) and increase the chances of successful implementation (90). Detecting and taking pain seriously at an early stage seems important to allow for appropriate management and may limit the time away from sports (91). This may also allow players to continue taking part in sessions, modifying their participation and activities rather than completely removing them from the team (92).
During the adolescent growth spurt and prior to skeletal maturity, it may be necessary to focus more on general movement skills and progressive physical development, being extra careful with increases in load (especially high-impact tasks, such as jumping, acceleration, deceleration) and allowing for sufficient rest and nutrition between sessions (93, 94). Overall load management (e.g., coordinating school, club and regional/national commitments) is particularly challenging, but important, at the youth level (95, 96). Finally, each player must be considered differently. With variations in growth and maturity timing and tempo, individuals will face challenges at different ages. Structured growth and maturity assessments are an option where resources allow it (93, 97); however, observing, talking to, and educating players and parents can perhaps be equally effective. Ultimately, we are all working toward a similar target: to provide players with opportunities to reach their own goals, hopefully enjoying the journey along the way!
Author contributions
The author confirms being the sole contributor of this work and has approved it for publication.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Malina RM, Bouchard C, Bar-Or O. Growth, Maturation, and Physical Activity. 2nd ed Champagne, IL: Human Kinetics. (2004).
2. Larruskain J, Lekue JA, Martin-Garetxana I, Barrio I, McCall A, Gil SM. Injuries are negatively associated with player progression in an elite football academy. Sci Med Football. (2021) 1−10. doi: 10.1080/24733938.2021.1943756
3. Maffulli N, Longo UG, Gougoulias N, Loppini M, Denaro V. Long-term health outcomes of youth sports injuries. Br J Sports Med. (2010) 44:21–5. doi: 10.1136/bjsm.2009.069526
4. McKay D, Broderick C, Steinbeck K. The adolescent athlete: a developmental approach to injury risk. Pediatr Exerc Sci. (2016) 28:488–500. doi: 10.1123/pes.2016-0021
5. Meeuwisse WH. Assessing causation in sport injury: a multifactorial model. Clin J Sport Med. (1994) 4:166–70. doi: 10.1097/00042752-199407000-00004
6. Meeuwisse WH, Tyreman H, Hagel B, Emery C. A dynamic model of etiology in sport injury: the recursive nature of risk and causation. Clin J Sport Med. (2007) 17:215–9. doi: 10.1097/JSM.0b013e3180592a48
7. Bittencourt NFN, Meeuwisse WH, Mendonca LD, Nettel-Aguirre A, Ocarino JM, Fonseca ST. Complex systems approach for sports injuries: moving from risk factor identification to injury pattern recognition-narrative review and new concept. Br J Sports Med. (2016) 50:1309–14. doi: 10.1136/bjsports-2015-095850
8. Tanner JM, Whitehouse RH, Takaishi M. Standards from birth to maturity for height, weight, height velocity, and weight velocity: British children, 1965. II. Arch Dis Child. (1966) 41:613–35. doi: 10.1136/adc.41.220.613
9. Largo RH, Gasser T, Prader A, Stuetzle W, Huber PJ. Analysis of the adolescent growth spurt using smoothing spline functions. Ann Hum Biol. (1978) 5:421–34. doi: 10.1080/03014467800003071
10. Preece MA, Baines MJ, A. new family of mathematical models describing the human growth curve. Ann Hum Biol. (1978) 5:1–24. doi: 10.1080/03014467800002601
11. Tanner JM, Whitehouse RH, Takaishi M. Standards from birth to maturity for height, weight, height velocity, and weight velocity: British children, 1965. I. Arch Dis Child. (1966) 41:454–71. doi: 10.1136/adc.41.219.454
12. MacMaster C, Portas M, Parkin G, Cumming S, Wilcox C, Towlson C. The effect of bio-banding on the anthropometric, physical fitness and functional movement characteristics of academy soccer players. PLoS ONE. (2021) 16:e0260136. doi: 10.1371/journal.pone.0260136
13. Quatman-Yates CC, Quatman CE, Meszaros AJ, Paterno MV, Hewett TE. A systematic review of sensorimotor function during adolescence: a developmental stage of increased motor awkwardness? Br J Sports Med. (2012) 46:649–55. doi: 10.1136/bjsm.2010.079616
14. Swain M, Kamper SJ, Maher CG, Broderick C, McKay D, Henschke N. Relationship between growth, maturation and musculoskeletal conditions in adolescents: a systematic review. Br J Sports Med. (2018) 52:1246–52. doi: 10.1136/bjsports-2017-098418
15. Beunen GP, Rogol AD, Malina RM. Indicators of biological maturation and secular changes in biological maturation. Food Nutr Bull. (2006) 27(4 Suppl):S244–56. doi: 10.1177/15648265060274S508
16. Wolf RM, Long D. Pubertal development. Pediatr Rev. (2016) 37:292–300. doi: 10.1542/pir.2015-0065
17. van Mechelen W, Hlobil H, Kemper HC. Incidence, severity, aetiology and prevention of sports injuries. A review of concepts. Sports Med. (1992) 14:82–99. doi: 10.2165/00007256-199214020-00002
18. Frisch A, Urhausen A, Seil R, Croisier JL, Windal T, Theisen D. Association between preseason functional tests and injuries in youth football: a prospective follow-up. Scand J Med Sci Sports. (2011) 21:e468–476. doi: 10.1111/j.1600-0838.2011.01369.x
19. Kemper GL, van der Sluis A, Brink MS, Visscher C, Frencken WG, Elferink-Gemser MT. Anthropometric injury risk factors in elite-standard youth soccer. Int J Sports Med. (2015) 36:1112–7. doi: 10.1055/s-0035-1555778
20. Cezarino LG, Gruninger B, Scattone Silva R. Injury profile in a brazilian first-division youth soccer team: a prospective study. J Athl Train. (2020) 55:295–302. doi: 10.4085/1062-6050-449-18
21. Hall ECR, Larruskain J, Gil SM, Lekue JA, Baumert P, Rienzi E, et al. An injury audit in high-level male youth soccer players from English, Spanish, Uruguayan and Brazilian academies. Phys Ther Sport. (2020) 44:53–60. doi: 10.1016/j.ptsp.2020.04.033
22. Sugimoto D, Loiacono AJ, Blenis A, Morse JM, Borg DR, Meehan WP 3rd. Risk factors in elite, adolescent male soccer players: prospective study. Clin Pediatr. (2020) 59:596–605. doi: 10.1177/0009922820916895
23. Rinaldo N, Gualdi-Russo E, Zaccagni L. Influence of size and maturity on injury in young elite soccer players. Int J Environ Res Public Health. (2021) 18:3120. doi: 10.3390/ijerph18063120
24. Wik EH, Lolli L, Chamari K, Materne O, Di Salvo V, Gregson W, et al. Injury patterns differ with age in male youth football: a four-season prospective study of 1111 time-loss injuries in an elite national academy. Br J Sports Med. (2021) 55:794–800. doi: 10.1136/bjsports-2020-103430
25. Jaber A, Weishorn J, Berrsche G, Ott H, Bangert Y. Injury profile among elite youth male football players in a German Academy. Int J Sports Med. (2022) 43:138–44. doi: 10.1055/a-1516-4139
26. Peterson L, Junge A, Chomiak J, Graf-Baumann T, Dvorak J. Incidence of football injuries and complaints in different age groups and skill-level groups. Am J Sports Med. (2000) 28:S51–57. doi: 10.1177/28.suppl_5.s-51
27. Junge A, Chomiak J, Dvorak J. Incidence of football injuries in youth players. Comparison of players from two European regions. Am J Sports Med. (2000) 28:S47–50. doi: 10.1177/28.suppl_5.s-47
28. Price RJ, Hawkins RD, Hulse MA, Hodson A. The Football Association medical research programme: an audit of injuries in academy youth football. Br J Sports Med. (2004) 38:466–71. doi: 10.1136/bjsm.2003.005165
29. Le Gall F, Carling C, Reilly T, Vandewalle H, Church J, Rochcongar P. Incidence of injuries in elite French youth soccer players: a 10-season study. Am J Sports Med. (2006) 34:928–38. doi: 10.1177/0363546505283271
30. Deehan DJ, Bell K, McCaskie AW. Adolescent musculoskeletal injuries in a football academy. J Bone Jt Surg Br. (2007) 89:5–8. doi: 10.1302/0301-620X.89B1.18427
31. Tourny C, Sangnier S, Cotte T, Langlois R, Coquart J. Epidemiologic study of young soccer player's injuries in U12 to U20. J Sports Med Phys Fitness. (2014) 54:526–35.
32. Bianco A, Spedicato M, Petrucci M, Messina G, Thomas E, Nese Sahin F, et al. A prospective analysis of the injury incidence of young male professional football players on artificial turf. Asian J Sports Med. (2016) 7:e28425. doi: 10.5812/asjsm.28425
33. Nilsson T, Ostenberg AH, Alricsson M. Injury profile among elite male youth soccer players in a Swedish first league. J Exerc Rehabil. (2016) 12:83–9. doi: 10.12965/jer.1632548.274
34. Renshaw A, Goodwin PC. Injury incidence in a Premier League youth soccer academy using the consensus statement: a prospective cohort study. BMJ Open Sport Exerc Med. (2016) 2:e000132. doi: 10.1136/bmjsem-2016-000132
35. Read PJ, Oliver JL, De Ste Croix MBA, Myer GD, Lloyd RS. An audit of injuries in six english professional soccer academies. J Sports Sci. (2018) 36:1542–8. doi: 10.1080/02640414.2017.1402535
36. Tears C, Chesterton P, Wijnbergen M. The elite player performance plan: the impact of a new national youth development strategy on injury characteristics in a premier league football academy. J Sports Sci. (2018) 36:2181–8. doi: 10.1080/02640414.2018.1443746
37. Bult HJ, Barendrecht M, Tak IJR. Injury risk and injury burden are related to age group and peak height velocity among talented male youth soccer players. Orthop J Sports Med. (2018) 6:2325967118811042. doi: 10.1177/2325967118811042
38. Rommers N, Rossler R, Goossens L, Vaeyens R, Lenoir M, Witvrouw E, et al. Risk of acute and overuse injuries in youth elite soccer players: Body size and growth matter. J Sci Med Sport. (2020) 23:246–51. doi: 10.1016/j.jsams.2019.10.001
39. Materne O, Chamari K, Farooq A, Weir A, Holmich P, Bahr R, et al. Injury incidence and burden in a youth elite football academy: a four-season prospective study of 551 players aged from under 9 to under 19 years. Br J Sports Med. (2021) 55:493–500. doi: 10.1136/bjsports-2020-102859
40. Monasterio X, Gil SM, Bidaurrazaga-Letona I, Lekue JA, Santisteban JM, Diaz-Beitia G, et al. The burden of injuries according to maturity status and timing: a two-decade study with 110 growth curves in an elite football academy. Eur J Sport Sci. (2021). doi: 10.1080/17461391.2021.2006316. [Epub ahead of print].
41. Thiebat G, Spreafico A, Mazzoni S, Ravasio G, de Girolamo L, Schoenhuber H. Incidence of injuries in young soccer players: epidemiological study in an Italian elite club. J Sports Med Phys Fitness. (2021) 61:80–6. doi: 10.23736/S0022-4707.20.11157-5
42. Toselli S, Benedetti L, Di Miceli R, Aiello P, Nanni G. Injury risk and maturity status in Italian elite young football player. MLTJ. (2021) 11:592–9. doi: 10.32098/mltj.03.2021.25
43. Watson A, Brickson S, Brooks A, Dunn W. Subjective well-being and training load predict in-season injury and illness risk in female youth soccer players. Br J Sports Med. (2017) 51:194–9. doi: 10.1136/bjsports-2016-096584
44. Richardson A, Clarsen B, Verhagen E, Stubbe JH. High prevalence of self-reported injuries and illnesses in talented female athletes. BMJ Open Sport Exerc Med. (2017) 3:e000199. doi: 10.1136/bmjsem-2016-000199
45. Wik EH, Materne O, Chamari K, Duque JDP, Horobeanu C, Salcinovic B, et al. Involving research-invested clinicians in data collection affects injury incidence in youth football. Scand J Med Sci Sports. (2019) 29:1031–9. doi: 10.1111/sms.13427
46. Merron R, Selfe J, Swire R, Rolf CG. Injuries among professional soccer players of different age groups : a prospective four-year study in an English Premier League Football Club: Research article. Int Sport Med J. (2006) 7:266–76.
47. Johnson A, Doherty PJ, Freemont A. Investigation of growth, development, and factors associated with injury in elite schoolboy footballers: prospective study. BMJ. (2009) 338:b490. doi: 10.1136/bmj.b490
48. Ergun M, Denerel HN, Binnet MS, Ertat KA. Injuries in elite youth football players: a prospective three-year study. Acta Orthop Traumatol Turc. (2013) 47:339–46. doi: 10.3944/AOTT.2013.3177
49. Bacon CS, Mauger AR. Prediction of overuse injuries in professional U18-U21 footballers using metrics of training distance and intensity. J Strength Cond Res. (2017) 31:3067–76. doi: 10.1519/JSC.0000000000001744
50. Bowen L, Gross AS, Gimpel M, Li FX. Accumulated workloads and the acute:chronic workload ratio relate to injury risk in elite youth football players. Br J Sports Med. (2017) 51:452–9. doi: 10.1136/bjsports-2015-095820
51. Delecroix B, Delaval B, Dawson B, Berthoin S, Dupont G. Workload and injury incidence in elite football academy players. J Sports Sci. (2019) 37:2768–73. doi: 10.1080/02640414.2019.1584954
52. Loose O, Fellner B, Lehmann J, Achenbach L, Krutsch V, Gerling S, et al. Injury incidence in semi-professional football claims for increased need of injury prevention in elite junior football. Knee Surg Sports Traumatol Arthrosc. (2019) 27:978–84. doi: 10.1007/s00167-018-5119-8
53. Raya-Gonzalez J, Suarez-Arrones L, Navandar A, Balsalobre-Fernandez C, Saez de. Villarreal E. Injury profile of elite male young soccer players in a spanish professional soccer club: a prospective study during 4 consecutive seasons. J Sport Rehabil. (2020) 29:801–7. doi: 10.1123/jsr.2019-0113
54. Sieland J, Krause F, Kalo K, Wilke J, Vogt L, Banzer W, et al. Injuries and functional performance status in young elite football players: a prospective 2-year monitoring. J Sports Med Phys Fitness. (2020) 60:1363–70. doi: 10.23736/S0022-4707.20.10886-7
55. Sprouse B, Alty J, Kemp S, Cowie C, Mehta R, Tang A, et al. The football association injury and illness surveillance study: the incidence, burden and severity of injuries and illness in men's and women's international football. Sports Med. (2020). doi: 10.1007/s40279-020-01411-8. [Epub ahead of print].
56. Light N, Johnson A, Williams S, Smith N, Hale B, Thorborg K. Injuries in youth football and the relationship to player maturation: an analysis of time-loss injuries during four seasons in an English elite male football academy. Scand J Med Sci Sports. (2021) 31:1324–34. doi: 10.1111/sms.13933
57. Hall ECR, Larruskain J, Gil SM, Lekue JA, Baumert P, Rienzi E, et al. Injury risk is greater in physically mature versus biologically younger male soccer players from academies in different countries. Phys Ther Sport. (2022) 55:111–8. doi: 10.1016/j.ptsp.2022.03.006
58. Le Gall F, Carling C, Reilly T. Injuries in young elite female soccer players: an 8-season prospective study. Am J Sports Med. (2008) 36:276–84. doi: 10.1177/0363546507307866
59. Clausen MB, Zebis MK, Moller M, Krustrup P, Holmich P, Wedderkopp N, et al. High injury incidence in adolescent female soccer. Am J Sports Med. (2014) 42:2487–94. doi: 10.1177/0363546514541224
60. Beech J, Jones B, King R, Bennett P, Young S, Williams S, et al. The incidence and burden of injuries in elite English youth female soccer players. Sci Med Footb. (2022). doi: 10.1080/24733938.2022.2051730. [Epub ahead of print].
61. Hawkins RD, Fuller CW. A prospective epidemiological study of injuries in four English professional football clubs. Br J Sports Med. (1999) 33:196–203. doi: 10.1136/bjsm.33.3.196
62. Brink MS, Visscher C, Arends S, Zwerver J, Post WJ, Lemmink KA. Monitoring stress and recovery: new insights for the prevention of injuries and illnesses in elite youth soccer players. Br J Sports Med. (2010) 44:809–15. doi: 10.1136/bjsm.2009.069476
63. van der Sluis A, Elferink-Gemser MT, Coelho-e-Silva MJ, Nijboer JA, Brink MS, Visscher C. Sport injuries aligned to peak height velocity in talented pubertal soccer players. Int J Sports Med. (2014) 35:351–5. doi: 10.1055/s-0033-1349874
64. Bahr R, Clarsen B, Derman W, Dvorak J, Emery CA, Finch CF, et al. International Olympic Committee consensus statement: methods for recording and reporting of epidemiological data on injury and illness in sport 2020 (including STROBE Extension for Sport Injury and Illness Surveillance (STROBE-SIIS)). Br J Sports Med. (2020) 54:372–89. doi: 10.1136/bjsports-2019-101969
65. Varley MC, Gregson W, McMillan K, Bonanno D, Stafford K, Modonutti M, et al. Physical and technical performance of elite youth soccer players during international tournaments: influence of playing position and team success and opponent quality. Sci Med Football. (2016) 1:18–29. doi: 10.1080/02640414.2016.1230676
66. Parr J, Winwood K, Hodson-Tole E, Deconinck FJA, Hill JP, Cumming SP. Maturity-associated differences in match running performance in elite male youth soccer players. Int J Sports Physiol Perform. (2021) 17:1352–60. doi: 10.1123/ijspp.2020-0950
67. Ekstrand J, Hagglund M, Walden M. Injury incidence and injury patterns in professional football: the UEFA injury study. Br J Sports Med. (2011) 45:553–8. doi: 10.1136/bjsm.2009.060582
68. Mayhew L, Johnson MI, Francis P, Lutter C, Alali A, Jones G. Incidence of injury in adult elite women's football: a systematic review and meta-analysis. BMJ Open Sport Exerc Med. (2021) 7:e001094. doi: 10.1136/bmjsem-2021-001094
69. Bahr R, Clarsen B, Ekstrand J. Why we should focus on the burden of injuries and illnesses, not just their incidence. Br J Sports Med. (2018) 52:1018–21. doi: 10.1136/bjsports-2017-098160
70. Kucera KL, Marshall SW, Kirkendall DT, Marchak PM, Garrett WE Jr. Injury history as a risk factor for incident injury in youth soccer. Br J Sports Med. (2005) 39:462. doi: 10.1136/bjsm.2004.013672
71. Caine D, DiFiori J, Maffulli N. Physeal injuries in children's and youth sports: reasons for concern? Br J Sports Med. (2006) 40:749–60. doi: 10.1136/bjsm.2005.017822
72. Hawkins D, Metheny J. Overuse injuries in youth sports: biomechanical considerations. Med Sci Sports Exerc. (2001) 33:1701–7. doi: 10.1097/00005768-200110000-00014
73. Faulkner RA, Davison KS, Bailey DA, Mirwald RL, Baxter-Jones AD. Size-corrected BMD decreases during peak linear growth: implications for fracture incidence during adolescence. J Bone Miner Res. (2006) 21:1864–70. doi: 10.1359/jbmr.060907
74. Blimkie CJ, Lefevre J, Beunen GP, Renson R, Dequeker J, Van Damme P. Fractures, physical activity, and growth velocity in adolescent Belgian boys. Med Sci Sports Exerc. (1993) 25:801–8. doi: 10.1249/00005768-199307000-00008
75. Holden S, Olesen JL, Winiarski LM, Krommes K, Thorborg K, Holmich P, et al. Is the Prognosis of Osgood-Schlatter Poorer Than Anticipated? A prospective cohort study with 24-month follow-up. Orthop J Sports Med. (2021) 9:23259671211022239. doi: 10.1177/23259671211022239
76. Caine D, Meyers R, Nguyen J, Schoffl V, Maffulli N. Primary periphyseal stress injuries in young athletes: a systematic review. Sports Med. (2022) 52:741–72. doi: 10.1007/s40279-021-01511-z
77. Materne O, Chamari K, Farooq A, Weir A, Holmich P, Bahr R, et al. Association of skeletal maturity and injury risk in elite youth soccer players: a 4-season prospective study with survival analysis. Orthop J Sports Med. (2021) 9:2325967121999113. doi: 10.1177/2325967121999113
78. Le Gall F, Carling C, Reilly T. Biological maturity and injury in elite youth football. Scand J Med Sci Sports. (2007) 17:564–72. doi: 10.1111/j.1600-0838.2006.00594.x
79. Monasterio X, Gil SM, Bidaurrazaga-Letona I, Lekue JA, Santisteban J, Diaz-Beitia G, et al. Injuries according to the percentage of adult height in an elite soccer academy. J Sci Med Sport. (2021) 24:218–23. doi: 10.1016/j.jsams.2020.08.004
80. Brukner P, Khan KM. Brukner & Khan's Clinical Sports Medicine. 4th ed. New York, NY: McGraw-Hill Medical. (2012).
81. Materne O, Chamari K, Farooq A, Tabben M, Weir A, Holmich P, et al. Shedding light on incidence and burden of physeal injuries in a youth elite football academy: a 4-season prospective study. Scand J Med Sci Sports. (2022) 32:165–76. doi: 10.1111/sms.14059
82. Kvist O, Luiza Dallora A, Nilsson O, Anderberg P, Sanmartin Berglund J, Flodmark CE, et al. A cross-sectional magnetic resonance imaging study of factors influencing growth plate closure in adolescents and young adults. Acta Paediatr. (2021) 110:1249–1256. doi: 10.1111/apa.15617
83. Monasterio X, Bidaurrazaga-Letona I, Larruskain J, Lekue JA, Diaz-Beitia G, Santisteban JM, et al. Relative skeletal maturity status affects injury burden in U14 elite academy football players. Scand J Med Sci Sports. (2022) 32:1400–9. doi: 10.1111/sms.14204
84. van der Sluis A, Elferink-Gemser MT, Brink MS, Visscher C. Importance of peak height velocity timing in terms of injuries in talented soccer players. Int J Sports Med. (2015) 36:327–32. doi: 10.1055/s-0034-1385879
85. Johnson DM, Williams S, Bradley B, Sayer S, Murray Fisher J, Cumming S. Growing pains: Maturity associated variation in injury risk in academy football. Eur J Sport Sci. (2020) 20:544–52. doi: 10.1080/17461391.2019.1633416
86. Rommers N, Rossler R, Shrier I, Lenoir M, Witvrouw E, D'Hondt E, et al. Motor performance is not related to injury risk in growing elite-level male youth football players. A causal inference approach to injury risk assessment. J Sci Med Sport. (2021) 24:881–5. doi: 10.1016/j.jsams.2021.03.004
87. Johnson DM, Cumming SP, Bradley B, Williams S. The influence of exposure, growth and maturation on injury risk in male academy football players. J Sports Sci. (2022) 40:1127–36. doi: 10.1080/02640414.2022.2051380
88. Read PJ, Oliver JL, De Ste Croix MB, Myer GD, Lloyd RS. Neuromuscular risk factors for knee and ankle ligament injuries in male youth soccer players. Sports Med. (2016) 46:1059–66. doi: 10.1007/s40279-016-0479-z
89. Soligard T, Myklebust G, Steffen K, Holme I, Silvers H, Bizzini M, et al. Comprehensive warm-up programme to prevent injuries in young female footballers: cluster randomised controlled trial. BMJ. (2008) 337:a2469. doi: 10.1136/bmj.a2469
90. O'Brien J, Santner E, Kroll J. Moving beyond one-size-fits-all approaches to injury prevention: evaluating how tailored injury prevention programs are developed and implemented in academy soccer. J Orthop Sports Phys Ther. (2021) 51:432–9. doi: 10.2519/jospt.2021.10513
91. DiFiori JP, Benjamin HJ, Brenner JS, Gregory A, Jayanthi N, Landry GL, et al. Overuse injuries and burnout in youth sports: a position statement from the American Medical Society for Sports Medicine. Br J Sports Med. (2014) 48:287–8. doi: 10.1136/bjsports-2013-093299
92. Rathleff MS, Winiarski L, Krommes K, Graven-Nielsen T, Holmich P, Olesen JL, et al. Activity modification and knee strengthening for osgood-schlatter disease: a prospective cohort study. Orthop J Sports Med. (2020) 8:2325967120911106. doi: 10.1177/2325967120911106
93. Towlson C, Salter J, Ade JD, Enright K, Harper LD, Page RM, et al. Maturity-associated considerations for training load, injury risk, and physical performance in youth soccer: One size does not fit all. J Sport Health Sci. (2021) 10:403–12. doi: 10.1016/j.jshs.2020.09.003
94. Bergeron MF, Mountjoy M, Armstrong N, Chia M, Cote J, Emery CA, et al. International Olympic Committee consensus statement on youth athletic development. Br J Sports Med. (2015) 49:843–51. doi: 10.1136/bjsports-2015-094962
95. Bjørndal CT, Gjesdal S. The role of sport school programmes in athlete development in Norwegian handball and football. Eur J Sport Soc. (2020) 17:374–96. doi: 10.1080/16138171.2020.1792131
96. Johnson DM, Cumming SP, Bradley B, Williams S. How much training do English male academy players really do? Load inside and outside of a football academy. Int J Sports Sci Coach. (2022). doi: 10.1177/17479541221101847
Keywords: soccer, sports medicine, growth and development, epidemiology, youth
Citation: Wik EH (2022) Growth, maturation and injuries in high-level youth football (soccer): A mini review. Front. Sports Act. Living 4:975900. doi: 10.3389/fspor.2022.975900
Received: 22 June 2022; Accepted: 24 August 2022;
Published: 01 November 2022.
Edited by:
Humberto M. Carvalho, Federal University of Santa Catarina, BrazilReviewed by:
Joe Eisenmann, University of Nebraska at Kearney, United StatesCopyright © 2022 Wik. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eirik Halvorsen Wik, ZXdpa0BzdW4uYWMuemE=
 Eirik Halvorsen Wik
Eirik Halvorsen Wik